Abstract
The purpose of this investigation was to examine the influence of antisociality and extent of multidrug use on cognitive and motor impulsivity among substance dependent individuals (SDIs) that used primarily cocaine and/or heroin. One hundred currently abstinent male SDIs participated in the study. Extent of multidrug use and degree of antisociality, assessed with the Socialization Scale of the California Psychological Inventory (So-CPI), were used to classify participants into one of four groups: high antisocial/low multidrug use, high antisocial/high multidrug use, low antisocial/low multidrug use, and low antisocial/high multidrug use. All subjects completed the Iowa Gambling Task to assess cognitive impulsivity and the Stroop Task to measure motor impulsivity. Contrary to expectations, antisociality was associated with more advantageous performance on the Iowa Gambling Task, independent of extent of multidrug use. In contrast, greater multidrug use was associated with general psychomotor slowing on the Stroop Task. Results suggest that a subclinical form of antisociality may have a paradoxically facilitating effect on decision-making and cognitive impulsivity among SDIs.
Keywords: drug addiction, impulsivity, antisocial, polysubstance use, multidrug use, decision-making
1. Introduction
Impulsivity is a multidimensional construct, considered a core component in drug addiction (Goldstein & Volkow, 2002). Reward-discounting or cognitive impulsivity refers to the preference for smaller immediate rewards over larger delayed rewards, whereas rapid-response or motor impulsivity is manifested by poor inhibitory control of pre-potent responses (Dougherty et al., 2003). Substance dependent individuals (SDIs) are often impaired on tasks measuring cognitive (Bechara et al., 2001) or motor impulsivity (Verdejo-Garcia & Perez-Garcia, 2007). However, not all SDIs manifest such impairments, which suggests that some additional risk factors may increase their vulnerability for cognitive and motor impulsivity. The current study explored whether two potential risk factors, namely antisociality and extent of multidrug use, both commonly observed in SDIs (Craig, 2000, Leri et al., 2003) and previously related to poor impulse control (Mitchell et al., 2002; Moeller et al., 2002), account for differences in cognitive and motor impulsivity among SDIs. We used the Iowa Gambling Task (IGT) and the Stroop Task: two common laboratory paradigms to measure cognitive and motor impulsivity, respectively. We hypothesized that both of these risk factors would be associated with greater impulsivity in SDIs.
2. Methods
Participants were 100 currently abstinent, HIV seronegative male participants with history of substance dependence, enrolled in a larger study of neurocognition and HIV among SDIs at the University of Illinois, Chicago. Subjects testing positive on urine toxicology screening or breathalyzer testing for alcohol, or with any history of potentially confounding neurologic illness or injury, schizophrenia, or current alcohol abuse or dependence were excluded.
History of substance abuse and dependence was determined using the Structured Clinical Interview for DSM-IV Substance Abuse Module (First et al., 1996). Antisociality was assessed by the Socialization Scale of the California Psychological Inventory (So-CPI; Gough, 1987), a common measure of antisociality among non-incarcerated individuals. We used the North American Adult Reading Test (Grober & Sliwinski, 1991) to estimate verbal IQ.
All participants had a positive history of cocaine dependence and 80% carried a diagnosis of past alcohol abuse or dependence. Subjects diagnosed additionally with opiate dependence (53% of the sample) were classified as “high multidrug use”, while all others were assigned to the “low multidrug use” group. Participants were further appointed to a “high” or “low antisocial” group on the basis of a median split (Md=27) of their So-CPI scores. With the exception of a positive Hepatitis C serostatus [X2 = 4.02, p < 0.04], the four groups were well-matched on demographic and substance dependence characteristics (Table 1).
Table 1.
Demographic and Substance Use Characteristics
| High Antisocial/Low Multidrug Use (n=15) | High Antisocial/High Multidrug Use (n=33) | Low Antisocial/Low Multidrug Use (n=32) | Low Antisocial/High Multidrug Use (n=20) | |
|---|---|---|---|---|
| Age | 42.33 (8.75) | 42.78 (6.38) | 42.3 (5.86) | 45.33 (6.11) |
| Years of Education | 12.33 (2.44) | 12.33 (1.80) | 12.67 (1.53) | 12.19 (1.17) |
| IQ | 98.83 (11.00) | 100.94 (9.29) | 104.17 (8.88) | 101.54 (6.95) |
| CPI-SO | 22.13 (2.85) | 21.31 (3.50) | 32.06 (3.73) | 30.81 (3.09) |
| Y Drug Use | 23.53 (9.27) | 21.91 (8.05) | 21.44 (7.79) | 25.43 (4.80) |
| D Last Use (median, IQR) | 80 (31, 304) | 82.5 (36.5, 287) | 115 (60.5, 195) | 90 (30, 240) |
Note: CPI-SO - California Psychological Inventory-Socialization Scale; Y Drug Use - Years of Drug Use; D Last Use - Number of days since last used drugs.
All subjects completed the computerized IGT and the Reaction Time (RT) Stroop Test (see Bechara et al., 2001 and Martin et al., 1992 for detailed descriptions). The IGT requires subjects to select a series of cards from one of four decks. Each card carries a monetary gain or loss of varying size. Patients with ventromedial prefrontal lesions and SDIs often perform the task poorly, by persistently choosing cards associated with large rewards but also with larger and more frequent losses. The computerized RT Stroop requires subjects to name the display color of a series of colored words under three conditions with varying demands on behavioral inhibition. The most taxing condition (i.e. the “incongruent condition”) requires subjects to name color-discordant words (e.g. “RED” presented in green) while suppressing the tendency to read the word.
3. Results
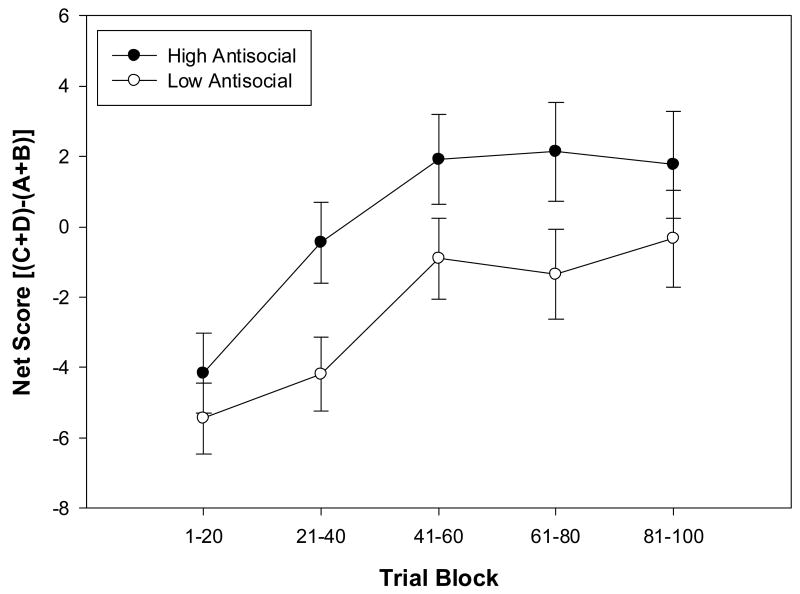
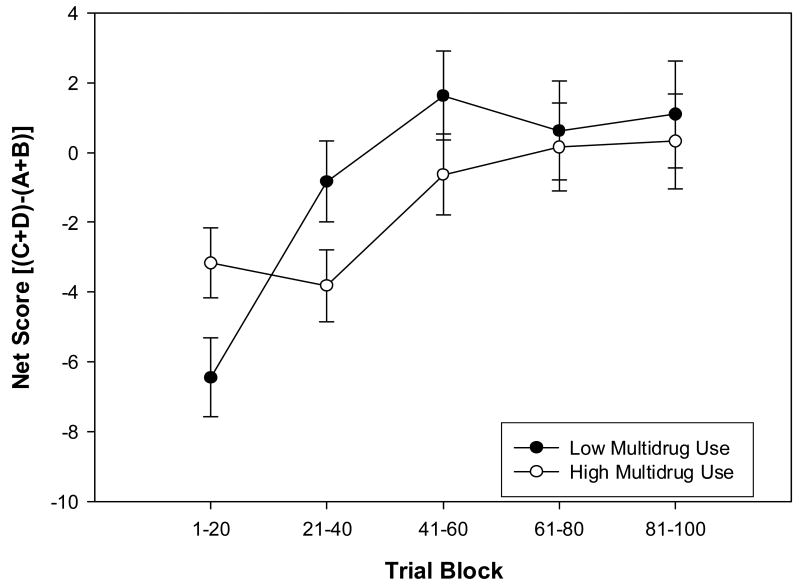
IGT data were scored according to the procedure first reported by Bechara et al. (2001). Data were analyzed with a mixed-model ANOVA, with trial block as the within-subject factor, and Multidrug Use and Antisociality as the between-subjects factors. As expected, all groups improved their performance as the task progressed [F (4,380) = 10.93, p < 0.0001]. However, contrary to expectations, higher levels of antisociality were associated with better IGT performance overall [F (1,95) = 5.17, p < 0.02] (Figure 1). Additionally, IGT scores for subjects in the “low multidrug use” group showed a significant improvement in performance over the 100 trials, whereas the subjects in the “high multidrug use” group showed no evidence of an improved performance as the task progresses, indicated by a significant interaction between Trial Block and Multidrug Use [F (4,380) = 2.77, p < 0.02] (Figure 2).
Figure 1.
Main effect of antisociality on Iowa Gambling Task
Figure 2.
Interaction between extent of multidrug use and trial block on the Iowa Gambling Task
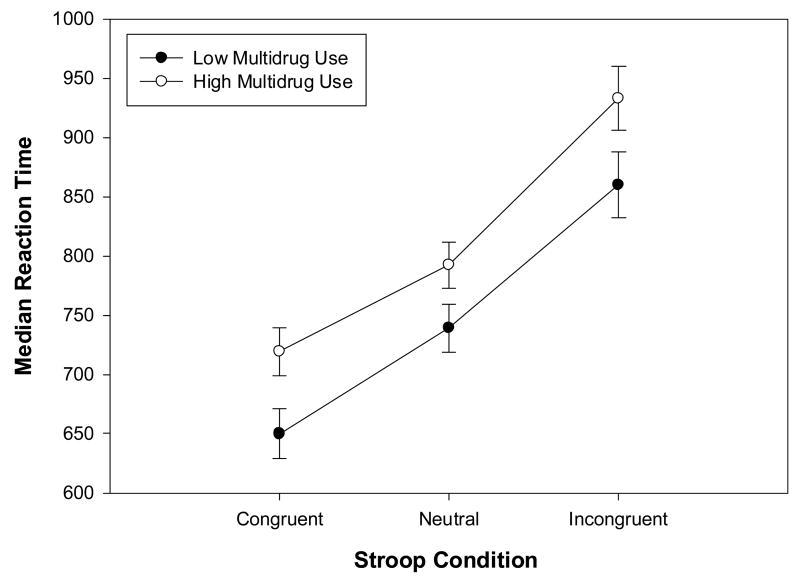
RT Stroop data was analyzed by 2 (Multidrug Use) × 2 (Antisociality) × 3 (Stroop Condition) mixed-model ANOVA1. All participants’ reaction times increased with increasing demands on response inhibition [F (2, 158) = 279.2; p < 0.0001]. The “high multidrug use” group was significantly slower (M = 814.95 ± 21.19) than the “low multidrug use” group (M = 749.66 ± 21.95) in all Stroop conditions [F (1,79) = 4.58, p < 0.03] (Figure 3); however, this group difference was no longer apparent when Hepatitis C serotatus was controlled.
Figure 3.
Main effect of extent of multidrug use on the Stroop Color Word Task
4. Discussion
To our knowledge, this is the first study to investigate specifically the effects of antisociality and extent of multidrug use on indices of impulsivity among SDIs. The study revealed three important findings. First and foremost, contrary to predictions, we found that antisociality was associated with more advantageous decision-making performance on the IGT and thus with better cognitive impulse control, independent of extent of multidrug use. Second, there was indication of a significant improvement in decision-making performance across IGT trial blocks for the low multidrug use but not for the high multidrug use group, evidenced by a flatter learning curve in the high multidrug use group. Finally, greater extent of multidrug use was associated with general psychomotor slowing, but not with motor impulsivity per se on the Stroop.
In light of our earlier finding that psychopathic heroin addicts evidence impaired performance on the IGT (Vassileva et al., 2007), current results suggest that impaired performance of antisocial individuals on the IGT may become evident only at the extreme end of the antisocial spectrum, when antisociality is a clinically diagnosable syndrome such as Antisocial Personality Disorder or Psychopathy, and not when it is manifested as a personality trait considered to be on a continuum with normality, such as degree of socialization as assessed by the CPI-So. One might thus speculate that a sub-clinical, “non-malignant” form of antisociality might exert a paradoxically facilitating effect on decision-making and cognitive impulsivity in SDIs. This will have to be investigated further by in future studies. Also, the fact that antisociality had no effect on motor impulsivity indexed by the Stroop task, but in contrast had a facilitating effect on decision-making/cognitive impulsivity may be related to better impulse control in the antisocial group particularly when rewards are involved.
With regards to our second finding, the flatter learning curve of the high multidrug use SDIs suggests that they do not learn the task contingencies and show greater tendency to perseverate on making decisions that were initially rewarding, but ultimately disadvantageous. Relative to the high multidrug use SDIs, our low multidrug use group was guided initially to a greater degree by the higher magnitude of the immediate rewards. Yet, they learned to shift their strategy as soon as the first punishment trials were delivered. In contrast, the high multidrug use subjects continued to be guided by the prospect of immediate short-term gains, and never changed their selection strategy throughout the task.
Finally, the significance of the overall slowing in the high multidrug use group on the Stroop Task remains unclear, because additional analyses revealed that differences in Stroop reaction times were found to be accounted for by Hepatitis C serostatus. This is consistent with a recent report from our laboratory (Martin et al., 2004) indicating that a positive Hepatitis C serostatus is associated with overall slower information processing on the Stroop task, and deserves further investigation.
Acknowledgments
We thank Joanna Jacobus, Stephanie King, and Niles Rains for their assistance with data collection. This research was supported by NIDA grants R21-DA18086 (JV), R01-DA12828 (EMM) and F32-DA018522 (RG).
Footnotes
Due to technical difficulties with the computer program, we had missing data from 18 subjects (valid n=88).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39:376–389. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- Craig RJ. Prevalence of Personality Disorders among Cocaine and Heroin Addicts. Substance Abuse. 2000;21:87–94. doi: 10.1080/08897070009511421. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Bjork JM, Harper RA, Marsh DM, Moeller FG, Mathias CW, Swann AC. Behavioral impulsivity paradigms: a comparison in hospitalized adolescents with disruptive behavior disorders. Journal of Child Psychology and Psychiatry. 2003;44:1145–1157. doi: 10.1111/1469-7610.00197. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: Biometrics Research; 1996. [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. American Journal of Psychiatry. 2002;159:1642–1652. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gough H. California Psychological Inventory administrator’s guide. Consulting Psychologists Press; Palo Alto, CA: 1987. [Google Scholar]
- Grober E, Sliwinski M. Development and validation of a model for estimating premorbid verbal intelligence in the elderly. Journal of Clinical and Experimental Neuropsychology. 1991;13:933–949. doi: 10.1080/01688639108405109. [DOI] [PubMed] [Google Scholar]
- Leri F, Bruneau J, Stewart J. Understanding polydrug use: review of heroin and cocaine co-use. Addiction. 2003;98:7–22. doi: 10.1046/j.1360-0443.2003.00236.x. [DOI] [PubMed] [Google Scholar]
- Martin EM, Novak RM, Fendrich M, Vassileva J, Gonzalez R, Grbesic S, Nunnally G, Sworowski L. Stroop performance in drug users classified by HIV and hepatitis C virus serostatus. Journal of the International Neuropsychological Society. 2004;10:298–300. doi: 10.1017/S135561770410218X. [DOI] [PubMed] [Google Scholar]
- Martin EM, Robertson LC, Edelstein HE, Jagust WJ, Sorensen DG, San Giovanni D, Chirurgi VA. Performance of patients with early HIV-1 infection on the Stroop Task. Journal of Clinical and Experimental Neuropsychology. 1992;14:857–858. doi: 10.1080/01688639208402867. [DOI] [PubMed] [Google Scholar]
- Mitchell DG, Colledge E, Leonard A, Blair RJ. Risky decisions and response reversal: is there evidence of orbitofrontal cortex dysfunction in psychopathic individuals? Neuropsychologia. 2002;40:2013–2022. doi: 10.1016/s0028-3932(02)00056-8. [DOI] [PubMed] [Google Scholar]
- Moeller GF, Dougherty DM, Barratt SE, Oderinde V, Mathias CW, Harper RA, Swann AC. Increased impulsivity in cocaine dependent subjects independent of antisocial personality disorder and aggression. Drug and Alcohol Dependence. 2002;68:105–111. doi: 10.1016/s0376-8716(02)00106-0. [DOI] [PubMed] [Google Scholar]
- Vassileva J, Petkova P, Georgiev S, Martin EM, Tersiyski R, Raycheva M, Velinov V, Marinov P. Impaired decision-making in psychopathic heroin addicts. Drug and Alcohol Dependence. 2007;86:287–289. doi: 10.1016/j.drugalcdep.2006.06.015. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Perez-Garcia M. Profile of executive deficits in cocaine and heroin polysubstance users: common and differential effects on separate executive components. Psychopharmacology. 2007;190:517–530. doi: 10.1007/s00213-006-0632-8. [DOI] [PubMed] [Google Scholar]