Abstract
The iterative development of the Falls Risk Assessment and Management System (FRAMS) drew upon research evidence and early consumer and clinician input through focus groups, interviews, direct observations, and an online questionnaire. Clinical vignettes were used to validate the clinical model and program logic, input, and output. The information model was developed within the Australian General Practice Data Model (GPDM) framework. The online FRAMS implementation used available Internet (TCP/IP), messaging (HL7, XML), knowledge representation (Arden Syntax), and classification (ICD10-AM, ICPC2) standards. Although it could accommodate most of the falls prevention information elements, the GPDM required extension for prevention and prescribing risk management. Existing classifications could not classify all falls prevention concepts. The lack of explicit rules for terminology and data definitions allowed multiple concept representations across the terminology–architecture interface. Patients were more enthusiastic than clinicians. A usable standards-based online-distributed decision support system for falls prevention can be implemented within the GPDM, but a comprehensive terminology is required. The conceptual interface between terminology and architecture requires standardization, preferably within a reference information model. Developments in electronic decision support must be guided by evidence-based clinical and information models and knowledge ontologies. The safety and quality of knowledge-based decision support systems must be monitored. Further examination of falls and other clinical domains within the GPDM is needed.
Electronic decision support and guideline delivery systems can assist clinicians and patients with risk assessment, diagnosis, and management strategies such as counseling,1,2 prevention, therapeutics,3 diagnostic procedures, referral, and review.1,2,4 Typically, these systems also hold patient state information, make decisions, and perform temporal and decision tree actions.5,6 Computer-interpretable guidelines require a formal ontology. Patient state information requires a formal information model to minimize ambiguity. A clinical and decision support model is required to relate the ontology to the information model.
In recognition of the importance of an information model to provide a consistent view of health data and their relationship to other data within and between clinical, administrative, financial, educational, and policy domains of the Australian “health infostructure,” the Australian General Practice Computing Group (GPCG) 1999 Strategic Framework and associated Work Plan7 funded the development of a General Practice Data Model and Core Data Set.8 The model was required to be consistent with relevant standards and protocols for the Australian National Health Data Dictionary (NHDD)9 and the HL7 Reference and Domain Information Models (HL7 RIM).10 The objective of this structured and standards-based approach was to generate precise messages, carrying consistent and “usable” data to the applications that exchange data within the model.
The GP Data Model (GPDM) provides a “map” of most of the key information areas of general practice, covering the domains of patient, provider, resources, schedules, programs, and clinical knowledge (decision support).8 Because it is impossible to print a readable copy of the data model in this article, the model and report can be viewed at the GP Computing Group website ( <www.gpcg.org>). Entities, which are logical collections of data (boxes in the data model diagram), and their relationships have been modeled, using the Unified Modeling Language (UML). For example, the entity “Service provider” has subtypes “Health service provider” (e.g., doctor or nurse) and “Organisational service provider” (e.g., government agency or professional body). The relationships between entities or subtypes may be mandatory or optional and may be one-to-one or one-to-many. The range of information flows encompasses clinical communications such as referrals, health information, and management plans; patient-related demographic information; administrative communications such as appointment bookings; financial transactions such as payments and claims; and policy information including standards advice, health program targets, and service performance reports.
The GPDM is well developed in the practice administration, scheduling, and medication domains but less so in the clinical knowledge domain. This pattern reflects the current state of the art in computer systems in Australia, with many well-developed administrative systems but few useful clinical systems (apart from prescribing systems). The clinical knowledge domain of the GPDM covers health problem, therapeutic, risk factor, service, and guideline groupings.
Why Falls Prevention?
The choice of falls prevention as an exemplar is strategic and conceptual. Falls occur frequently, are preventable,11 and create a high burden of morbidity in the community, acute hospitals, and subacute or rehabilitation settings.12 Prevalence ranges from 2–5% in acute care settings to 25–40% in subacute care and 33% of community-dwelling older people.12 Falls cost the Australian taxpayer $406 million per year in the management of injuries and fractures and increased demand for hospitalization and residential care.13
Falls prevention is a sufficiently complex and multidisciplinary activity to adequately test the robustness of the GPDM. Because of many associated risk factors, intrinsic (e.g., polypharmacy) and extrinsic (e.g., loose carpets) to the patient,14 falls prevention is a complex biopsychosocial and environmental health issue. It requires meaningful engagement of patients and caregivers to identify risk of falls or risk of falls-related injury via environmental safety and clinical assessment and the use of multiple-risk factor intervention strategies to reduce the risk of falling and address secondary problems, such as fear of falling and reduced activity level. Like all multifactorial health problems, prevention and management of falls require frequent referral and information sharing among GPs, nurses, allied health practitioners, medical and surgical specialists, and falls clinics, emphasizing the need for a shared communication infrastructure based on common technical, messaging, and semantic standards to link community and hospital-based health services.15
This article describes how an evidence-based clinical model for falls prevention was developed to guide the development of an information model, which then was examined for its conformity with the GPDM and its reference standards such as the National Health Data Dictionary.9 The adequacy of two of the current classifications used in Australia—the International Classification of Diseases Version 10 with Australian Modifications (ICD10-AM)16 and International Classification of Primary Care Version 2 (ICPC2)17—to support this evidence-based falls prevention model was also examined.
Methods
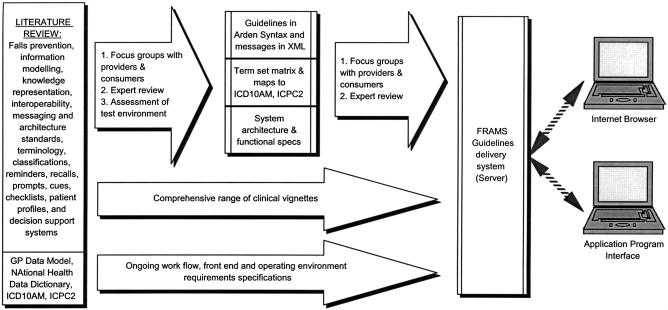
The methodology of the Falls Risk Assessment and Management System (FRAMS) was based on our belief that the main reasons the electronic health record (EHR) and clinical decision support systems have not achieved their potential are the lack of (1) a flexible, modular, and standards-based approach to development of online software to work in a distributed environment; (2) a reference information model for a structured approach to the sharing of precise messages among applications with standardized information architectures; (3) a reference terminology that is sufficiently structured with explicit entities, relationships, constraints, and qualifiers; and (4) adequate and timely user input into design, development, implementation, and use. ▶ describes how the FRAMS was developed over several overlapping phases: literature review, clinical and information models development, terminology documentation and mapping, knowledge representation, and prototype development and testing.
Figure 1.
Key processes in the development and implementation of FRAMS.
Literature Search
The following domains and concepts were searched: falls risk factors, falls prevention strategies, and evidence for their effectiveness across a range of health care settings; information modelling; knowledge representation; interoperability, messaging, and semantic and architecture standards; terminology and classifications; reminders, recalls, prompts, cues, checklists, patient profiles; and decision making and decision support systems (see box at right for a description of the literature search, which included hand searching of key journals, reference lists of obtained articles, and personal contact with content experts in the general practice, public health, and informatics fields).
Databases and Publications Used for the Literature Search
Cochrane Database of Systematic Reviews (to second quarter 2000)
Database of Abstracts of Reviews of Effectiveness (to first quarter, 2000)
Best Evidence (1991 to March/April 2000)
Cochrane Controlled Trials Register (to first quarter 2000)
MEDLINE (1966 to 2000), CINAHL (1982 to April 2000)
Psychlit
AUSHEALTH
World Health Organisation
NHS Centre for Reviews and Dissemination
New York Academy of Medicine
New York Academy of Public Health Medicine
National Cancer Institute's CancerNet (PDQ site)
NIS (PARQ) databases
US Centre for Advanced Health
Canadian Health Promotion Development Section
Centre for Evidence Based Mental Health (UK)
Australian Institute of Health & Welfare
Department of Health & Aged Care
NSW Health Publications
RACGP Publications
State Departments of Health/Human Services
University of Melbourne Faculty of Education Mind Matters site
NHMRC National Rural Research Project database (April 2000)
American Journal of Preventive Medicine
Annual Review of Public Health
Australian Family Physician
Australian Journal of Rural Health
BMJ
BJGP
CMAJ
Family Practice
Health Services Journal
Health Promotion International
IMIA Yearbooks (last 10 years) Informatics in Healthcare Australia
International Journal of Medical Informatics
International Journal of Health Promotion
Joint Commission Journal on Quality Improvement
Journal of the American Medical Association
Journal of the American Medical Informatics Association
Journal of Advanced Nursing
Electronic version of Medical Journal of Australia (MJAe)
Australian and New Zealand Journal of Public Health (1994–2000)
Proceedings of the SCAMC and AMIA Conferences (Spring and Fall)
Proceedings of Medinfo
Proceedings of Conferences of the Primary Health Care Special Interest Group of the British Computer Society
Falls risk factors were included only if they met the requirements for strength of the evidence for different levels of risk (based on odds ratios published in identified prospective studies using multivariate analyses), had relevance in the screening process, and had a range of recommended actions corresponding to each identified risk factor. This phase guided the initial development of the ontology of the falls prevention guidelines database and the clinical model for primary and secondary falls prevention within a multidisciplinary integrated care context.
Clinical Model, Vignettes, and Focus Groups
As part of the clinical model development, we developed a range of clinical vignettes, which comprehensively addressed falls prevention and the associated terminology descriptors across a range of falls risk factors and care settings, e.g., gender, age, disability, polypharmacy, comorbidity, and exposure to extrinsic risk factors in the community and hospital settings. The logic of the vignettes and the consistency, comprehensiveness, and appropriateness of the terminology were tested, refined, and validated by focus groups of health care providers* and health care consumers.† These vignettes were used throughout the development cycle to test the logic and information requirements of FRAMS.
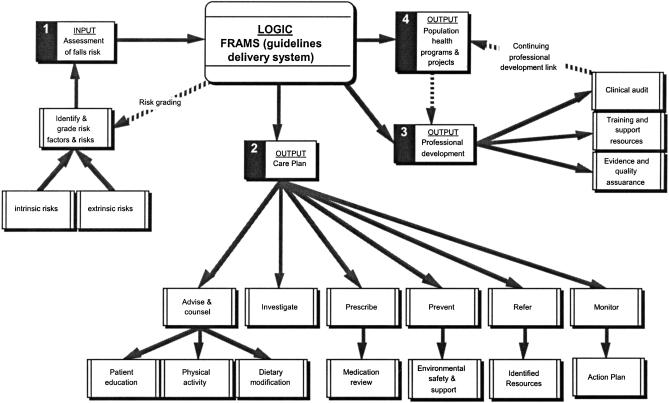
The final clinical model, based on the literature plus patient and provider input, defines the input process (diagnosis and risk factors) and output to assist with patient management (▶). Constraint issues such as workflow, safety, and quality were emphasized.
Figure 2.
Clinical (business process) model for falls risk assessment and management.
Information Model and Term Set Development
The formal description of the entities, their instances, and their relationships in the falls domain was developed, using the GPDM as a template. Information model development paralleled terminology development. This was an important attribute of the FRAMS methodology because it raised issues and highlighted gaps in the terminology–architecture overlap. The National Health Data Dictionary, National Minimum Data Set for Injury Surveillance, and GPDM guided the specification of a “term set matrix,” to store the categories of data and attributes for manipulation and communication (▶). Terms generated from the literature and focus groups were categorized using the clinical model developed (▶) as diagnosis, risk factors, management (including prevention and rehabilitation), professional development, and population health. Terms were further categorized according to whether they referred to actor, action, reason, outcome, modifier and qualifier for time, duration, location, anatomy, intrinsic and extrinsic causes, and the nature of the injury.
Table 1.
Term Set Matrix with Examples
| Dimension of Action | Actor | Action | Reason | Outcome | Qualifier (e.g., place, time) | Modifier | Comment | ICD10-AM Code | ICPC2 Code |
|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Patient Clinician | Medication overdose (ingested) | Medication overdose (accidental) | Death | At home At night | Prescribed medication | X44, Y92.9 | ||
| Management | Clinician | Strengthen muscles | Increase confidence Reduce falls risk | Referral to physio care plan | Hospital | Weekly | |||
| Prescribe | GP Specialist Veterinary Dentist Nurse practitioner | Prescribing service (MBS item) | Prescription Medication | Current New Previous | 96027-00 J45.9 | ||||
| Professional development | Clinician Educators Division CME providers | Vocational training Upskilling | Vocational registration QACPD | Architecture or terminology? | Z56.7 | ||||
| Population health | Epidemiologist Biostatistician Program manager | Measurement Evaluation Program management | Program evaluation | Rates Risks | Season Longitudinal study | Architecture or terminology? |
Following categorization into the “term set matrix” (▶), the terms were mapped to the ICD10-AM index of terms, using documentation supplied by the National Centre for Classification in Health (NCCH) and PrimeCoder,18 a software application to allocate ICD10-AM codes to terms. Uncoded items were rechecked manually for synonyms and other variations, after which the term set was again mapped to ICD10-AM via PrimeCoder. A similar iterative process was used for the ICPC2. This staged process provided an estimate of the clinical relevance and specificity of ICD10-AM and ICPC2 for falls prevention.
Development of the FRAMS Prototype
Physically, the FRAMS prototype consists of three modular standards-based components—a guidelines delivery system (server), an Internet browser–based client software, and an interface implementation to interface with desktop clinical software—deployed in a distributed environment. The information model for FRAMS was framed around the input, logic, and output items defined in the clinical model (▶). Input items were risk factors for falling. The output included an assessment of the risk for falling and a care plan outlining strategies for improved patient management. Risk was categorized as mild, moderate, or high, with high risk factors colored red. The strategies included medication review; patient education; recommendations, e.g., physical activity, dietary modification; environmental safety assessment; injury minimization strategies; and clinical assessment and review of sensory capabilities, health status, and activities of daily living (ADL). The output also included resources for clinician education on falls prevention and management of falls risks and related injuries. Education and professional development resources included reference to evidence-based publications, videos, clinical audits, and assessment tools.
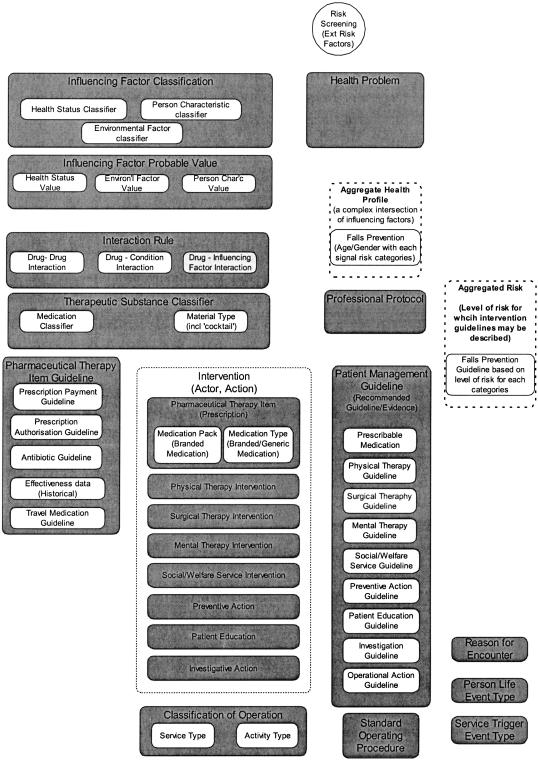
Figure 3.
The Clinical Knowledge domain of the GP Data Model with candidate entities for falls prevention shown in dashed boxes and yellow-colored boxes (links not shown to keep the diagram simple).
The Arden Syntax19 was used to represent the evidence-based guidelines and rules for use in the logic engine (Table 2, available as an online data supplement at <www.jamia.org>). The rules for each risk factor were implemented as single medical logic modules (MLM). The MLMs were built into protocols to form the falls prevention knowledge base—the guidelines server. The content of the messages and queries were coded in XML.20 The guidelines were made available via the FRAMS website, <www.falls.unimelb.edu.au>, as a direct SQL request via an Internet Browser or via an Application Program Interface (API) using XML messaging over TCP/IP in the Internet environment.
Privacy Concerns
The FRAMS application is freestanding, separate from patient data, thereby addressing privacy and confidentiality issues. Permanent patient information remains on the clinicians' desktop software. The reduced number of transactions also reduces privacy risks and potentially improves work efficiencies. No record of any transaction is available unless the care plan is printed or saved as a file electronically.
Testing and Evaluating the FRAMS Prototype
Individual and group testing sessions were held, in which patients and clinicians (GPs, rehabilitation and aged care specialists, including allied health staff) were taught to access and use the online FRAMS and were encouraged to test the logic as provided in the output (care plan), determine the relevance and comprehensiveness of the term set, and determine how the interface and functionalities affected their work processes. A number of sessions involved rehabilitation and aged care specialists using the FRAMS with their patients. Participants were observed during these sessions, and feedback was obtained during and after the sessions by a research assistant.
Clinicians and their patients were encouraged to access and test the FRAMS on their own time. An online questionnaire, along with phone and fax contact details, was included to obtain ongoing feedback on the system. In addition, a number of FRAMS workshops were held at general practice conferences and falls prevention specialist meetings, using the same methodology. This preliminary user testing is part of an ongoing iterative strategic evaluative process to address the logic, terminology, design, interface, and work flow issues. Although mostly positive, these preliminary findings are be reported in this article.
Outcomes and Discussion
The clinicians who participated in the clinical modeling and terminology focus groups as well as the user testing sessions reported that this comprehensive iterative process assisted them in understanding the software development process and in appreciating the evidence base for the FRAMS prototype. The use of clinical vignettes and “use cases” throughout the development cycle worked well to relate the FRAMS to clinical and business processes. The comprehensive and iterative input from a broad range of consumers and clinicians appeared to enhance the relevance and usefulness of the falls prevention term set and information model significantly. This strategic evaluative process is ongoing, and the preliminary information available is mainly qualitative. Summative evaluation is planned in the near future.
After removal of duplicates and misspelled terms, 871“clean unique terms” remained. One fifth (20.6%) of clinical concepts, e.g., “Frail/aged,” “Injury, unintentional,” “Tripping, slipping hazards,” “Unable to care for self/require care provider,” “Reversible problem,” were either not classifiable or classified ambiguously in both ICD10-AM and ICPC2. Based on a count of the clean terms mapped, ICPC2 (6.3% mapped) was not as comprehensive as ICD10-AM (73% mapped) in describing the falls prevention domain. This is understandable because the ICPC2 is a classification, not a terminology, and it is focused on breadth not depth. Furthermore, much of the falls prevention literature and activity is in the secondary care setting. Clearly, a comprehensive clinical terminology is required to completely describe the falls prevention domain.
The varying levels of granularity of the six domains of the GPDM, in the context of integrated and coordinated care to prevent and manage falls, was a technical issue. To allow the implementation of a falls prevention information model within the GPDM, high-level generic concepts such as “aggregated health profile,” had to be extended. The “influencing factor” entity (data element) was extended to include intrinsic risk factors for falls and the “risk assessment” entity was extended to include extrinsic risk factors. All these risk factors were subsumed within the “aggregated risk” entity. Demographic risk factors, age and gender, were subsumed within the “aggregated health profile,” an entity located at a level higher than the clinical knowledge domain in the GPDM. These proposed enhancements (candidate entities) to the GPDM are shown in ▶ (as boxes with dashed lines or are colored yellow).
Rules are required to standardize the extension of the information model. In addition, rules are required for the use of the information model. For example, risk factor data may be classified as a health problem, influencing factor or a risk factor. Because risk factors may be of different durations or severities, and the clinician may screen for, diagnose, or manage the risk factor(s), temporal and staging qualifiers are necessary. All these aspects require standardization.
A consistent level of granularity across the terminology, information, and knowledge representation models is important to promote consistent user data entry as the trigger for decision support actions—in both the Internet (TCP/IP) and Electronic Health Record (EHR) environments. Where decision support and guideline delivery systems interface with terminologies (e.g., SNOMED-CT) or classifications (e.g., ICD10-AM) with an inherent ontology, there is a potential for conflict between terminological and clinical rules and reasoning.21 Clinical users and developers of patient information databases and guideline delivery systems need to understand and be aware of this potential conflict in their systems' design, implementations, and monitoring for safety and quality.
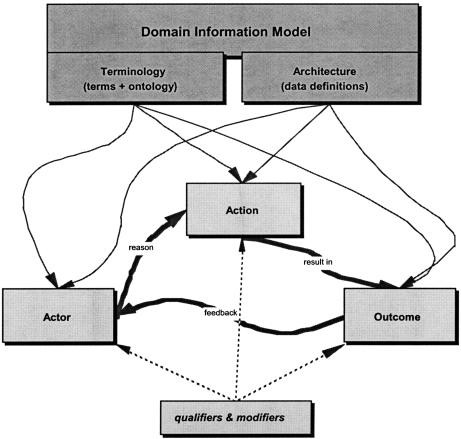
Concurrent term set and information model development, within the framework of the National Health Data Dictionary (NHDD) and GPDM, allowed the FRAMS process to identify data element overlaps, gaps, and equivalent terms. Is “comorbidity” or “dependency level” more appropriate as a data element in the falls prevention information model than as a term or concept in a falls prevention terminology? Is it better to have a concept “dependence” with qualifiers for “levels?” The concept “family history” can be a part of the information architecture or a “qualifier” to a range of clinical concepts in a terminology. Thus, “family history of osteoporosis” may be a unique concept or a concept “osteoporosis” qualified by concept “family history.” Some concepts are better addressed in a terminology (e.g., osteoporosis), some in the information model and architecture (e.g., family history) and some in the decision support system (e.g., severity, site, duration, or onset). A reference information model is essential to ensure consistency and a shared understanding and to guide implementation decisions as to which health care concepts are integral to the terminology and which to the architecture. ▶ shows the relationship between an information model's architecture and terminology.
Figure 4.
Relationship between an information model's architecture and terminology.
In Australia, this reinforces the need for a terminology that is harmonized with the GP Data Model and National Health Data Dictionary within a reference information model, which may be the HL7 RIM. The GPDM maps well to HL7 RIM, but not vice versa. Because the lack of a standard interface between the terminology and information models is an issue relevant to the whole health sector, other relevant information models such as the Community Health Information Model must be included. It may be time to resurrect the National Health Information Model.22
One way forward has been the work by Standards Australia Committee on Health Informatics (IT-14) Working Group 2 on Health Concept Representation. This draws heavily on the work of ISO TC215 on health concept representation (Working Group 3) and health records and modeling coordination (Working Group 1), which acknowledges and addresses the terminology–architecture gaps, user interface, and design to optimize use at the clinical interface. Although this is a positive direction, the ultimate solution lies at a political and policy level. In Australia, a “Short Term Taskforce on Terminologies,” bringing together the terminology and classification experts, is beginning to grapple with these issues at the Commonwealth Government policy level.
Conclusion
The FRAMS methodology emphasizes evidence for safety and effectiveness, user-centerdness, and privacy in a generic, modular, standards-based, and distributed approach to the modeling of the clinical process, information required, knowledge base, and decision logic. It reaffirms the need for a systems approach, well grounded in clinical practice, to enable the effective use and refinement of the evolving work in reference information models, reference terminologies, and health concept representation and to bring best practice guidelines to the clinicians' desktops. Software implementations must encourage the routine use of guidelines in daily practice. Ongoing refinement and implementation of the FRAMS prototype and methodology can lead to useful applications in a range of clinical domains.
The current lack of national and international agreement on a common reference terminology and a reference information model are barriers. However, ongoing FRAMS work will contribute to the current efforts to harmonize interoperability standards around health concept representation and terminological and information models. It sets the benchmark, scope, and process for system developers and researchers to continually monitor and refine the interoperability standards and benchmarks required for safe and effective decision support systems.
Supplementary Material
The authors thank the GP Computing Group for funding this project, FRAMS project team and clinicians, and consumers who contributed to the terminology and the clinical and information models.
Footnotes
Included five general practitioners, a practice manager, a pharmacist, two aged care and rehabilitation specialists, two health promotion specialists, a physiotherapist, two rehabilitation specialists, an integrated care manager, and an information technology specialist.
Included a consumer advocate and five older patients with a range of chronic diseases such as arthritis and diabetes.
References
- 1.Johnston ME, Langton KB, Haynes RB, Mathieu A. Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994; 120:135–42. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan F, Mitchell E. Has GP computing made a difference to patient care? Systematic review of published reports. BMJ. 1995; 311:848–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzmaurice D, Hobbs F, Murray E, Bradley C, Holder R. Evaluation of computerized decision support for oral anticoagulation management based in primary care. Br J Gen Pract. 1996; 46:533–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Shea S, DuMouchel W, Bahamonde L. Meta-analysis of 16 RCTs to evaluate computer-based clinical reminder systems for preventive care in ambulatory settings. JAMIA. 1996; 3:399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, Peleg M, Tu S, Shortliffe E, Greenes R. Representation of clinical practice guidelines for computer-based implementations. In: Patel V, (eds). Medinfo. Amsterdam: London: IOS Press; 2001. [PubMed]
- 6.Pattison-Gordon EG, Cimino J, Tu S, Gennari J, Jain N, Greenes R. Requirements of a Sharable Guideline Representation for Computer Applications. Stanford, CA: Stanford University, 1996.
- 7.GP Computing Group, Commonwealth Department of Health and Aged Care. Strategic Framework: General Practice Information Management and Technology. <www.gpcg.org>, Canberra, 1999.
- 8.GP Computing Group, Commonwealth Department of Health and Aged Care. General Practice Data Model and Data Dictionary. <www.gpcg.org>, Canberra, 2000.
- 9.National Health Data Committee National Health Data Dictionary Version 5.0. Canberra: Australian Institute of Health & Welfare, 1996.
- 10.Heitman K, Blobel B, Dudeck J. HL7 Communication Standard in Medicine (ed 1). Cologne: Verlag Alexander Monch, 1999.
- 11.Gillespie L, Gillespie W, Robertson M, Lamb S, Cumming R, Rowe B. Interventions for preventing falls in elderly people (Cochrane Review). Cochrane Database Syst Rev 3: CD000340, 2001. [DOI] [PubMed]
- 12.Hill K, Smith R, Murray K, et al. An Analysis of Research on Preventing Falls and Falls Injury in Older People: Community, Residential Care and Hospital Settings. Melbourne: Department of Human Services, 2000.
- 13.Mathers C, Penm R. Health System Costs of Injury, Poisoning and Musculoskeletal Disorders in Australia 1993–1994. Canberra: Australian Institute of Health and Welfare, 1999. Report No., Health and Welfare Series No 6.
- 14.Lord S, Sherrington C, Menz H. Falls in Older People: Risk Factors and Strategies for Prevention. Cambridge, UK: Cambridge University Press, 2001.
- 15.Stalenhoef PA, Diederiks JPM, Knottnerus JA, de Witte LP, Crebolder H. The construction of a patient record-based risk model for recurrent falls among elderly people living in the community. Fam Pract. 2000; 17:490–6. [DOI] [PubMed] [Google Scholar]
- 16.NCCH, National Centre for Coding and Classification in Health The International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Australian Modification (ICD-10-AM). Sydney: Commonwealth of Australia, 2000. [PubMed]
- 17.WONCA Classification Committee International Classification of Primary Care (ed 2) (ICPC-2). Oxford: World Organisation of Family Doctors, 1998.
- 18.Grain H. (personal communication). PrimeCoder. <www.primecoder.com.au>. Accessed June 2001.
- 19.HL7 (Health Level Seven) Arden Syntax for Medical Logic Systems. Ann Arbor, MI: American Society for Testing and Materials (ASTM), 1999.
- 20.WWW Consortium. Extensible Markup Language (XML), 1997.
- 21.Rector A. The Interface between information, terminology, and inference models. In: Patel V, Rogers R, Haux R, (eds). Medinfo 2001. Amsterdam: London: IOS Press, 2001, pp 246–50. [PubMed]
- 22.AIHW, Australian Institute of Health and Welfare. National Health Information Model. URL <http://www.aihw.gov.au/inet/knowledgebase/indexkbhealth.html>. Accessed January 2001.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.