Abstract
The mechanism of heat transduction in vertebrate sensory neurons was investigated in vitro by using cultured dorsal root ganglion neurons from adult rat. In response to a physiologically relevant range of stimulus temperatures (23–45°C), a subpopulation of small dorsal root ganglion neurons are depolarized by a cation current (heat-activated current, Iheat) that is antagonized by extracellular cesium. Heat-induced single-channel currents in cell-attached patches are evoked at a similar range of temperatures. Iheat is a calcium-dependent current activated indirectly by heat-evoked release of calcium from intracellular stores. This suggests that the channel itself is not the transducer of thermal energy. Similar to nociceptive heat sensation in vivo, Iheat is enhanced by the hyperalgesic agent prostaglandin E2 and only partially adapts during prolonged heat stimuli. To our knowledge, these data provide the first demonstration that ion channels can mediate heat transduction in mammalian sensory neurons and provide evidence that heat causes the channels to open via an increase in the intracellular second messenger calcium.
Keywords: somatosensory transduction, primary afferent, pain, temperature
The mechanism of stimulus transduction is a fundamental issue in understanding any sensory system. However, investigation of transduction mechanisms in sensory nerves has been impeded by the inaccessibly small size of the receptive endings in vivo and the lack of a suitable in vitro model. We hypothesized that heat transduction mechanisms of thermosensitive nerve endings would be expressed in isolated dorsal root ganglion (DRG) neuron cell bodies in vitro, as are a variety of other properties associated with nociceptive nerve fibers in vivo (1–3). The possibility that heat activates a nonselective cation channel in rat sensory neurons is suggested by a report that heat evokes a nonselective cation current in neonatal rat sensory neurons (4) and by our observation that heat can stimulate transmembrane influx of cobalt ions into these neurons (5).
MATERIALS AND METHODS
Lumbar DRGs were dissected from adult male Sprague–Dawley rats (Charles River Breeding Laboratories) and incubated 2 hr at 37°C in 0.125% collagenase type IV (Sigma), followed by 10 min in 0.25% trypsin (Sigma). After addition of trypsin inhibitor at 100 μg/ml, ganglia were triturated, plated onto glass coverslips coated with laminin and poly(d-ornithine), and incubated at 37°C in 3% CO2/97% air.
Recordings were performed in a chamber perfused rapidly with bath containing 130 mM NaCl, 3 mM KCl, 2.5 mM CaCl2, 10 mM Hepes, and 10 mM glucose, pH 7.4, 320 milliosmolar (mOsM). Electrodes (1–10 MΩ) contained 55 mM K2SO4, 2 mM NaCl, 2 mM MgCl2, 1 mM CaCl2, 11 mM EGTA, and 10 mM Hepes, pH 7.1, 310 mOsM. To facilitate adequate control of membrane voltage, all voltage-clamp data shown were obtained from neurons between 12 and 28 hr after plating, when no neurites are visible. After the first day in culture, as the cells developed and extended neurites, heat-evoked currents became progressively larger (data not shown). Neurons were voltage clamped at −65 mV, near their resting potential.
Temperature of the entire contents of the recording chamber is controlled by heating and cooling the extracellular solution flowing into the chamber. Immediately before entering the chamber, solution flows over the face of a Peltier thermoelectric device. The rapid exchange of solution in the chamber (2 ml/min flows into the 0.5-ml chamber) permits temperature changes up to 5°C per sec. Temperature in the bath is measured with a miniature thermocouple (response time constant = 5 msec; Physitemp, Clifton, NJ) placed within 1 mm of the cell being studied. Between stimulus applications the chamber was maintained at room temperature (21–23°C). All drugs were bath-applied through the perfusion/heating apparatus. Heat stimuli above 50°C were not routinely employed since they can cause abrupt and irreversible loss of the transmembrane potential. Decreases in pH induced by the heat stimuli were insufficient to evoke proton-induced currents in these cells (data not shown). Data are expressed as the mean ± SEM.
The current–voltage relation for the heat-activated current (Iheat) was determined by a voltage ramp protocol in which the neuron was heated, the membrane potential was stepped to +60 mV for 50 msec to reduce inactivating currents, and the membrane potential was then ramped from +60 mV to −75 mV over a 250-msec period. Leak current was determined by the same voltage protocol applied after recovery from the heat stimulus. La3+ (100 μM) was present in the bath throughout the experiment to suppress voltage-gated calcium currents.
For cell-attached patch single-channel recordings, cells were prepared as described for whole-cell recording. Single-channel recordings were performed 12–36 hr after plating in cells less than 35 μm to maximize the possibility of observing heat-activated channels. The bath solution was the same that was employed in whole-cell experiments, and the electrode contained a solution identical to the bath solution but osmolarity was adjusted to 310 mOsM. To minimize electrical interference, the Peltier device was not used; instead, heat stimuli were delivered by switching to bath from a preheated resevoir. Patches were voltage-clamped at 0 mV relative to the reference electrode in the bath, and a resting membrane potential of −60 mV was assumed for calculation of conductance. Data were sampled at 10 kHz and digitally filtered at 2 kHz.
For calcium fluorimetry, DRG neurons were prepared as described above for electrophysiology, and the same recording chamber, heating device, and extracellular solution were used. Neurons were loaded 10 min in 1 μM fura-2 acetoxymethyl ester (Molecular Probes) at room temperature. To allow for more complete deesterification of the dye, the cells remained at least 20 min in fura-free solution before recordings began. To measure the intracellular concentration of free calcium ions ([Ca2+]i) in neurons, digital imaging of fura-2 fluorescence was performed by using an intensified charge-coupled device camera. DRG neurons have phase-bright round cell bodies that are easily distinguished from nonneuronal cells. Background-subtracted spatially averaged single-cell ratiometric values were calculated and recorded. Background fluorescence was obtained from a cell- and debris-free region of the coverslip close to the cells studied. Autofluorescence in these cells is low and was not corrected. For each wavelength, eight frames were averaged, and pairs of images were collected less than 500 msec apart every 1.5 sec. At the end of each experiment, intracellular calibration of maximum and minimum fluorescence ratios, and a test of sensitivity to Mn2+ quenching was performed.
RESULTS
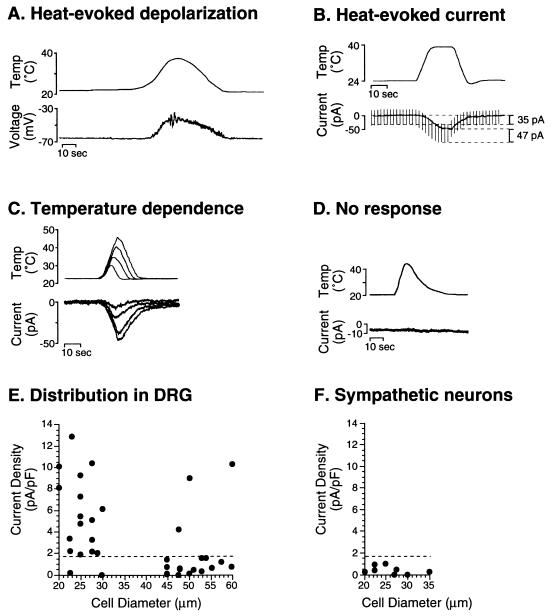
Whole-cell recordings were performed on cultured adult rat DRG neurons, and heat stimuli were delivered by rapidly heating the extracellular solution. Whole-cell current clamp recordings demonstrated that heat stimulation can depolarize DRG neurons (Fig. 1A). In voltage clamp, a heat-evoked current (Iheat) was observed that was associated with a decrease in input resistance (Fig. 1B) and often with an increase in whole-cell noise (see, for example, Fig. 2B), suggesting that the current is caused by opening of ion channels in the plasma membrane. The magnitude of Iheat depended on the intensity of the heat stimulus within a range of temperatures encountered physiologically (Fig. 1C). That some DRG neurons express little or no Iheat (Fig. 1D) suggests that the current is not an artifact of the recording method or a nonspecific effect of heat on, for example, cell membranes.
Figure 1.
Heat-evoked depolarizing inward current in a subpopulation of cultured DRG neurons. (A) In a neuron current-clamped at 0 pA, heating to 39°C caused a depolarization from −66 mV to −35 mV. (B) A neuron voltage-clamped at −65 mV responded to heat with an inward current (Iheat). Input resistance decreased during Iheat; the current required to deliver a −20-mV 10-msec voltage step command increased from 35 pA before heating to 47 pA during heat, indicating a decrease in input resistance of approximately 25%. (C) The magnitude of Iheat is progressively larger as the peak stimulus temperature increases. This cell was heated to peak stimulus temperatures of approximately 30, 35, 40, and 45°C. (D) Some DRG neurons exhibit no detectable response to heat, as in this neuron heated to 45°C. (E) Expression of Iheat is greatest in small-diameter neurons. The response to a 40°C stimulus was measured in small-diameter (≤28 μm) and large-diameter (≥45 μm) DRG neurons. The magnitude of Iheat increases markedly over time during the first 24 hr neurons are maintained in culture (data not shown). Therefore, to study the distribution of Iheat among DRG neurons of different sizes, recordings were performed only between 12 and 18 hr after cell plating, in a sequence that strictly alternated between small- and large-diameter DRG neurons. Data were obtained from cells isolated from six rats. To correct for different membrane areas in different-sized neurons, current density was calculated based on the whole-cell capacitance. Most small-diameter neurons exhibit Iheat of greater than 1.75 pA/pF (broken line) and most large-diameter neurons exhibit Iheat of less than 1.75 pA/pF. (F) The response to a 40°C stimulus was measured in sympathetic neurons isolated from the superior cervical ganglion. All neurons tested responded with an inward current of less than 1.75 pA/pF.
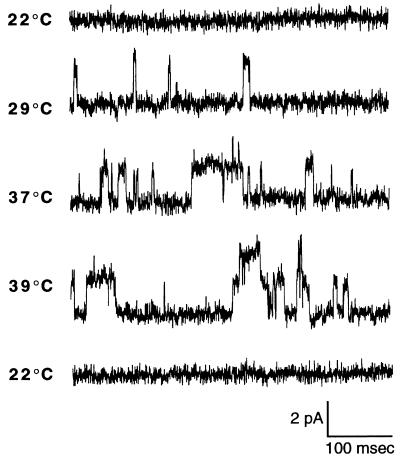
Figure 2.
Heat activates single-channel currents in rat dorsal root ganglion neurons. Cell-attached patch recordings were performed with the electrode voltage clamped at 0 mV. No single-channel activity was observed at 22°C. Upon heating the bath, brief single-channel inward currents began to appear at approximately 29°C. At 37°C, channel openings became more frequent and longer in duration. At 39°C, openings of a second heat-activated channel became more frequent. Both heat-activated single-channel currents in this patch exhibited a similar amplitude of approximately 2 pA. If a resting potential of −60 mV is assumed, this would reflect a single-channel conductance of 33 pS. Finally, subsequent cooling of the bath to 22°C caused single-channel activity to cease.
In the rat in vivo, heat-evoked activity is observed only in the subpopulation of C-fiber primary afferent nociceptors (6). We investigated whether there is a similar selective expression of Iheat in vitro. Because there is a correlation both in vivo and in vitro between small cell body diameter and expression of nociceptor-related properties (2, 7), we measured Iheat in small- and large-diameter neurons. To quantitatively compare expression of Iheat between different neurons, the current amplitude was normalized to membrane surface area (estimated by whole-cell capacitance). A standard stimulus temperature of 40°C was used to evoke relatively large currents in these DRG neurons grown in culture less than 24 hr, while remaining well below temperatures (above approximately 50°C) that consistently damage most neurons. As shown in Fig. 1E, the mean peak current density of Iheat evoked by a 40°C stimulus in small-diameter DRG neurons (≤28 μm) was 5.3 ± 0.9 pA/pF (n = 18) and in large-diameter neurons (≥45 μm) was 1.8 ± 0.7 pA/pF (n = 19). Thus, Iheat was significantly larger (P = 0.002) in small-diameter neurons compared with that in large-diameter neurons.
To determine whether Iheat is a distinctive property of sensory neurons, heat responses were measured in neurons isolated from the superior cervical ganglion. These peripheral sympathetic neurons have no known thermoreceptive function. These neurons exhibited small heat-evoked currents similar in magnitude to those of the poorly responsive large-diameter DRG neurons (Fig. 1F). The mean current density of Iheat in sympathetic neurons was 0.53 ± 0.17 pA/pF (n = 8).
Like other enzymes, ion channels exhibit temperature-dependent kinetics (8). Such a temperature-dependent shift in channel kinetics has been suggested as an explanation for cold-evoked activity in sensory neurons in which an oscillating membrane potential causes continual activation and inactivation of voltage- and calcium-dependent currents (9). However, a similar mechanism is inadequate to explain Iheat since, as illustrated in Fig. 1, the membrane potential and transmembrane current of these neurons is stable before and after heat stimulation. Therefore, based on our observation of voltage-clamped currents evoked by heat, we hypothesized that heat does not depolarize DRG neurons by simply altering kinetics of channels that have already been activated but instead causes closed ion channels to open.
To test the hypothesis that heat opens ion channels in rat sensory neurons, we performed cell-attached patch single-channel recordings. To determine unequivocally whether heat can cause closed channels to open, only “silent” patches that exhibited no ongoing single-channel activity at room temperature were tested for responses to heat. In 5 of 15 silent patches examined, heating to approximately 40°C caused channels to open. As illustrated in Fig. 2, channel openings became more frequent and had a longer duration at higher temperatures. The heat-activated channels exhibited similar open-channel conductance amplitudes of 34.8 ± 0.6 pS (n = 7), suggesting that only a single species of channel is activated by heat.
To characterize the channel that mediates Iheat, we investigated ion selectivity and voltage dependence of the current. When all Na+ was removed from the extracellular bath (substituted with choline), the peak amplitude of Iheat was reduced by 85 ± 7% (n = 5), suggesting that Na+ is the principal charge carrier (Fig. 3A). In addition, removing extracellular Ca2+ reduced Iheat by 21 ± 9% (n = 7; Fig. 3B). These observations are consistent with the channel being a sodium- and calcium-permeable nonselective cation channel. Investigation of the voltage dependence of Iheat (Fig. 3C) revealed that the current has a negative reversal potential that suggests further that the cation channel may be permeable to potassium ions. The current–voltage relation also exhibits outward rectification, with decreasing slope conductance at potentials more negative than the reversal potential.
Figure 3.
Characteristics of the Iheat current. (A) Iheat was reduced by 67% in this DRG neuron when extracellular Na+ was substituted by choline. (B) Iheat was reduced by 37% in another DRG neuron when Ca2+ was removed from the extracellular solution. (C) At 10 mM, extracellular Cs+ reduced Iheat in this neuron by 85%. Iheat recovered nearly to control levels within 2 min after removal of Cs+. (D) La3+ (100 μM) does not reduce Iheat. (E) A plot of leak-subtracted Iheat during a voltage ramp shows outward rectification at membrane potentials more negative than approximately −40 mV. (Inset) Protocol in which a voltage ramp is applied at the peak of the response to a 38°C stimulus (ramp 1), and leak current is measured by the same ramp applied after recovery from the stimulus (ramp 2).
In addition to its relatively unusual voltage dependence (10, 11), the profile of sensitivity of Iheat to channel-blocking agents suggests that the current is mediated by a novel cation channel. Thus, Iheat was not significantly reduced by agents that block a variety of nonselective cation channels (12), including lanthanum (100 μM; n = 5; Fig. 3D), as well as cobalt (2.5 μM, n = 4), nickel (5 mM, n = 2), magnesium (2.5 μM, n = 7), and gadolinium (100 μM, n = 4) (data not shown). Iheat was also not significantly reduced by agents that block ligand- and voltage-gated cation channels in DRG neurons, including the N-methyl-d-aspartate receptor blocker MK-801 (10 μM, n = 4), the acetylcholine receptor blocker hexamethonium (10 μM, n = 3), the capsaicin receptor blocker (13) ruthenium red (100 μM; n = 4), the competitive antagonist of capsaicin receptors (14) capsazepine (10 μM; n = 4), and the sodium channel blocker tetrodotoxin (10 μM, n = 6) (data not shown).
On the other hand, one agent that reduces Iheat was identified: cesium (Cs+). At 5 mM, Cs+ in the extracellular solution reduced Iheat by 62 ± 9% (n = 7), and at 10 mM, Cs+ reduced Iheat by 89 ± 2% (n = 6; Fig. 3E). The block by Cs+ was rapidly reversible (Fig. 3E). The identification of Cs+ as a reversible antagonist of Iheat provides a useful pharmacological tool for study of the current and distinguishes it from most other currents. Other currents blocked by extracellular cesium are easily distinguished from Iheat; the Cs+-sensitive nonselective cation channel expressed in DRG neurons (15), designated Ih, is distinguished from Iheat by the hyperpolarization-dependent activation of Ih that is incompatible with the outward rectification exhibited by Iheat. Similarly, the inward rectifier potassium-selective current is also blocked by extracellular Cs+ (16), but this outward current is obviously distinct from the inward Iheat current.
Heat might cause the Iheat channel to open by either direct or indirect mechanisms. Indirect gating, involving a second messenger, was suggested by our occasional observation of Iheat currents that do not recover immediately to prestimulus baseline after the end of the heat stimulus; instead, such responses exhibit a second slower phase of recovery in which the current decreases over a period of several seconds. This phenomenon is reproducible within a single neuron. Such a slowly recovering response is shown in Fig. 4A. We tested the hypothesis that activation of Iheat depends on increases in intracellular [Ca2+] by measuring the effect of increased intracellular buffering of Ca2+ by the Ca2+ chelator 1,2-bis(2-aminophenoxy)ethane-N,N,N′,N′-tetraacetic acid acetoxymethyl ester (BAPTA-AM; Fig. 4A). In neurons loaded with 100 μM BAPTA-AM, the heat-evoked current was reduced by 63% ± 4% (n = 5) compared with pre-BAPTA-AM controls, suggesting that heat activates Iheat by increasing [Ca2+]i. BAPTA vehicle (0.1% dimethyl sulfoxide/0.025% pluronic acid) had no significant effect on the amplitude of Iheat (n = 5).
Figure 4.
Iheat is activated by calcium released from intracellular stores. (A) Loading cells with the calcium chelator BAPTA reduces Iheat. Iheat was evoked in a neuron by heating to 40°C (Control), then the neuron was exposed to a bath containing 100 μM BAPTA-AM for 5 min at room temperature, BAPTA-AM was washed out of the bath, and the stimulus was reapplied (BAPTA). In this neuron, BAPTA reduced the peak Iheat by 78%. The control response of this neuron also illustrates that in some neurons, Iheat does not return to baseline (broken line) immediately upon cessation of the heat stimulus. (B) Heat stimulates [Ca2+]i increases in the absence of extracellular Ca2+. Heating to 40°C caused [Ca2+]i to increase by approximately 200 nM. Removal of Ca2+ from the extracellular bath completely blocked Ca2+ entry evoked by K+ depolarization but the heat-evoked increase in [Ca2+]i persisted.
To determine directly whether heat can stimulate increases in [Ca2+]i in sensory neurons and to determine the source of Ca2+ ions, we measured the effect of heat on [Ca2+]i by fura-2 fluorimetric imaging. Heat caused increases in [Ca2+]i, and these [Ca2+]i increases could be evoked in the absence of extracellular Ca2+ (Fig. 4B), suggesting that heat causes the release of Ca2+ from intracellular stores. In six cells tested, the heat-evoked [Ca2+]i increase, in the absence of extracellular Ca2+, was 87 ± 9% of the increase in the presence of Ca2+. This observation and the electrophysiological characterization of Iheat strongly suggest that transduction of heat stimuli by rat sensory neurons occurs by heat-stimulated release of Ca2+ from intracellular stores with subsequent activation of a calcium-dependent nonselective cation channel. To our knowledge, heat-evoked release of Ca2+ from intracellular stores in neurons has not been reported previously. However, our observations might explain a previous report that the ability of caffeine to elevate [Ca2+]i in avian sensory neurons is reduced by prolonged exposure to similar elevated temperatures (17).
In addition to the finding that Iheat is activated at a physiologically relevant range of temperatures, further electrophysiological characterization of Iheat revealed other aspects of the current that resemble heat transduction by sensory nerves in vivo. (i) During a prolonged constant heat stimulus, the magnitude of Iheat reaches a peak and then decreases to a stable plateau level (Fig. 5A); adaptation was observed in eight of eight DRG neurons that were tested for adaptation to various holding temperatures ranging from 38 to 48°C (data not shown). (ii) As shown in Fig. 5B, after a 5-min exposure to the inflammatory mediator, prostaglandin E2 (PGE2; 10 nM), in a subset of neurons (four of seven) the magnitude of Iheat was increased by 61 ± 11% compared with predrug trials. In contrast, in three of seven neurons, the change in current magnitude was less than 5% (−0.6 ± 1.6%), and application of vehicle caused no significant change in Iheat (0.8 ± 1.1%; n = 5). The effect of PGE2 was tested only in small-diameter (<35 μm) neurons because expression of Iheat is greater in these cells and because PGE2-induced electrical hyperexcitability is most common in small-diameter neurons (2). In vivo PGE2 causes heat hyperalgesia and sensitizes the responses of sensory nerve fibers to heat stimuli (18, 19).
Figure 5.
Iheat exhibits properties consistent with heat transduction in vivo. (A) Magnitude of Iheat adapts to maintained stimuli. In a neuron heated to approximately 43°C for about 2 min, Iheat reached a peak during the first minute and then decayed to a plateau level of about 50% of peak for the remainder of the stimulus. (B) PGE2 enhances Iheat. PGE2 (10 nM) was perfused through the recording chamber for 10 min. Within 1 min after the beginning of wash-out of PGE2, the 43°C stimulus was reapplied. In this neuron, the peak amplitude of Iheat after exposure to PGE2 was 192% of the control value obtained before PGE2.
DISCUSSION
We conclude that, in small-diameter sensory neurons isolated from adult rat, heat stimuli are transduced by a calcium-dependent nonselective cation current (Iheat). That Iheat is mediated by ion channels rather than by membrane damage is suggested by the following observations: (i) the amplitude and time course (including recovery) of Iheat currents in single neurons are highly reproducible, (ii) Iheat is largely blocked by extracellular cesium ions, (iii) Iheat exhibits a nonlinear current–voltage relation, (iv) Iheat is preferentially expressed in small-diameter DRG neurons vs. large-diameter DRG neurons and vs. small-diameter sympathetic neurons, (v) Iheat is enhanced by PGE2, and (vi) small-diameter DRG neurons express ion channels that are opened by heat in the same temperature range that Iheat is activated and that exhibit a fixed single-channel conductance regardless of temperature.
That a single type of inward current predominantly underlies Iheat is supported by the observations that heat-evoked single-channel currents observed are of similar amplitude and that the whole-cell current is largely blocked by extracellular Cs+ or by intracellular BAPTA. We conclude that the ion channel that underlies Iheat is a nonselective cation channel because its reversal potential is inconsistent with its being a channel selective for sodium, potassium, calcium, or chloride. The Iheat channel might be a previously undescribed channel since the combination of it’s susceptibility to block by cesium, insensitivity to a wide range of other blockers of nonselective cation channels, and current–voltage relation are, to our knowledge, unique.
Our observations show that activation of Iheat requires increases in [Ca2+]i and suggest that the principal source of Ca2+ is heat-releasable intracellular stores. Therefore, it is likely that the channel itself is not a transducer of thermal energy but instead that energy transduction occurs at a point upstream to the calcium-dependent activation of the channel. It will be of interest to characterize this store and to study the mechanism by which heat mobilizes it. Ca2+ released from the store might activate Iheat by either a direct action on the channel or an indirect action via Ca2+-activated intracellular second messenger pathways. A heat-activated current in DRG neurons from neonatal rat was recently reported (4). Although that nonselective cation current appears similar to Iheat, the cellular distribution of that current, the means by which heat activates it, and the possibility that the current was mediated by an ion channel were not investigated.
In support of the idea that Iheat mediates heat transduction in vivo, Iheat is preferentially expressed in the subpopulation of cultured DRG neurons that, based on their small cell body size, are presumed to be neurons that gave rise to nociceptors in vivo. Heat-sensitive nerve fibers in the rat in vivo are almost exclusively nociceptors (6, 20). In addition, a connection between Iheat and in vivo thermal transduction is strengthened by our observation that the current is enhanced by PGE2. In vivo, PGE2 sensitizes heat-evoked responses of nociceptive sensory nerve fibers and induces thermal hyperalgesia (18). Thus, PGE2-induced enhancement of Iheat might contribute to inflammation-induced heat hyperalgesia [in concert with PGE2-induced enhancement of voltage-dependent currents in these cells (21–24)]. Finally, our observation that in the presence of sustained heat stimulation Iheat adapts to a maintained amplitude is consistent with maintained responses of sensory nerve fibers to sustained heat.
Iheat is a second-messenger-activated nonselective cation channel involved in sensory transduction. We suggest that the Iheat channel might be related to the cyclic nucleotide-gated channels that are involved in visual and olfactory transduction. In particular, the similar nonlinear voltage dependence (in the presence of extracellular Ca2+) shared by Iheat and olfactory transduction currents (25) and the observation of impaired heat responsiveness in Caenorhabditis elegans lacking the cyclic nucleotide-gated channel (26) suggest an important relationship between the two channels. The analogy implies that calcium might indirectly activate the Iheat channel by stimulating increases in the intracellular concentration of a cyclic nucleotide, perhaps via the nitric oxide–cGMP signaling pathway previously demonstrated in nociceptors (27, 28).
This research was supported by National Institutes of Health Grant NS21647 to J.D.L., and D.B.R. was supported in part by a research fellowship of the American Heart Association, California Affiliate.
ABBREVIATIONS
- BAPTA-AM
1,2-bis(2-aminophenoxy)ethane-N,N,N′,N′-tetraacetic acid acetoxymethyl ester
- [Ca2+]i
intracellular concentration of free calcium ions
- DRG
dorsal root ganglion
- Iheat
heat-activated current
- PGE2
prostaglandin E2
Note Added in Proof
In preliminary experiments we found that DRG neurons isolated from “knock-out” mice that lack functional cyclic nucleotide-gated olfactory channels (29) (generous gift of John Ngai) exhibit Iheat current, and that these mice do not exhibit impaired behavioral responsiveness to radiant heat stimuli (dat not shown). These observations suggest that the olfactory cyclic nucleotide-gated ion channel itself is not required for heat transduction in mouse.
References
- 1.Urban L, Dray A. Neurosci Lett. 1993;157:187–190. doi: 10.1016/0304-3940(93)90733-2. [DOI] [PubMed] [Google Scholar]
- 2.Gold M S, Dastmalchi S, Levine J D. Neuroscience. 1996;71:265–275. doi: 10.1016/0306-4522(95)00433-5. [DOI] [PubMed] [Google Scholar]
- 3.Baccaglini P I, Hogan P G. Proc Natl Acad Sci USA. 1983;80:594–598. doi: 10.1073/pnas.80.2.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cesare P, McNaughton P. Proc Natl Acad Sci USA. 1996;93:15435–15439. doi: 10.1073/pnas.93.26.15435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reichling D B, Barratt L, Levine J D. Neuroscience. 1997;77:291–294. doi: 10.1016/s0306-4522(96)00511-8. [DOI] [PubMed] [Google Scholar]
- 6.Lynn B, Carpenter S E. Brain Res. 1982;238:29–43. doi: 10.1016/0006-8993(82)90768-5. [DOI] [PubMed] [Google Scholar]
- 7.Lee K H, Chung K, Chung J M, Coggeshall R E. J Comp Neurol. 1986;243:335–346. doi: 10.1002/cne.902430305. [DOI] [PubMed] [Google Scholar]
- 8.Nobile M, Carbone E, Lux H D, Zucker H. Pflugers Arch. 1990;415:658–663. doi: 10.1007/BF02584002. [DOI] [PubMed] [Google Scholar]
- 9.Braun H A, Bade H, Hensel H. Pflugers Arch. 1980;386:1–9. doi: 10.1007/BF00584180. [DOI] [PubMed] [Google Scholar]
- 10.Schild D. In: Nonselective Cation Channels: Pharmacology, Physiology and Biophysics. Siemen D, Hescheler J, editors. Basel: Birkhäuser; 1993. pp. 165–171. [Google Scholar]
- 11.Nilius B, Riemann D. Gen Physiol Biophys. 1990;9:89–111. [PubMed] [Google Scholar]
- 12.Siemen D. EXS. 1993;66:3–25. doi: 10.1007/978-3-0348-7327-7_1. [DOI] [PubMed] [Google Scholar]
- 13.Dray A, Forbes C A, Burgess G M. Neurosci Lett. 1990;110:52–59. doi: 10.1016/0304-3940(90)90786-9. [DOI] [PubMed] [Google Scholar]
- 14.Bevan S, Hothi S, Hughes G, James I F, Rang H P, Shah K, Walpole C S, Yeats J C. Br J Pharmacol. 1992;107:544–552. doi: 10.1111/j.1476-5381.1992.tb12781.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scroggs R S, Todorovic S M, Anderson E G, Fox A P. J Neurophysiol. 1994;71:271–279. doi: 10.1152/jn.1994.71.1.271. [DOI] [PubMed] [Google Scholar]
- 16.Schlichter R, Bader C R, Bernheim L. J Physiol (London) 1991;442:127–145. doi: 10.1113/jphysiol.1991.sp018786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ivanenko A, Baring M D, Airey J A, Sutko J L, Kenyon J L. J Neurophysiol. 1993;70:710–722. doi: 10.1152/jn.1993.70.2.710. [DOI] [PubMed] [Google Scholar]
- 18.Ferreira S H. Agents Actions. 1986;19:91–98. [PubMed] [Google Scholar]
- 19.Kumazawa T, Mizumura K, Minagawa M, Tsujii Y. J Neurophysiol. 1991;66:1819–1824. doi: 10.1152/jn.1991.66.6.1819. [DOI] [PubMed] [Google Scholar]
- 20.Hellon R F, Taylor D C M. J Physiol (London) 1982;326:319–328. doi: 10.1113/jphysiol.1982.sp014195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gold M S, Reichling D B, Shuster M J, Levine J D. Proc Natl Acad Sci USA. 1996;93:1108–1112. doi: 10.1073/pnas.93.3.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grega D S, Macdonald R L. J Neurosci. 1987;7:700–707. doi: 10.1523/JNEUROSCI.07-03-00700.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicol G D, Klingberg D K, Vasko M R. J Neurosci. 1992;12:1917–1927. doi: 10.1523/JNEUROSCI.12-05-01917.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.England S, Bevan S, Docherty R J. J Physiol (London) 1996;495:429–440. doi: 10.1113/jphysiol.1996.sp021604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Firestein S, Zufall F. Semin Cell Biol. 1994;5:39–46. doi: 10.1006/scel.1994.1006. [DOI] [PubMed] [Google Scholar]
- 26.Komatsu H, Mori I, Rhee J S, Akaike N, Ohshima Y. Neuron. 1996;17:707–718. doi: 10.1016/s0896-6273(00)80202-0. [DOI] [PubMed] [Google Scholar]
- 27.Qian Y, Chao D S, Santillano D R, Cornwell T L, Nairn A C, Greengard P, Lincoln T M, Bredt D S. J Neurosci. 1996;16:3130–3138. doi: 10.1523/JNEUROSCI.16-10-03130.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bauer M B, Murphy S, Gebhart G F. J Neurochem. 1995;65:363–372. doi: 10.1046/j.1471-4159.1995.65010363.x. [DOI] [PubMed] [Google Scholar]
- 29.Brunet L J, Gold G H, Ngai J. Neuron. 1996;17:681–693. doi: 10.1016/s0896-6273(00)80200-7. [DOI] [PubMed] [Google Scholar]