Abstract
The mitogen-activated protein kinase (MAPK) pathway is frequently activated in human cancers, leading to malignant phenotypes such as autonomous cellular proliferation. Here, we demonstrate a novel role of the activated MAPK pathway in immune evasion by melanoma cells with the mutation of BRAF, which encodes a MAPKKs, (BRAFV600E). MEK inhibitor U0126 or RNA interference (RNAi) for BRAFV600E decreased production of the immunosuppressive soluble factors interleukin (IL)-10, VEGF, or IL-6 from melanoma cells to levels comparable to those after signal transducer and activator of transcription (STAT)3 inactivation. The suppressive activity of the culture supernatants from the melanoma cells on the production of inflammatory cytokines IL-12 and tumor necrosis factor α by dendritic cells upon lipopolysaccharide stimulation was markedly reduced after transduction with BRAFV600E RNAi, comparable to the effects observed with STAT3 RNAi transduction. No additive or synergistic effects were observed by the simultaneous transduction of RNAi for both BRAFV600E and STAT3. Furthermore, specific DNA binding and transcriptional activity of STAT3 were not affected by down-regulation of the MAPK signaling with the BRAF RNAi. These results indicate that the MAPK signal, along with the STAT3 signal, is essential for immune evasion by human melanomas that have constitutively active MAPK signaling and is a potential molecular target for overcoming melanoma cell evasion of the immune system.
Immune responses to human melanoma have been extensively studied, and various immunotherapies have been developed (1–4). One of the major problems contributing to immunological rejection of cancer is immune evasion through various mechanisms (5). Immune evasion is one of the malignant phenotypes that allows cancer cells to survive in the host. It is important to understand the molecular mechanisms of immune evasion to allow the development of cancer immunotherapy. Most cancer cells produce several immune suppressive factors that allow them to evade the host immune system (6, 7). The mechanisms for the production of these effector molecules in cancer cells have not been investigated well, although oncogenic STAT3 signaling has recently been reported to result in immune evasion through production of immune suppressive factors in various murine cancers (8, 9). In this study, we have evaluated the role of mitogen-activated protein kinase (MAPK) signaling in the production of various immune-suppressive cytokines. MAPK activation occurs frequently in human cancers due to various genetic changes, and MAPK signaling is also important in the regulation of cytokine signal pathways. Using a MAPK inhibitor and lentiviral BRAFV600E RNA interference (RNAi), we demonstrated that the MAPK pathway, along with STAT3 pathway signaling, is essential for production of immunosuppressive factors by human melanoma cells that have constitutively activated MAPK signaling due to the BRAFV600E mutation, which is detected in 66% of melanomas (10).
RESULTS AND DISCUSSION
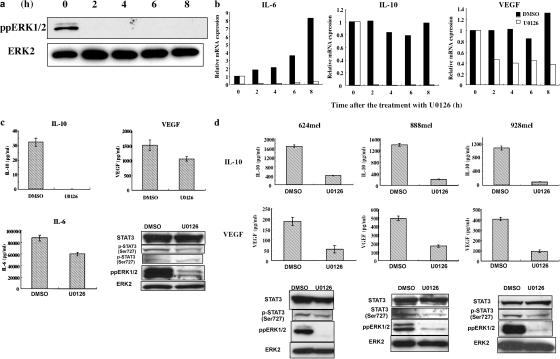
An A375 melanoma cell line with a constitutively activated MAPK due to a BRAFV600E mutation was treated with MEK inhibitor U0126 at a concentration of 25 μM for 8 h, resulting in the suppression of the ERK phosphorylation (Fig. 1 a). Immune-suppressive soluble factor mRNAs, including IL-6, IL-10, and VEGF, significantly decreased with the U0126 treatment (Fig. 1 b), whereas the control DMSO treatment did not affect the production of IL-10 and VEGF mRNAs, and only slightly increased the level of IL-6 mRNA. An 18-h exposure to U0126 also suppressed the production of IL-10, VEGF, and IL-6 at the protein level, indicating that activated ERKs may be responsible for suppressing local immune responses against melanoma by producing these immunosuppressive factors (Fig. 1 c). In addition, the suppression of ERK phosphorylation and the inhibition of IL-6, IL-10, and VEGF production occurred even after reducing the concentration of the U0126 treatment to 10 μM (not depicted). During this study, no significant cytotoxic effects were observed with the U0126 treatment of the A375 cells. Although U0126 is known to inhibit MEK5 in addition to MEK1/2, phosphorylated ERK5, the MEK5 substrate, was not detected in the A375 cells (not depicted), indicating that the MEK1/2–ERK1/2 pathway is responsible for the effects observed with U0126 treatment. The suppressive effects of U0126 on IL-10 and VEGF production were also demonstrated in three other melanoma cell lines with the BRAFV600E mutation, 624mel, 888mel, and 928mel, without any significant cellular toxicity (Fig. 1 d). Because these melanoma cell lines do not produce IL-6, activated MAPK signaling appears to have a general role in the production of immunosuppressive factors IL-10 and VEGF in BRAFV600E+ melanoma cell lines.
Figure 1.
Decreased production of immunosuppressive soluble factors IL-6, IL-10, and VEGF from melanoma cell lines with constitutively active MAPK through the BRAFV600E mutation by inhibition of the MAPK signaling with a MEK inhibitor, U0126. (a) Inhibition of phosphorylation of ERK1/2 was detected by Western blot analysis of the A375mel melanoma cell line with the BRAFV600E mutation before and 2, 4, 6, and 8 h after treatment with MEK inhibitor U0126 at a concentration of 25 μM. (b) Inhibition of mRNA expression for immunosuppressive soluble factors IL-6, IL-10, and VEGF in A375 cells. The mRNAs for various soluble factors, including IL-6, IL-10, and VEGF, were measured by quantitative RT-PCR before and 2, 4, 6, and 8 h after the treatment with U0126. The control treatment was performed with a DMSO solution. The mRNA levels at each time point were normalized to GAPDH mRNA and indicated as the relative value to that of 0 h. (c) Decreased production of IL-6, IL-10, and VEGF proteins from A375 cells after an 18-h treatment with U0126 at a concentration of 25 μM. The expression was detected by ELISA with the culture supernatants. The ratio of viability of U0126-treated cells DMSO-treated cells at the harvest was 77%. The cytokine production was normalized to the value of control DMSO-treated cells based on the cell count. Western blot showed strong inhibition of ERK phosphorylation, but not of STAT3 protein, or its phosphorylation at Ser727 and Tyr705. (d) Decreased production of IL-10 and VEGF from three melanoma cell lines with the BRAFV600E mutation, 624mel, 888mel, and 928mel after an 18-h treatment with U0126 at a concentration of 25 μM, which was detected by ELISA with the culture supernatants. The ratios of viability of U0126-treated cells DMSO-treated cells at the harvest were 95% for 624mel, 103% for 888mel, and 100% for 928mel. The cytokine production was normalized to the value of control DMSO-treated cells based on the cell count. Western blot showed strong inhibition of ERK phosphorylation, but not of STAT3 protein. Slight decrease of Ser727 phosphorylation of STAT3 was observed in 888mel and 928mel cells, but not in 624mel cells. These results are representative of three or four independent experiments with similar results.
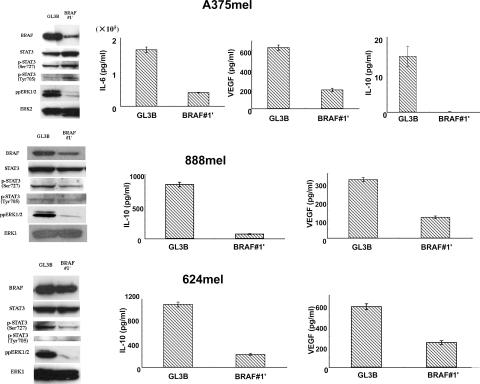
However, nonspecific effects of U0126 on the cytokine production via pathways other than the MAPK signaling cannot be completely ruled out from these experiments because of the observed slight decrease in STAT3 phosphorylation at Ser727 in 888mel and 928mel (Fig. 1 d). To confirm the role of the activated MAPK due to the BRAFV600E mutation in the production of IL-10, VEGF, and IL-6, BRAFV600E-specific RNAi was transfected into three melanoma cell lines, A375, 888mel, and 624mel, using the lentivirus expressing BRAFV600E-specific short hairpin RNA (shRNA) (11). The BRAFV600E-specific RNAi significantly inhibited IL-10, VEGF, and IL-6 production as well as suppressed ERK phosphorylation (Fig. 2). These results confirm that the inhibition of these factors by U0126 (Fig. 1) is correlated with the specific inhibition of the MAPK pathway. These results are consistent with recent papers showing ERK1/2-induced IL-10 production in murine macrophages (12) and BRAFV600E-dependent VEGF production for promotion of angiogenesis (13).
Figure 2.
Decreased production of immunosuppressive factors IL-6, IL-10, and VEGF from three melanoma cell lines with the BRAFV600E mutation by BRAFV600E-specific RNAi. The three melanoma cell lines with the BRAFV600E mutation, A375mel, 888mel, and 624mel, were infected with the lentivirus vectors encoding short hairpin RNA for either firefly luciferase mRNA (GL3B; as control) or BRAFV600E mRNA (BRAF#1′) at 50 or 100 multiplicity of infection. At 5 or 6 d after the infection, proteins were extracted and subjected to Western blot analysis. Profound decrease of phosphorylation of ERK1/2 with decrease of the BRAF protein was observed by the BRAFV600E-specific RNAi. No significant difference in STAT3 protein and phosphorylation of STAT3 at Ser727 or Tyr705 was observed. A slight decrease of phosphorylation at Ser727 was observed in 888mel and 624mel cells after BRAF RNAi. 5 or 6 d after the lentivirus infection, the equal number of the melanoma cells was dispensed at a density of 1–2 × 106 cells/2 ml, and the culture supernatants after 18 h were subjected to ELISA for IL-6, IL-10, or VEGF. Profound decrease of IL-6, IL-10, and VEGF was observed. One representative result of two or three independent experiments with similar results is shown.
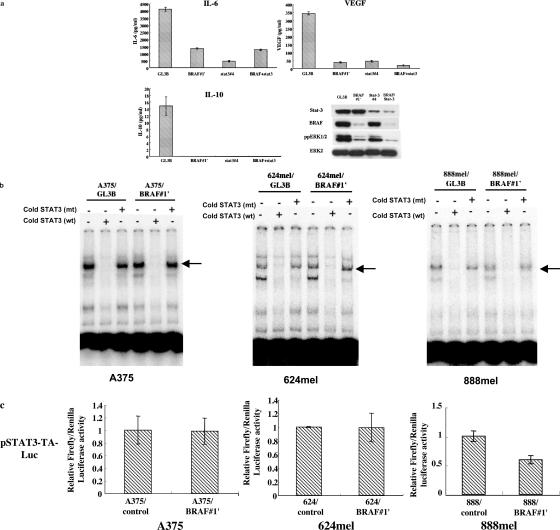
Because activated STAT3 signaling has been determined to result in immune evasion from cancer through the production of various factors including VEGF (8, 9), we investigated the relationship between the MAPK and the STAT3 pathways concerning the production of immunosuppressive factors in the A375 melanoma cell line. The production of IL-6, IL-10, and VEGF was profoundly inhibited by RNAi targeting either BRAFV600E alone or STAT3 alone (Fig. 3 a). No clear additive or synergistic effect was observed by simultaneously restricting the BRAF–MAPK and STAT3 pathways (Fig. 3 a). BRAFV600E RNAi in the A375 cells did not decrease the STAT3 DNA-binding activity (Fig. 3 b), the STAT3 promoter activity (Fig. 3 c), or STAT3 phosphorylation at either Ser727 or Tyr705 (Fig. 2), although ERKs were reported to be potentially able to phosphorylate STAT3 at Ser727 (14). However, STAT3 phosphorylation can also occur by an ERK-independent pathway (15). In 624mel cells, although there was a slight decrease of Ser727-phosphorylated STAT3, DNA-binding activity (Fig. 3 b) and STAT3 promoter activity (Fig. 3 c) were not affected by the BRAFV600E RNAi (Fig. 2). In 888mel cells, there was a similar decrease of Ser727 phosphorylation, but, conversely, both STAT3 DNA-binding activity (Fig. 3 b) and STAT3 promoter activity (Fig. 3 c) decreased after the BRAFV600E RNAi (Fig. 2). These results suggest that the reduction in the STAT3 transcription activity is not the main mechanism generating the immunosuppressive factor suppression by the down-regulation of the MAPK signaling in these melanoma cell lines.
Figure 3.
Inhibition of IL-6, IL-10, and VEGF production in A375 cells through the RNAi for BRAFV600E alone, STAT3 alone, or both, without significant changes in the DNA-binding and promoter activity of STAT3. (a) Profound inhibition of IL-6, IL-10, and VEGF production in A375 through the RNAi for BRAFV600E alone, STAT3 alone, or both. 5 or 6 d after the infection, the equal number of the cells was dispensed at a density of 106 cells/2 ml, and the culture supernatant after 18 h was subjected to ELISA for IL-6, VEGF, and IL-10. Decrease of BRAF and phosphorylated ERK1/2 by the BRAFV600E-specific RNAi and decrease of STAT3 by the STAT3-specific RNAi were confirmed by Western blot analysis. One representative result of six independent experiments with similar results is shown. (b) No significant change of the STAT3 DNA-binding activity by the inhibition of MAPK signaling with BRAF RNAi in melanoma cell lines. STAT3 DNA-binding activity was examined by EMSA of the nuclear extracts from melanoma cell lines with either control GL3B or BRAF#1′ shRNA vector treatment. Specific STAT3 bands indicated by arrows disappeared with cold wild-type STAT3 DNA probe (wt), but not with mutant STAT3 DNA probe (mt). Only a slight decrease of STAT3 DNA-binding activity was observed in 888mel cells. (c) STAT3 reporter assays in A375, 624mel, and 888mel cells. 2–4 × 105 cells with either control or BRAF#1′ shRNA vector infection were transfected with 0.4 μg pSTAT3-TA-Luc and 0.4 μg pRL-SV40 with Effectene Transfection Reagent. 24 h after the transfection, the cells were harvested and analyzed for firefly and renilla luciferase activity. Each firefly luciferase activity was normalized with the renilla luciferase activity. Shaded bars and error bars indicate the mean and standard deviation of the triplicate assays, respectively. One representative experiment of three or four independent experiments is shown. STAT3-driven transcription was not changed after the BRAF RNAi in A375 and 624mel, but it slightly decreased in 888mel.
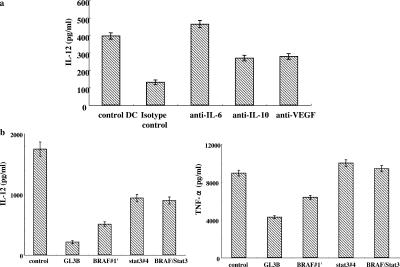
Next, the potential effects caused by the soluble factors induced by the MAPK and STAT3 signaling in the supernatant of the A375 cultures upon the maturation of DCs were investigated. The supernatant from the cultured A375 melanoma cells contains soluble factors that inhibit human monocyte-derived DC (MoDC) maturation when stimulated with Toll-like receptor ligands such as LPS. The addition of the A375 culture supernatants to MoDC cultures at a final concentration of 10–20% significantly decreased the production of inflammatory cytokines, including IL-12 and TNF-α, in MoDCs as well as CD1a and CD83 cellular surface molecules, but not CD80, CD86, CD40, or HLA-DR on MoDCs. Supernatants from the other three melanoma cell lines produced the same results when added to the MoDC cultures (not depicted). The suppressive activity of the melanoma cell supernatants stems from the production of IL-6, IL-10, and VEGF because the addition of specific antibodies for these factors reduced the suppressive activity of the A375 culture supernatants (Fig. 4 a). Disparities between our observations and the previously reported results concerning murine B16 melanoma cell supernatant with an activated STAT3 inhibiting the expression of MHC class II and CD40 may be explained by different tumor cells or species (8).
Figure 4.
Decreased suppressive activity of the A375 melanoma culture supernatants by pretreatment with RNAi for BRAFV600E alone, STAT3 alone, or both on LPS-induced IL-12 and TNF-α production from DCs. (a) Neutralization of IL-6, IL-10, or VEGF in the culture supernatants of A375 melanoma cells restored the inhibition of IL-12 production from LPS-stimulated human DCs. Human MoDCs were cultured with the A375 supernatants in the presence or absence of the monoclonal antibody for IL-6, IL-10, VEGF, or an isotype control antibody at 1 μg/ml. IL-12 production in the culture supernatants was determined by ELISA 24 h after the LPS stimulation at 100 ng/ml. (b) CD14+ monocytes were isolated from PBMCs by using MACS and cultured in the media containing RPMI 1640, 10% (vol/vol) FBS, 100 ng/ml GM-CSF, and 50 ng/ml IL-4 with or without 20% (vol/vol) of the culture supernatant of the A375mel cells prepared in Fig. 3. (a) Half of the media, cytokines, and the culture supernatant was changed every 2 d. On day 5 of the culture, LPS was added at 100 ng/ml. After 15 h, the culture supernatants were collected and subjected to ELISA of IL-12 and TNF-α.
The suppressive activity of the A375 culture supernatants on the IL-12 and TNF-α production of the LPS-treated MoDCs was restored by pretreating the A375 cells with either RNAi targeting BRAFV600E alone, STAT3 alone, or both BRAFV600E and STAT3 (Fig. 4 b). Although the STAT3 RNAi appeared to reduce the suppressive activity of the A375 culture supernatants more than the BRAFV600E RNAi, the difference may be simply caused by different RNAi activities. However, it is important to note that no additive and synergistic effects by the RNAi simultaneous-targeting BRAF and STAT3 were observed; again, indicating the essential roles of both signaling pathways in the production of suppressive factors on DC maturation. Although activation of DCs by the supernatant from murine CT26 colon cancer cell line transfected with a dominant-negative form of STAT3 possibly through the increased production of proinflammatory cytokines had been reported, activation of DCs was not observed in this study. It may be explained by an incomplete inhibition of BRAF and STAT3, no augmented proinflammatory cytokine production in the BRAF shRNA-transfected melanoma cells, or by differences in tumor cells or species.
In summary, we have demonstrated for the first time an essential role of the MAPK signaling along with the STAT3 pathway on the production of various immunosuppressive factors in melanoma cell lines with constitutively active MAPK due to the common BRAFV600E mutation. Thus, the MAPK pathway may be a potentially significant molecular target for overcoming immune evasion of various cancers because it is frequently activated in several types of cancers, including melanoma without BRAFV600E mutation (16, 17).
MATERIALS AND METHODS
Cell lines and reagents.
A375, 624mel, 888mel, and 928mel were cultured in RPMI 1640 media supplemented with 10% FBS, penicillin, and streptomycin. Stock solution of MEK inhibitor U0126 (Sigma-Aldrich) was made by dissolving the U0126 in DMSO.
Quantitative RT-PCR.
RT-PCR was performed by using TaqMan PCR assay probe/primers (Assay-on-Demand, Gene Expression Products; Applied Biosystems) for IL-6, IL-10, VEGF, and GAPDH by using ABI PRISM 7900HT (Applied Biosystems), and a relative quantitative method was applied for the target mRNA, which was normalized by the control GAPDH mRNA.
ELISA.
Human VEGF, IL-6, IL-12, and TNF-α were measured by using the DuoSet ELISA Development System (R&D Systems), and human IL-10 was measured by using the BD OptiEIA kit (BD Biosciences).
Lentivirus-mediated RNAi.
HIV lentiviral vectors for shRNA expression were prepared as described previously (11). The shRNA target sequences were as follows: for mutated BRAF (V600E), (BRAF#1′) GCTACAGAGAAATCTCGAT; for STAT3, (STAT3#4) ATAGGAAGGTTTAAGGAGA; and for firefly luciferase (control shRNA, GL3B) GTGCGCTGCTGGTGCCAAC. The construction of an HIV-U6-BRAF/STAT3-GFP vector with the tandem arranged two shRNA units was similar with the previous report (18).
5–6 d after the transduction, the melanoma cells were analyzed for the cytokine production and signaling molecules by ELISA and Western blot analysis, and the equivalent transduction was confirmed by the GFP expression from the vector (11) by flow cytometry analysis.
EMSA.
5 μg of nuclear extracts was mixed with 5× binding buffer, poly d (I-C), and [γ32P] ATP-labeled STAT3 double-stranded oligonucleotide probe with or without either unlabeled wild (5′-GATCCTTCTGGGAATTCCTAGATC-3′) or mutant (5′-GATCCTTCTGGGCCGTCCTAGATC-3′) STAT3 double-stranded oligonucleotide probe. The mixed samples were then subjected to electrophoresis in a 6.0% polyacrylamide gel. The radioactivity on the gel was developed by using a BAS imaging system (FUJI).
Western blot.
Anti-BRAF (Santa Cruz Biotechnology, Inc.), anti-ERK2 (Santa Cruz Biotechnology, Inc.), anti-ppERK1/2 (Cell Signaling), anti-STAT3 (Cell Signaling), anti–phospho-STAT3 (Ser727; Cell Signaling), and anti–phospho-STAT3 (Tyr705; Cell Signaling) antibodies were used for the first antibody. A horseradish peroxidase–conjugated anti-IgG antibody was used for the second antibody.
STAT3 reporter assay.
0.4 μg pSTAT3-TA-Luc (CLONTECH Laboratories, Inc.) with 0.4 μg pRL-SV40 were cotransfected to 2–4 × 105 melanoma cells with or without BRAF RNAi. 24 h after the transfection, the cells were analyzed for the firefly and renilla luciferase activity. Each firefly luciferase activity was normalized to renilla luciferase activity.
DC induction.
Human CD14+ monocytes isolated by using CD14 MicroBeads (Miltenyi Biotec) were cultured in RPMI 1640 medium supplemented with 10% FBS, 100 ng/ml GM-CSF, and 50 ng/ml IL-4 with or without the conditioned medium of the A375mel cells transduced with HIV lentiviral vectors. On day 5 of the culture, LPS was added at 100 ng/ml for the maturation of DCs, and on day 6, the culture supernatant was collected and analyzed for ELISA.
Acknowledgments
We thank Dr. M. Miyagishi and Dr. K. Taira, Department of Chemistry and Biotechnology, School of Engineering, The University of Tokyo, Tokyo, Japan for helping us generate shRNA lentiviruses. We thank Dr. N. Tsukamoto for technical advice. We thank Dr. H. Miyoshi (RIKEN Tsukuba Institute, Japan) for providing us with pCMV-VSV-G-RSV-Rev and pCAG-HIVgp for the HIV vector. We also thank Misako Horikawa, Ryoko Suzuki, and Starlyn Okada for preparation of the manuscript.
This work was supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (nos. 16591119, 15591193, 12217132, 14104013, and 17016070), a grant-in-aid for Cancer Research from the Ministry of Health, Labor and Welfare, Japan (15-17 and 15-10) for Second Term Comprehensive 10-year Strategy for Cancer Control, and the Keio Gijuku Academic Development Funds.
The authors have no conflicting financial interests.
References
- 1.Kawakami, Y., T. Fujita, Y. Matsuzaki, T. Sakurai, M. Tsukamoto, M. Toda, and H. Sumimoto. 2004. Identification of human tumor antigens and its implications for diagnosis and treatment of cancer. Cancer Sci. 95:784–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawakami, Y., S. Eliyahu, C.H. Delgado, P.F. Robbins, L. Rivoltini, S.L. Topalian, T. Miki, and S.A. Rosenberg. 1994. Cloning of the gene coding for a shared human melanoma antigen recognized by autologous T cells infiltrating into tumor. Proc. Natl. Acad. Sci. USA. 91:3515–3519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kawakami, Y., S. Eliyahu, C.H. Delgado, P. Robbins, K. Sakaguchi, E. Appella, J. Yannelli, G.J. Adema, T. Miki, and S.A. Rosenberg. 1994. Identification of a human melanoma antigen recognized by tumor infiltrating lymphocytes associated with in vivo tumor rejection. Proc. Natl. Acad. Sci. USA. 91:6458–6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenberg, S.A., J.C. Yang, D.J. Schwartzentruber, P. Hwu, F.M. Marincola, S.L. Topalian, N.P. Restifo, M.E. Dudley, S.L. Schwarz, P.J. Spiess, et al. 1998. Immunologic and therapeutic evaluation of a synthetic peptide vaccine for the treatment of patients with metastatic melanoma. Nat. Med. 4:321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marincola, F.M., E.M. Jaffee, D.J. Hicklin, and S. Ferrone. 2000. Escape of human solid tumors from T-cell recognition: molecular mechanisms and functional significance. Adv. Immunol. 74:181–273. [DOI] [PubMed] [Google Scholar]
- 6.Gabrilovich, D. 2004. Mechanisms and functional significance of tumor-induced dendritic-cell defects. Nat. Rev. Immunol. 4:941–952. [DOI] [PubMed] [Google Scholar]
- 7.Zou, W. 2005. Immunosuppressive networks in the tumor environment and their therapeutic relevance. Nat. Rev. Cancer. 5:263–274. [DOI] [PubMed] [Google Scholar]
- 8.Wang, T., G. Niu, M. Kortylewski, L. Burdelya, K. Shain, S. Zhang, R. Bhattacharya, D. Garbilovich, R. Heller, D. Coppola, et al. 2004. Regulation of the innate and adaptive immune responses by Stat-3 signaling in tumor cells. Nat. Med. 10:48–54. [DOI] [PubMed] [Google Scholar]
- 9.Nefedova, Y., M. Huang, S. Kusmartsev, R. Bhattacharya, P. Cheng, R. Salup, R. Jove, and D. Gabrilovich. 2004. Hyperactivation of STAT3 is involved in abnormal differentiation of dendritic cells in cancer. J. Immunol. 172:464–474. [DOI] [PubMed] [Google Scholar]
- 10.Davies, H., G.R. Bignell, C. Cox, P. Stephens, S. Edkins, S. Clegg, J. Teague, H. Woffendin, M.J. Garnett, W. Bottomley, et al. 2002. Mutations of the BRAF gene in human cancer. Nature. 417:949–954. [DOI] [PubMed] [Google Scholar]
- 11.Sumimoto, H., M. Miyagishi, H. Miyoshi, S. Yamagata, A. Shimizu, K. Taira, and Y. Kawakami. 2004. Inhibition of growth and invasive ability of melanoma by inactivation of mutated BRAF with lentivirus-mediated RNA interference. Oncogene. 23:6031–6039. [DOI] [PubMed] [Google Scholar]
- 12.Mathur, R.K., A. Awasthi, P. Wadhone, B. Ramanamurthy, and B. Saha. 2004. Reciprocal CD40 signals through p38MAPK and ERK-1/2 induce counteracting immune responses. Nat. Med. 10:540–544. [DOI] [PubMed] [Google Scholar]
- 13.Sharma, A., N.R. Trivedi, M.A. Zimmerman, D.A. Tuveson, C.D. Smith, and G.P. Robertson. 2005. Mutant V599E B-Raf regulates growth and vascular development of malignant melanoma tumors. Cancer Res. 65:2412–2421. [DOI] [PubMed] [Google Scholar]
- 14.Wen, Z., Z. Zhong, and J.E. Darnell Jr. 1995. Maximal activation of transcription by stat1 and stat3 requires both tyrosine and serine phosphorylation. Cell. 82:241–250. [DOI] [PubMed] [Google Scholar]
- 15.Chung, J., E. Uchida, T.C. Grammer, and J. Blenis. 1997. STAT3 serine phosphorylation by ERK-dependent and -independent pathways negatively modulates its tyrosine phosphorylation. Mol. Cell. Biol. 17:6508–6516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanami, H., I. Imoto, A. Hirasawa, Y. Yuki, I. Sonoda, J. Inoue, K. Yasui, A. Misawa-Furihata, Y. Kawakami, and J. Inazawa. 2004. Involvement of overexpressed wild-type BRAF in the growth of malignant melanoma cell lines. Oncogene. 23:8796–8804. [DOI] [PubMed] [Google Scholar]
- 17.Satyamoorthy, K., G. Li, M.R. Gerrero, M.S. Brose, P. Volpe, B.L. Weber, P. van Belle, D.E. Elder, and M. Herlyn. 2003. Constitutive mitogen-activated protein kinase activation in melanoma is mediated by both BRAF mutations and autocrine growth factor stimulation. Cancer Res. 63:756–759. [PubMed] [Google Scholar]
- 18.Sumimoto, H., K. Hirata, S. Yamagata, H. Miyoshi, M. Miyagishi, K. Taira, and Y. Kawakami. 2006. Effective inhibition of cell growth and invasion of melanoma by combined suppression of BRAF (V599E) and Skp2 with lentiviral RNAi. Int. J. Cancer. 118:472–476. [DOI] [PubMed] [Google Scholar]