Abstract
Objectives
To examine the psychosocial correlates of chronic tension-type headache and the impact of chronic tension-type headache on work, social functioning, and well-being.
Methods
Two hundred forty-five patients (mean age=37.0 years) with chronic tension-type headache as a primary presenting problem completed an assessment protocol as part of a larger treatment outcome study. The assessment included a structured diagnostic interview, the Medical Outcomes Study Short Form, Disability Days/Impairment Ratings, Recurrent Illness Impact Profile, Beck Depression Inventory, State-Trait Anxiety Inventory—Trait Form, Primary Care Evaluation for Mental Disorders, and the Hassles Scale Short Form. Comparisons were made with matched controls (N=89) and, secondarily, with Medical Outcomes Study data for the general population, arthritis, and back problem samples.
Results
About two thirds of those with chronic tension-type headache recorded daily or near daily (≥25 days per month) headaches with few (12%) recording headaches on less than 20 days per month. Despite the fact that patients reported that their headaches had occurred at approximately the present frequency for an average of 7 years, chronic tension-type headache sufferers were largely lapsed consulters (54% of subjects) or current consulters in primary care (81% of consulters).
Significant impairments in functioning and well-being were evident in chronic tension-type headache and were captured by each of the assessment devices. Although headache-related disability days were reported by 74% of patients (mean=7 days in previous 6 months), work or social functioning was severely impaired in only a small minority of patients. Sleep, energy level, and emotional well-being were frequently impaired with about one third of patients recording impairments in these areas on 10 or more days per month. Most patients with chronic tension-type headache continued to carry out daily life responsibilities when in pain, although role performance at times was clearly impaired by headaches and well-being was frequently impaired.
Chronic tension-type headache sufferers were 3 to 15 times more likely than matched controls to receive a diagnosis of an anxiety or mood disorder with almost half of the patients exhibiting clinically significant levels of anxiety or depression. Affective distress and severity of headaches (Headache Index) were important determinants of headache impact/impairment.
Conclusions
Chronic tension-type headache has a greater impact on individuals' lives than has generally been realized, with affective distress being an important correlate of impairment. If treatment is to remedy impairment in functioning, affective distress, as well as pain, thus needs to be addressed.
Keywords: chronic tension-type headache, disability, impairment, affective distress
In the decade since the International Headache Society (IHS) classification system provided the operational diagnostic criteria that distinguish episodic (ETTH) and chronic (CTTH) forms of tension-type headache (see Table 1),1 surprisingly little information has appeared on either the psychosocial correlates or the impact of CTTH. Migraine, which is more prevalent than CTTH in the general population and is encountered more often in many clinical settings, has, understandably, occupied the attention of most investigators. Studies of tension-type headache that might have provided information about CTTH typically have failed to distinguish ETTH from CTTH. Most of these studies also fail to rule out the possibility that frequent headaches are maintained by high levels of analgesic use and are, thus, more accurately diagnosed as headaches induced by chronic medication use than as tension-type headaches. As a result, our knowledge of the psychosocial correlates and the impact of CTTH remains limited.
Table 1.
International Headache Society Diagnostic Criteria for Episodic and Chronic Tension-type Headache1
| 2.1 Episodic tension-type headache | 2.2 Chronic tension-type headache |
|---|---|
| A. At least 10 previous headache episodes fulfilling criteria B-D listed below. Number of days with such headache < 180/year (< 15/month). | A. Average headache frequency 15 days/month (180 days/year) for 6 months fulfilling criteria B-D listed below. |
| B. Headache lasting from 30 minutes to 7 days. | B. No duration criterion (headache may be unremitting). |
| C. At least 2 of the following pain characteristics: (1) pressing/tightening (non-pulsating) quality, (2) mild or moderate intensity (may inhibit, but does not prohibit activities), (3) bilateral location, (4) no aggravation by walking stairs or similar routine physical activity. | C. Same. |
| D. Both of the following: (1) no nausea or vomiting (anorexia may occur), (2) photophobia and phonophobia are absent, or one but not the other is present. | D. Both of the following: (1) no vomiting, (2) no more than one of the following: nausea, photophobia or phonophobia. |
| E. History, physical, neurological exams (and if called for, appropriate investigations) rule out secondary headache, or if present secondary headache does not occur in close temporal relation to tension-type headache. | E. Same. |
Epidemiological studies that have examined the psychological correlates of tension-type headache generally fail to provide information specifically about CTTH. Merikangas et al,2,3 for example, found no indication that anxiety or mood disorders were more prevalent or that reports of psychological symptoms (Symptom Checklist 904) were more frequent in ETTH sufferers than in controls without headache problems. It is unclear, however, if these findings can be generalized to CTTH, because much higher rates of psychiatric comorbidity are observed in CTTH than in ETTH, at least in clinical samples.5,6 Conversely, Rasmussen7 found elevated neuroticism scores (Eysenck Personality Inventory8) and more frequent reports of fatigue and sleep problems in tension-type headache sufferers than controls, but she did not indicate whether these problems occurred disproportionately in the CTTH sufferers in her sample. In addition, psychiatric diagnoses were not made in the latter study so it cannot be determined whether elevations in neuroticism scores reflected complaints of fatigue, sleep problems, and other symptoms that commonly accompany frequent tension-type headaches,9 or whether there was an increased prevalence of psychiatric disorders.
Available information about the psychological correlates of CTTH is limited even in clinical samples. Studies using patient samples rarely distinguish ETTH and CTTH, although patient samples would be more likely to include CTTH sufferers than would samples from the general population. In both clinical and nonclinical samples, individuals with frequent tension-type headaches obtain higher scores on psychological symptom measures and on daily life stress measures than do healthy controls.10–12 However, it is unclear if elevations of psychological symptom measures reflect the presence of psychiatric disorders or the report of symptoms like fatigue and sleep disruption that commonly accompany frequent headaches even when no psychiatric disorder is present. In subspecialty headache treatment centers, half or more CTTH sufferers may receive anxiety or mood disorder diagnoses,5,6 indicating that these disorders are frequently comorbid with CTTH, at least in patients seen at such centers. However, comorbid psychiatric disorders may be one of the primary reasons why patients are referred to subspecialty centers; thus, CTTH sufferers seen in subspecialty centers are unlikely to be representative of CTTH sufferers seen in primary practice, let alone CTTH sufferers who do not receive treatment. The high prevalence of analgesic overuse headaches in patients at many subspecialty centers also makes the alternative hypothesis that psychiatric disorders are comorbid with analgesic overuse headaches, and not with CTTH, difficult to exclude.
The impact of CTTH on functioning is also poorly understood. In the one epidemiological study to report findings separately for CTTH and ETTH, Schwartz et al13 reported that almost 12% of CTTH sufferers in their population sample reported lost workdays due to headache, and 40% of these individuals reported 40 or more lost workdays in the last year. Thus, there is at least a subset of CTTH sufferers with quite high levels of work impairment and, presumably, impairments in other areas of their lives. In a subspecialty headache center sample, Solomon et al14 found that tension-type (N=41) headache sufferers exhibited equivalent or higher levels of impairment in social and role functioning, as assessed by the Medical Outcomes Study General Health Survey Short Form 20 (MOS-SF20) General Health Inventory,15 than did patients with migraine or comorbid migraine and tension-type headaches. If we make the assumption that CTTH sufferers tend to be more impaired than the ETTH sufferers, this would suggest particularly high levels of impairment for the subgroup of CTTH sufferers in their sample.
Studies that fail to distinguish episodic from chronic forms of tension-type headache may obscure other important differences between these two conditions. In the epidemiological study by Schwartz et al,13 ETTH and CTTH had different demographic and clinical correlates. For example, the female preponderance was greater in CTTH than in ETTH, and CTTH was most prevalent in individuals with less education and over 50 years of age, while ETTH was most prevalent in individuals with more education aged between 30 and 39 years. In addition, as might be expected, CTTH was much more likely than ETTH to be associated with a high number (>40 per year) of lost workdays. Interestingly, pain ratings were also higher for CTTH than for ETTH, suggesting that headache parameters may differ in CTTH and ETTH in ways not currently recognized by the IHS classification system.
In this study, we examine the characteristics of CTTH, the psychosocial correlates of this disorder, and assess the impact of CTTH on functioning and quality of life in patients similar to those seen in primary practice settings. We also identify specific patient characteristics that are associated with high levels of impairment.
SUBJECTS AND METHODS
Subjects
Individuals with frequent headaches were recruited from the general population in both urban (Columbus, Ohio and surrounding suburban areas) and rural (southern Ohio and western West Virginia) areas. Individuals who responded to announcements or advertisements for a clinical trial evaluating drug and nondrug therapies for chronic headache problems were evaluated at sites in either the Columbus area or in Athens, Ohio. Chronic tension-type headache sufferers were required to receive an IHS 2.2 diagnosis of CTTH and to have CTTH as their primary presenting problem, and not to receive an IHS 8.2 diagnosis (headache induced by chronic substance use or exposure)1 at each of two assessments: a neurological evaluation by a project neurologist and an independent structured diagnostic interview conducted by a second staff member. (Headache induced by chronic substance use was provisionally diagnosed if the patient was using 180 or more pills per month of a mild analgesic, 100 or more pills per month of an analgesic combined with barbiturates or other nonopiod compound, or an opiod analgesic, or if in the clinician's judgment of excessive analgesic use was likely to be aggravating the patient's headache problems.) In order to obtain an assessment of psychosocial correlates and the impact of CTTH in the absence of prophylactic or psychotropic therapies, the only participants who were evaluated were those who were not using antidepressant, mood-stabilizing, or other prophylactic headache medications, and were not regularly using tranquilizers at the time of the assessment. Finally, participants were required to record at least 15 headache days during 1 month of daily headache recordings to confirm the diagnosis of CTTH. The CTTH sample was predominately female (78%) and white (95%; 3% African American; 2% other ethnic background), with a mean age of 37 years (range, 17 to 65). The men were slightly older (mean, 41 years) than the women (mean, 36 years; t243 = 2.62, P=.009).
Healthy controls (N=89) were identified by CTTH sufferers from among their peers or had responded to advertisements for persons who did not experience problem headaches. Controls were paid $15 for completing a structured diagnostic interview, medical history, and psychosocial evaluation. Controls were required to report fewer than 10 headaches per year and to be free from chronic pain disorders. Controls did not differ significantly from CTTH sufferers in gender (78% female), age (mean, 38 years), or ethnic background (90% white, 5% African American, 5% other ethnic background).
Previously published data from the MOS are also reported for three comparison samples.16,17 Data from a representative sample from the US adult population (N=2008) assessed by telephone between August and October 1984 provided one comparison group; individuals with acute or chronic illnesses, as well as healthy individuals, were included in this sample. Comparison groups of patients who self-reported arthritis (N=2079) or back problems (N=486) were also obtained from the MOS data. These patients were seen by 1 of the 362 physician participants in the MOS in three cities (Boston, Chicago, and Los Angeles) during 9-day screening periods from February to October 1986. In each city, patients were sampled from one large HMO, numerous subspecialty groups, and a representative sample of solo practices. These data allow us to compare impairments observed in our sample of CTTH sufferers with impairments observed in both the general population and in relevant patient samples with other pain disorders; however, these comparisons are only approximate because the samples were acquired under different sampling procedures and are not matched demographically.
Evaluation
Headache Characteristics
The frequency and duration of headache episodes, as well as pain intensity, were assessed both by patient reports collected during the initial diagnostic and neurological evaluations and by 4 weeks of daily recording of headache activity. Headache history, medical history, and a detailed description of headache symptoms were collected in a 1- to 1 1/2-hour structured interview. Patients' reports of the typical frequency (days per week), duration (in hours with a maximum of 16 hours for unremitting headaches), and severity (0 = no pain to 10 = pain as bad as could be) of headache episodes were collected during this evaluation for comparison with daily recordings.
Patients recorded headache activity four times a day using a 10-point rating scale with five anchors that ranged from “no pain” to “extremely painful—I can't do anything when I have a headache.”18 The Headache Index (average of all diary ratings including zeros), the number of headache days (pain rating >1), and the number of days a headache of at least moderate severity (pain rating ≥5) was recorded provided measures of headache activity. Peak headache intensity ratings (for each week) were also averaged to provide a measure of peak pain intensity.
Psychological Correlates
PSYCHOLOGICAL SYMPTOMS
The Beck Depression Inventory (BDI)19 is a 21-item self-report measure that assesses symptoms of depression. The BDI is widely used in the assessment of individuals with recurrent headache disorders.11 Factor analysis of the BDI in individuals with headache problems reveals two factors: physical symptoms and cognitive/affective symptoms.9 Because physical symptoms (eg, insomnia) may be consequences of pain rather than symptoms of depression, it has been argued that cognitive/affective symptoms are a better indication of depression than physical symptoms.9 Therefore, scores were calculated separately for physical and cognitive/affective symptoms. The Trait Anxiety Scale (TA) of the State-Trait Anxiety Inventory20 is a 20-item self-report measure designed to assess relatively enduring symptoms of anxiety and is widely used in the assessment of individuals with recurrent headache problems.11
The Primary Care Evaluation for Mental Disorders (Prime MD)21 is designed to facilitate the diagnosis of psychiatric disorders commonly seen in medical settings. It includes a patient-completed questionnaire of key symptoms and a clinician-administered structured interview (Clinician Evaluation Guide), which yield a subset of diagnoses included in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).21 Diagnoses of the most commonly encountered mood (major depressive disorder, dysthymia, and minor depressive disorder) and anxiety disorders (panic disorder, generalized anxiety disorder, and anxiety disorder not otherwise specified [NOS]) were made by psychologists using the Prime MD Mood and Anxiety Modules. The two subclinical diagnoses (minor depression and anxiety disorder NOS) have slightly more liberal diagnostic criteria in the Prime MD than in the DSM-IV. Essentially, these two subclinical diagnoses are coded when symptoms of depression or anxiety are of significant magnitude to warrant clinical attention, but they do not satisfy criteria for one of the clinical diagnostic categories included in the Prime MD.
DAILY LIFE STRESS
The Hassles Scale-Short Form is an abbreviated version of the Daily Hassles Scale,22 which is designed to assess common everyday life stresses. The Hassles Scale-SF consists of 42 items: the 6 highest loading items from each of 6 Hassles Scale factors (inner concerns, financial concerns, time pressures, work hassles, environmental hassles, family hassles) plus an additional more generally worded item written for each factor.23 Items from the health hassles factor were excluded, as these items were likely to directly reflect headache problems rather than other sources of stress in the individual's life. For each item, respondents indicate whether they experienced the stressor and, if they did experience it, they rate the severity of the stressor on a scale from 1 (“not severe”) to 5 (“extremely severe”).
Functioning/Quality of Life
MEDICAL OUTCOMES STUDY GENERAL HEALTH SURVEY
The MOS-SF2015,17,24 is an abbreviated form of the full-length MOS Health Survey, which was designed to assess the impact of chronic disease on quality of life.25–27 The MOS-SF20 consists of 20 items designed to assess the impact of health problems in six areas. Of interest in assessing headache impact were three subscales designed to assess the impact of health problems on functional status: physical functioning (tasks of daily living), role functioning (work/school/home), and social functioning (social/recreational). In addition, a mental health subscale provides a measure of psychological symptoms (anxiety/depression), and the pain subscale provides a global pain measure assessing limitations associated with bodily pain. Subscales are scaled so that higher scores indicate less impairment, with a score of 100 indicating the absence of impairment. Detailed psychometric information has been reported on this instrument as part of the medical outcomes study.15,24
DISABILITY DAYS/IMPAIRMENT RATINGS
Headache-related disability and impairment in work and social/recreational activities were assessed with four questions developed for this purpose by Von Korff et al.28 Disability days were assessed by the following question: How many days in the last 6 months have you been kept from your usual activities (work, school, or housework) because of headaches? Impaired functioning was assessed by the following three questions rated on a 0 to 10 scale where 0 was “no interference” and 10 was “unable to carry out any activities”: (1) In the past 6 months, how much have your headaches interfered with your daily activities? (2) In the past 6 months, how much have your headaches interfered with your ability to take part in recreational, social, and family activities? and (3) In the past 6 months, how much have your headaches interfered with your ability to work (including housework)? Two additional questions inquired about the severity of the patient's typical headache and the patient's worst headache in the last 6 months and were rated on a 0 to 10 scale, where 0 was “no pain” and 10 was “pain as bad as it could be.” Ratings of 1 to 3 were categorized as mild impairment, 4 to 7 as moderate impairment, and 8 to 10 as severe impairment. A composite of the three items provided an overall measure of impairment. The three items had similar standard deviations, means, and were intercorrelated (r=.76 to .84). Cronbach α for the resulting three-item scale was .92.
RECURRENT ILLNESS IMPACT PROFILE
Recurrent Illness Impact Recordings (RIIR)29 were completed weekly for 1 month. Respondents recorded the number of days each week their functioning in each of 12 areas (eg, work or school performance, leisure activities) was impaired by headaches. The internal consistency (Cronbach α=.94) and the split half reliability (Spearman-Brown=.84) of the 12 items on this instrument were high. Stability across a 1-month period was also relatively high (r=.83), given that scores were likely to vary with the occurrence of headaches.
RESULTS
Headache Characteristics
Diagnostic Evaluation
All patients were required to receive a CTTH diagnosis and to identify tension-type headaches as their primary headache problem, however, 28% of patients also received a concurrent migraine diagnosis. Patients with CTTH reported an average 12-year (mean, 148 months) history of problem headaches with headaches occurring at the current frequency for more than 7 years (mean, 86 months). Approximately two thirds of patients (67%) reported a family history of problem headaches. Stress was the most frequently reported headache trigger (88% of patients), but diet (33% of patients) and menstrual cycle (34% of women) were also reported as triggers by a significant subset of patients. These three headache triggers were equally likely to be reported by patients who received a comorbid migraine diagnosis and by patients who received only a CTTH diagnosis.
Headache Recordings
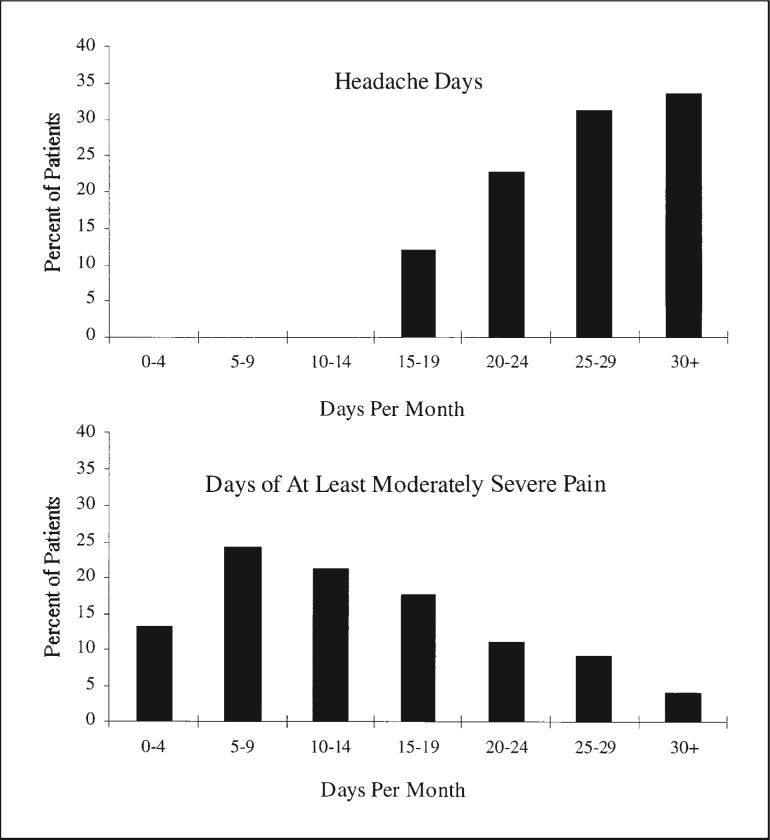
Daily diary data presented in Figure 1 describe the typology of CTTH. It can be seen that about two thirds (65%) of patients recorded daily or near daily headaches (25 days or more per month), and only a small number (12%) recorded fewer than 20 headache days per month. Thus, headaches were the norm.
Fig 1.
Number of days per month that patients with CTTH recorded headaches (top) and recorded at least moderately severe (pain rating ≥5) headaches (bottom).
Although headaches occurred nearly every day for most patients, the level of pain was quite variable across headache days. Only one patient recorded mild pain (<5 on a 10-point scale) on all headache days, and only a small number (4%) of patients recorded pain of at least moderate severity (≥5) every headache day. On average, patients recorded pain of at least moderate intensity on about half (52%) of their headache days. Pain of this intensity was recorded 10 or more days a month by a majority (63%) of patients and 15 or more days per month by over 40% of patients.
For most patients (58%), the average weekly peak intensity fell between 6 (“painful—but I can continue what I am doing”) and 8 (“very painful—my pain makes concentration difficult but I can perform undemanding tasks”), with 28% of patients recording lower peak intensities and 14% reporting higher peak intensities. Only 4.1% of patients tended to record severe pain at some point each week (average peak intensity ≥9), and 30% of these patients received a comorbid migraine diagnosis. This percentage did not differ from the percentage of patients in the total sample (28%) with a comorbid migraine diagnosis. A subset of patients with a confirmed CTTH diagnosis thus recorded severe pain at some point in the week.
The frequency of headaches assessed by patients' daily diary recordings and as reported by patients during the diagnostic evaluation were moderately correlated (r=.46). On average, diaries revealed more frequent headache days (mean, 6.1 per week) than were reported by patients in the diagnostic interview (mean, 5.3; t243=8.9, P<.001).
Health Care Behavior
Most CTTH sufferers (79%) reported having consulted a physician for their headache problems. However, the median time since the last consultation was 9 months. About half (54%) of the individuals who had consulted a physician could be considered lapsed consulters,30 defined here as not having consulted in at least 6 months despite persistent headache problems. Individuals who had consulted a physician in the last 6 months for their headaches generally had consulted their primary care physician (81% of consulters). Fifteen percent of patients consulted a nonmedical health professional for headache treatment in the past 6 months, with consultations reported most frequently with chiropractors (57% of nonmedical consultations ) and massage therapists (40% of nonmedical consultations). Only about 1 in 5 patients (19%) who consulted a nonmedical health professional also consulted a physician in the previous 6 months.
Those with CTTH who had consulted a health care professional in the previous 6 months appeared to have only slightly more severe headache problems than individuals who had not consulted in the last 6 months. Consulters recorded more headache days per month (mean, 27 versus mean, 25 t243=3.72, P<.001) and more days of at least moderate severity headaches (mean, 15 versus mean, 13, t243=2.11, P=.035), but they did not report a longer history of headache problems. However, there were no significant differences between CTTH sufferers who had consulted a health care professional in the last 6 months and patients who had not consulted in receipt of anxiety or mood diagnoses or in reports of psychological symptoms on the BDI or TA scales.
Psychological Correlates
It can be seen in Table 2 that CTTH sufferers reported higher levels of daily life stress than controls on the Hassles Scale-SF. Chronic tension-type headache sufferers not only reported a greater number of daily stresses but also rated the daily stresses they had encountered as more stressful (mean, 2.0) than did controls (mean, 1.5, t327= 6.03, P<.001). On all six Hassles Scale-SF subscales, CTTH sufferers reported a greater number of stressful events and rated the stressful events they experienced as more severe than controls. Male and female CTTH sufferers did not differ in the number of daily life stressors they reported. However, female CTTH sufferers rated the stresses they experienced as more stressful (mean, 2.0) than did male CTTH sufferers (mean, 1.8, t238=2.31, P=.022).
Table 2.
Psychological Measures: Chronic Tension-type Headache Sufferers and Control Subjects
| Chronic Tension-type Headache |
Control |
|||||
|---|---|---|---|---|---|---|
| Instrument | Mean (SD) | N | Mean (SD) | N | z | P |
| Beck Depression Inventory | 8.9 (6.6) | 245 | 4.8 (7.2) | 89 | 6.69 | <.001 |
| Trait Anxiety Inventory | 41.9 (10.4) | 245 | 31.2 (7.8) | 89 | 8.29 | <.001 |
| Hassles-SF total score | 54.6 (27.0) | 240 | 34.1 (20.7) | 89 | 6.44 | <.001 |
| Prime MD diagnosis | % Patients | N | % Patients | N | χ2 (df) | P |
|---|---|---|---|---|---|---|
| Mood or anxiety disorder | 45.5 | 242 | 9.0 | 89 | 37.72 (1) | <.001 |
| Prime mood disorder | 28.9 | 242 | 7.9 | 89 | 16.17 (1) | <.001 |
| Prime anxiety disorder | 34.7 | 242 | 2.2 | 89 | 35.66 (1) | <.001 |
Wilcoxon-Mann-Whitney U test.
Prime MD indicates Primary Care Evaluation for Mental Disorders.
Beck Depression Inventory total scores (and both the cognitive and somatic subscale scores) and TA scale scores were also elevated in CTTH sufferers relative to healthy controls (see Table 2). The average BDI and TA scores were elevated by about a standard deviation for the CTTH sufferers. Females reported a higher BDI (mean, 9.6 versus mean, 6.6, t243=2.93, P=.004) and TA scores (mean, 42.7 versus mean, 9.4, t243=2.07, P=.040) than males. Prime MD diagnoses of anxiety and mood disorders were 3 to 15 times as frequent in CTTH sufferers than in matched controls (see Table 2). If diagnoses of minor depression and anxiety NOS are excluded, these differences are somewhat less dramatic with 21% of CTTH receiving a depression diagnosis, 17% received an anxiety diagnosis, and about a third of patients (31%) receiving at least one diagnosis. Nonetheless, Prime MD data suggest that the symptoms of anxiety or depression, or both, were of sufficient magnitude to require attention in headache management efforts in about half of CTTH sufferers.
Among the 70 patients who received a mood disorder diagnosis, BDI scores were moderately (mean, 15.6) elevated, with 26% of patients obtaining sufficiently elevated scores (≥19) to suggest at least moderately severe depression. Only 5% of patients obtained BDI scores greater than 29, suggesting severe depression.31 It, thus, appears that the observed depression levels were typically mild to moderate in severity. Among patients who received an anxiety disorder diagnosis, TA scores were elevated (mean, 48.0) about one standard deviation above the mean reported for a normative sample (mean, 37.9) and were similar to scores reported for patients in psychiatric settings with anxiety disorder diagnoses (mean, 49.0).20 The mean for all CTTH sufferers in our sample (41.9) was similar to the mean previously reported for general medical and surgical patients (41.9). Thus, CTTH sufferers who received anxiety disorder diagnoses reported anxiety levels that were sufficiently high to impair functioning.
Headache Impact
Medical Outcomes Study General Health Survey Short Form
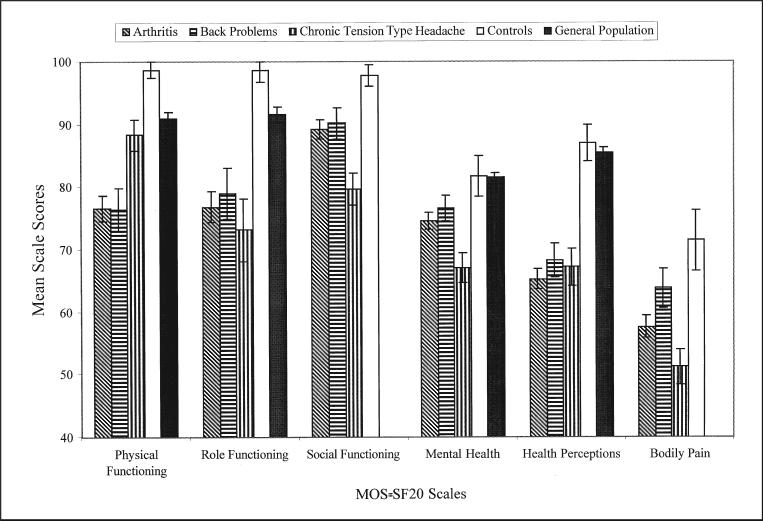
In Figure 2, it can be seen that CTTH sufferers obtained lower scores than controls on all six MOS-SF20 subscales (P<.001), suggesting that CTTH has a broad negative impact on quality of life. Table 3 presents the proportion of individuals who met MOS criteria for impairment for CTTH sufferers and for two available comparison samples. It can be seen that in 5 of the 6 areas assessed by the MOS-SF20, over 40% of CTTH sufferers were classified as impaired; in contrast, controls were rarely identified as impaired. Furthermore, the majority of CTTH sufferers (62%), but few controls (9%), met the criteria for impaired functioning on the physical, role, or social functioning subscales. Thus, CTTH was commonly associated with impairments in daily activities of living. When compared with the MOS national reference sample from the general population, CTTH sufferers were two to five times more likely to be classified as impaired.
Fig 2.
Means for MOS-SF20 subscales with error bars displaying the standard error of the mean. Lower scores indicate greater impairment. Data for the general population and for patients with arthritis and back problems come from the Medical Outcomes Study.16,17 The pain and social functioning scales were not reported for the general population.
Table 3.
Percentage of Patients Impaired on the Medical Outcomes Study (MOS) Short Form 20
| MOS Scale | Chronic Tension-type Headache (N=245) | Controls (N=89) | General Population (N=2008) |
|---|---|---|---|
| Physical Functioning | 44.5 | 7.9 | 22 |
| Role Functioning | 44.5 | 3.4 | 12 |
| Social Functioning | 8.2 | 0.0 | NA |
| Mental Health | 44.5 | 11.2 | 19 |
| Health Perceptions | 50.6 | 13.5 | 20 |
| Bodily Pain | 54.3 | 13.5 | NA |
The percentages of impaired subjects were significantly higher for chronic tension-type headache sufferers than for controls and the general population on all MOS scales. The percentages of impaired subjects were significantly higher in the general population than controls on physical and role functioning scales only. The chi-square test for independence was used to test differences at the .05 level. The general population data and disability cutoffs are taken from Stewart et al.15
Figure 2 also presents previously published data from the MOS for two additional comparison groups. Although any comparison with our data is only approximate, it can be seen that CTTH sufferers appear to exhibit levels of impairment that are similar to or greater than the impairments exhibited by patients with arthritis and back problems. As might be expected, self-care activities assessed by the physical functioning subscale were relatively unimpaired in CTTH, however, significant impairments were evident on all the remaining subscales, with CTTH sufferers exhibiting high levels of impairment even relative to the arthritis and back pain samples on the social functioning, mental health, and bodily pain subscales.
Disability Days and Impairment Ratings
Patients reported that headaches kept them from work or from their usual activities for an average of 7.0 days (median, 4.0 days) in the last 6 months, with 74% of patients reporting at least 1 disability day. Only 18% of the patients reported 12 or more disability days in the last 6 months, but this small group of patients averaged 24 disability days in the previous 6 months and accounted for a disproportionate share (61%) of total disability days.
The moderate intensity but persistent pain characteristic of CTTH might be expected to impair functioning without necessarily forcing the cancellation of work or social activities. Consistent with this possibility, fewer than 1 in 10 (7%) patients indicated that headaches had not impaired their work performance, with even fewer (4%) patients indicating that headaches had not impaired social functioning. Most (60%) patients who indicated that their headaches impaired their work performance rated this impairment as moderate in severity; only 6% rated their work performance as severely impaired. Similarly, most (57%) patients who indicated that their social functioning was impaired by their headaches rated this impairment as moderate in severity; only 9% rated their social functioning as severely impaired.
Recurrent Illness Impact Profiles
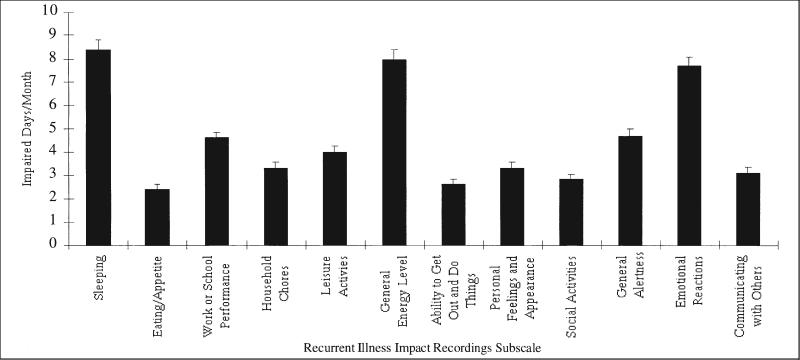
It can be seen in Figure 3 that patients' weekly recordings revealed that CTTH has the greatest impact on patients' quality of life in three areas: sleep, energy level, and emotional well-being. In each area, CTTH sufferers recorded on average about 8 days of impairment per month. However, patients recorded at least 2 days of impairment per month in every area assessed, confirming that CTTH had an impact on all areas of the patients' lives that were assessed by the RIIR. A subset of patients recorded impairments in functioning 10 days per month or more. This level of impairment was most frequently recorded in the areas of sleep (37% of patients), energy (35%), and emotional well-being (33%). Relatively few (6% to 13%) patients recorded this level of impairment in the other areas that were assessed.
Fig 3.
Recurrent Illness Impact Recordings scores for CTTH sufferers. The error bars represent the standard error of the mean.
Determinants of Headache Impact
We examined the ability of demographic, headache, and psychological variables to predict impairment. Demographic variables (age, gender), headache severity (Headache Index, concurrent migraine diagnosis), and affective distress (TA, Prime MD diagnosis) were examined as predictors of impairment in backward regressions conducted on four impairment measures. The results are presented in Table 4*.
Table 4.
Results of Regression Analyses
| Solution |
|||||||
|---|---|---|---|---|---|---|---|
| Dependent Variable | R2 | F | P | Variables | Beta | t | P |
| MOS-20* (n=242) | .22 | 13.70 | <.001 | Trait Anxiety | −.25 | 3.56 | <.001 |
| Migraine Dx | −.18 | 3.13 | .002 | ||||
| Prime MD Dx | −.16 | 2.38 | .018 | ||||
| Headache Index | −.15 | 2.59 | .010 | ||||
| Age | .10 | 1.73 | .084 | ||||
| RIIR (n=240) | .41 | 53.79 | <.001 | Headache Index | .35 | 6.81 | <.001 |
| Trait Anxiety | .31 | 5.23 | <.001 | ||||
| Prime MD Dx | .23 | 3.92 | <.001 | ||||
| Interference (n=240) | .15 | 13.88 | <.001 | Headache Index | .24 | 4.02 | <.001 |
| Prime MD Dx | .24 | 3.93 | <.001 | ||||
| Gender | −.16 | 2.58 | .010 | ||||
| Disability Days** (n=235) | .11 | 9.31 | <.001 | Gender | −.25 | 3.99 | <.001 |
| Headache Index | .17 | 2.76 | .006 | ||||
| Prime MD Dx | .13 | 2.16 | .032 | ||||
Gender is coded 1 for female and 2 for male. Prime MD Dx and Migraine are coded 0 for absent and 1 for present.
The Pain and Mental Health Subscales are not included in this MOS-SF20 total score because they were redundant with predictor variables.
Because the disability days variable was highly skewed a log10(X+1) transformation was used on this variable.
It can be seen that high levels of headache activity and high levels of affective distress were associated with greater impairment in every analysis, indicating that these variables are two important determinants of headache impact. In contrast, comorbid migraine diagnosis was relatively unimportant, being associated with only one impairment measure, the MOS-SF20. Similarly, gender (female) was predictive of disability days and, to a lesser extent, ratings of impaired functioning, but not of other measures of headache impact. Over 40% of the variance in weekly recordings of headache-related impairment (RIIR) and 20% of the variance in MOS-SF20 scores could be explained by the variables of interest, however, only a relatively small portion (15% or less) of the variance in disability days and in impairment ratings was explained by the same predictor variables.
COMMENTS
Daily diary data were used to describe the typology of headaches experienced by individuals with a primary presenting problem of CTTH. Two thirds of CTTH sufferers recorded headaches every day or nearly every day (at least 25 days per month), and only a small minority recorded headaches on fewer than 20 days per month. Thus, headaches were the norm for most individuals. Headaches also tended to vary in severity. It was rare for an individual to experience just mildly painful headaches or just to experience headaches that were at least moderately painful. However, headaches with pain of at least moderate severity were recorded, on average, on about half of an individual's headache days. Thus, while pain typically varied in intensity, headaches frequently were sufficiently painful that normal activities would be impaired or require extra effort. Comparison of our data with data from a recent population sample13 suggests that participants in this study experienced more frequent and more painful headaches than is typical in the population of CTTH sufferers. However, this apparent difference in headache severity may also reflect the fact that headache parameters were assessed by daily headache diaries here and by telephone interviews in the above epidemiological survey.
Chronic tension-type headaches appeared to have a pervasive negative impact on patients' lives but severely impaired functioning in only a minority of individuals. Irrespective of whether headache impact was assessed by standard quality-of-life measures, by reported disability days, or by weekly records kept by patients, the negative impact of CTTH on quality of life was clearly evident. Thus, CTTH sufferers were seven times more likely than were controls to be classified as impaired on the subscales measuring physical, social, or role functioning of the MOS-SF20. Impairments exhibited by CTTH sufferers on the MOS-SF20 also appeared to be similar to or greater than impairments exhibited by patients with arthritis or back problems. About three quarters of CTTH sufferers reported being kept from their normal activities by headaches at some time in the last 6 months. Nonetheless, CTTH sufferers did not usually discontinue work or other activities when they experienced headaches. Over half of the CTTH sufferers also rated their work and social functioning as mildly or moderately impaired rather than as severely impaired by headaches.
Information from patients' weekly headache impact recordings provided additional details about the areas where CTTH was most likely to have an impact on patients' lives, but the overall picture of headache impact obtained from daily recordings was largely consistent with findings from other measures. Thus, headache-related impairments were recorded in all 12 areas of patient functioning that were assessed at some time during the 1-month recording period, providing additional evidence of the pervasive impact of CTTH on patients' lives. However, impairments were recorded most frequently in sleep, energy level, and emotional well-being (where patients recorded an average of 8 days impaired functioning per month) and less frequently in other areas of the patients' lives such as work or school performance. The high level of sleep disturbance observed here in CTTH is consistent with findings from other studies.32 Thus, the picture of the CTTH sufferer that emerges from our data is one of an individual who, most of the time, continues to carry out daily life responsibilities when in pain, although role performance is sometimes impaired by headaches and well-being is frequently impaired.
In a minority of patients, CTTH was associated with severe impairments in functioning. While fewer than 1 in 5 patients reported more than 12 headache-related disability days in the last 6 months, these individuals averaged 24 disability days in this period and, thus, these individuals contributed disproportionately to total disability days. A third of patients recorded headache-related impairment of sleep, energy level, or emotional well-being on 10 or more days a month. This suggests that emotional well-being is more frequently impaired in CTTH than is role performance.
The prevalence of anxiety and mood disorders was strikingly elevated in CTTH sufferers, with almost half of CTTH sufferers, but less than 10% of controls, qualifying for an anxiety or mood disorder diagnosis. If subclinical diagnoses of minor depression and anxiety disorder NOS are excluded, about a third of CTTH sufferers and 2% of controls qualified for one of the remaining anxiety and mood disorder diagnoses. In either case, affective distress was such a prominent correlate of CTTH as to argue for careful attention to symptoms of anxiety and depression in the evaluation of CTTH (see Holroyd et al33 for a discussion of the affective distress construct). Fortunately, symptoms were often mild or moderate in severity. For example, almost 75% of patients who received a mood disorder diagnosis obtained BDI scores in the mild depression range. This figure may underestimate the severity of depression in a few patients who may hesitate to acknowledge psychological symptoms on self-report inventories. However, for many individuals, symptoms of anxiety and depression are likely to be subtle and not easily articulated. As a result, these affective symptoms may be easily overlooked in patients who present with headache as the more salient problem. It should also be kept in mind that mild or moderate levels of depressive symptoms are associated with significant impairments in functioning in patients seen in primary practice settings.34,35 Consistent with these observations, the mild-to-moderate symptoms of depression and anxiety observed here also appeared to be associated with notable impairments in functioning.
Affective distress as well as the severity of headaches (Headache Index) appeared to be an important determinant of the impact CTTH has on patients' lives. Irrespective of the type of measure used to assess headache impact, impairment was observed to increase with higher levels of headache activity and with higher levels of affective distress. Consequently, patients with near daily headaches who received a comorbid anxiety or mood disorder diagnosis were frequently classified as impaired on the MOS-SF20, with 96% of these patients classified as impaired on at least one MOS-SF20 subscale. Nonetheless, the patient variables we examined accounted for a moderate 10% to 40% of the variance in our headache impact measures, so other factors are also likely to be important in determining the impact of headaches on patients' lives. Disability days, in particular, were only weakly related to either headache activity or affective distress. It may be that environmental factors such as available social support for disability or demands and incentives for performance are more important in influencing actual disability days than the variables we examined. Overall, however, our findings suggest that if treatment is to remedy impairments in functioning, then affective distress, as well as pain, will need to be addressed.
There are several limitations to the present study. First, patients were seeking treatment in response to announcements for a clinical trial. Although our recruitment process was designed to yield as broad a range of patients as possible with CTTH as their primary presenting problem, and sample characteristics suggested that we were successful in recruiting a patient sample similar to those seen in many primary practice settings, it is not a randomly selected sample from a well-defined population. Measures of headache impact, whether they were standardized measures such as the MOS-SF20, weekly recordings, or patient ratings, relied on patient report. We did not have access to work records, nor were we able to collect behavioral observations of patients in their natural environment with which to verify data provided by patients. Finally, because our data are correlational, it cannot be concluded with certainty that headache severity or affective distress caused associated impairments in functioning; it is at least theoretically possible that impairments in functioning aggravated both headaches and affective distress or that all three problems were caused by a third factor.
Despite the above limitations, the present findings provide a more comprehensive description of the CTTH sufferers seen in primary care settings than has previously been available. It appears that CTTH sufferers experience more disability than previously thought, rivaling the disability seen in back pain and arthritis sufferers. Most patients reported near daily headaches with about half of these being of moderate or severe intensity. With this high level of pain, most CTTH sufferers had consulted a physician concerning their headaches, but just over half of these patients had lapsed from treatment (had not consulted in the past 6 months despite near daily headache). The majority of CTTH sufferers reported some functional impairment, usually of moderate severity. Common areas of impairment appear to be emotional well-being, sleep disturbance, and energy level. Consistent with these areas of impairment is the striking finding that close to half of the patients experienced either a mood or anxiety disorder. In conclusion, our data suggest that CTTH has a greater impact on individuals' lives than has generally been appreciated, with affective distress being an important correlate of impairment. Thus, if treatment is to remedy impairments in functioning, affective distress, as well as pain, will often need to be addressed.
Acknowledgments
Support for this research was provided in part by a grant from The National Institutes of Health (NINDS # NS32374). Appreciation is expressed to Mary Katherine Davis, Douglas French, Peter Malinoski, Adriana Meade, Angela Nicolosi, Carol Nogrady, Cornelia Pinnell, France Talbot, Robert Trombley, and Sharon Waller.
Abbreviations
- ETTH
episodic tension-type headache
- CTTH
chronic tension-type headache
- MOS-SF20
Medical Outcomes Study General Health Survey Short Form
- BDI
Beck Depression Inventory
- TA
Trait Anxiety Scale
- Prime MD
Primary Care Evaluation for Mental Disorders
- NOS
not otherwise specified
Footnotes
Because the Trait Anxiety Scale and the Beck Depression Inventory yielded overlapping information when included in the regression analysis only one of the measures was included.
REFERENCES
- 1.Headache Classification Committee of the International Headache Society Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988;8(suppl 7):1–96. [PubMed] [Google Scholar]
- 2.Merikangas KR, Stevens DE, Angst J. Psychopathology and headache syndromes in the community. Headache. 1994;34:517–522. doi: 10.1111/j.1526-4610.1994.hed3408s17.x. [published correction appears in Headache. 1995;35:preceding table of contents] [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, Stevens DE, Angst J. Headache and personality: results of a community sample of young adults. J Psychiatr Res. 1993;27:187–196. doi: 10.1016/0022-3956(93)90007-o. [DOI] [PubMed] [Google Scholar]
- 4.Derogatis RL. R-version Manual 1: Scoring, Administration, and Procedures for the SCL-90. Johns Hopkins University Press; Baltimore: 1977. Symptom Checklist 90. [Google Scholar]
- 5.Guidetti V, Galli F, Fabrizi P, et al. Headache and psychiatric comorbidity: clinical aspects and outcome in an 8-year follow-up study. Cephalalgia. 1998;18:455–462. doi: 10.1046/j.1468-2982.1998.1807455.x. [DOI] [PubMed] [Google Scholar]
- 6.Goncalves JA, Monteiro P. Psychiatric analysis of patients with tension-type headache. In: Olesen J, Schoenen J, editors. Tension-type Headache: Classification, Mechanisms, and Treatment. New York; Raven Press: 1993. pp. 167–172. [Google Scholar]
- 7.Rasmussen BK. Migraine and tension-type headache in a general population: psychosocial factors. Int J Epidemiol. 1992;21:1138–1143. doi: 10.1093/ije/21.6.1138. [DOI] [PubMed] [Google Scholar]
- 8.Eysenck HJ, Eysenck SB. Manual of the Eysenck Personality Questionnaire. Hodder and Stoughton; London: 1975. [Google Scholar]
- 9.Holm JE, Penzien DB, Holroyd KA, Brown TA. Headache and depression: confounding effects of transdiagnostic symptoms. Headache. 1994;34:418–423. doi: 10.1111/j.1526-4610.1994.hed3407418.x. [DOI] [PubMed] [Google Scholar]
- 10.Andrasik F, Blanchard EB, Arena JG, Teders SJ, Teevan RC, Rodichok LD. Psychological functioning in headache sufferers. Psychosom Med. 1982;44:171–182. doi: 10.1097/00006842-198205000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Penzien DB, Rains JC, Holroyd KA. Psychological assessment of the recurrent headache sufferer. In: Tollison CD, Kunkel RS, editors. Headache: Diagnosis and Treatment. Williams and Wilkins; Baltimore: 1993. pp. 39–49. [Google Scholar]
- 12.Holm JE, Holroyd KA, Hursey KG, Penzien DB. The role of stress in recurrent tension headache. Headache. 1986;26:160–167. doi: 10.1111/j.1526-4610.1986.hed2604160.x. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA. 1998;279:381–383. doi: 10.1001/jama.279.5.381. [DOI] [PubMed] [Google Scholar]
- 14.Solomon GD, Skobieranda FG, Gragg LA. Does quality of life differ among headache diagnoses? Analysis using the medical outcomes study instrument. Headache. 1994;34:143–147. doi: 10.1111/j.1526-4610.1994.hed3403143.x. [DOI] [PubMed] [Google Scholar]
- 15.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262:907–913. [published correction appears in JAMA. 1989;262:2542] [PubMed] [Google Scholar]
- 17.Ware JE, Nelson EC, Sherbourne CD, Stewart A. Developing and testing the MOS 20-item Short-Form Health Survey: a general population application. In: Stewart AL, Ware JE, editors. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Duke University Press; Durham, NC: 1992. pp. 277–290. [Google Scholar]
- 18.Holroyd KA, Nash JM, Pingel JD, Cordingley GE, Jerome A. A comparison of pharmacological (amitriptyline HCL) and nonpharmacological (cognitive-behavioral) therapies for chronic tension headaches. J Consult Clin Psychol. 1991;59:387–393. doi: 10.1037//0022-006x.59.3.387. [DOI] [PubMed] [Google Scholar]
- 19.Beck AT, Steer RA. Beck Depression Inventory Manual. Psychological Corp; New York: 1987. [Google Scholar]
- 20.Spielberger CD, Jacobs G, Crane R, et al. State-Trait Personality Inventory. University of South Florida Human Resources Institute; Tampa: 1979. [Google Scholar]
- 21.Spitzer AL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-111-R. American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- 22.Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: daily hassles and uplifts versus major life events. J Behav Med. 1981;4:1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- 23.Holm J, Holroyd KA. The Daily Hassles Scale (revised): does it measure stress or symptoms? Behav Assess. 1992;14:465–482. [Google Scholar]
- 24.Ware JE, Sherbourne CD, Davis AR. Developing and testing the MOS 20-item short form health survey: a general population application. In: Stewart AL, Ware JE, editors. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Duke University Press; Durham, NC: 1992. [Google Scholar]
- 25.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 26.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 28.Von Korff M, Stewart WF, Lipton RB. Assessing headache severity. New directions. Neurology. 1994;44(suppl 4):S40–S46. [PubMed] [Google Scholar]
- 29.Holroyd KA, France JA, Rokicki L. Assessing the impact of recurrent pain on quality of life: illness impact recordings. Ann Behav Med. 1994;16(suppl):S064. [Google Scholar]
- 30.Edmeads J, Findlay H, Tugwell P, Pryse-Phillips W, Nelson RF, Murray TJ. Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use: a Canadian population survey. Can J Neurol Sci. 1993;20:131–137. doi: 10.1017/s0317167100047697. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 32.Monteiro P, Barros J, Correia P, Pinheiro J. Sleep and tension-type headaches. In: Olesen J, Schoenen J, editors. Tension-Type Headache: Classification, Mechanisms, and Treatment. Raven Press; New York: 1993. pp. 201–206. [Google Scholar]
- 33.Holroyd KA, Malinoski P, Davis MK, Lipchik GL. The three dimensions of headache impact: pain, disability and affective distress. Pain. 1999;83:571–578. doi: 10.1016/s0304-3959(99)00165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Katon W, Lin E, Von Korff M, et al. The predictors of persistence of depression in primary care. J Affect Disord. 1994;31:81–90. doi: 10.1016/0165-0327(94)90111-2. [DOI] [PubMed] [Google Scholar]
- 35.Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA. 1989;262:914–919. [PubMed] [Google Scholar]