Case history
A 33‐year‐old man was brought by ambulance to the emergency department from a local park with a right‐sided headache and amnesia. He did not know his name, age, address, occupation or marital status. He could not remember how he came to be in the park, nor could he recall any autobiographical event before that morning. Despite this alarming deficit, he responded to all questions directly, showing surprisingly little distress at his predicament. Cognitive testing showed that he was orientated to time and place, and able to perform well on tests of attention, concentration and recall. He was afebrile, and his physical examination was unremarkable. We observed no signs of head trauma or substance intoxication or withdrawal. His blood alcohol concentration was 0 and a urinary drug screen was unremarkable. A white cell count showed mild neutrophilia, but all other haematological and biochemical indices were normal. Cerebral computed tomography and lumbar puncture were normal. He started receiving empirical intravenous antibiotic and antiviral treatment and was admitted for observation.
The next morning, the patient's headache continued and he remained profoundly amnesic. However, he was able to write down a motorcycle license‐plate number which was used by police to identify him. Further history then available from family members and the patient's regular neurologist showed a 20‐year history of migraine with aura consisting of blurred vision and scintillation spectra, often followed by unilateral paraesthesias of one hand culminating in frontal headache contralateral to the hand.1 The patient had experienced numerous prior episodes of amnesia often involving travel within the city and on one occasion several hundred kilometres between cities. Each episode invariably occurred in the context of a migraine, with the fugue state occurring after the onset of headache but not preceding it. The patient had also experienced migraines with shorter periods of amnesia lasting minutes, in which he forgot what he was doing but did not result in travel. On presentation, there were no historical features to indicate a primary psychiatric disorder and nothing to suggest the patient might be malingering. There were no recent psychosocial stressors. Cerebral magnetic resonance imaging (MRI) performed 3 months earlier had shown foci of increased signal in the subcortical white matter, consistent with white matter hyperintensities described in previous imaging studies of migraineurs.2 We found no space occupying lesions or other structural abnormalities.
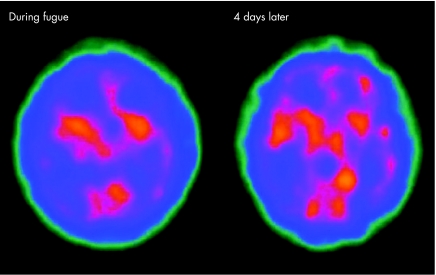
Migrainous fugue was diagnosed, and the patient was given 50 mg of sumatriptan. Within 3 h his headache improved, his autobiographical data returned, and he was suddenly able to give a comprehensive and lucid personal history confirming historical details already sourced from his family and doctors. The role of a single unblinded dose of sumatriptan in his recovery should be interpreted with caution, as the patient subsequently reported that he had tried numerous drugs for his migraines (including sumatriptan) without success. An electroencephalogram (EEG) performed 3 h after the return of the patient's memory was normal. A SPECT scan also performed at this time showed moderate hypoperfusion of the right temporal and parietal lobes and mild frontal hypoperfusion compared with a follow‐up scan at 4 days (fig 1).
Figure 1 A single‐photon emission computed tomography scan showing moderate hypoperfusion of the right temporal and parietal lobes during fugue with a follow‐up scan 4 days later.
Discussion
Fugue states are characterised by a complete loss of memory for all personal details and are often associated with travel from home. Although often witnessed on stage and screen, real‐life fugue states are rare. The classical psychogenic dissociative fugue is said to be an unconscious reaction to a traumatic event where the person “forgets” in an effort to cope with the anxiety the event evoked.3 However, a range of organic causes have been reported, including complex partial seizures, drugs and head trauma.3 Changes in cerebral perfusion during migraine have been described in the literature.4 We hypothesise that our patient's recurrent fugue states are causally related to migrainous hypoperfusion of the temporal and frontal lobes, and the limbic region, in keeping with the SPECT findings. Markowitsch et al investigated a case of autobiographical amnesia and found similar perfusion changes on positron emission tomography scanning.5 However, to the best of our knowledge, there have been no previous case reports of fugue in the context of migraine with aura, with changes in cerebral perfusion documented by SPECT scanning.
Acknowledgements
We thank Dr Andrew Duggins, Consultant Neurologist, University of Sydney and Westmead Hospital, Sydney, New South Wales, Australia.
Footnotes
Competing interests: None.
Informed consent was obtained for publication of the patient's details described in this report.
References
- 1.Headache Classification Committee of The International Headache Society The international classification of headache disorders (2nd edn). Cephalalgia 200424(Suppl 1)1–160. [DOI] [PubMed] [Google Scholar]
- 2.Porter A, Gladstone J P, Dodick D W. Migraine and white matter hyperintensities. Curr Pain Headache Rep 20059289–293. [DOI] [PubMed] [Google Scholar]
- 3.Coons P M. The dissociative disorders. Rarely considered and underdiagnosed. Psychiatr Clin North Am 199821637–648. [DOI] [PubMed] [Google Scholar]
- 4.Calandre E P, Bembibre J, Arnedo M L.et al Cognitive disturbances and regional cerebral blood flow abnormalities in migraine patients: their relationship with the clinical manifestations of the illness. Cephalalgia 200222291–302. [DOI] [PubMed] [Google Scholar]
- 5.Markowitsch H J, Calabrese P, Fink G R.et al Impaired episodic memory retrieval in a case of probable psychogenic amnesia. Psychiatry Res 199774119–126. [DOI] [PubMed] [Google Scholar]