Abstract
Acute appendicitis is the most common presentation of the acute abdomen in the UK. Although in most cases this is an easily reached diagnosis, presentation is not always typical and there are certain other conditions which may mimic appendicitis. Diagnostic adjuncts usually provide the additional information required to make a confident diagnosis; however, in some circumstances, the safest and most reliable course of action is appropriate surgical intervention. A case report is presented of a 43-year-old woman who presented with history of peri-umbilical pain migrating to the right iliac fossa. Following further investigation, with routine blood tests, plain radiographs, ultrasound examination of the abdomen and pelvis, and CT scanning not pointing towards a definitive diagnosis, she eventually underwent a diagnostic laparoscopy which revealed primary omental torsion. An open omentectomy was performed and 2 months on she remains well.
Keywords: Omental torsion, Appendicitis, Omentectomy
Acute appendicitis is the most common presenting condition of the acute abdomen. In the vast majority of cases, the diagnosis is reached on accurate history taking and thorough clinical examination alone without the need of diagnostic adjuncts. Furthermore, if the diagnosis is proving to be troublesome, repeated clinical examination and monitoring of the patient's condition during a period of observation will usually direct the clinician to the correct diagnosis. However, this is not always the case and particular age groups and the sex of the patient may lead to atypical presentations. Blood tests and radiological imaging may provide further clues, but it is only through surgical intervention that confirmation of the diagnosis can be made confidently.
Case report
A 43-year-old woman presented with a 3-day history of peri-umbilical pain which had localised to the right iliac fossa by the time she attended hospital. She described the pain as sharp in nature, constant and was aggravated by movement. She had no bowel or urinary symptoms and no previous abdominal problems. Upon admission, she had a low-grade pyrexia. Examination findings revealed a soft abdomen with tenderness and guarding in the right iliac fossa. There appeared to be a fullness over the tender area, but there was no rebound tenderness and she was Rovsing's sign negative. Urinalysis revealed no abnormality and routine blood tests showed a mild leukocytosis of 12.5 × 109/l (range, 4.0–11.0 × 109/l) with a neutrophilia of 10.5 × 109/l (range. 2.0–7.5 × 109/l). Chest and abdominal radiographs were unremarkable.
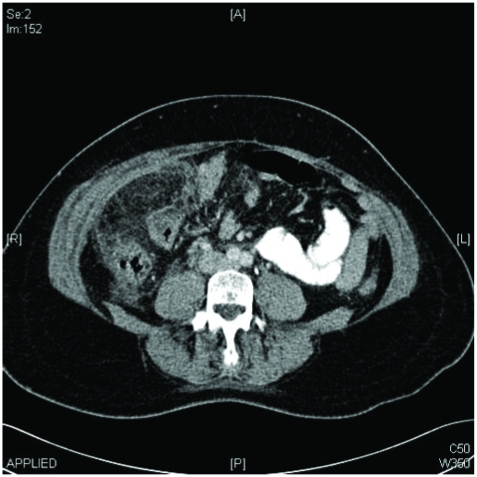
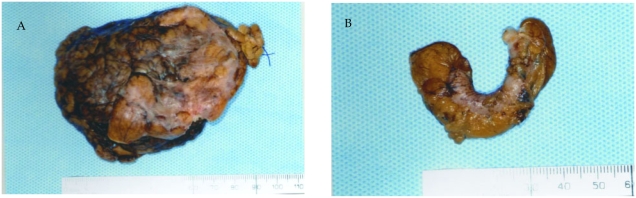
The following morning, she showed a slight improvement with conservative management and a period of observation, although she still had a low-grade pyrexia and was tender on palpation in the right iliac fossa. This was initially thought most likely to be an atypical presentation of appendicitis or an appendicular mass. An ultrasound scan of the abdomen and pelvis demonstrated a minimal amount of fluid in the pelvis. Following a further day of observation, a CT scan was performed which proved to be equivocal, although the possibility of appendicitis and omental torsion was raised (Fig. 1). Further blood testing showed an improvement in the neutrophil count, but she remained tender in the right iliac fossa. As there was no diagnosis reached by day 4, and with no definitive improvement, the decision was made to perform a laparoscopy with a view to undertake an appendicectomy. At laparoscopy, the appendix appeared normal, along with all other major abdominal organs. However, there was a large 8 cm by 7 cm omental mass positioned in the right lower quadrant and a definite point of torsion. Histology confirmed this as a segment of ischaemia omentum. An omentectomy and appendicectomy was performed. Histological analysis proved the surgical specimen to be a segment of ischaemic omentum (Fig. 2A), with a normal appendix (Fig. 2B). She had an uneventful postoperative recovery and 2 months further on remains well.
Figure 1.
Axial CT scan of abdomen showing ‘streaky’ appearance of omentum and extraperitoneal fat.
Figure 2.
(A) Omental specimen. (B) Normal appendix.
Discussion
Acute appendicitis is more common in teenagers and young adults, although not exclusive to this group. With advancing age, it is important to include other pathologies in the list of differentials, albeit, the clinical signs should direct the clinician to the correct diagnosis.
Acute omental torsion is a rare cause of an acute abdomen and can often mimic both appendicitis1 and acute cholecystitis.2 Although first described more than 100 years ago, it still proves to be a diagnostic challenge. It represents an ischaemic condition with some degree of inflammation, which leads to the presence of localised peritonitis. This may be classified as primary, as in the aforementioned case, or secondary, e.g. due to associated lesions such as appendicitis, hernias or neoplasms. The aetiology of primary omental torsion is unclear, although some have suggested obesity and anatomical variants of the omentum to be the cause.3 Precipitating factors related to sudden change of position, abdominal trauma and changes in abdominal compartment pressure, ultimately lead to a displacement of the omentum, which is then under risk of torsion.
As with torsion of any organ, twisting around a focal point leads to a compromise of initially venous, and then arterial blood flow to the omentum. This results in oedema and swelling which causes further compromise of the blood supply. As this disruption progresses, the omentum distal to the point of torsion becomes ischaemic and eventually necrotic. It is the irritation of the overlying peritoneum that leads to the physical signs. If the ischaemic omentum is palpable, it may be mistaken for an appendicular mass, neoplastic lesion or organomegaly. Routine blood tests may not be helpful and at best imply the presence of an inflammatory process. Imaging studies may show specific patterns which are consistent with ischaemic omentum, and there are several reports of a ‘whirling’ appearance of fatty streaks on CT scanning (Fig. 1).4 As CT imaging is becoming more readily available and, therefore, increasingly used as a diagnostic tool in acute abdominal presentation, the incidence of pre-operative diagnosis of omental torsion will no doubt increase. The images, however, can be difficult to interpret, particularly when the axis of rotation is not perpendicular to the transverse plane of scanning, and it is the clinical picture that eventually decides whether surgical intervention is appropriate.
An added difficulty is encountered in the presence of a palpable mass. The traditional treatment of an appendicular mass is an initial conservative approach followed by an elective procedure subsequent to the settling of inflammation. The use of antibiotics and fluids will lead to resolution of the symptoms in most cases, and allow for an interval appendicectomy. This is not appropriate for omental torsion. The natural history of this condition leads to necrotic tissue which necessitates removal at laparotomy or laparoscopy.5
Conclusions
Although there are cases of omental torsion in the literature, they are predominantly in a paediatric population. The authors would like to highlight the potential pitfalls in diagnosing acute abdominal conditions, in particular those which mimic appendicitis, and the resistance to using imaging tools to exclude serious surgical pathology when the diagnosis is uncertain. Ultimately, in many cases, it is only by clinical suspicion and appropriate surgical intervention that a confident diagnosis can be made.
Acknowledgments
Written consent was obtained from the patient to use medical records and images in the publication of this manuscript. The authors have no competing nor financial interests.
References
- 1.Saborido BP, Romero CJ, Medina EM, Calvo AG, Perez PR, Casado OA, et al. Idiopathic segmental infarction of the greater omentum as a cause of acute abdomen: report of two cases and review of literature. Hepatogastroenterology. 2000;48:737–40. [PubMed] [Google Scholar]
- 2.Kimber CP, Westmore P, Hutson JM, Kelly JH. Primary omental torsion in children. J Paediatr Child Health. 1996;32:22–4. doi: 10.1111/j.1440-1754.1996.tb01535.x. [DOI] [PubMed] [Google Scholar]
- 3.Al-Husaini H, Onime A, Oluwole SF. Primary torsion of the greater omentum. J Natl Med Assoc. 2000;92:306–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Kim J, Kim Y, Cho OK, Rhim H, Koh BH, Kim YS, et al. Omental torsion: CT features. Abdom Imaging. 2004;29:502–4. doi: 10.1007/s00261-003-0155-2. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez J, Rosado R, Ramirez D, Medina P, Mezquita S, Gallardo A. Torsion of the greater omentum: treatment by laparoscopy. Surg Laparosc Endosc Percutan Technol. 2002;12:443–5. doi: 10.1097/00129689-200212000-00012. [DOI] [PubMed] [Google Scholar]