Abstract
INTRODUCTION
Hidradenitis suppurativa (HS) is a chronic, inflammatory and suppurative disorder of skin bearing apocrine glands. The most severe complication is squamous cell carcinoma (SCC) and we here present three cases, all of which proved fatal, and review the past 40 years of published cases.
PATIENTS AND METHODS
Three advanced cases of SCC arising in chronic HS have been referred for reconstructive surgery over the past 8 years. Another 28 cases published over the past 40 years were identified using a Medline search (search items in combination: hidradenitis, squamous, carcinoma).
RESULTS
The male:female ratio was 4:1, most (61%) were perineal or buttock. We found no reports of SCC arising in axillary disease. The symptomatic history of HS prior to SCC diagnosis ranged from 3–50 years with a mean of 25 years. Age at diagnosis of SCC ranged from 27–71 years, and 15 patients (48%) died within 2 years of SCC diagnosis.
CONCLUSIONS
We advocate that hidradenitis suppurativa arising in extra-axillary sites is a pre-malignant condition, and should not be treated conservatively; curative resection is the mainstay of management.
Keywords: Squamous cell carcinoma, Hidradenitis suppurativa, Management
We report three cases of squamous cell carcinoma (SCC) arising in hidradenitis suppurativa where there was delayed diagnosis of malignant change. All presented late, and all patients died from their disease. These cases highlight the need for a greater clinical awareness that long-standing buttock and perineal hidradenitis suppurativa is a pre-malignant condition and should not be managed conservatively. We also present a review of all cases published in the English language in the last 40 years of SCC arising in hidradenitis suppurativa.
Case 1
A 50-year-old man was first diagnosed with hidradenitis suppurativa when aged 18 years after the development of an abscess on his buttock. At that time, he was told that this was an incurable condition, and he endured many years of recurrent abscesses. He was referred to the gastroenterologists with peri-anal suppuration who diagnosed Crohn's disease although he had normal small bowel imaging and normal rectal biopsies. Steroids gave no symptomatic relief, and the disease continued to progress. He developed an ulcerated lesion on his right buttock, biopsy of which showed SCC (Fig. 1). Surgery was not considered at this stage. A 6-week course of radiotherapy and chemotherapy followed, which gave moderate symptomatic relief. Eight months later, he developed an SCC in his left buttock, and was referred to our service. The extent of his disease required a radical excision from both buttocks and perineum along with an abdominoperineal resection of the rectum and a groin dissection. The defect was reconstructed with a pedicled rectus abdominis musculocutaneous flap and split skin grafts. Two months later, he developed a recurrence in the other groin and proceeded to a second groin dissection. All excised nodes were positive for SCC metastasis. Nine months later, he developed a recurrence in his right thigh. Investigations showed the tumour involved much of his postero lateral thigh musculature and femur. Local control was achieved by a right hip disarticulation and anterior thigh flap cover. He suffered a further buttock recurrence 4 months later, and died following a rapid deterioration 26 months after diagnosis.
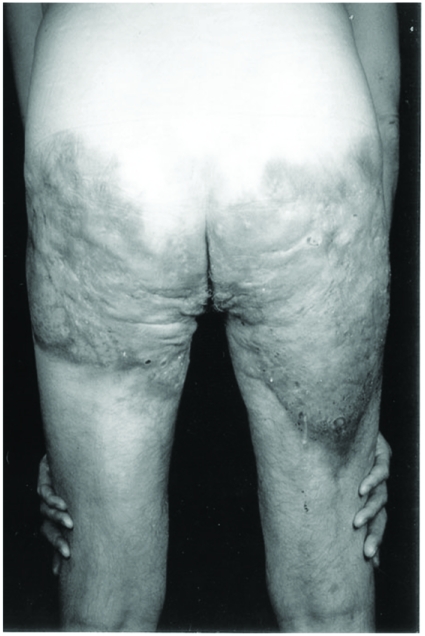
Figure 1.
Case 1 showing very extensive buttock hidradenitis suppurativa. There are ulcerated areas on the medial aspect of each buttock that proved positive for SCC.
Case 2
A 61-year-old woman was referred to the general surgeons with a right groin abscess. The patient gave a 40-year history of hidradenitis, initially confined to her axillae, with her first episode of perineal hidradenitis 10 years previously. In the previous 18 months, she had been troubled with discharge from her perineum. The right groin abscess was incised and 300 ml of pus drained. Further sepsis involving her right vulva and perineum was noted, but no biopsies were taken. The patient was referred for a dermatology opinion. She developed a right iliofemoral vein thrombosis, and was commenced on heparin and warfarin. She was then referred to our service. An examination under anaesthetic was carried out. She had a large fixed mass in the right iliac fossa arising from her pelvis with a very large, deeply fixed sacral ulcer extending anteriorly (Fig. 2), a large ulcer with gross induration of her right vulva extending to the groin, and extensive left groin lymphadenopathy. Multiple biopsies were taken of all affected areas, and a fine needle aspiration of the left groin node. Colonoscopy was normal. All specimens contained SCC. In view of the extent of the disease, surgery would not have been curative, and the patient was offered palliative radiotherapy. She received half of her planned treatment before she died from an episode of sepsis and acute haemorrhage 2 months after diagnosis.
Figure 2.
Case 2 showing a large ulcerated SCC on the sacrum. The tumour extended anteriorly to the perianal region, vulva and groin.
Case 3
A 47-year-old man with a 9-year history of hidradenitis suppurativa affecting both buttocks, groin and peri-anal regions was referred to our service for wide excision and split skin grafting. During the previous 4 years, he had multiple treatments for his abscesses and sinuses. MRI imaging 2 years previously had shown changes that were suspicious, but not diagnostic, of osteomyelitis in his ischial tuberosity. He had developed a large peri-anal ulcer. A biopsy showed SCC. He was also under the care of the orthopaedic surgeons for severe hip pain. An MRI at this stage showed that the tumour had spread extensively and affected his ischial tuberosity, pelvic floor, obturator internus and medial border of gluteus maximus. Given the extensive spread, the tumour was deemed inoperable, and the patient was given palliative chemotherapy and radiotherapy. He died 9 months after SCC diagnosis.
Discussion
Using a search on Medline (search items in combination: hidradenitis, squamous, carcinoma), we reviewed the identified 28 cases published in the past 40 years (Table 1). Out of 31 individual cases (including the three reported here), 15 originated in the buttocks/thigh, nine in the perianal region, four in the perineum, two in the vulva and one arose in the groin.
Table 1.
Reported cases of SCC arising in hidradenitis suppurativa
| Author | Age | Sex | History of HS (years) | Nodes | Surgery performed | Outcome |
|---|---|---|---|---|---|---|
| Case 1 | 50 | M | 32 | + | Abdominoperineal resection | Died at 24 months |
| Case 2 | 61 | F | 40 | + | None | Died at 2 months |
| Case 3 | 47 | M | 9 | + | None | Died at 9 months |
| Rosenzweig et al.1 | 50 | M | 20 | ? | Excision and skin graft | Well at 1 year |
| Bocchini et al.2 | 36 | M | ? | ? | Multiple surgical interventions | Died at 18 months |
| Altunay et al.3 | 54 | M | 30 | + | None | Died at 3 months |
| Manolitsas et al.4 | 52 | F | 30 | ? | Radical local resection | Full recovery |
| Lin et al.5 | 55 | M | 30 | + | Wide excision | Died at 2 months |
| Ritz et al.6 | 61 | M | 45 | + | Radical resection | Died at 4 months |
| Li et al.7 | 68 | M | 50 | ? | Resected | No comment |
| Malaguarnera8 | 65 | M | 20 | + | Radical excision | Died at 7 months |
| Dufresne et al.9 | 52 | F | 36 | + | Mohs micrographic excision | Died at 7 months |
| Shukla et al.10 | 71 | F | 50 | ? | Massive resection | Symptom-free at 4 years |
| Perez-Diaz et al.11 | 60 | M | 25 | + | Completely excised | Disease-free at 1 year |
| Welsh et al.12 | 50 | M | 20 | + | Incomplete resection | Died at 2 months |
| Mendonca et al.13 | 57 | M | 35 | − | Wide excision and skin graft | Well at 1 year |
| Williams et al.14 | 27 | M | 11 | − | Wide local excision | Well at 1 year |
| Anstey et al.15 | 67 | M | 40 | ? | Massive resection | Died at 2 years |
| Weber et al.16 | 48 | F | 37 | − | En bloc dissection | No comment |
| Chicarilli17 | 59 | M | 30 | ? | Massive resection | Disease-free at 2 years |
| Zachary et al.18 | 55 | M | 3 | ? | Radical excision | Disease-free at 1 year |
| Sparks et al.19 | 35 | M | 10 | + | None | Died |
| Johnston et al.20 | 54 | M | 4 | ? | Wide resection | Died at 6 months |
| Mora et al.21 | 47 | M | 5 | ? | Abdominoperineal resection | Disease-free at 2 years |
| Mora et al.21 | 54 | M | Many | ? | None | Died at 5 months |
| Blacket et al.22 | 44 | M | 21 | ? | Radical excision | Died at 2 years |
| Gordon23 | 28 | F | 17 | + | Wide local excision | No comment |
| Thornton et al.24 | ? | ? | 20 | ? | No comment | No comment |
| Alexander25 | 40 | M | 20 | − | Abdominoperineal resection | Died at 18 months |
| Humphrey et al.26 | 48 | M | 8 | + | Radical excision | Alive – unknown follow-up time |
| Donsky et al.27 | 44 | M | 23 | ? | Radical excision | No comment |
HS, hidradenitis suppurativa.
Although the cases are limited in their reported followup, 15 patients (48%) died within 2 years of SCC diagnosis. The age at diagnosis of SCC ranged from 27–71 years with a mean of 51 years. The symptomatic history of hidradenitis suppurativa prior to SCC diagnosis ranged from 3–50 years with a mean of 25 years.
The male:female ratio was 24:6 with one case unknown. This is in keeping with the finding that although hidradenitis suppurativa overall is more prevalent in women, the incidence of extra-axillary disease is much more common in men.10 We found no reports of SCC arising in axillary disease. Of the 13 cases (42%) with positive nodes at SCC diagnosis in which outcome at 2 years is known, only one patient was still alive.11
A common theme in the reported cases is multiple minor surgical interventions, under different specialists, over months or years prior to a diagnosis of SCC. The three cases we present are notable for the delayed histological diagnosis, and thus advanced stage at referral to our service. As radical surgery can be curative, they serve as a pertinent reminder of the importance of early histological diagnosis, either by incision or excision biopsies, in all non-healing or otherwise suspicious lesions in chronic hidradenitis suppurativa.
Conclusions
We advocate that hidradenitis suppurativa arising in extra-axillary sites is a pre-malignant condition, and should not be treated conservatively; curative resection is the mainstay of management.
References
- 1.Rosenzweig MD, Brett AS, Lefaivre J, Vandersteenhoven JJ. Hidradenitis suppurativa complicated by squamous cell carcinoma and paraneoplastic neuropathy. Am J Med Sci. 2005;329:150–2. doi: 10.1097/00000441-200503000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Bocchini SF, Habr-Gama A, Desidério R, Imperiale AR, Araujo S. Gluteal and perineal hidradenitis suppurativa. Surgical treatment by wide excision. Dis Colon Rectum. 2003;46:944–9. doi: 10.1007/s10350-004-6691-1. [DOI] [PubMed] [Google Scholar]
- 3.Altunay IK, Gökdemir G, Kurt A, Kayaoglu S. Hidradenitis suppurativa and squamous cell carcinoma. Dermatol Surg. 2002;28:88–90. doi: 10.1046/j.1524-4725.2002.01090.x. [DOI] [PubMed] [Google Scholar]
- 4.Manolitsas T, Biankin S, Jaworski R, Wain G. Vulval squamous cell carcinoma arising in chronic hidradenitis suppurativa. Gynecol Oncol. 1999;75:285–8. doi: 10.1006/gyno.1999.5547. [DOI] [PubMed] [Google Scholar]
- 5.Lin M, Breiner M, Fredricks S. Marjolin's ulcer occurring in hydradenitis suppurativa. Plast Recon Surg. 1999;103:1541–3. doi: 10.1097/00006534-199904050-00046. [DOI] [PubMed] [Google Scholar]
- 6.Ritz J, Runkel N, Haier J, Buhr H. Extent of surgery and recurrence rate of hidradenitis suppurativa. Int J Colored Dis. 1998;13:164–8. doi: 10.1007/s003840050159. [DOI] [PubMed] [Google Scholar]
- 7.Li M, Hunt M, Commens C. Hidradenitis suppurativa, Dowling Degos disease and perianal squamous cell carcinoma. Aust J Dermatol. 1997;38:209–11. doi: 10.1111/j.1440-0960.1997.tb01700.x. [DOI] [PubMed] [Google Scholar]
- 8.Malaguarnera M. Squamous cell cancer in Verneuil's disease (hidradenitis suppurativa) Lancet. 1996;348:1449. doi: 10.1016/S0140-6736(04)70093-8. [DOI] [PubMed] [Google Scholar]
- 9.Dufresne R, Ratz J, Bergfeld W, Roenigk R. Squamous cell carcinoma arising from the follicular occlusion triad. J Am Acad Dermatol. 1996;35:475–7. doi: 10.1016/s0190-9622(96)90632-5. [DOI] [PubMed] [Google Scholar]
- 10.Shukla V, Hughes L. A case of squamous cell carcinoma complicating hidradenitis suppurativa. Eur J Surg Oncol. 1995;21:106–9. doi: 10.1016/s0748-7983(05)80084-8. [DOI] [PubMed] [Google Scholar]
- 11.Pérez-Diaz D, Calvo-Serrano M, Mártinez-Hijosa E, Fuenmayor-Valera L, Munoz-Jimnez F, Turégano-Fuentes F, et al. Squamous cell carcinoma complicating perianal hidradenitis suppurativa. Int J Colorect Dis. 1995;10:225–8. doi: 10.1007/BF00346224. [DOI] [PubMed] [Google Scholar]
- 12.Welsh D, Powers J. Elevated parathyroid hormone-related protein and hypercalcaemia in a patient with cutaneous squamous cell carcinoma complicating hidradenitis suppurativa. South Med J. 1993;86:1403–4. doi: 10.1097/00007611-199312000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Mendonça H, Rebelo C, Fernandes A, Lino A, Garcia-e-Silva L. Squamous cell carcinoma arising in hidradenitis suppurativa. J Dermatol Surg Oncol. 1991;17:830–2. doi: 10.1111/j.1524-4725.1991.tb03269.x. [DOI] [PubMed] [Google Scholar]
- 14.Williams S, Busby R, DeMuth R, Nelson H. Perineal hidradenitis suppurativa: presentation of two unusual complications and a review. Ann Plast Surg. 1991;26:456–62. [PubMed] [Google Scholar]
- 15.Anstey A, Wilkinson J, Lord P. Squamous cell carcinoma complicating hidradenitis suppurativa. Br J Dermatol. 1990;123:527–31. doi: 10.1111/j.1365-2133.1990.tb01460.x. [DOI] [PubMed] [Google Scholar]
- 16.Weber L, Kantor G, Bergfeld W. Reticulate pigmented anomaly of the flexures (Dowling Degos disease): a case report associated with hidradenitis suppurativa and squamous cell carcinoma. Cutis. 1990;45:446–50. [PubMed] [Google Scholar]
- 17.Chicarilli Z. Follicular occlusion triad: hidradenitis suppurativa, acne conglobata, and dissecting cellulites of the scalp. Ann Plast Surg. 1987;18:230–7. doi: 10.1097/00000637-198703000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Zachery L, Robson M, Rachmaninoff N. Squamous cell carcinoma occurring in hidradenitis suppurativa. Ann Plast Surg. 1987;18:71–3. doi: 10.1097/00000637-198701000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Sparks M, Kuhlman D, Prieto A, Callen J. Hypercalcaemia in association with cutaneous squamous cell carcinoma. Arch Dermatol. 1985;121:243–6. [PubMed] [Google Scholar]
- 20.Johnston W, Miller T, Frileck S. Atypical pseudoepitheliomatous hyperplasia and Squamous cell carcinoma in chronic cutaneous sinuses and fistulas. Plast Recon Surg. 1980;66:395–9. [PubMed] [Google Scholar]
- 21.Mora R, Perniciaro C. Cancer of the skin in blacks. I. A review of 163 black patients with cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1981;5:535–43. doi: 10.1016/s0190-9622(81)70113-0. [DOI] [PubMed] [Google Scholar]
- 22.Black S, Woods J. Squamous cell carcinoma complicating hidradenitis suppurativa. J Surg Oncol. 1982;19:25–6. doi: 10.1002/jso.2930190108. [DOI] [PubMed] [Google Scholar]
- 23.Gordon S. Squamous cell carcinoma arising in hidradenitis suppurativa. Plast Recon Surg. 1977;60:800–2. doi: 10.1097/00006534-197711000-00027. [DOI] [PubMed] [Google Scholar]
- 24.Thornton J, Abcarian H. Surgical treatment of perianal and perineal hidradenitis suppurativa. Dis Colon Rectum. 1978;21:573–7. doi: 10.1007/BF02586399. [DOI] [PubMed] [Google Scholar]
- 25.Alexander S. Squamous cell carcinoma in chronic hydradenitis suppurativa. Cancer. 1979;43:745–8. doi: 10.1002/1097-0142(197902)43:2<745::aid-cncr2820430251>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 26.Humphrey L, Playforth H, Leavell U. Squamous cell carcinoma arising in hidradenitis suppurativum. Arch Dermatol. 1969;100:59–62. [PubMed] [Google Scholar]
- 27.Donsky H, Mendelson C. Squamous cell carcinoma as a complication of hidradenitis suppurativa. Arch Dermatol. 1964;90:488–91. doi: 10.1001/archderm.1964.01600050036008. [DOI] [PubMed] [Google Scholar]