Abstract
The Wiskott-Aldrich syndrome, a primary human immunodeficiency, results from defective expression of the hematopoietic-specific cytoskeletal regulator Wiskott-Aldrich syndrome protein (WASP). Because CD4+CD25+Foxp3+ naturally occurring regulatory T (nTreg) cells control autoimmunity, we asked whether colitis in WASP knockout (WKO) mice is associated with aberrant development/function of nTreg cells. We show that WKO mice have decreased numbers of CD4+CD25+Foxp3+ nTreg cells in both the thymus and peripheral lymphoid organs. Moreover, we demonstrate that WKO nTreg cells are markedly defective in both their ability to ameliorate the colitis induced by the transfer of CD45RBhi T cells and in functional suppression assays in vitro. Compared with wild-type (WT) nTreg cells, WKO nTreg cells show significantly impaired homing to both mucosal (mesenteric) and peripheral sites upon adoptive transfer into WT recipient mice. Suppression defects may be independent of antigen receptor–mediated actin rearrangement because both WT and WKO nTreg cells remodeled their actin cytoskeleton inefficiently upon T cell receptor stimulation. Preincubation of WKO nTreg cells with exogenous interleukin (IL)-2, combined with antigen receptor–mediated activation, substantially rescues the suppression defects. WKO nTreg cells are also defective in the secretion of the immunomodulatory cytokine IL-10. Overall, our data reveal a critical role for WASP in nTreg cell function and implicate nTreg cell dysfunction in the autoimmunity associated with WASP deficiency.
The Wiskott-Aldrich syndrome is a rare X-linked human immunodeficiency with affected patients developing recurrent infections, thrombocytopenia, eczema, and, in up to 70% of cases, autoimmunity (1). WASP is a multidomain-containing protein that regulates the actin cytoskeleton in hematopoietic cells. In T cells, after TCR activation, Wiskott-Aldrich syndrome protein (WASP) relocalizes to lipid rafts, regulating localized actin polymerization and the formation/function of an immunological synapse (2–5). In peripheral T cells, the absence of WASP leads to aberrant actin rearrangement and immunological synapse formation with associated decreases in TCR-induced proliferation and aberrant IL-2 production (3–7).
WASP-deficient (WASP knockout [WKO]) mice share many features of the human disease, including global defects in leukocyte migration and podosome formation, defects in T and B cell signaling, defects in the generation of effective immune responses, and the development of autoimmunity (6–10). The majority of WKO mice develop an inflammatory bowel disease (IBD) limited to the colon (6, 11). Adoptive transfer of WKO CD4+ T cells is sufficient to induce colitis in immunodeficient hosts (unpublished data). Although WKO CD4+ T cells can induce colitis, it is not clear whether colitis in WKO mice is the result of an abnormal autoreactive effector T cell population, a defect in a regulatory T cell population, or a combination of defects in both effector and regulatory T cell function.
Naturally occurring regulatory T (nTreg) cells are defined as a subgroup of CD4+CD25+ T cells that express the forkhead winged helix transcription factor Foxp3 and are able to modulate T cell responses (12–14). nTreg cells have been implicated broadly in immune regulation and have been found to modulate transplantation tolerance, autoimmunity, tumor immunity, and the immune response against pathogens (for review see references 15–20). An imbalance between effector T cells and regulatory T cells has been implicated in many murine models of IBD. A role for nTreg cells has perhaps been defined most clearly in the CD45RB transfer model (21). In this model, adoptive transfer of CD4+CD45RBhi T cells (effector cells) to immunodeficient mice results in severe colitis. Cotransfer of CD4+CD45RBlo T cells with CD4+CD45RBhi T cells prevents disease induction, demonstrating the suppressive effect of the CD4+CD45RBlo T regulatory cell–containing population.
In this report, we show that WKO mice have reduced numbers of CD4+CD25+Foxp3+ T cells in lymphoid organs and hypothesize that colitis in WKO mice results from defective regulatory T cell function. We demonstrate that nTreg cells from WKO mice fail to protect against the colitis induced by WT or WKO CD45RBhi T cells. WKO CD4+CD25+ cells are also defective in suppressing the proliferation of WT and WKO CD4+CD25− T cells in vitro. Exogenous IL-2 administration in the presence of antigen receptor stimulation substantially rescues the defect in suppression. WKO nTreg cells are also defective in the secretion of IL-10, a cytokine shown previously to be critical for prevention of colitis (22, 23).
RESULTS
WKO mice have reduced numbers of CD4+CD25+ regulatory T cells
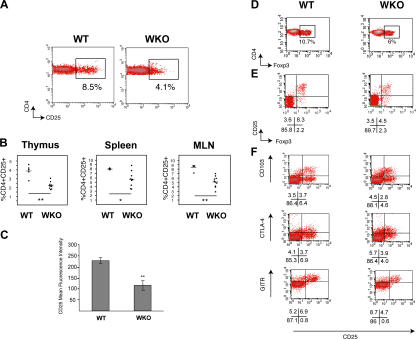
We have previously demonstrated that WKO mice develop colitis (6) and that WKO CD4+ T cells are sufficient to induce disease when transferred to RAG-2–deficient mice (unpublished data). Because nTreg cells are known to control autoimmunity in several disease states (17), we hypothesized that the colitis in WKO mice may be associated with aberrant differentiation, development, or function of nTreg cells. We first assessed the numbers of regulatory T cells in lymphoid organs from WT and WKO mice. The percentage of CD4+CD25+ regulatory T cells in the WKO spleen, mesenteric lymph nodes, and thymus was significantly reduced when compared with the percentage of nTreg cells in WT lymphoid organs (Fig. 1, A and B). In addition, WKO CD4+ T cells had reduced expression of cell surface CD25 (Fig. 1 C).
Figure 1.
WKO mice have reduced CD4+CD25+Foxp3+ regulatory T cell numbers. (A) Flow cytometric analysis of CD4 and CD25 expression on WT (left) and WKO (right) splenocytes within a CD4+ lymphocyte gate. Numbers indicate the percentage of CD25+ cells in the indicated gate. Shown are FACS profiles representative of 18 WT and 24 WKO mice on the 129SvEv background. (B) Percentage of CD4+CD25+ T cells within the CD4+ gate in the spleen (left), mesenteric lymph node (MLN; middle), and inside a CD4+CD8− single positive thymocyte gate (right). The horizontal gray bars represent the average. Shown are results of one of five independent experiments. (C) Average mean fluorescence intensity of CD25 of WT (left; n = 5) and WKO (right; n = 9) CD4+CD25+ splenocytes. Error bars represent standard deviations. (D) Decreased percentage of CD4+Foxp3+ cells in WKO mice. Shown are density plots of CD4 and Foxp3 expression in WT (left) and WKO (right) CD4+ lymphocytes (mesenteric lymph node). Numbers indicate the percentage of Foxp3+ cells in the indicated gate. FACS profiles shown are representative of >10 mice in each group. (E) Dot plots of CD25 and Foxp3 expression in CD4+ T cells from WT (left) and WKO mice (right). Shown are representative profiles from the mesenteric lymph node (similar results were obtained in the spleen). Numbers represent the percentage of cells in the corresponding quadrant. Data shown is representative of analysis of 10 individual mice (129SvEv) in each group. (F) Density plots of CD25 and CD103, CTLA-4, or GITR expression on CD4+ splenocytes from WT (left) and WKO (right) mice. Numbers represent the percentage of cells inside the corresponding quadrants. Shown are data representative of 8 WT and 12 WKO mice. *, P < 0.05; **, P < 0.01.
WKO nTreg cells have normal expression of Foxp3 and other regulatory T cell markers
Regulatory T cell differentiation and function is dependent on Foxp3, a forkhead winged helix transcription factor (13, 14, 24). Foxp3−CD4+CD25+ T cells fail to suppress proliferation in vitro (13). The numbers of WKO CD4+Foxp3+ T cells, like WKO CD4+CD25+ cells, are also decreased in peripheral lymphoid organs (Fig. 1 D). The percentage and mean fluorescence intensity of Foxp3+ cells among WKO CD4+CD25+ T regulatory cells is similar to WT T regulatory cells, suggesting adequate differentiation and lineage specification of WKO T regulatory cells despite their reduced percentage (Fig. 1, D and E). Cytotoxic T lymphocyte–associated antigen 4 (CTLA-4), CD103, and glucocorticoid-induced TNF receptor (GITR), like CD25, are cell surface markers that have been also associated with a regulatory CD4+ T cell phenotype (25–27). Expression of CTLA-4, CD103, and GITR was indistinguishable between WT and WKO CD4+ T cells (Fig. 1 F).
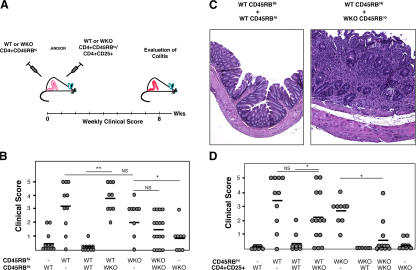
WKO regulatory T cells fail to protect against development of colitis in vivo
We first sought to determine whether WASP is required for nTreg cell suppression in vivo. To this end, we used a modification of the CD45RB transfer model of colitis (Fig. 2 A) (21). This model has the advantage of assessing both effector and regulatory T cell function. SCID mice were injected intraperitoneally with CD45RBhi T cells from either WT or WKO mice alone or in combination with WT or WKO CD45RBlo T cells (Fig. 2 A). Mice were assessed weekly for clinical signs of colitis for 8 wk, followed by histological analysis. WT CD45RBhi T cells, when injected alone, induced severe colitis (Fig. 2 B). Colitis induction was suppressed when WT CD45RBlo T cells were cotransferred with WT CD45RBhi T cells (Fig. 2, B and C). In contrast, WKO CD45RBlo T cells were unable to suppress colitis induction when cotransferred with WT CD45RBhi T cells (Fig. 2, B and C). When CD45RBhi T cells from WKO mice were injected alone, mice developed colitis, although associated with later onset and decreased severity (Fig. 2 B). Not surprisingly, fewer CD4+ T cells were recovered from the periphery of recipient mice receiving WKO CD45RBhi T cells (not depicted). Nonetheless, cotransfer of WKO CD45RBlo T cells could not prevent the onset of colitis in these mice. As expected, neither WT CD45RBlo nor WKO CD45RBlo T cells when injected alone induced colitis (Fig. 2 B). These data demonstrate that WKO CD45RBlo T cells were unable to protect against colitis induction by WT CD45RBhi T cells.
Figure 2.
WKO nTreg cells fail to suppress colitis induction in the CD45RB transfer model. (A) WT or WKO CD4+CD45RBhi T cells were injected alone or together with WT or WKO CD4+CD45RBlo T cells into SCID mice at day 0. Mice were assessed clinically weekly for a total of 8–12 wk followed by histological analysis. In a different set of experiments, CD4+CD25+ T cells were used instead of CD4+CD45RBlo T cells. (B) Clinical score of colitis 8 wk after transfer of WT or WKO CD4+CD45RBhi T cells and WT or WKO CD4+CD45RBlo T cells. Each dot represents an individual mouse. Horizontal bars represent average. Shown are combined data of four independent experiments. (C) Hematoxylin and eosin–stained cross sections of colonic sections taken 8 wk after transfer of WT CD4+CD45RBhi T cells and WT (left) or WKO (right) CD4+CD45RBlo T cells to SCID recipient mice. (D) Clinical score of colitis 8 wk after transfer of WT or WKO CD4+CD45RBhi T cells and WT or WKO CD4+CD25+ nTreg cells. Each dot represents an individual mouse. Horizontal bars represent average. Shown are the combined data of three independent experiments. NS, Nonsignificant (P > 0.05). *, P < 0.05; **, P < 0.01.
To determine whether the CD4+CD25+Foxp3+ nTreg cells within the CD45RBlo population were responsible for the observed suppression defects, we performed analogous cotransfer experiments in which CD4+CD25+ T cells were transferred in combination with CD45RBhi T cells (Fig. 2 A). As expected, the transfer of WT CD45RBhi T cells alone induced colitis, a process that was blocked by the cotransfer of WT CD4+CD25+ T cells (Fig. 2 D). Neither WT nor WKO CD4+CD25+ T cells induced colitis when transferred alone. Importantly, WKO CD4+CD25+ T cells did not suppress colitis induction when cotransferred with WT CD45RBhi T cells (Fig. 2 D). However, WKO CD4+CD25+ T cells suppressed colitis induction by WKO CD45RBhi. These findings, although in contrast to the lack of suppression seen with WKO CD45RBlo on WKO CD45RBhi T cells, correlated well with the enrichment of nTreg cells within the CD4+CD25+ population (Fig. S1, available at http://www.jem.org/cgi/content/full/jem.20061338/DC1) and with our in vitro experiments described below.
We further assessed whether WKO CD45RBhi T cells could receive a suppressive signal from WT CD4+CD25+ T cells. WT CD4+CD25+ T cells effectively blocked colitis induction by WKO CD45RBhi T cells, indicating that WASP is not required for CD45RBhi T cells to receive a suppressive signal from nTreg cells (Fig. 2 D). In all groups examined, the histopathological assessment of colitis correlated well with the clinical scores (not depicted). Collectively, these data indicate that WKO nTreg cells are less effective at suppressing colitis induction in the CD45RB transfer model.
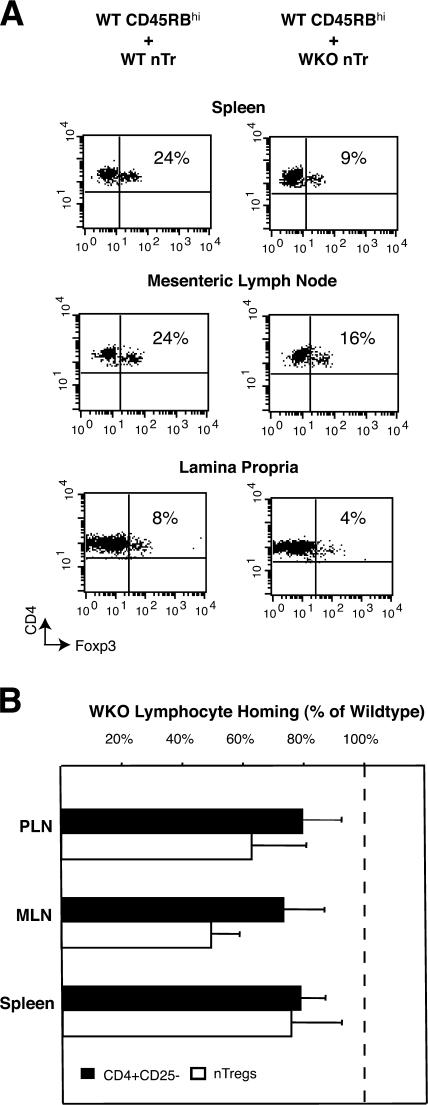
Defective homing of WKO nTreg cells to peripheral lymphoid organs
We have previously demonstrated in vitro and in vivo that WKO mice have global defects in directed leukocyte migration (28). We hypothesized that the failure of WKO nTreg cells to suppress colitis in the CD45RB transfer model may result, at least in part, from defects in migration of WKO nTreg cells to target organs. Consistent with this hypothesis, the numbers of WKO nTreg cells recovered from the spleen, mesenteric lymph nodes, and lamina propria was reduced compared with WT nTreg cells in mice cotransferred with WT CD45RBhi T cells (Fig. 3 A).
Figure 3.
Defective homing of WKO nTreg cells to peripheral lymphoid organs. (A) Reduced accumulation of WKO nTreg cells in the CD45RB transfer model. SCID mice were cotransferred with WT CD4+CD45RBhi and either WT (left) or WKO (right) nTreg cells. 10 wk after transfer, spleen, mesenteric lymph node, and colonic lamina propria cells were collected and stained for CD4 and Foxp3. Shown are representative dot plots of 6 and 10 mice per group. (B) nTreg cells or CD4+CD25− cells were isolated from peripheral lymphoid organs of WT and WKO mice, labeled with CFSE (WT) or TRITC (WKO), and mixed at a 1:1 ratio before intravenous injection to WT mice. Spleen and peripheral and mesenteric lymph nodes of recipient mice were harvested after 12–15 h, and the percentage of WKO lymphocyte homing relative to WT was determined. Shown are averages ± SD of combined data from two experiments including eight (CD4+CD25−) and seven (nTreg cells) mice per group. Dashed line represents the input percentage.
To assess directly whether WKO nTreg cells had defects in migration to peripheral lymph nodes, we used an in vivo migration assay. Equal numbers of WT and WKO nTreg cells were labeled with either tetramethylrhodamine isothiocyanate (TRITC) (red) or CFSE (green). Both populations were mixed at a ratio of 1:1 immediately before intravenous injection into a WT recipient mouse. To monitor the homing characteristics, recipient mice were killed 12–15 h after adoptive transfer. Analogous experiments were performed with WT and WKO CD4+CD25− T cells. Lymphoid organs were harvested, and single cell suspensions were analyzed using flow cytometry (Fig. 3 B). There was a statistically significant decrease in the homing of WKO nTreg cells or WKO CD4+CD25− T cells to the spleen and peripheral and mesenteric lymph node when compared with WT cells.
In light of the relative homing defects, we asked whether the defects in suppression by WKO nTreg cells in the CD45RB transfer model of colitis might be overcome by increasing the number of nTreg cells at the time of transfer. In contrast to the failure of suppression of colitis by WKO nTreg cells when transferred at a standard 1:4 ratio with WT CD45RBhi cells, colitis was effectively suppressed when WKO nTreg cells were transferred at a higher 1:1 ratio (clinical score: 3.3, WT CD45RBhi alone; 0.3, WT CD45RBhi plus WT nTreg cell [low dose]; 2.3, WT CD45RBhi plus WKO nTreg cell [low dose]; 0.0, WT CD45RBhi plus WKO nTreg cell [high dose]; 0.2, WKO nTreg cell alone [high dose]; n = 3–5 animals/group).
The observation that transfer of increased numbers of WKO nTreg cells (relative to WT) effectively suppresses the colitis induced by the transfer of CD45RBhi cells is consistent with the relatively inefficient homing of WKO nTreg cells to mucosal surfaces demonstrated in Fig. 3 (A and B).
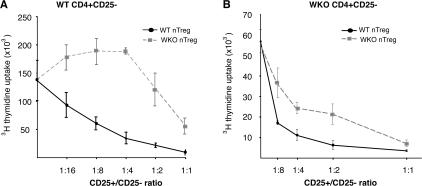
WKO nTreg cells have defective suppressor function in vitro
We next sought to extend our in vivo findings by using an in vitro suppression assay (29). WT CD4+CD25− T cells were cocultured with mitomycin-treated WT APCs in the presence of anti-CD3ɛ antibodies and WT or WKO nTreg cells. Suppression of proliferation by WT or WKO nTreg cells was assessed by [3H]thymidine incorporation. As expected, WT nTreg cells efficiently suppressed proliferation, readily apparent at a CD25+/CD25− cell ratio of 1:16 (Fig. 4 A) (29). In contrast, even at a 1:1 CD25+/CD25− cell ratio, WKO nTreg cells failed to suppress the proliferation of WT CD25− cells (Fig. 4 A). Moreover, consistent with these findings, preliminary data suggest that WT but not WKO nTreg cells suppress the secretion of IFN-γ by WT CD25− T cells in this coculture system (unpublished data).
Figure 4.
WKO nTreg cells are defective in suppressing T cell proliferation in vitro. CD4+CD25− cells were isolated from the spleens of WT (A) and WKO (B) mice and were cocultured with mitomycin-treated T cell–depleted splenocytes and 0.5 μg/ml anti-CD3ɛ for 3 d in the presence of varying numbers of CD4+CD25+ regulatory T cells (nTreg cells) coming from the spleen of WT (black full line, dots) or WKO (gray dashed curve, squares) mice. Proliferation was measured by [3H]thymidine uptake (y axis). Ratios of CD25+/CD25− T cells are indicated on the x axis. Shown is one representative of five (left) and three (right) independent experiments performed in triplicate.
As in our in vivo studies, WT nTreg cells inhibited the proliferation of WKO CD4+CD25− T cells (Fig. 4 B), demonstrating that WKO responder T cells can receive a suppressive signal coming from WT nTreg cells. However, although suppressive at maximal ratios, WKO nTreg cells were less effective than WT nTreg cells at suppressing proliferation of WKO CD4+CD25− (consistent with our in vivo data; Fig. 2 D). Suppression of WKO but not WT naive T cells by WKO nTreg cells may be explained by evidence in vitro and in vivo supporting reduced activation/proliferation of WKO effector cells. First, as shown previously with total WKO T cells (6, 7), WKO CD4+CD25− T cells proliferate poorly upon antigen receptor activation (Fig. 4). Second, as discussed above, WKO CD45RBhi T cells induce colitis upon transfer with lower severity than WT CD45RBhi T cells and are associated with decreased numbers of T cells in recipient mice.
WKO nTreg cells are not associated with TCR-induced defects in actin remodeling
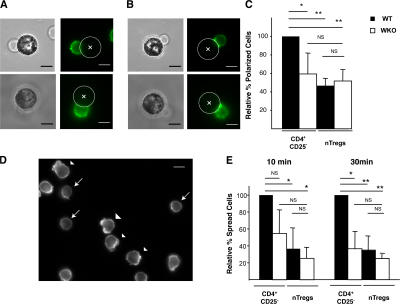
Although remodeling of the actin cytoskeleton and formation of an immunological synapse appear to be important for TCR signaling in peripheral T cells (30–32), a role for actin remodeling and immunological synapse formation has not been described for regulatory T cells. Because WASP has been demonstrated to regulate actin remodeling and immunological synapse formation, we hypothesized that deficiencies in these processes might contribute to WKO nTreg cell dysfunction (2–5). When compared with WT CD4+CD25− cells, both WT and WKO nTreg cells polarized their actin cytoskeleton less efficiently upon stimulation with anti-CD3/anti-CD28–coated beads (Fig. 5, A–C, and Table S1, which is available at http://www.jem.org/cgi/content/full/jem.20061338/DC1). As expected, WKO CD4+CD25− T cells polarized their actin cytoskeleton inefficiently when compared with WT CD4+CD25− cells (2–5).
Figure 5.
WT and WKO nTreg cells inefficiently remodel their actin cytoskeleton upon T cell receptor activation. (A–C) Reduced actin polarization of WT and WKO nTreg cells upon incubation with anti-CD3/anti-CD28–coated beads. Representative examples of cells with nonpolarized (A) and polarized actin (B) are displayed. Left panels represent phase images, and right panels show actin staining. Beads are marked with a cross. Bars, 5 μm. The percentage of CD4+CD25− or nTreg cells (black, WT; white, WKO) with polarized cytoskeleton relative to WT CD4+CD25− is shown in C. For each group, at least 300 conjugated cells have been examined. Shown are averages of three independent experiments ± SD. (D and E) Reduced T cell spreading by WT and WKO nTreg cells. An example of actin staining of WT CD4+CD25− splenocytes 10 min after incubation on anti-CD3/anti-CD28–coated coverslips is shown in D. Examples of spread T cells are indicated by arrowheads, and unspread T cells are represented by arrows. Bar, 5 μm. The percentage of CD4+CD25− or nTreg cells (isolated from WT [black] or WKO [white] mice) that were spread relative to WT CD4+CD25− is shown in E. For each group, at least 300 cells have been examined. Shown are averages of three independent experiments ± SD. NS, Nonsignificant (P > 0.05). *, P < 0.05; **, P < 0.01.
We next analyzed T cell spreading on anti-CD3/anti-CD28–coated coverslips (Fig. 5, D and E, and Table S1). As observed for polarization, we observed a decrease in the spreading of WT nTreg cells when compared with WT CD4+CD25− cells at both 10 and 30 min after TCR stimulation (Fig. 5 E and Table S1). The percentage of spread WKO nTreg cells was similar to WT nTreg cells. Finally, the percentage of spread WKO CD4+CD25− cells was reduced when compared with WT CD4+CD25− cells (Fig. 5 E and Table S1). Collectively, our data suggest that WT and WKO nTreg cells remodel their actin cytoskeleton upon TCR stimulation less efficiently than CD4+CD25− T cells.
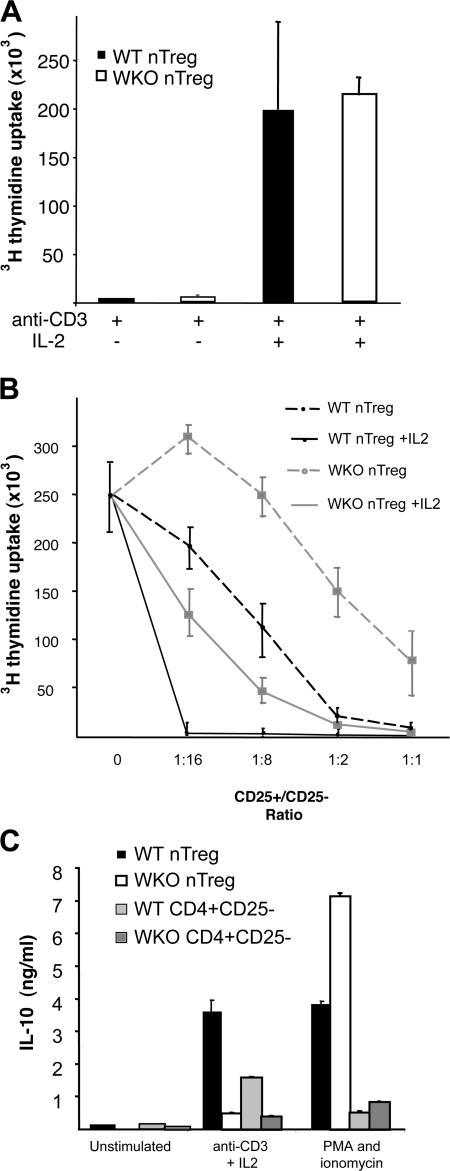
Defective suppression by WKO nTreg cells is substantially rescued by exogenous IL-2 stimulation
Previous work has demonstrated that, in vitro, the resistance of CD4+CD25+ nTreg cells to TCR-induced stimulation can be overcome by the addition of exogenous IL-2 (29). We have found that, like WT nTreg cells, the inability of WKO nTreg cells to proliferate in response to TCR-induced stimulation is overcome by the addition of exogenous IL-2 (Fig. 6 A). IL-2 has also been shown to be required for efficient generation of CD4+CD25+Foxp3+ cells in vivo (33–35) as well as for their maximal suppressive activity (36, 37). IL-2 secretion is also required to control self-reactive T cells, as demonstrated by pronounced autoimmune pathologies developed by IL-2–deficient mice (38). Because defective IL-2 secretion is one of the hallmarks of WASP deficiency in T cells, we reasoned that WKO nTreg cell dysfunction might result from impaired IL-2–induced signaling and inadequate nTreg cell activation. To address this issue, we precultured WT or WKO CD4+CD25+ nTreg cells with 10 μg/ml of plate-bound anti-CD3ɛ and 25 μg/ml IL-2 for 3 d and compared suppression to freshly isolated WT or WKO nTreg cells (Fig. 6 B). As expected, IL-2 preactivation enhanced suppression by WT nTreg cells (37). IL-2 preactivation of WKO nTreg cells enhanced suppression to levels comparable with freshly isolated WT nTreg cells. Although WKO nTreg cell suppressive function improved with exogenous IL-2, the suppressive activity of preactivated WKO nTreg cells was lower than that of the preactivated WT nTreg cells, suggesting that IL-2–independent signaling defects contribute to WKO nTreg cell dysfunction. This is reminiscent of our prior data demonstrating rescue, at least in part, of antigen receptor–mediated defects in proliferation of WKO T cells through exogenous addition of IL-2 (6).
Figure 6.
Exogenous IL-2 rescues WKO nTreg cell dysfunction. (A) WKO nTreg cells do not proliferate upon CD3-mediated stimulation and respond to exogenous IL-2. [3H]thymidine uptake of CD4+CD25+ nTreg cells isolated from the spleens of WT (black bars) or WKO (white bars) mice 3 d after stimulation with mitomycin-treated T cell–depleted splenocytes and 0.5 μg/ml anti-CD3ɛ or 0.5 μg/ml anti-CD3ɛ plus 10 μg/ml IL-2. Shown are averages ± SD of one representative of three independent experiments performed in triplicate. (B) IL-2 and antigen receptor–mediated preactivation of WKO nTreg cells substantially rescues their proliferation defects. [3H]thymidine uptake of CD4+CD25− T cells isolated from the spleens of WT mice and cocultured with CD4+CD25+ cells from WT (black curves) or WKO (gray curves) mice at different CD25+/CD25− ratios. Dashed curves represent suppressive effects of WT or WKO nTreg cells after a prior 3-d activation with 10 μg/ml of plate-bound anti-CD3ɛ and 25 μg/ml IL-2. Shown are results of one out of three independent experiments performed in triplicate. (C) Decreased IL-10 secretion of stimulated WKO nTreg cells. IL-10 concentrations were determined by ELISA in the supernatant of nTreg cells or CD4+CD25− splenocytes isolated from WT or WKO mice that were unstimulated or stimulated for 3 d with 10 μg/ml anti-CD3ɛ and 25 μg/ml IL-2, or PMA and ionomycin. Shown are averages of one representative of four independent experiments, each performed in duplicate. Error bars represent standard deviations.
Defective IL-10 secretion by WKO nTreg cells
IL-10 has been shown to play a major role in the regulation of colitis in the CD45RB transfer model (22, 23, 39). We therefore analyzed IL-10 secretion by WKO T cells. WT and WKO CD4+CD25+ nTreg cells were cultured for 3 d with plate-bound anti-CD3 and IL-2 or PMA and ionomycin, and culture supernatants were harvested to assay IL-10 concentration by ELISA. IL-10 secretion was dramatically decreased upon stimulation of WKO nTreg cells (Fig. 6 C). In contrast, stimulation with PMA and ionomycin, which bypasses proximal TCR signals, rescued this defect (Fig. 6 C). This defect in IL-10 secretion was not nTreg cell specific because the same defect was observed in WKO CD4+CD25− cells.
DISCUSSION
Autoimmunity is one of the hallmarks of the Wiskott-Aldrich syndrome, with a majority of patients suffering from at least one autoimmune disorder (hemolytic anemia, neutropenia, arthritis, skin vasculitis, glomerulonephritis, or IBD) (1). Likewise, 100% of WKO mice develop colitis by 6 mo of age (unpublished data) (6, 11). The colitis in WKO mice is unique among murine models of IBD in that it is the only model that has a human counterpart. We sought to investigate the mechanisms responsible for the immune dysregulation leading to colitis in WKO mice and postulated that abnormalities in the homeostasis/function of regulatory T cells may play a contributing role.
CD4+CD25+Foxp3+ regulatory T cells are key regulators of autoreactive T cells in vivo (15–19). In mice, CD4+CD25+Foxp3+ nTreg cells are generated in the thymus during the first weeks of life and are dependent on the expression of Foxp3 (40). We have demonstrated that WASP is important for the homeostasis of CD4+CD25+Foxp3+ T cells in the thymus as well as in peripheral lymphoid organs. Furthermore, WASP is critically required for the ability of CD4+CD25+ T cells to mediate suppression in vivo and in vitro. The observed defects in suppression in vivo correlate well with the demonstrated defects in homing of WKO CD4+CD25+ T cells to target organs, findings that are consistent with the known defects in global migration by WKO leukocytes (28). Nonetheless, migration defects cannot fully explain the suppression defects because these defects are still evident in the in vitro coculture system, an assay in which migratory capacity is unlikely to play a significant role.
T cell activation by APCs is associated with reorganization of the actin cytoskeleton and the concomitant formation of an immunological synapse (31, 32). In peripheral T cells, WASP plays a critical role in the reorganization of the actin cytoskeleton and immunological synapse formation (3–7). We postulated that defects in antigen receptor–induced actin remodeling and immunological synapse formation might be responsible for the regulatory T cell defects in WKO mice. However, both WT and WKO CD4+CD25+ nTreg cells poorly remodeled their actin cytoskeleton after antigen receptor stimulation when compared with WT CD4+CD25− nTreg cells. Recently, nTreg cells and dendritic cells have been demonstrated to interact directly in vivo (41). Although our data do not exclude a role for actin remodeling and immunological synapse formation in nTreg cell function, they clearly suggest different signaling requirements for the induction of antigen receptor–induced cytoskeletal changes in nTreg cells.
Although WASP is not required for the development of CD4+ T cells (6, 7), the generation/homeostasis of CD4+CD25+Foxp3+ T cells may be particularly sensitive to WASP deficiency. Numerous studies have demonstrated a critical role for WASP in antigen receptor–induced signaling in T cells (6, 7, 42). Studies using TCR-transgenic mice suggest that WT nTreg cells are generated after recognition of self-antigens in the thymus, with nTreg cell–selective events requiring relatively high affinity interactions (43, 44). CD28 costimulation and IL-2 are also required for efficient nTreg cell generation in thymocytes, as illustrated by decreased nTreg cell numbers in CD28 knockout and IL-2 knockout mice (33, 45, 46). However IL-2 appears to have a more critical role in nTreg cell maintenance in the periphery (33). Although CD28-mediated signals have been shown to partly rescue the proliferation defects of WKO T cells (4, 6), and potential defects in CD28 costimulation in WKO nTreg cells were not assessed in this report, a complementary report suggests that CD28 signaling does not rescue the defects in proliferation by WKO nTreg cells (see Marangoni et al. on p. 369 of this issue). Defects in IL-2 production and secretion have been observed consistently in WKO T cells (2, 6, 7, 42). Exogenous IL-2 can rescue, at least in part, antigen receptor–induced signaling events in both naive WKO T cells (6, 7) and WKO nTreg cells. We have also demonstrated a reduction in CD25 (i.e., IL-2Rα) surface expression on WKO nTreg cells. Collectively, we hypothesize that defective IL-2 production and antigen receptor activation contribute to the observed decrease in numbers and function of naturally occurring nTreg cells in WKO mice (Fig. 7). This defect in antigen receptor activation may result, in part, by an increase in the activation threshold of WKO nTreg cells that is overcome by IL-2 stimulation. This is further supported by recent complementary data directly demonstrating that proliferative defects of WKO nTreg cells can be diminished with increased stimulation through the TCR (Marangoni et al., in this issue). Defective IL-2 secretion or IL-2–induced signaling events are unlikely to be solely responsible for the nTreg cell dysfunction because CD4+Foxp3+ cells from IL-2 or CD25 knockout mice are as suppressive in vitro as WT cells (33). Because Foxp3 is expressed normally in WKO CD4+CD25+ cells, our data do not support a direct role for either WASP or antigen receptor–mediated signaling events in regulating Foxp3 expression and suggest that the suppressive defects in WKO nTreg cells are downstream and/or independent of Foxp3.
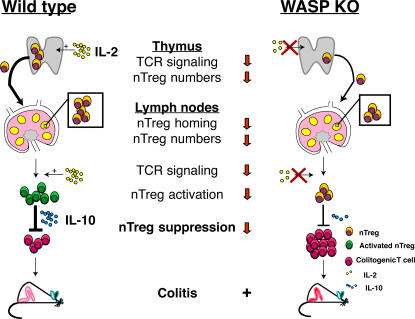
Figure 7.
Proposed model for nTreg cell dysfunction and colitis development in WKO mice. Decreased nTreg cell numbers in both the thymus and the periphery (lymph nodes) are observed in WKO mice and may result from IL-2 deficiency and TCR activation defects. IL-2 deficiency, aberrant nTreg cell homing, activation, and reduced IL-10 secretion lead to impaired suppression of colitogenic T cells and colitis.
IL-10 appears to be a key player in the regulation of autoimmunity in the colon. IL-10–producing T cells (Tr1) can prevent colitis induction in the CD45RB transfer model (23). However, regulatory T cells isolated from IL-10–deficient mice do not protect against colitis induced by WT CD45RBhi cells (22). Further, injection of an anti–IL-10–neutralizing antibody together with WT CD4+CD45RBlo cells abrogates suppression (22). In this report, in vitro stimulation of WKO T cells was associated with a marked defect in IL-10 secretion, suggesting a contributing role for IL-10 in WKO nTreg cell dysfunction in vivo (Fig. 7). However, preliminary data suggest that IL-10 supplementation at the time of suppression does not rescue the defects in suppression observed in vitro by WKO nTreg cells (unpublished data).
Abnormalities in nTreg cell function have been implicated in the development of autoimmunity, immunopathology, and allergy in several human diseases. The rare X-linked recessive autoimmune/inflammatory syndrome IPEX (immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome) is also associated with an autoimmune enteropathy (47). This disorder is caused by a mutation in Foxp3 and results from a profound reduction of CD4+CD25+ nTreg cells (48, 49). Our data now implicate regulatory T cell dysfunction in the pathogenesis of the immune dysregulation associated with another human disorder, the autoimmunity associated with the Wiskott-Aldrich syndrome (Fig. 7). Lending further support to this hypothesis are recent data identifying defects in suppression in human nTreg cells analogous to those described herein with murine nTreg cells (Marangoni et al., in this issue).
MATERIALS AND METHODS
Mice.
WKO mice (129 SvEv background) were generated as described previously (6) and backcrossed >10 generations onto the BALB/c background. C.B-17 SCID mice were purchased from Taconic. Mice were maintained in specific pathogen-free animal facilities at Massachusetts General Hospital. WKO mice on both the 129 SvEv and BALB/c background developed colitis in our facility. All experiments were conducted after approval and according to regulations of the Subcommittee on Research Animal Care at Massachusetts General Hospital.
Antibodies and reagents.
PE- and allophycocyanin-labeled coupled anti-CD25 antibodies; FITC-conjugated or peridinin chlorophyll protein anti-CD4; FITC-conjugated anti-CD103; PE-coupled anti–CTLA-4; PE-coupled streptavidin; and PE- and FITC-coupled anti-CD45RB antibodies were purchased from BD Biosciences. Biotinylated anti-GITR antibodies were purchased from R&D Systems, and intranuclear Foxp3 staining was performed using the FITC-coupled anti-Foxp3 intracellular staining kit (eBioscience).
Flow cytometry.
Flow cytometric analyses were performed on a FACSCalibur flow cytometer (Becton Dickinson) using CELLQuest software (Becton Dickinson). More than 10,000 events were recorded through a lymphocyte gate. Analyses of CD4+CD25+ cells from the thymus and lymph nodes were performed on both the BALB/c and the 129 SvEv background, and similar findings were obtained.
Isolation of cell subsets.
For the CD45RB transfer studies, mesenteric lymph nodes were carefully dissected from 10 WT or WKO BALB/c mice, and lymphocytes were isolated by gently mincing the lymph nodes through a cell strainer in RPMI 1640 supplemented with 10% FCS, 100 U/ml penicillin, 100 μg/ml streptomycin, 2 mM l-glutamine (all from Invitrogen), and 50 μM β-mercaptoethanol (Sigma-Aldrich). CD4+ cells were then negatively selected using magnetic cell sorting according to the manufacturer's recommendations (CD4+ isolation kit; Miltenyi Biotec). CD45RBhi and CD45RBlo T cells from the CD4+ population were isolated using a MoFlo cell sorter (DakoCytomation). CD4+CD25+ T cells were isolated from the spleen and positively selected using magnetic cell sorting (regulatory T cell isolation kit; Miltenyi Biotec).
For the in vitro suppression assay, spleens were dissected from WT or WKO BALB/c mice, and splenocytes were isolated by gently mincing the spleens through a cell strainer in FCS-supplemented RPMI. Cells were then spun down and resuspended in ACK lysis buffer to lyse erythrocytes before proceeding to cell separation. CD4+CD25+ T cells were positively selected using magnetic cell sorting as described above (purity typically ranged between 90 and 95%). CD4+CD25− cells were isolated using the flow-through from the previous step, followed by further purification with a CD4+ isolation kit (Miltenyi Biotec). Purity typically was ∼95%.
APCs were isolated by incubating total WT splenocytes with an anti-Thy1.2 antibody (Cedarlane Laboratories), followed by treatment with rabbit complement (1:10 dilution, 107 cells/ml; Cedarlane Laboratories) for 1 h at 37°C. Dead cells were removed using a lympholyte-M gradient (Cedarlane Laboratories). The resulting T cell–depleted splenocytes were treated with 50 μg/ml mitomycin in PBS for 20 min at 37°C and washed thoroughly before in vitro usage.
For lamina propria cell isolation, colons from WT and WKO mice were washed with PBS and digested with 2 mg/ml dispase (Invitrogen) at 37°C for 1 h in complete media (RPMI 1640 media supplemented with 4% FCS, 2 mM l-glutamine, 10 mM Hepes, 100 U/ml penicillin, 100 μg/ml streptomycin, and 250 ng/ml amphotericin) to remove the epithelial compartment including intraepithelial lymphocytes. Samples were then minced into small pieces and further digested with 1 mg/ml collagenase (Invitrogen) and 1.5 mg/ml dispase (Invitrogen) for 1 h at 37°C. After washing, cells were passed through a glass wool column and further purified via a 40/70% Percoll gradient method to remove epithelial and dead cells. Cells at the interface were isolated and washed with PBS before flow cytometric staining.
Functional assessment of nTreg cells in vivo.
CD45RBhi, CD45RBlo, or CD4+CD25+ T cells were isolated from WT or WKO BALB/c mice as described above. At day 0, C.B-17 SCID mice were injected intraperitoneally with 4 × 105 CD4+CD45RBhi T cells alone or in combination with 2 × 105 CD45RBlo or 105 CD4+CD25+ T cells. Mice were clinically assessed every week for signs of colitis. The clinical score was defined as follows: Wasting: 0, no wasting; 1, 0.1–10% loss of initial total body weight; 2, >10% loss of initial total body weight; diarrhea: 0, none; 1, soft stool; 2, watery and/or bloody; hunching/bristled fur/skin lesions: 0, unchanged; 1, any positive sign; rectum prolapse: 0, absent; 1, present. 8–12 wk after transfer, mice were killed and colons were dissected, fixed in 10% buffered formalin, and embedded in paraffin for histological analysis.
Histology and histological grading.
Hematoxylin and eosin staining was performed using standard techniques. Histological grading was based on mucosal thickening (0–3), lymphocyte infiltration (0–3), and crypt abscess occurrence (0–1).
In vivo homing assays.
Analysis of homing of WKO nTreg cells was performed as described previously (50). Single cell suspensions of spleen, mesenteric lymph node and peripheral lymph node lymphocytes were prepared from WT and WKO mice. First, 107 cells (for CD4+CD25− cells) and 106 cells (for nTreg cells) of each population was labeled for 20 min at 37°C with either CFSE or TRITC (both from Invitrogen) spun down on an FBS gradient and washed three times with cold RPMI 1640 containing 10% FCS (Life Technologies). Cells were then mixed and injected in the retroorbital plexus of anesthetized WT recipient mice. Remaining cells were analyzed to determine the exact cell input. After 12–15 h, spleen, peripheral lymph nodes, and mesenteric lymph nodes from recipient mice were analyzed by FACS after gating for viable lymphocytes by forward and light scatter characteristics. The relative frequency of the two donor cell populations was determined for each individual organ, and a homing index was calculated as described previously (50). Identical results were obtained when WT and WKO cells were stained with the alternative labeling agent.
In vitro suppression assays.
For in vitro anti-CD3ɛ–induced proliferation, 5 × 104 CD4+CD25− cells were cultured in 96-well round-bottom plates together with 105 mitomycin-treated T cell–depleted splenocytes and 0.5 μg/ml anti-CD3ɛ (BD Biosciences). CD4+CD25+ cells from WT or WKO mice were added to the culture in various ratios as indicated in Fig. 4. Proliferation was measured by pulsing the cells for 12 h with 1 μCi [3H]thymidine after 60 h of stimulation. For the preactivation of nTreg cells with IL-2, splenic nTreg cells from WT or WKO mice were cultured with 10 μg/ml of plate-bound anti-CD3ɛ and 25 μg/ml IL-2 (both from BD Biosciences) for 3 d and washed extensively before the in vitro suppression assays.
Cytokine analysis in culture supernatant.
CD4+CD25− or CD4+CD25+ splenocytes from WT or WKO mice were isolated and cultured in the presence of 10 μg/ml of plate-bound anti-CD3ɛ and 25 μg/ml IL-2, or 5 ng/ml PMA and 500 ng/ml ionomycin (both from Sigma-Aldrich). After 3 d of stimulation, culture supernatants were harvested, spun down, and stored at −20°C before ELISA analysis. IL-10 concentrations were determined by ELISA as described previously (51).
T cell–bead conjugates.
10-μm latex beads were coated with 10 μg/ml anti-CD3ɛ and 10 μg/ml anti-CD28 (BD Biosciences) for 1 h at 37°C, washed thoroughly with PBS, and blocked with PBS/BSA 1% for 30 min. Purified T cell subsets (2 × 105 cells/ml) were then incubated with the coated beads (4 × 105 beads/ml) for 10 or 30 min in supplemented medium (RPMI 1640) at 37°C to create T cell–bead conjugates. The conjugates were then plated on poly-l-lysine–coated coverslips for 10 min and fixed with 4% paraformaldehyde. Cells were then permeabilized using 0.2% Triton X-100 in PBS and actin stained with AlexaFluor-488 Phalloidin (Cambrex Bio Science Inc.). Coverslips were then mounted using Vectorshield mounting medium (Vector Laboratories) and examined by fluorescence microscopy (100× objective). Cells were defined as polarized if the intensity of the actin staining was stronger on the pole of the cell in contact with the bead, whereas unpolarized cells were defined as having a uniform staining pattern.
T cell spreading.
Coverslips were coated with 10 μg/ml anti-CD3ɛ and 10 μg/ml anti-CD28 (BD Biosciences) for 1 h at 37°C and washed thoroughly. 105 CD4+CD25− or CD4+CD25+ cells from WT or WKO animals were then incubated on coated coverslips for the desired time and fixed, permeabilized, stained, and mounted as described above. Spread cells were defined as cells having a flattened lamellipodia-like sheath of actin, whereas unspread cells were round in shape.
Statistical analysis.
Significance was assessed for nTreg cell numbers using the Mann-Whitney test. For intergroup comparisons in the CD45RB transfers as well as in the actin polarization and spreading experiments, an unpaired two-tailed Student's t test was used. p-values of <0.05 were considered significant.
Online supplemental material.
Fig. S1 characterizes CD25 and Foxp3 expression of WKO CD4+CD45RBlo cells. Table S1 gives the raw data of the three independent experiments (shown in Fig. 4) assessing spreading and actin polarization of WT or WKO CD4+CD25− cells and nTreg cells. The online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20061338/DC1.
Supplemental Material
Acknowledgments
We thank Raif Geha, Daniel K. Podolsky, Richard Blumberg, and Lisa Westerberg for review of the manuscript; Hajime Isomoto for assistance with preliminary experiments; Svend Rietdij and Cox Terhorst for assistance with the initial CD45RB transfers; and Andrew Luster, Shannon Bromley, and Rodrigo Mora for input on the homing assays. Finally, we thank Maria-Grazia Roncarolo, Loic Dupre, Sara Trifari, and Francesco Marangoni for sharing results before publication.
This work was supported by National Institutes of Health grants HL59561 (to S.B. Snapper), AI50950 (to S.B. Snapper), DK47677 (to A.K. Bhan), and DK43351 (to S.B. Snapper, A.K. Bhan, and C. Nagler), and postdoctoral support from CAPES (to V. Cotta-de-Almeida), the SICPA foundation, and Lausanne University Hospital (to M.H. Maillard).
The authors have no conflicting financial interests.
Abbreviations used: CTLA-4, cytotoxic T lymphocyte–associated antigen 4; GITR, glucocorticoid-induced TNF receptor; IBD, inflammatory bowel disease; nTreg, naturally occurring regulatory T; TRITC, tetramethylrhodamine isothiocyanate; WASP, Wiskott-Aldrich syndrome protein; WKO, WASP knockout.
M.H. Maillard and V. Cotta-de-Almeida contributed equally to this work.
References
- 1.Dupuis-Girod, S., J. Medioni, E. Haddad, P. Quartier, M. Cavazzana-Calvo, F. Le Deist, G. de Saint Basile, J. Delaunay, K. Schwarz, J.L. Casanova, et al. 2003. Autoimmunity in Wiskott-Aldrich syndrome: risk factors, clinical features, and outcome in a single-center cohort of 55 patients. Pediatrics. 111:e622–e627. [DOI] [PubMed] [Google Scholar]
- 2.Cannon, J.L., and J.K. Burkhardt. 2004. Differential roles for Wiskott-Aldrich syndrome protein in immune synapse formation and IL-2 production. J. Immunol. 173:1658–1662. [DOI] [PubMed] [Google Scholar]
- 3.Badour, K., J. Zhang, F. Shi, M.K. McGavin, V. Rampersad, L.A. Hardy, D. Field, and K.A. Siminovitch. 2003. The Wiskott-Aldrich syndrome protein acts downstream of CD2 and the CD2AP and PSTPIP1 adaptors to promote formation of the immunological synapse. Immunity. 18:141–154. [DOI] [PubMed] [Google Scholar]
- 4.Dupre, L., A. Aiuti, S. Trifari, S. Martino, P. Saracco, C. Bordignon, and M.G. Roncarolo. 2002. Wiskott-Aldrich syndrome protein regulates lipid raft dynamics during immunological synapse formation. Immunity. 17:157–166. [DOI] [PubMed] [Google Scholar]
- 5.Sasahara, Y., R. Rachid, M.J. Byrne, M.A. de la Fuente, R.T. Abraham, N. Ramesh, and R.S. Geha. 2002. Mechanism of recruitment of WASP to the immunological synapse and of its activation following TCR ligation. Mol. Cell. 10:1269–1281. [DOI] [PubMed] [Google Scholar]
- 6.Snapper, S.B., F.S. Rosen, E. Mizoguchi, P. Cohen, W. Khan, C.H. Liu, T.L. Hagemann, S.P. Kwan, R. Ferrini, L. Davidson, et al. 1998. Wiskott-Aldrich syndrome protein-deficient mice reveal a role for WASP in T but not B cell activation. Immunity. 9:81–91. [DOI] [PubMed] [Google Scholar]
- 7.Zhang, J., A. Shehabeldin, L.A. da Cruz, J. Butler, A.K. Somani, M. McGavin, I. Kozieradzki, A.O. dos Santos, A. Nagy, S. Grinstein, et al. 1999. Antigen receptor–induced activation and cytoskeletal rearrangement are impaired in Wiskott-Aldrich syndrome protein–deficient lymphocytes. J. Exp. Med. 190:1329–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Badolato, R., S. Sozzani, F. Malacarne, S. Bresciani, M. Fiorini, A. Borsatti, A. Albertini, A. Mantovani, A.G. Ugazio, and L.D. Notarangelo. 1998. Monocytes from Wiskott-Aldrich patients display reduced chemotaxis and lack of cell polarization in response to monocyte chemoattractant protein-1 and formyl-methionyl-leucyl-phenylalanine. J. Immunol. 161:1026–1033. [PubMed] [Google Scholar]
- 9.de Noronha, S., S. Hardy, J. Sinclair, M.P. Blundell, J. Strid, O. Schulz, J. Zwirner, G.E. Jones, D.R. Katz, C. Kinnon, and A.J. Thrasher. 2005. Impaired dendritic-cell homing in vivo in the absence of Wiskott-Aldrich syndrome protein. Blood. 105:1590–1597. [DOI] [PubMed] [Google Scholar]
- 10.Westerberg, L., M. Larsson, S.J. Hardy, C. Fernandez, A.J. Thrasher, and E. Severinson. 2005. Wiskott-Aldrich syndrome protein deficiency leads to reduced B-cell adhesion, migration, and homing, and a delayed humoral immune response. Blood. 105:1144–1152. [DOI] [PubMed] [Google Scholar]
- 11.Klein, C., D. Nguyen, C.H. Liu, A. Mizoguchi, A.K. Bhan, H. Miki, T. Takenawa, F.S. Rosen, F.W. Alt, R.C. Mulligan, and S.B. Snapper. 2003. Gene therapy for Wiskott-Aldrich syndrome: rescue of T-cell signaling and amelioration of colitis upon transplantation of retrovirally transduced hematopoietic stem cells in mice. Blood. 101:2159–2166. [DOI] [PubMed] [Google Scholar]
- 12.Fontenot, J.D., M.A. Gavin, and A.Y. Rudensky. 2003. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat. Immunol. 4:330–336. [DOI] [PubMed] [Google Scholar]
- 13.Fontenot, J.D., J.P. Rasmussen, L.M. Williams, J.L. Dooley, A.G. Farr, and A.Y. Rudensky. 2005. Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity. 22:329–341. [DOI] [PubMed] [Google Scholar]
- 14.Hori, S., T. Nomura, and S. Sakaguchi. 2003. Control of regulatory T cell development by the transcription factor Foxp3. Science. 299:1057–1061. [DOI] [PubMed] [Google Scholar]
- 15.Fontenot, J.D., and A.Y. Rudensky. 2005. A well adapted regulatory contrivance: regulatory T cell development and the forkhead family transcription factor Foxp3. Nat. Immunol. 6:331–337. [DOI] [PubMed] [Google Scholar]
- 16.Coombes, J.L., N.J. Robinson, K.J. Maloy, H.H. Uhlig, and F. Powrie. 2005. Regulatory T cells and intestinal homeostasis. Immunol. Rev. 204:184–194. [DOI] [PubMed] [Google Scholar]
- 17.Sakaguchi, S. 2005. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat. Immunol. 6:345–352. [DOI] [PubMed] [Google Scholar]
- 18.von Boehmer, H. 2005. Mechanisms of suppression by suppressor T cells. Nat. Immunol. 6:338–344. [DOI] [PubMed] [Google Scholar]
- 19.Piccirillo, C.A., and E.M. Shevach. 2004. Naturally-occurring CD4+CD25+ immunoregulatory T cells: central players in the arena of peripheral tolerance. Semin. Immunol. 16:81–88. [DOI] [PubMed] [Google Scholar]
- 20.Nagler-Anderson, C., A.K. Bhan, D.K. Podolsky, and C. Terhorst. 2004. Control freaks: immune regulatory cells. Nat. Immunol. 5:119–122. [DOI] [PubMed] [Google Scholar]
- 21.Powrie, F., M.W. Leach, S. Mauze, L.B. Caddle, and R.L. Coffman. 1993. Phenotypically distinct subsets of CD4+ T cells induce or protect from chronic intestinal inflammation in C. B-17 scid mice. Int. Immunol. 5:1461–1471. [DOI] [PubMed] [Google Scholar]
- 22.Asseman, C., S. Mauze, M.W. Leach, R.L. Coffman, and F. Powrie. 1999. An essential role for interleukin 10 in the function of regulatory T cells that inhibit intestinal inflammation. J. Exp. Med. 190:995–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Groux, H., A. O'Garra, M. Bigler, M. Rouleau, S. Antonenko, J.E. de Vries, and M.G. Roncarolo. 1997. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 389:737–742. [DOI] [PubMed] [Google Scholar]
- 24.Khattri, R., T. Cox, S.A. Yasayko, and F. Ramsdell. 2003. An essential role for Scurfin in CD4+CD25+ T regulatory cells. Nat. Immunol. 4:337–342. [DOI] [PubMed] [Google Scholar]
- 25.Banz, A., A. Peixoto, C. Pontoux, C. Cordier, B. Rocha, and M. Papiernik. 2003. A unique subpopulation of CD4+ regulatory T cells controls wasting disease, IL-10 secretion and T cell homeostasis. Eur. J. Immunol. 33:2419–2428. [DOI] [PubMed] [Google Scholar]
- 26.McHugh, R.S., M.J. Whitters, C.A. Piccirillo, D.A. Young, E.M. Shevach, M. Collins, and M.C. Byrne. 2002. CD4(+)CD25(+) immunoregulatory T cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 16:311–323. [DOI] [PubMed] [Google Scholar]
- 27.Read, S., V. Malmstrom, and F. Powrie. 2000. Cytotoxic T lymphocyte–associated antigen 4 plays an essential role in the function of CD25+CD4+ regulatory cells that control intestinal inflammation. J. Exp. Med. 192:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snapper, S.B., P. Meelu, D. Nguyen, B.M. Stockton, P. Bozza, F.W. Alt, F.S. Rosen, U.H. von Andrian, and C. Klein. 2005. WASP deficiency leads to global defects of directed leukocyte migration in vitro and in vivo. J. Leukoc. Biol. 77:993–998. [DOI] [PubMed] [Google Scholar]
- 29.Thornton, A.M., and E.M. Shevach. 1998. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J. Exp. Med. 188:287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cannon, J.L., and J.K. Burkhardt. 2002. The regulation of actin remodeling during T-cell-APC conjugate formation. Immunol. Rev. 186:90–99. [DOI] [PubMed] [Google Scholar]
- 31.Dustin, M.L. 2005. A dynamic view of the immunological synapse. Semin. Immunol. 17:400–410. [DOI] [PubMed] [Google Scholar]
- 32.Lin, J., M.J. Miller, and A.S. Shaw. 2005. The c-SMAC: sorting it all out (or in). J. Cell Biol. 170:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fontenot, J.D., J.P. Rasmussen, M.A. Gavin, and A.Y. Rudensky. 2005. A function for interleukin 2 in Foxp3-expressing regulatory T cells. Nat. Immunol. 6:1142–1151. [DOI] [PubMed] [Google Scholar]
- 34.Kramer, S., A. Schimpl, and T. Hunig. 1995. Immunopathology of interleukin (IL) 2-deficient mice: thymus dependence and suppression by thymus-dependent cells with an intact IL-2 gene. J. Exp. Med. 182:1769–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Setoguchi, R., S. Hori, T. Takahashi, and S. Sakaguchi. 2005. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J. Exp. Med. 201:723–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thornton, A.M., E.E. Donovan, C.A. Piccirillo, and E.M. Shevach. 2004. Cutting edge: IL-2 is critically required for the in vitro activation of CD4+CD25+ T cell suppressor function. J. Immunol. 172:6519–6523. [DOI] [PubMed] [Google Scholar]
- 37.Thornton, A.M., C.A. Piccirillo, and E.M. Shevach. 2004. Activation requirements for the induction of CD4+CD25+ T cell suppressor function. Eur. J. Immunol. 34:366–376. [DOI] [PubMed] [Google Scholar]
- 38.Sadlack, B., H. Merz, H. Scholrle, A. Schimpi, A. Feller, and I. Horak. 1993. Ulcerative colitis-like disease in mice with a disrupted interleukin-2 gene. Cell. 75:253–261. [DOI] [PubMed] [Google Scholar]
- 39.Foussat, A., F. Cottrez, V. Brun, N. Fournier, J.P. Breittmayer, and H. Groux. 2003. A comparative study between T regulatory type 1 and CD4+CD25+ T cells in the control of inflammation. J. Immunol. 171:5018–5026. [DOI] [PubMed] [Google Scholar]
- 40.Fontenot, J.D., J.L. Dooley, A.G. Farr, and A.Y. Rudensky. 2005. Developmental regulation of Foxp3 expression during ontogeny. J. Exp. Med. 202:901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tang, Q., J.Y. Adams, A.J. Tooley, M. Bi, B.T. Fife, P. Serra, P. Santamaria, R.M. Locksley, M.F. Krummel, and J.A. Bluestone. 2006. Visualizing regulatory T cell control of autoimmune responses in nonobese diabetic mice. Nat. Immunol. 7:83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Molina, I.J., J. Sancho, C. Terhorst, F.S. Rosen, and E. Remold-O'Donnell. 1993. T cells of patients with the Wiskott-Aldrich syndrome have a restricted defect in proliferative responses. J. Immunol. 151:4383–4390. [PubMed] [Google Scholar]
- 43.Apostolou, I., A. Sarukhan, L. Klein, and H. von Boehmer. 2002. Origin of regulatory T cells with known specificity for antigen. Nat. Immunol. 3:756–763. [DOI] [PubMed] [Google Scholar]
- 44.Hogquist, K.A., T.A. Baldwin, and S.C. Jameson. 2005. Central tolerance: learning self-control in the thymus. Nat. Rev. Immunol. 5:772–782. [DOI] [PubMed] [Google Scholar]
- 45.Tang, Q., K.J. Henriksen, E.K. Boden, A.J. Tooley, J. Ye, S.K. Subudhi, X.X. Zheng, T.B. Strom, and J.A. Bluestone. 2003. Cutting edge: CD28 controls peripheral homeostasis of CD4+CD25+ regulatory T cells. J. Immunol. 171:3348–3352. [DOI] [PubMed] [Google Scholar]
- 46.Tai, X., M. Cowan, L. Feigenbaum, and A. Singer. 2005. CD28 costimulation of developing thymocytes induces Foxp3 expression and regulatory T cell differentiation independently of interleukin 2. Nat. Immunol. 6:152–162. [DOI] [PubMed] [Google Scholar]
- 47.Ruemmele, F.M., N. Brousse, and O. Goulet. 2004. Autoimmune enteropathy: molecular concepts. Curr. Opin. Gastroenterol. 20:587–591. [DOI] [PubMed] [Google Scholar]
- 48.Bennett, C.L., J. Christie, F. Ramsdell, M.E. Brunkow, P.J. Ferguson, L. Whitesell, T.E. Kelly, F.T. Saulsbury, P.F. Chance, and H.D. Ochs. 2001. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat. Genet. 27:20–21. [DOI] [PubMed] [Google Scholar]
- 49.Wildin, R.S., F. Ramsdell, J. Peakes, F. Faravelli, J.L. Casanova, N. Buist, E. Levy-Lahad, M. Mazzella, O. Goulet, L. Perroni, et al. 2001. X-linked neonatal diabetes mellitus, enteropathy and endocrinopathy syndrome is the human equivalent of mouse scurfy. Nat. Genet. 27:18–20. [DOI] [PubMed] [Google Scholar]
- 50.Weninger, W., M.A. Crowley, N. Manjunath, and U.H. von Andrian. 2001. Migratory properties of naive, effector, and memory CD8+ T cells. J. Exp. Med. 194:953–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shi, H.N., C.J. Ingui, I. Dodge, and C. Nagler-Anderson. 1998. A helminth- induced mucosal Th2 response alters nonresponsiveness to oral administration of a soluble antigen. J. Immunol. 160:2449–2455. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.