Abstract
Background
Acute isolated disorientation of time, chronotaraxis, is an uncommon manifestation of thalamic stroke. To our knowledge, acute thalamic chronotaraxis with MRI findings has not previously been reported.
Objective
To describe five patients with chronotaraxis after thalamic stroke and attempt to demonstrate the correlation between lesion location and neurological findings.
Patients, methods and results
Isolated time disorientation and loss of time sense were found in five of 120 patients (4%) with ischaemic thalamic stroke in our centre. All patients had disorientation to actual date, inability to know the exact time of the day and under or overestimation of the time passed during examination. Patients expressed themselves as having time blindness with an inability to estimate and guess the actual time.
Conclusion
Acute thalamic chronotaraxis is a specific clinical picture that accurately predicts a small artery disease of the thalamus involving the mediodorsal nucleus of the thalamus. This clinical syndrome appears to have a good clinical recovery.
Disorientation of time, place and person, and distortion of personal and extrapersonal memory systems may occur after mediodorsal thalamotomy, and may also be observed in paramedian or polar artery infarction.1,2 Isolated prominent disorientation of time is extremely rare, and the term chronotaraxis has been used to describe this phenomenon.3 The meaning of the Greek name chronotaraxis is distortion or disorientation of the sense of time, such as for dates, seasons of the year, times of the day, and overestimation or underestimation of duration of time.
We present a consecutive series of five patients with chronotaraxis, and attempt to clarify the correlation between lesion location and related behavioural findings.
Patients and methods
Patients were recruited from our prospective hospital based registry of acute stroke. Five patients without previous neuropsychiatric disease (mean age 63 (10) years; range 53–76) or dementia, admitted within 24 h of stroke onset, were evaluated by neurological and neuropsychological examinations. Lesions were assessed with MRI (T1, T2, diffusion weighted and FLAIR imagings), and reproduced on specific anatomical templates of the thalamus.4 All patients were evaluated daily for their orientation to time, place and person, and noted disturbance of time sense and presence of emotional and behavioural abnormalities. Time orientation and sense were assessed by a short questionnaire in all stroke patients. Time performances of a matched control group (30 cases) were calculated as the mean performance with a number of SDs. To determine the evaluation specificity of patients, at least 2 SDs below or above the mean were considered pathological. We considered time disorientation (chronotaraxis) present if the patient was oriented to the place and persons around him at any moment during the examination, but two of the following time evaluations were disturbed: unaware of the exact date (>±2 days), inability to estimate the exact time of the examination (>±2 h), over or underestimation of the duration of time of the examination performed by his physician (>±20 minutes), unaware of the season of the year (when asked what season is it? What months are in that season?) or inability to judge how long a trip from home to hospital or from home to the centre of his town by car should take (>±20 minutes). We noted all inaccurate estimations of time outside the mean ±2SDs of the control group. Cognitive functions, short and delayed verbal and non‐verbal memory and attention were evaluated by the Mini‐Mental State Examination, word list learning and delayed recall, Rey–Osterrieth Complex Figure Test copy and delayed recall, and digit spans backwards and forwards. Patients were followed for 6 months with standard neurological examinations and evaluation of the orientation of time.
All patients had disorientation to actual date, inability to estimate the exact time of the day and under or overestimation of the time passed during the examination. Patients expressed themselves as having time blindness, with inability to estimate and know the actual time, and guess the passed time since they were in hospital. Three patients (Nos 1, 2, 3) had disorientation to actual season of the year. After the first week of stroke, patient Nos 1 and 2 also had disorientation to place which recovered in 1 week. Patient Nos 1, 2 and 3 presented with mild impairments in the delayed recall verbal and non‐verbal memory tests (table 1). Luria's and Stroop's frontal function tests were normal in all patients. In patient Nos 3, 4 and 5, chronotaraxis disappeared in the first month of stroke but in patient No 2 it continued for 2 months. Patient No 1 was still unable to understand the time of day, or estimate the duration of the interview performed by the physician after 6 months of follow‐up.
Table 1 Clinical and neuropsychological disturbances in the patients.
| Patient/sex/age | Clinical findings | Orientation to date | Orientation to time of day | Orientation to seasons of the year | Estimation of the duration of time | MMSE | ROCF | Word list | Digit span | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C (0–36) | DR (0–36) | Learn (0–10) | DR (0–10) | Forw (0–9) | Back (0–8) | |||||||
| 1/M/69 | Apathy, somnolence, emotional blunting, reduced verbal fluency | D | D | D | D | 25 | 25 | 19 | 7 | 3 | 6 | 4 |
| 2/F/63 | Apathy, vertical gaze palsy | D | D | D | D | 26 | 25 | 20 | 6 | 3 | 7 | 4 |
| 3/M/54 | Inappropriate behaviours, aggressive outbursts, ataxia | D | D | D | D | 27 | 26 | 21 | 7 | 3 | 7 | 5 |
| 4/F/53 | Reduced verbal fluency | D | D | N | D | 28 | 29 | 24 | 8 | 3 | 8 | 6 |
| 5/F/76 | Apathy, emotional blunting | D | D | N | D | 28 | 28 | 24 | 7 | 4 | 8 | 6 |
Back, backwards; C, copy; D, disturbed; DR, delayed recall; F, female; Forw, forwards; Learn, learning; M, male; MMSE, Mini‐Mental State Examination; N, normal; ROCF, Rey‐Osterrieth Complex Figure.
*Values between parentheses are score range.
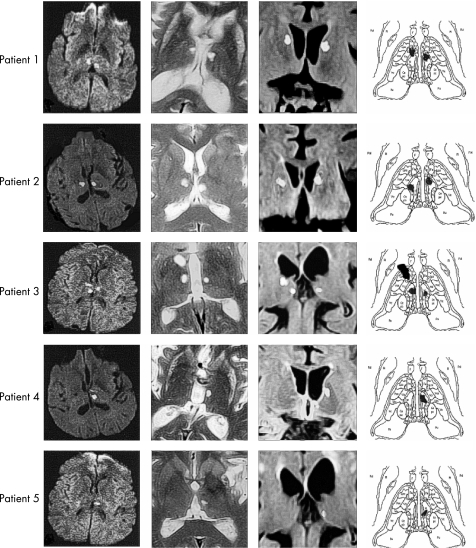
Three patients had bilateral and two patients had unilateral lesions. In all patients, the left mediodorsal nucleus (MD) was involved, and three patients who had bilateral lesions had concomitant right median (No 3), lateral (No 2) or anterior (No 1) MD involvement. Patient No 3 presented an additional anteromedial nucleus lesion extending to the anterior limb of the internal capsule (fig 1).
Figure 1 Diffusion weighted, axial, coronal MRI and schematic representation of the lesions of the patients with chronotaraxis. Apr, nucleus anterior principalis; Cemc, nucleus centralis magnocellularis; Cepc, nucleus centralis parvocellularis; Co, commisural nuclei; Dc, nucleus dorsocaudalis; Fa, nucleus fascicularis; HI, nucleus habenularis lateralis; HM, nucleus hebenulais medialis; IML, internal medullary lamina; Lpo, nucleus lateropolais; M, nucleus dorsomedialis; MTM, tract of Meynert; MTT, mamillothalamic tract; Pu, pulvinar; R, reticular nuclei; Vc, nucleus ventrocaudalis; Vim, nucleus ventro‐oralis intermedius.
Discussion
In our patients with bilateral (in three) and unilateral (in two) circumscribed lesions in the region of the MD nucleus, there was distortion and disorientation to date, season of the year and time of the day. In all patients there was also a tendency to overestimate and sometimes underestimate duration of time, such as the patient's interview or examination time, or stay in hospital or at home. Usually the chronotaraxis was associated with mild memory defects affecting recent as well as delayed recall, and a combination of emotional changes occurred in some patients. In patients with bilateral lesions, there was no feeling of the passage of time or judgement of time, as obtained from intellectual processes or surveillance of changes around them. In patients with unilateral lesions, there was no sense of time, for dates, times of day, feeling of the passage of time and there was tendency to judge and guess time using their intellectual processes. None of the patients could be considered as suffering from dementia, transient global amnesia or amnestic time relevant cognitive disorder, because their daily living and social activities were normal, and there was no prominent cognitive–verbal or non‐verbal amnesic dysfunctions.
Lesions in the region of the thalamic paramedian artery may produce inappropriate social behaviours, impulsive aggressive outbursts, emotional blunting, loss of initiative and absence of spontaneous thoughts or mental activities.5,6,7 We observed some of these symptoms in our patients but they recovered completely within the first week of stoke onset. This observation seems to support the fact that there is no relationship between behavioural–emotional symptoms and time orientation.
In our patients, the MD nucleus was the most frequently involved nucleus. Various circuits may participate in the mechanism of temporal orientation, particularly connections from the medial part (magnocellular MD (MDmc)) to the paralimbic regions (medial and orbital prefrontal cortices), and of the intermediate part of the MD (parvicellular MD (MDpc)) to the dorsolateral and dorsomedial prefrontal cortices, areas 9 and 46. The ventral amygdalofugal pathway links the amygdala with the medial part of the MD, and damage may contribute to disorientation as well as to emotional dysregulation.8,9,10 The multiplicity of the participating circuits explains the fact that circumscribed lesions of the single MD thalamic nucleus produce only loss of orientation to date, season of the year and time of the day, but bilateral lesions may also disturb initiation of intellectual processes or surveillance of temporal changes around them.
Acute isolated chronotaraxis is likely to result from MD lesions. Our results seem to support the view that orientation to time could be distorted by single or bilateral lesions involving the MD nucleus, which is the relay centre between the limbic and cortical pathways, creating sense and perception of time.
Abbreviations
MD - mediodorsal nucleus
Footnotes
Competing interests: None.
References
- 1.Castaigne P, Lhermitte F, Buge A.et al Paramedian thalamic and midbrain infarct: clinical and neuropathological study. Ann Neurol 198110127–148. [DOI] [PubMed] [Google Scholar]
- 2.Graff‐Radford N R, Eslinger P J, Damasio A R.et al Nonhemorrhagic infarction of the thalamus: behavioral, anatomic, and physiologic correlates. Neurology 19843414–23. [DOI] [PubMed] [Google Scholar]
- 3.Spiegel E A, Wycis H T, Orchinik C.et al Thalamic chronotaraxis. Am J Psychiatry 195611397–105. [DOI] [PubMed] [Google Scholar]
- 4.Hirai T, Jones E G. A new parcellation of the human thalamus on the basis of histochemical staining. Brain Res Rev 1989141–34. [DOI] [PubMed] [Google Scholar]
- 5.Stuss D T, Guberman A, Nelson R.et al The neuropsychology of paramedian thalamic infarction. Brain Cogn 19888348–378. [DOI] [PubMed] [Google Scholar]
- 6.Kumral E, Evyapan D, Balkır K.et al Bilateral thalamic infarction. Clinical, etiological and MRI correlates. Acta Neurol Scand 2001103135–142. [DOI] [PubMed] [Google Scholar]
- 7.Schmahmann J D. Vascular syndromes of the thalamus. Stroke 2003342264–2278. [DOI] [PubMed] [Google Scholar]
- 8.Macchi G. Thalamic functions as interpreted from human lesions. In: Steriade M, Jones EG, McCormick DA, eds. Thalamus, vol II: experimental and clinical aspects. New York: Elsevier, 1997542–615.
- 9.Russchen F T, Amaral D G, Price J L. The afferent input to the magnocellular division of the mediodorsal thalamic nucleus in the monkey, Macaca fascicularis. J Comp Neurol 1987256175–210. [DOI] [PubMed] [Google Scholar]
- 10.Siwek D F, Pandya D N. Prefrontal projections to the mediodorsal nucleus of the thalamus in the rhesus monkey. J Comp Neurol 1991312509–524. [DOI] [PubMed] [Google Scholar]