Abstract
Background
Chronic tinnitus is a disabling, almost untreatable, condition, usually accompanied by psychiatric distress. In patients with complex neuropsychiatric diseases, such as chronic pain, with which tinnitus shares pathophysiological similarities, placebo effects may be pronounced. Moreover, it may be difficult to distinguish actual repetitive transcranial magnetic stimulation (rTMS) induced clinical benefits beyond placebo effects in neuropsychiatric patients.
Methods
16 patients with chronic tinnitus underwent a randomised, double blind, crossover, placebo controlled trial of 1 Hz rTMS (120% of motor threshold; 1200 stimuli/day for 5 days) of the left temporoparietal region. Patients were screened for psychiatric comorbidity; additionally, anxiety and depression were monitored throughout the study. Moreover, an original placebo rTMS procedure produced the same activation of ipsilateral face muscles (a condition which may per se change the subjective rating of tinnitus) as the real rTMS.
Results
There were 8 out of 14 responders. Two patients dropped out for transient worsening of tinnitus. Active rTMS induced an overall significant, but transient, improvement (35% of the basal score) of subjective tinnitus perception that was independent of either tinnitus laterality or mood or anxiety changes. No correlations were found between response to rTMS and tinnitus duration, initial subjective score or patient age. When asked after the study was over, 71.4% of patients failed to identify the temporal sequence of the real or sham rTMS interventions.
Conclusion
The beneficial effects of rTMS on tinnitus are independent of mood changes. Moreover, they appear in the context of an original placebo stimulation designed to more closely replicate the somatic sensation of active stimulation. Because of the limited temporal duration of the clinical benefit, these neuromodulatory effects could be mediated by transient functional changes taking place in the neural circuits underlying tinnitus processing.
Tinnitus is a subjective auditory perception of sounds or noise, not triggered by external auditory stimuli, which affects millions of people.1 It is estimated that in 1–3% of the general population tinnitus becomes chronic and sufficiently intrusive to interfere with the patient's quality of life, mainly because of psychiatric distress, including sleep disturbances, thereby leading to work impairment.2 Pharmacological and physical/behavioural treatments in severe cases are generally unsatisfactory.3
Experimental data based on transection of4 or drug effects on5 the cochlear nerve, and in vivo human brain imaging studies,6,7,8 converge in suggesting that tinnitus could be associated with maladaptive plastic brain reorganisations, taking place at multiple brain levels following—and thereafter being maintained independently by—an initial cochlear dysfunction.9 Functional brain changes associated with tinnitus showed hyperactivity of discrete temporoparietal regions, including both the primary auditory cortex (AC)10,11,12,13 and the secondary, or associative, AC.7,11,14,15,16,17,18 More comprehensive views on the generation and maintenance of tinnitus indicate involvement of a broader neural network, most likely including the primary and associative AC (although it is difficult to disentangle the relative contribution of these two areas by positron emission tomography (PET) scans19), part of the limbic system,17 the anterior cingulated cortex18 and higher order processing areas.20,21
More direct evidence for the key role played by the AC in the perception/elaboration of tinnitus comes from studies with repetitive transcranial magnetic stimulation (rTMS), a technique that transiently modulates/disrupts the brain function of the targeted area(s) in several perceptive, motor and cognitive domains22: high‐frequency rTMS (ie, 10 Hz or more for 2 s or less) applied on the scalp overlying the hyperactive left AC produced an intense, short lived tinnitus attenuation (see table 1).16,12,23,24 Although these studies were not designed to “treat” tinnitus, they demonstrate that the AC is definitely involved in the expression of tinnitus. Interestingly, high frequency rTMS has been applied successfully to produce transient clinical benefits in other deafferentation induced disorders, such as chronic neurogenic pain,25,26 which shares pathophysiological similarities with tinnitus in terms of maladaptive plastic changes at the cortical level.27
Table 1 Full papers on repetitive transcranial magnetic stimulation studies (single case reports are not considered) in chronic tinnitus.
| Plewnia 200216 | Eichhammer 200339 | Kleinjung 200513 | De Ridder 200523 | |
|---|---|---|---|---|
| No of patients | 14 | 3 | 14 | 114 |
| Treatment duration | Single application | 5 days | 5 days | Single application |
| rTMS frequency/length of the train/No of stimuli | 10 Hz for 3 s (30 pulses) | 1 Hz (2000 stimuli/day) | 1 Hz (2000 stimuli/day) | 1, 3, 5, 10, 20 Hz (200 pulses each) |
| Stimulus intensity (% of RMT) | 120% | 110% | 110% | 90% |
| Coil type | Figure‐of‐eight | Figure‐of‐eight | Figure‐of‐eight | Circular non‐focal |
| Individual neuronavigation | No | PET guided | PET guided | fMRI guided in 10 |
| Target brain area | Temporoparietal (halfway between C3/T5 or C4/T6) and Pz | PAC | Hyperactive PAC | Unspecified coil positioning “on the AC” in 104 |
| Controlled study | TMS delivered on additional 11 scalp positions | Double blind (placebo TMS with a sham coil) | Double blind (placebo TMS with a sham coil) | Sham with the coil at 90°. Unspecified blindness |
| Crossover | No | Yes | Yes | No |
| Percentage of responders | 57% | 2/3 patients | 78.6% | 53% with active, 63% with sham (but significantly more with active rTMS) |
| Duration of effects after the last rTMS application | Seconds | One week | Up to 6 months | Unspecified, presumably seconds |
| Correlations between rTMS and clinical characteristics | — | Responders had hyperactive PAC | Initial tinnitus grading and symptom duration negatively influenced rTMS response | High frequency better for acute tinnitus; low frequency better for chronic tinnitus |
| Plewnia 200617 | Plewnia 200618 | Langguth 200640 | Fregni 2006 24 | |
|---|---|---|---|---|
| No of patients | 9 | 6 (retested after17) | 28 | 7 |
| Treatment duration | Single application | 20 consecutive working days | 10 consecutive working days | Single application |
| rTMS frequency/length of the train/No of stimuli | 1 Hz for 5, 15 or 30 min (300, 900 or 1800 pulses) | 1 Hz for 30 min/day (1800 pulses/day) | 1 Hz for 33.3 min/day (2000 pulses/day) | 3 trains 10 Hz for 3 s (30 pulses each) |
| Stimulus intensity (% of the RMT) | 120% | 120% | 110% | 120% |
| Coil type | Figure‐of‐eight | Figure‐of‐eight | Figure‐of‐eight | Figure‐of‐eight |
| Individual neuronavigation | PET guided | PET guided | No | No |
| Target brain area | Hyperactive BA 39 or 22 | Hyperactive BA 39 or 22 | Left PAC, determined on 10‐20 EEG system | Left temporoparietal (halfway between C3/T5 and Pz) |
| Controlled study | Double blind (sham delivered on the lower occiput) | Double blind (sham delivered on the lower occiput) | No | Yes, sham coil. Unspecified blindness. Additional scalp positions stimulated |
| Crossover | Yes | Yes | No | No |
| Percentage of responders | 75% | 83.3% | 67.8% | 42% |
| Duration of effects after the last rTMS application | Up to 30 min, dose dependent | 2 weeks | Up to 13 weeks | Less than 5 min |
| Correlations between rTMS and clinical characteristics | Previous tinnitus duration negatively influenced rTMS response | Hyperactivity of the ACC predicted the response to rTMS | Not reported | Responders had less hearing loss |
AC, auditory cortex; ACC, anterior cingulate cortex; BA, Brodman Area; C3, C4, C5, C6, Pz, electrode positions according to the International 10‐20 EEG system; fMRI, functional MRI; PAC, primary auditory cortex; PET, positron emission tomography; RMT, resting motor threshold; rTMS, repetitive transcranial magnetic stimulation.
Medline search updated on 30 October 2006 (keywords: tinnitus, TMS or rTMS). Only peer reviewed international journals are taken into account.
When rTMS is applied at a low frequency (ie, 1 Hz or less) for longer periods of time (tens of minutes, eventually with daily applications), or as continuous theta burst stimulation,28,29 it induces relatively long lasting inhibitory changes in cortical excitability, probably mediated by long term synaptic depression, that can be associated with transient beneficial effects on clinical manifestations of neuropsychiatric disorders characterised by regional cortical hyperactivity30 as painful dystonia related axial spasms31 or obsessive–compulsive disorders.32 Moreover, slow rTMS of the left temporoparietal region significantly attenuated auditory hallucinations in schizophrenia,33,34,35,36,37 the most relevant finding in view of rTMS application in chronic tinnitus. Previous studies of rTMS of temporoparietal regions at 1 Hz in patients with chronic tinnitus (see table 1)13,17,18,38,39,40 generally reported a considerable subjective improvement, occasionally lasting up to 6 months,13 with a dose dependency of rTMS induced beneficial effects.17
Despite the fact that psychiatric comorbidity, such as mood or anxiety disorders, are relevant in chronic tinnitus sufferers,2 this aspect has not been taken into account in previous controlled rTMS studies. Most importantly, there is agreement that the applied placebo conditions were suboptimal41,42,43: this is because active rTMS of the temporoparietal regions may elicit strong activation of ipsilateral muscles supplied by the facial nerve, not reproduced by previous placebo rTMS conditions, but possibly influencing per se perception of tinnitus (see later in the discussion). We present a randomised, double blind, crossover, placebo controlled trial of daily 1 Hz rTMS on chronic tinnitus in which eventual mood changes were also monitored. Moreover, an original placebo condition is introduced, which minimises the possibility of subject awareness of the active or sham rTMS. This is relevant for at least two reasons: (i) patients with tinnitus are known to exhibit a particularly strong placebo response44; (ii) it may be difficult to distinguish the actual rTMS induced clinical benefit beyond a placebo effect in neuropsychiatric patients,45,46 including those with chronic pain26 or tinnitus.3,43
Methods
Patients selection
Sixteen consecutive, fully informed, fully right handed patients were included in the study (see details in table 2), after approval by the local ethics committee. Inclusion criteria were: presence of mono‐ or bilateral tinnitus from more than 1 year, normal neurological examination and normal cranial magnetic resonance. Exclusion criteria were: history of neuropsychiatric disorders or neuroactive treatments (with the exception of antidepressant therapy previously taken for tinnitus therapy, withdrawn for at least 1 month), and presence of significant other medical illness. To exclude concomitant axis I psychiatric disorders, all patients also underwent the Structured Clinical Interview for DSM.
Table 2 Characteristics of the 14 patients who completed the study.
| Patient No/sex | Age (y) | Responder | Hypoacousia | Tinnitus features | |||
|---|---|---|---|---|---|---|---|
| Aetiology | Localisation | Duration (y) | Initial rating (VAS 0–100) | ||||
| 1/M | 38 | Yes | Yes | Idiopathic | Bilateral | 20 | 80 |
| 2/F | 57 | Yes | Yes | Iatrogenic | Left | 8 | 60 |
| 3/M | 52 | Yes | Yes | Idiopathic | Right | 5 | 90 |
| 4/F | 52 | No | Yes | Idiopathic | Left | 2 | 35 |
| 5/F | 62 | No | Yes | Idiopathic | Bilateral | 1 | 80 |
| 6/M | 35 | Yes | Yes | Idiopathic | Left | 2 | 50 |
| 7/M | 59 | No | Yes | Idiopathic | Right | 5 | 100 |
| 8/M | 44 | No | Yes | Idiopathic | Bilateral | 15 | 70 |
| 9/M | 55 | Yes | No | Noise trauma | Bilateral | 3 | 35 |
| 10/M | 72 | Yes | Yes | Idiopathic | Right | 12 | 80 |
| 11/M | 60 | No | Yes | Idiopathic | Bilateral | 7 | 60 |
| 12/M | 53 | Yes | Yes | Idiopathic | Left | 6 | 40 |
| 13/M | 59 | Yes | Yes | Idiopathic | Bilateral | 25 | 80 |
| 14/M | 37 | No | No | Idiopathic | Bilateral | 1 | 75 |
VAS, Visual Analogue Scale.
Patients gave written informed consent prior to study entry, after approval of the protocol by the local ethics committee.
Study design and tinnitus rating
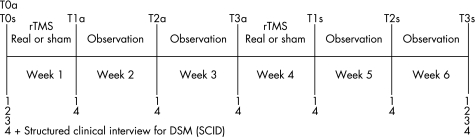
Figure 1 summarises the details of the study. After verifying the inclusion/exclusion criteria, and having obtained the average patient's tinnitus rating in the weeks preceding enrolment, patients were randomly assigned to receive, as the first intervention, active (T0a, 8 patients) or sham (T0s, 6 patients) rTMS. Each week of intervention was followed by 2 weeks of observation. Clinical variables were sampled immediately after the end of the active (T1a) or sham (T1s) rTMS, after 1 week (T2a and T2s, respectively) and after 2 weeks (T3a and T3s, respectively). The crossover was after the first 2 weeks of observation.
Figure 1 Design and timetable of the study (see text for details). 1 = 0–100 Visual Analogue Scale (VAS) for tinnitus rating; 2 = otoacoustic emissions (only for normoacoustic patients); 3 = tonal audiometry; 4 = psychiatric testing (Hamilton Anxiety and Depression Scale). rTMS, repetitive transcranial magnetic stimulation
Tinnitus was rated by a 0–100 Visual Analogue Scale (VAS), where 0 was wellness and 100 was the worst possible tinnitus related discomfort. Anxiety and depression were rated, respectively, by the 14 item Hamilton scale (HAM‐A, maximum score 56) and by the 21 item Hamilton scale (HAM‐D, maximum score 66). Audiometry and otoscopy were performed at enrolment and at the end of the study. Otoacoustic emissions were also evaluated in normoacoustic patients. Tinnitus, anxiety and depression ratings and acoustic evaluations were collected by experimenters blind to the type of rTMS applied.
TMS procedures and placebo condition
Subjects wore ear plugs. Active and sham rTMS was delivered through a focal coil (outer diameter of each wing 7 cm) connected with a standard Mag‐Stim Super Rapid stimulator (maximum output 2.2 Tesla). Individual resting excitability thresholds for left motor cortex stimulation were determined each day, according to International Guidelines,47 prior to the rTMS session, by using the same coil and stimulator; afterwards, the intensity was increased by 20% and the coil was moved towards the target region.
As neuroimaging studies described mainly left hypermetabolism irrespective of tinnitus laterality,13,48 the left temporoparietal region was targeted, in accordance with other studies.24,40 In eight patients, the coil was navigated to the secondary AC (Brodman Area 22, coordinates −44, −50, 20) by the Stereotaxic Navigator SofTax System (EMS Italy, www.emsmedical.net). Accuracy of TMS coil positioning with this system in different brain regions can be estimated in the order of <1 cm (for details, see Rossi and colleagues49,50,51). In the remaining eight patients, a stimulation site corresponding to the scalp projection of the secondary AC was identified by placing the anterior junction of the two coil wings halfway between T3 and C3/T5 (10‐20 international EEG system).16 In these patients, the estimated average mismatch between the coil position and the exact anatomical location of the secondary AC was 1.8±1 cm. The handle of the coil was angled backwards by about 45° away from the midline. This position was marked on a transparent bathing cuff firmly attached to the scalp, on which anatomical landmarks (nasion, inion, preauricolar points and vertex) were marked. This allowed the same repositioning of the coil on successive days.
Repetitive TMS consisted of 1200 stimulations/day (three trains of 400 stimuli with an inter‐train interval of 30 s) at 1 Hz and 120% of the motor threshold, for five consecutive days (from Monday to Friday, between 12 and 13pm). A high number of stimuli/day were applied because of the previously suggested dose dependency of tinnitus alleviation by rTMS.17,23 Furthermore, the use of such relatively high intensity assured the stimulation of most of the target region, even in the case of mismatch between the scalp position and the underlying anatomy, which can be expected using the International EEG system as anatomical reference for TMS stimulation.40,52
For sham stimulation, the coil was still centred on the same scalp position, but it was tilted to 90° so that scalp contact and discharging noise were similar, but the magnetic field did not reach cortical neurons at a biologically active level. In order to minimise subjective differences between active and sham stimulations, a concurrent low intensity electrical stimulation (square wave pulses of 0.2 ms and intensity of 5–15 mA) of the ipsilateral facial nerve trunk was applied through bipolar adhesive surface electrodes connected to the EMG machine which triggered the magnetic stimulator. Thus electrical stimuli were synchronous with either active or sham stimuli. This original placebo condition allowed mild activation of both ipsilateral facial muscles and trigeminal afferents, that would be otherwise perceived by patients only in case of active rTMS.
Data analysis
Clinical evaluations along the time course of the study were carried out by experimenters blind to the type of rTMS that had been applied.
Comparative analyses of VAS, HAM‐A and HAM‐D scores at different time points of the trial were carried out by the Wilcoxon matched pairs test as these data were not normally distributed. Comparisons took into account mean values of the three clinical scores obtained after the week of the active rTMS (T1a, T2a, T3a) or after the week of sham rTMS (T1s, T2s, T3s) versus mean basal values obtained in the week immediately preceding the active (T0a) or sham (T0s) intervention. Finally, the maximal VAS improvement was plotted against tinnitus duration, initial rating and patient age (Spearman's rho correlation). For each test, the level of significance was p = 0.05.
Results
The characteristics of the patients who completed the study (11 males; 3 females) are summarised in table 2. Only two were normoacoustic. Mean age was 52.5 (10.6) years (range 35–72). Tinnitus duration ranged from 1 to 25 years (mean 8 (7.4) years), it produced subjective considerable discomfort (mean basal VAS 66.8 (20.6), range 35–100) and was bilateral in 7, right‐sided in 3 and left‐sided in 4 patients. The origin of tinnitus was mainly idiopathic and associated with hypoacousia.
The majority of patients did not complain of side effects from rTMS, apart from a slight transient headache on the stimulation site which did not require pharmacological treatment. Approximately 30% of patients complained of tongue paraesthesia occurring during the active rTMS. Most of patients reported transient worsening of their tinnitus in the first 2–3 days of active rTMS. Two male patients, one receiving active rTMS and one sham rTMS as the first intervention, dropped out of the study for this reason. However, their tinnitus rating recovered to basal values within 2 days. Otoscopy and otological measurements (tonal audiometry in all patients and otoacoustic emissions in the normoacoustic patients) remained stable throughout the study, implicitly suggesting that rTMS was safe at the cochlear level.
Individual motor threshold of stimulation ranged between 48% and 60% of the maximal stimulator output (mean 54%). Therefore, the intensity used for rTMS interventions ranged from 58% to 72% of the maximal stimulator output.
After the trial was over, patients were asked about the order of the type of rTMS received: 10/14 (71.4%) failed to correctly identify the temporal sequence of the two TMS interventions (ie, they did not realise the difference between real rTMS and placebo stimulation).
Evaluation of clinical scores (VAS, HAM‐A, HAM‐D)
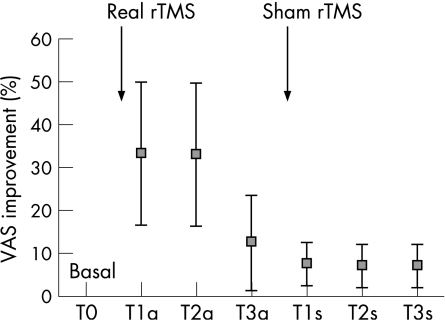
The analysis carried out at the three sampling times after the active rTMS, including the whole sample of patients (responders and non‐responders), showed a significant reduction in the mean VAS score at T1a (47.1 (24.6); p = 0.025) and T2a (51.8 (24.2); p = 0.032) versus T0a (66.8 (20.6)), while after 2 weeks (T3a) the difference was not significant (63.9 (23.1); p = 0.71), suggesting a transient improvement in perception of tinnitus.
The mean VAS score at T0s (66.6 (20.8)), which was the same as that at T0a, was not significantly modified by the sham rTMS at T1s (60 (25.9); p = 0.43), T2s (60.4 (26.2); p = 0.49) or T3s (60.4 (26.2); p = 0.49), suggesting no influence on perception of tinnitus. Direct comparisons between active and sham treatments showed significantly different VAS improvement at T1a versus T1s (p = 0.021), T2a versus T2s (p = 0.017), but not at T3a versus T3s (p = 0.60).
Descriptively, the VAS improvement in the whole sample of patients (responders and non‐responders) in the 2 weeks following the active rTMS was about 35% versus the basal score, while the sham rTMS produced no significant effect (fig 2). Six patients (42.8%) did not show any substantial modification of the VAS scores (less than 25% of the basal value) and therefore were arbitrarily classified as non‐responders. Of these, four patients had bilateral tinnitus, one had left‐sided tinnitus and one had right‐sided tinnitus. In four non‐responders, neuronavigation was used for coil positioning. The VAS improvement in responders (8 out of 14) increased to 60% of the basal score, but still returned close to basal values after 2 weeks.
Figure 2 Per cent changes in the Visual Analogue Scale (VAS) score in the 14 patients who completed the study (responders and non‐responders). As basal individual VAS values were variable (see table 1), individual basal values were normalised to 100% (independently by its absolute score) and variations at different sampling times expressed as a percentage. This was done for graphical representation only. Statistics (in the text) refer to raw values. rTMS, repetitive transcranial magnetic stimulation.
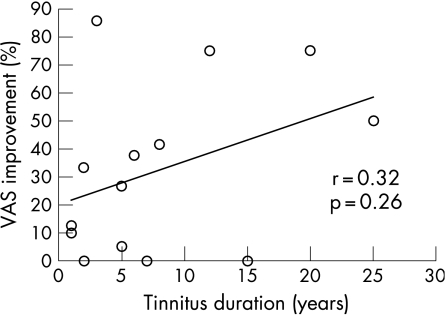
When tinnitus duration was plotted against the maximal improvement in VAS score following rTMS, no significant correlation emerged pooling responders and non‐responders (r = 0.32, p = 0.26) (fig 3) or selecting only responders (r = 0.56, p = 0.15). There was no correlation between VAS improvement with the age of the patient (r = 0.08, p = 0.76) or with initial VAS score (r = 0.14, p = 0.619).
Figure 3 Plot of tinnitus duration against the maximal improvement in Visual Analogue Scale (VAS) score after repetitive transcranial magnetic stimulation (rTMS). There was no significant correlation, suggesting that previous tinnitus duration did not influence the positive response to the rTMS treatment.
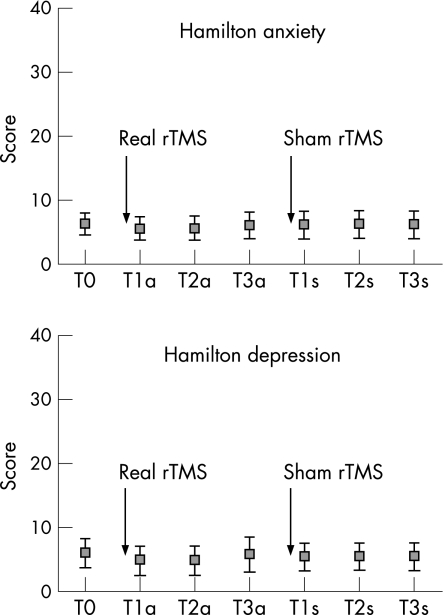
HAM‐A and HAM‐D scores were not influenced by active or sham rTMS (fig 4). In detail, the average score of HAM‐A at T0a (6.3 (3.5)) did not differ from those sampled at T1a (5.6 (3.7); p = 0.062), T2a (5.6 (3.8); p = 0.094) or T3a (6.1 (4.2); p = 0.687). Similarly, the average score of HAM‐A at T0s (6.42 (3.94)) did not differ from those sampled at T1s (6.2 (4.4); p = 0.937), T2s (6.2 (4.3); p = 0.843) or T3s (6.2 (4.4); p = 0.937).
Figure 4 Hamilton anxiety and depression mean scores in the 14 patients who completed the study (responders and non‐responders). There was no significant change throughout the study. Statistics are given in the text. rTMS, repetitive transcranial magnetic stimulation.
The average score of the HAM‐D at T0a (6.1 (4.6)) did not differ from those sampled at T1a (4.9 (4.6); p = 0.125), T2a (4.9 (4.6); p = 0.125) or T3a (5.8 (4.5); p = 0.5). Similarly, the average score of the HAM‐D at T0s (6.0 (5.1)) did not differ from those sampled at T1s (5.5 (4.4); p = 0.25), T2s (5.5 (4.3); p = 0.25) or T3s (5.5 (4.3); p = 0.25). Direct comparisons between active and sham treatments showed no significant differences between HAM‐A and HAM‐D at T1a versus T1s, T2a versus T2s or T3a versus T3s (always p>0.05).
Discussion
Our randomised, crossover, double blind, placebo controlled study confirms that daily application of high intensity 1 Hz rTMS to the left temporoparietal region is an efficient neuromodulatory strategy to transiently alleviate chronic tinnitus, independent of tinnitus lateralisation or bilaterality and of eventual concurrent changes in mood. Moreover, rTMS induced clinical improvement clearly emerged in the context of a placebo stimulation designed to more closely replicate the somatic sensation of active stimulation.
This represents a methodological key point and deserves further comment. Indeed, it should be taken into account that during TMS of the temporoparietal region, induced currents flow towards the skull base, leading to peripheral activation of the ipsilateral facial nerve and trigeminal afferents, especially when relatively high intensity stimulations are used. This provokes variable subjective discomfort and muscular activation of the face, which cannot be reproduced with conventional “sham” conditions, in which the coil is tilted at 90° or is held at a distance from the scalp so that no current reaches the brain at a useful degree. Neither commercially available sham coils, which produce the sound of stimulation in the absence of the magnetic field generation, are useful in this sense. Therefore, subjects can easily distinguish the difference between active and sham rTMS applications,53 especially during stimulation of the temporal region, thereby strongly biasing their judgments on eventual clinical benefits. This is extremely relevant in the case of patients with tinnitus, in which placebo effects can be particularly strong.3,44 Interestingly, even in patients with auditory hallucinations, which generally show improvement after rTMS,54 placebo effects may be particularly relevant.55 Moreover, it cannot be excluded a priori that repetitive activation of the muscles supplied by the facial nerve, occurring synchronously with real TMS pulses, could influence perception of tinnitus, considering that some patients can alleviate their tinnitus by simply moving their orofacial muscles.6,56 The use of low concurrent peripheral stimulation during both sham and active rTMS is an easy way to minimise this possible bias and to reduce behavioural differences between the two stimulation conditions: indeed, when asked at the end of the study, most subjects (71.4%), which were naïve for TMS procedures, did not realise the difference between the real and placebo rTMS.
In patients with chronic tinnitus, psychiatric comorbidity such as mood or anxiety disorders are relevant2 and may partly find their functional counterpart in the activation of higher order processing areas18,20,21 and of the limbic system.17 Therefore, careful psychiatric selection of patients seems mandatory, and it has been recently invoked for forthcoming clinical rTMS trials with the aim of excluding the fact that subjective improvement in tinnitus was not caused by concomitant alleviation of depression.43 Even in the absence of a concomitant overt psychiatric disorder, however, it seems important to monitor eventual changes in mood and anxiety throughout the rTMS study: indeed, subjective tinnitus rating might be affected by eventual subclinical changes of both mood and anxiety, which cannot be excluded a priori as rTMS affects brain regions outside the prefrontal cortex.57 Notably, rTMS can modify mood, even in healthy individuals.58 In the patients in the current study, ratings for subclinical depression and anxiety did not change (fig 4), thus suggesting that improvement in the perception of tinnitus was a specific rTMS effect.
At variance with previous studies,17,23 we did not find a negative correlation between previous tinnitus duration and positive clinical response to rTMS (fig 3), despite comparable symptom duration. This correlation did not emerge when either responders plus non‐responders or only responders were considered. Even patient age and initial tinnitus rating did not influence the rTMS response. It can be hypothesised that the degree of responsiveness to rTMS might be influenced by the amount of pre‐existing structural tinnitus related brain changes59: indeed, these may vary interindividually, are hardly predictable and have reasonably few chances of being modified by rTMS, although the possibility that rTMS might induce structural modifications at the level of the auditory cortex is emerging.60
Most likely, 1 Hz rTMS of temporoparietal regions might have restored a more physiological level of intracortical inhibition in the brain regions functionally relevant for tinnitus maintenance: indeed, intracortical inhibition is known to be reduced in chronic tinnitus because of afferent deprivation following receptor damage.9 This hypothesis stems from the notion that, at the level of the motor cortex, 1 Hz‐rTMS increases cortical inhibitory mechanisms (as tested via paired pulse TMS) in subjects with low baseline inhibition levels61 and may increase the length of the cortical silent period, another index of cortical inhibition.61,62,63 Notably, slow rTMS is thought to maximally induce proinhibitory effects in cortical areas of increased activity,64 such as those implicated in tinnitus processing, through a mechanism of depotentiation of pathologically potentiated synapses,30 in line with the concept of “homeostatic plasticity”.64 Also, the short lived time course of the effects (ie, no more than 2 weeks of the current study, in accordance with previous findings17,18) speaks in favour of rTMS induced functional, rather than structural,60 changes.
Because of the anatomical location of the primary AC (ie, buried deep within the Sylvian fissure for the most part), it is physically improbable that a direct TMS induced modulation occurred at this level.16 Taking into account that TMS preferentially activates interneurons located superficially in the cortex,65 it seems more plausible that neuronal populations of the more superficially located secondary AC were directly impacted by temporoparietal rTMS. However, trans‐synaptic spread to primary AC cannot be ruled out.
On first sight, possible limitations of the current study are the absence of a PET (or functional magnetic resonance) guided neuronavigation system for TMS coil placement and the choice of the dominant hemisphere for stimulation, irrespective of the side(s) of tinnitus perception. These factors, nonetheless, might even have negatively influenced the positive results (ie, the number of responders and degree of tinnitus alleviation), as in patients with bilateral tinnitus (50% in our cohort), left hyperactivation of AC is very likely,13,48 but cannot be considered the rule.17,18,59 Of note, the rate of responders in the current study (about 60%) was similar to previous studies in which rTMS was neuronavigated towards areas of hypermetabolism.17 This suggests that the use of extremely expensive and time consuming PET guided TMS systems may not be strictly necessary in clinical practice.
Some central questions about the relationships between rTMS in chronic tinnitus and metabolic brain activity associated with tinnitus remain open and warrant further larger studies for more definite answers: the former is whether rTMS is beneficial only when a local AC hyperactivation is taking place, and the latter is that it is still not known whether successful rTMS treatment for tinnitus is accompanied by normalisation of metabolic hyperactivation found in these patients, as recently reported in a single case of auditory hallucinations.66 Finally, even relationships between hemispheric dominance, tinnitus and metabolic hyperactivity of temporoparietal regions still need to be investigated by the rTMS approach.
Acknowledgements
We thank Dr Bruno De Capua, from the ORL Department, for recruitment of patients.
Abbreviations
AC - auditory cortex
HAM‐A - Hamilton Anxiety Scale
HAM‐D - Hamilton Depression Scale
PET - positron emission tomography
rTMS - repetitive transcranial magnetic stimulation
VAS - Visual Analogue Scale
Footnotes
Competing interests: None.
References
- 1.Heller A J. Classification and epidemiology of tinnitus. Otolaryngol Clin North Am 200336239–248. [DOI] [PubMed] [Google Scholar]
- 2.Dobie R. Depression and tinnitus. Otolaryngol Clin North Am 200336383–388. [DOI] [PubMed] [Google Scholar]
- 3.Dobie R. A review of randomized clinical trials in tinnitus. Laryngoscope 19991091202–1211. [DOI] [PubMed] [Google Scholar]
- 4.Lenarz T, Schreiner C, Snyder R L.et al Neural mechanisms of tinnitus. Eur Arch Otorhynolaringol 1993249441–446. [DOI] [PubMed] [Google Scholar]
- 5.Bauer C A, Brozoski T J, Holder T M.et al Effects of chronic salycilate on GABAergic activity in rat inferior colliculus. Hear Res 2000147175–182. [DOI] [PubMed] [Google Scholar]
- 6.Lockwood A H, Wack D S, Burkard R F.et al The functional anatomy of gaze‐evoked tinnitus and sustained lateral gaze. Neurology 200156472–480. [DOI] [PubMed] [Google Scholar]
- 7.Giraud A L, Chery C S, Fischer G.et al A selective imaging of tinnitus. Neuroreport 1999101–5. [DOI] [PubMed] [Google Scholar]
- 8.Mirz F, Pedersen B, Ishizu K.et al Positron emission tomography of cortical centers in tinnitus. Hear Res 1999134133–144. [DOI] [PubMed] [Google Scholar]
- 9.Eggermont J J, Roberts L E. The neuroscience of tinnitus. Trends Neurosci 200427676–682. [DOI] [PubMed] [Google Scholar]
- 10.Mühlnickel W, Elbert T, Taub E.et al Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci 19989510340–10343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson G, Lyttkens L, Hervela C.et al Regional cerebral blood flow during tinnitus: a PET case study with lidocaine and auditory stimulation. Acta Otolaryngol 2000120967–972. [DOI] [PubMed] [Google Scholar]
- 12.De Ridder D, De Mulder G, Walsh V.et al Magnetic and electrical stimulation of the auditory cortex for intractable tinnitus. Case report. J Neurosurg 2004100560–564. [DOI] [PubMed] [Google Scholar]
- 13.Kleinjung T, Eichhammer P, Langguth B.et al Long‐term effects of repetitive transcranial magnetic stimulation (rTMS) in patients with chronic tinnitus. Otolaryngol Head Neck Surg 2005132566–569. [DOI] [PubMed] [Google Scholar]
- 14.Mirz F, Gjedde A, Ishizu K.et al Cortical networks subserving the perception of tinnitus—a PET study. Acta Otolaryngol Suppl 2000543241–243. [DOI] [PubMed] [Google Scholar]
- 15.Reyes S A, Salvi R J, Burkard R F.et al Brain imaging of the effects of lidocaine on tinnitus. Hear Res 200217143–50. [DOI] [PubMed] [Google Scholar]
- 16.Plewnia C, Bartels M, Gerloff C. Transient suppression of tinnitus by transcranial magnetic stimulation. Ann Neurol 200353263–266. [DOI] [PubMed] [Google Scholar]
- 17.Plewnia C, Reimond M, Najib A.et al Dose‐dependent attenuation of auditory phantom perception (Tinnitus) by PET‐guided repetitive transcranial magnetic stimulation. Hum Brain Mapp 200728238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plewnia C, Reimold M, Najib A.et al Moderate therapeutic efficacy of PET‐navigated repetitive transcranial magnetic stimulation against chronic tinnitus: a randomized, controlled pilot study. J Neurol Neurosurg Psychiatry 200778152–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnsrude I S, Giraud A L, Frackowiak R S. Functional imaging of the auditory system: the use of positron emission tomography. Audiol Neurootol 20027251–276. [DOI] [PubMed] [Google Scholar]
- 20.Cacace A T. Expanding the biological basis of tinnitus: cross‐modal origins and the role of neuroplasticity. Hear Res 2003175112–132. [DOI] [PubMed] [Google Scholar]
- 21.Moller A R. Pathophysiology of tinnitus. Otolaryngol Clin North Am 200336249–266. [DOI] [PubMed] [Google Scholar]
- 22.Rossi S, Rossini P M. TMS in cognitive plasticity and the potential for rehabilitation. Trends Cogn Sci 20048273–279. [DOI] [PubMed] [Google Scholar]
- 23.De Ridder D, Verstrateten E, Van der Kelen K.et al Transcranial magnetic stimulation for tinnitus: influence of tinnitus duration on stimulation parameter choice and maximal tinnitus suppression. Otol Neurotol 200526616–619. [DOI] [PubMed] [Google Scholar]
- 24.Fregni F, Marcondes R, Boggio P S.et al Transient tinnitus suppression induced by repetitive transcranial magnetic stimulation and transcranial direct current stimulation. Eur J Neurol 200613966–1001. [DOI] [PubMed] [Google Scholar]
- 25.Lefaucheur J P, Drouot X, Menard‐Lefaucheur I.et al Neurogenic pain relief by repetitive transcranial magnetic cortical stimulation depends on the origin and the site of pain. J Neurol Neurosurg Psychiatry 200475612–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andre‐Obadia N, Peyron R, Mertens P.et al Transcranial magnetic stimulation for pain control. Double‐blind study of different frequencies against placebo, and correlation with motor cortex stimulation efficacy. Clin Neurophysiol 20061171536–1544. [DOI] [PubMed] [Google Scholar]
- 27.Moller A R. Similarities between severe tinnitus and chronic pain. J Am Acad Audiol 200011115–124. [PubMed] [Google Scholar]
- 28.Huang Y Z, Edwards M J, Rounis E.et al Theta burst stimulation of the human motor cortex. Neuron 200545201–206. [DOI] [PubMed] [Google Scholar]
- 29.Di Lazzaro V, Pilato F, Saturno E.et al Theta‐burst repetitive transcranial magnetic stimulation suppresses specific excitatory circuits in the human motor cortex. J Physiol56945–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoffman R E, Cavus I. Slow transcranial magnetic stimulation, long‐term depotentiation, and brain hyperexcitability disorders. Am J Psychiatry 20021591093–1102. [DOI] [PubMed] [Google Scholar]
- 31.Lefaucheur J P, Fenelon G, Menard‐Lefaucheur I.et al Low‐frequency repetitive TMS of premotor cortex can reduce painful axial spasms in generalized secondary dystonia: a pilot study of three patients. Neurophysiol Clin 200434141–145. [DOI] [PubMed] [Google Scholar]
- 32.Mantovani A, Lisanby S H, Pieraccini F.et al Repetitive transcranial magnetic stimulation (rTMS) in the treatment of obsessive–compulsive disorder (OCD) and Tourette's syndrome (TS). Int J Neuropsychopharmacol 2006995–100. [DOI] [PubMed] [Google Scholar]
- 33.Hoffman R E, Boutros N N, Hu S.et al Transcranial magnetic stimulation and auditory hallucinations in schizophrenia. Lancet 20003551073–1075. [DOI] [PubMed] [Google Scholar]
- 34.Hoffman R E, Hawkins K A, Gueorguieva R.et al Transcranial magnetic stimulation of the left temporoparietal cortex and medication‐resistant auditory hallucinations. Arch Gen Psychiatry 20036049–56. [DOI] [PubMed] [Google Scholar]
- 35.Poulet E, Brunelin J, Bediou B.et al Slow transcranial magnetic stimulation can rapidly reduce resistant auditory hallucinations in schizophrenia. Biol Psychiatry 200557188–191. [DOI] [PubMed] [Google Scholar]
- 36.Chibbaro G, Daniele M, Alagona G.et al Repetitive transcranial magnetic stimulation in schizophrenic patients reporting auditory hallucinations. Neurosci Lett 200538354–57. [DOI] [PubMed] [Google Scholar]
- 37.Jandl M, Steyer J, Weber M.et al Treating auditory hallucinations by transcranial magnetic stimulation: a randomized controlled cross‐over trial. Neuropsychobiology 20065363–69. [DOI] [PubMed] [Google Scholar]
- 38.Langguth B, Eichhammer P, Wiegand R.et al Neuronavigated rTMS in a patient with chronic tinnitus. Effects of 4 weeks treatment. Neuroreport 200314977–980. [DOI] [PubMed] [Google Scholar]
- 39.Eichhammer P, Langguth B, Marienhagen J.et al Neuronavigated repetitive transcranial magnetic stimulation in patients with tinnitus: a short case series. Biol Psychiatry 200354862–865. [DOI] [PubMed] [Google Scholar]
- 40.Langguth B, Zowe M, Landgrebe M.et al Transcranial magnetic stimulation for the treatment of tinnitus: a new coil positioning method and first results. Brain Topogr 200618241–247. [DOI] [PubMed] [Google Scholar]
- 41.Plewnia C, Kammer T, Gerloff C. Comment on neuronavigated repetitive transcranial magnetic stimulation in patients with tinnitus: a short case series. Biol Psychiatry 2004551117–1118. [DOI] [PubMed] [Google Scholar]
- 42.Eichhammer P, Langguth B, Hajak G. Reply. Biol Psychiatry 2004551117–1118.15158432 [Google Scholar]
- 43.Pridmore S, Kleinjung T, Langguth B.et al Transcranial magnetic stimulation: potential treatment for tinnitus? Psychiatry Clin Neurosci 200660133–138. [DOI] [PubMed] [Google Scholar]
- 44.Lockwood A H, Salvi R J, Burkard R F. Tinnitus. N Engl J Med 2002347904–910. [DOI] [PubMed] [Google Scholar]
- 45.Wasserman E M, Lisanby S H. Therapeutic application of repetitive transcranial magnetic stimulation: a review. Clin Neurophysiol 20011121367–1377. [DOI] [PubMed] [Google Scholar]
- 46.Miniussi C, Bonato C, Bignotti S.et al Repetitive Transcranial Magnetic Stimulation (rTMS) at high and low frequency: an efficacious therapy for major, drug‐resistant depression? Clin Neurophysiol 20051161062–1071. [DOI] [PubMed] [Google Scholar]
- 47.Rossini P M, Barker A T, Berardelli A.et al Non‐invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Electroenceph Clin Neurophysiol 19949179–92. [DOI] [PubMed] [Google Scholar]
- 48.Arnold W, Bartenstein P, Oestreicher E.et al Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus. A PET study with [18F]Deoxyglucose. ORL 199658195–199. [DOI] [PubMed] [Google Scholar]
- 49.Rossi S, Cappa S F, Babiloni C.et al Prefrontal cortex in long‐term memory: an “interference” approach using magnetic stimulation. Nat Neurosci 20014948–952. [DOI] [PubMed] [Google Scholar]
- 50.Rossi S, Miniussi C, Pasqualetti P.et al Age‐related functional changes of prefrontal cortex in long‐term memory. A repetitive transcranial magnetic stimulation (rTMS) study. J Neurosci 2004247939–7944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rossi S, Pasqueletti P, Zito G C.et al Prefrontal and parietal cortex in episodic memory. An interference study with rTMS. Eur J Neurosci 200623793–800. [DOI] [PubMed] [Google Scholar]
- 52.Herwig U, Satrapi P, Schonfeldt‐Lecuona C. Using the international 10‐20 EEG system for positioning of transcranial magnetic stimulation. Brain Topogr 20031695–99. [DOI] [PubMed] [Google Scholar]
- 53.Rossi S, Ferro M, Cincotta M.et al A real electro‐magnetic placebo (REMP) device for sham transcranial magnetic stimulation. Clin Neurophysiol 2007118709–716. [DOI] [PubMed] [Google Scholar]
- 54.Hoffman R E, Gueorguieva R, Hawkins K A.et al Temporoparietal transcranial magnetic stimulation for auditory hallucinations: safety, efficacy and moderators in a fifty patient sample. Biol Psychiatry 20055897–104. [DOI] [PubMed] [Google Scholar]
- 55.McIntosh A M, Semple D, Tasker K.et al Transcranial magnetic stimulation for auditory hallucinations in schizophrenia. Psychiatry Res 20041279–17. [DOI] [PubMed] [Google Scholar]
- 56.Lockwood A H, Salvi R J, Coad M L.et al The functional neuroanatomy of tinnitus: evidence for limbic system links and neural plasticity. Neurology 199850114–120. [DOI] [PubMed] [Google Scholar]
- 57.Schatter D, Van Honk J. A framework for targeting alternative brain regions with repetitive transcranial magnetic stimulation in the treatment of depression. J Psychiatry Neurosci 20053091–97. [PMC free article] [PubMed] [Google Scholar]
- 58.Pascual‐Leone A, Catala M D, Pascual‐Leone Pascual A. Lateralized effect of rapid‐rate transcranial magnetic stimulation of the prefrontal cortex on mood. Neurology 199646499–502. [DOI] [PubMed] [Google Scholar]
- 59.Muhlau M, Rauschecker J P, Oestreicher E.et al Structural brain changes in tinnitus. Cereb Cortex 2006161283–1288. [DOI] [PubMed] [Google Scholar]
- 60.May A, Hajak G, Ganssbauer S.et al Structural brain alterations following 5 days of intervention: dynamic aspects of neuroplasticity. Cereb Cortex 200717205–210. [DOI] [PubMed] [Google Scholar]
- 61.Daskalakis Z J, Moller B, Christensen B K.et al The effects repetitive transcranial magnetic stimulation on cortical inhibition in healthy human subjects. Exp Brain Res 2006174403–412. [DOI] [PubMed] [Google Scholar]
- 62.Romeo S, Gilio F, Pedace F.et al Changes in the cortical silent period after ripetitive transcranial magnetic stimulation of cortical motor areas. Exp Brain Res 2000135504–510. [DOI] [PubMed] [Google Scholar]
- 63.Cincotta M, Borgheresi A, Gambetti C.et al Suprathreshold 0. 3 Hz ripetitive TMS prolongs the cortical silent period: potential implications for therapeutic trials in epilepsy. Clin Neurophysiol 20031141827–1833. [DOI] [PubMed] [Google Scholar]
- 64.Siebner H R, Lang N, Rizzo V.et al Preconditioning of low‐frequency repetitive transcranial magnetic stimulation with transcranial direct current stimulation: evidence for homeostatic plasticity in the human motor cortex. J Neurosci 2004243379–3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Di Lazzaro V, Oliviero A, Pilato F.et al The physiological basis of transcranial motor cortex stimulation in conscious humans. Clin Neurophysiol 2004115255–266. [DOI] [PubMed] [Google Scholar]
- 66.Langguth B, Eichhammer P, Zowe M.et al Neuronavigated transcranial magnetic stimulation and auditory hallucinations in a schizophrenic patient: monitoring of neurobiological effects. Schizophr Res 2006b84185–186. [DOI] [PubMed] [Google Scholar]