Dysmetropsia is a disorder of visual perception characterised by an apparent modification of the size of perceived objects.1,2,3 Objects can appear larger (macropsia) or smaller (micropsia) than their actual size. Dysmetropsia can result from retinal oedema causing a dislocation of the receptor cells and from lesions affecting other parts of extracerebral visual pathways. Transient micropsia can also result from epileptic seizure, migraine, infectious mononucleosis, the action of mescaline and other hallucinogenic drugs, and psychopathological phenomena.
Permanent dysmetropsia following focal cerebral lesions is rare. Most of the prior reports described hemimicropsia due to lesions mainly involving the lateral aspect of the visual association cortex.1,2,3 However, reports of hemimacropsia following focal cerebral lesions have been extremely rare1,4 and hemimacropsia following a focal vascular lesion has not been described previously. We describe a patient with left hemimacropsia due to right medial temporo‐occipital infarction.
Case report
A 64‐year‐old right‐handed man with hypertension was admitted 4 days after a sudden onset of visual disturbance. He reported that objects in the left side of the visual fields appeared larger in size without distortion of the shape. On neurological examination, he was alert and fully oriented to time and space. His visual acuity was normal, but left homonymous upper quadrantanopsia was found on confrontation tests. He was able to recognise objects, and name colours and his family members. He was fluent and had no problems in comprehension, reading and writing. There was no evidence of visuospatial dysfunction in a cancellation task and line bisection test. He had no weakness or sensory deficit. Babinski sign was not elicited bilaterally. Humphrey perimetry showed left homonymous upper quadrantanopsia (fig 1A). To verify hemimacropsia, we performed size discrimination tasks. We instructed him to stare at the examiner's right eye with his right eye covered and then presented a circle of 1, 1.5 or 2 cm diameter in the nasal and temporal side of his left eye separately. After taking away the circle, we asked him to indicate a circle of the same size among circles of variable sizes ranging from 0.5 to 4 cm in diameter with binocular viewing. We repeated the same task with his left eye covered. He always selected a circle of larger size than the one presented when the circle appeared in the temporal field of the left eye and in the nasal field of the right eye. However, he was able to choose a circle of the same size when the circle was presented in the temporal field of the right eye or in the nasal field of the left eye.
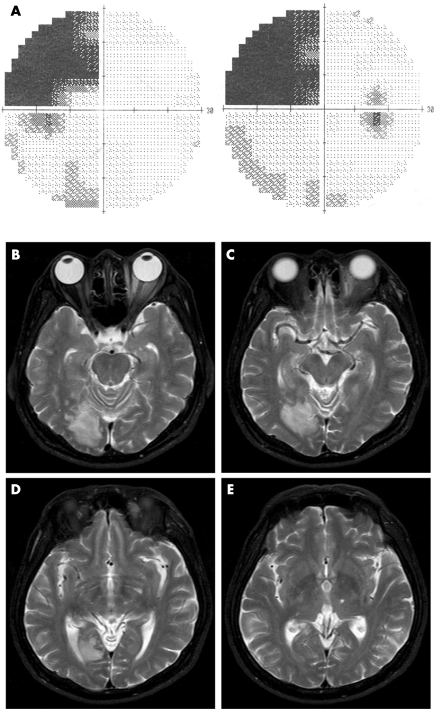
Figure 1 Humphrey perimetry shows left homonymous upper quadrantanopsia (A) and brain MRIs (B–E) show an infarction in right medial temporo‐occipital lobe (Brodmann areas 17, 18 and 19).
MRI disclosed an infarction in the right medial temporo‐occipital region, which corresponded to the medial aspect of Brodmann areas 17, 18 and 19 (fig 1B–E). The macropsia resolved completely 1 month after symptom onset, but left homonymous upper quadrantanopsia remained unchanged on follow‐up perimetry.
Comment
Although precise anatomical details on the cerebral lesions responsible for dysmetropsia remain uncertain, hemimicropsia has mostly been reported in lesions involving the lateral aspect of the visual association cortex (Brodmann areas 18 and 19).1,2,3
The striate cortex is the source of two multisynaptic corticocortical pathways.5 The occipitotemporal projection system is crucial for the visual identification of objects, whereas the occipitoparietal projection system is critical for the visual location of objects. Authors have argued that the prestriate areas are responsible for hemimicropsia, because the reported patients did not show any evidence of contralesional spatial neglect or a systematic bias in locating contralesional objects towards the ipsilesional side despite the lesions in the lateral aspect of the visual association cortex.1,2,3
On the other hand, the anatomical substrate and the pathophysiological mechanism of hemimacropsia have not been well described, and reports of hemimacropsia following focal cerebral lesions have been sparse.1,4 Previously, a patient experienced right hemimacropsia immediately after excision of a tumour involving the inferior portion of the left occipital lobe,1 and another experienced micropsia for objects presented in the left visual field due to a right occipital lesion from blunt head trauma, but the disorder reversed to macropsia under certain circumstances.4
Our patient showed left hemimacropsia and homonymous upper quadrantanopsia, without any other aspect of visual processing being affected. Brain MRI documented an infarction in the medial aspect of the right temporo‐occipital lobe. Our case suggests that, unlike hemimicropsia, hemimacropsia may be associated with a lesion in the ventral portion of the occipitotemporal projection, including the lingual and fusiform gyri, which play a decisive role in the visual identification of objects by interconnecting the striate, prestriate and inferior temporal areas. Patients with hemimacropsia may have an anatomical localisation of the lesions in the medial aspect of the temporo‐occipital lobe, whereas hemimicropsia usually results from lesions in the lateral aspect.
Footnotes
Competing interests: None declared.
References
- 1.Frassinetti F, Nichelli P, di Pellegrino G. Selective horizontal dysmetropsia following prestriate lesion. Brain 1999122339–350. [DOI] [PubMed] [Google Scholar]
- 2.Ebata S, Ogawa M, Tanaka Y.et al Apparent reduction in the size of one side of the face associated with a small retrosplenial haemorrhage. J Neurol Neurosurg Psychiatry 19915468–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen L, Gray F, Meyrignac C.et al Selective deficit of visual size perception: two cases of hemimicropsia. J Neurol Neurosurg Psychiatry 19945773–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bender M B, Teuber H L. Spatial organization of visual perception following injury to the brain. Arch Neurol Psychiatry 19485939–62. [DOI] [PubMed] [Google Scholar]
- 5.Rizzo M, Nawrot M, Blake R.et al A human visual disorder resembling area V4 dysfunction in the monkey. Neurology 1992421175–1180. [DOI] [PubMed] [Google Scholar]