Abstract
Objective To summarise the long term efficacy of anti-obesity drugs in reducing weight and improving health status.
Design Updated meta-analysis of randomised trials.
Data sources Medline, Embase, the Cochrane controlled trials register, the Current Science meta-register of controlled trials, and reference lists of identified articles. All data sources were searched from December 2002 (end date of last search) to December 2006.
Studies reviewed Double blind randomised placebo controlled trials of approved anti-obesity dugs used in adults (age over 18) for one year or longer.
Results 30 trials of one to four years’ duration met the inclusion criteria: 16 orlistat (n=10 631 participants), 10 sibutramine (n=2623), and four rimonabant (n=6365). Of these, 14 trials were new and 16 had previously been identified. Attrition rates averaged 30-40%. Compared with placebo, orlistat reduced weight by 2.9 kg (95% confidence interval 2.5 kg to 3.2 kg), sibutramine by 4.2 kg (3.6 kg to 4.7 kg), and rimonabant by 4.7 kg (4.1 kg to 5.3 kg). Patients receiving active drug treatment were significantly more likely to achieve 5% and 10% weight loss thresholds. Orlistat reduced the incidence of diabetes and improved concentrations of total cholesterol and low density lipoprotein cholesterol, blood pressure, and glycaemic control in patients with diabetes but increased rates of gastrointestinal side effects and slightly lowered concentrations of high density lipoprotein. Sibutramine lowered concentrations of high density lipoprotein cholesterol and triglycerides but raised blood pressure and pulse rate. Rimonabant improved concentrations of high density lipoprotein cholesterol and triglycerides, blood pressure, and glycaemic control in patients with diabetes but increased the risk of mood disorders.
Conclusions Orlistat, sibutramine, and rimonabant modestly reduce weight, have differing effects on cardiovascular risk profiles, and have specific adverse effects.
Introduction
Obesity and overweight are highly and increasingly prevalent chronic conditions currently affecting over 1.1 billion individuals worldwide and are associated with premature mortality, chronic morbidity, and increased healthcare use.1 2 Recently published guidelines recommend lifestyle modification as the initial treatment for obesity and suggest that adjunctive drug treatment is considered in patients with a body mass index ≥30 or 27-29.9 with medically complicated obesity.2 Orlistat, a gastrointestinal lipase inhibitor, sibutramine, a centrally acting monoamine reuptake inhibitor, and rimonabant, an endocannabinoid receptor antagonist, are approved for long term treatment of obesity (one year or more).3
Treatment with anti-obesity drugs is common, with global sales in 2005 estimated at $1.2bn.4 As weight losses achieved with lifestyle intervention are modest and limited by high rates of recidivism and compensatory slowing of metabolism,5 6 there is potential for even greater use of drug treatment. Furthermore, as the prevalence and incidence of obesity grow and as newer agents are developed, use of these drugs will probably increase further.
We carried out an updated systematic review and meta-analysis to quantify the efficacy of and adverse effects associated with the long term use of anti-obesity drugs. This paper is a summary of a recently updated Cochrane collaboration systematic review.7
Methods
Inclusion and exclusion criteria and outcomes
With the help of a medical librarian we searched Medline, Embase, the Cochrane controlled trials register, and the metaregister of controlled trials (www.controlled-trials.com) from December 2002 to December 2006 and examined reference lists of identified articles. In the original version of this review, the search covered the period from the inception of each database to December 2002.8 We searched for placebo controlled clinical trials of at least one year in duration that evaluated the effects of anti-obesity drugs on weight, cardiovascular risk factors, cardiovascular morbidity and mortality, and overall mortality. A subgroup analysis examined weight loss and glycaemic control in patients with type 2 diabetes. All trials had to be double blind (patient and care provider) randomised controlled trials examining overweight or obese adults (age 18 years or over) that used intention to treat analysis. Quasi-randomised, open label crossover trials and studies published only in abstract form were not included. There were no language restrictions.
Selection and data extraction
Two unblinded reviewers performed electronic searches and screened the initial results. Articles that clearly did not meet inclusion criteria were rejected on initial review. If uncertainty existed, the full text of the article was reviewed. Two reviewers independently assessed all potentially relevant studies for inclusion and extracted and recorded data. Disagreements were resolved by consensus. Agreement between raters was assessed with Cohen’s κ coefficient. If the published article provided inadequate information for a given end point, we contacted the primary author. We also approached pharmaceutical companies for missing data elements and information on unpublished trials.
Assessment of quality
Two authors independently scored the nine criteria of the Verhagen Delphi list to assess quality.9 This was reported in a descriptive fashion rather than using a numerical quality score because such scores can be inaccurate and poorly reproducible when they are used to differentiate between high and low quality studies.10 Further details can be found in the full Cochrane review.7
Measures of treatment effect, heterogeneity, and publication bias
We calculated difference in risk for dichotomous outcomes and weighted mean differences for continuous outcomes at the end of follow-up. When studies reported results for different doses, we abstracted the dose most commonly used in clinical practice (orlistat 120 mg three times a day, sibutramine 15 mg daily, and rimonabant 20 mg daily). Quantitative analyses of outcomes were based on intention to treat results. In studies with high attrition rates, we preferentially abstracted results reported in a last observation carried forward fashion (in which the last observation on record was used as a surrogate for the final value). The meta-analysis used a random effects model with RevMan 4.2.9.
We used χ2 to assess heterogeneity and the Higgins I2 statistic to determine the percentage of total variation across studies due to heterogeneity.11 If the I2 statistic showed substantial heterogeneity (over 50%), we did not quantitatively pool results unless the observed statistical heterogeneity was judged to be of little clinical relevance (that is, studies consistently reporting results in the same direction with clinically insignificant differences between studies).
We visually examined funnel plots to determine publication bias if there were over 10 studies for a given drug.
Results
Search results
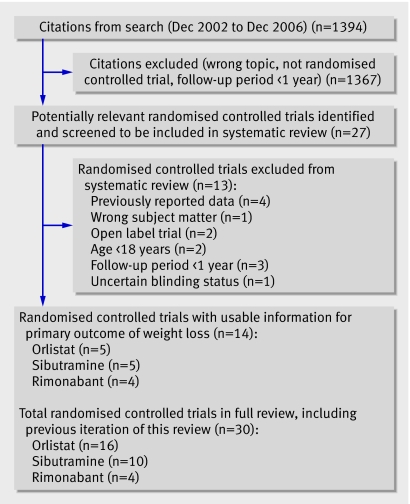
Figure 1 summarises the results of the search (fig 1). We identified 27 potentially relevant trials, and five orlistat, five sibutramine, and four rimonabant studies met final inclusion criteria. These were added to the 11 orlistat and five sibutramine trials previously identified.8 Cohen’s κ coefficient for inter-rater agreement measured 0.95 for trial selection and 0.85 for study quality.
Fig 1 Results of search for relevant studies
Description of studies
Thirty double blind placebo controlled randomised controlled trials were included in the final review: 16 orlistat (n=10 631 participants), 10 sibutramine (n=2623), and four rimonabant (n=6635) (tables 1-3).w1-30 Twenty seven of these studies received funding from the drug manufacturer.
Table 1.
Included studies on effect of orlistat on weight loss
| Study population | Mean age (years) | Mean BMI | Mean weight (kg) | Comparison | Attrition (% drug/placebo) | Cointerventions | |
|---|---|---|---|---|---|---|---|
| Bakrisw1 | 554 with hypertension, 1 year follow-up, (US) | 53 | 35.6 | 101 | Orlistat 120 mg three times daily (n=278); placebo (n=276) | 42/61 | 2.5 MJ/day deficit diet; educational literature |
| Bernew2 | 220 with type 2 diabetes receiving oral hypoglycaemics, 1 year follow-up (Sweden) | 59 | 32.7 | 96 | Orlistat 120 mg three times daily (n=111); placebo (n=109) | 14/14 | 2.5 MJ/day deficit diet; exercise counselling; educational package |
| Broomw3 | 531 with hypertension, impaired glucose tolerance, or dyslipidaemia, 1 year follow-up (UK) | 46 | 37.1 | 101 | Orlistat 120 mg three times daily (n=265); placebo (n=266) | 30/40 | 2.5-3.8 MJ/day deficit diet; food diary |
| Davidsonw4 | 892 followed for 1 year and a second weight maintenance year, (UK) | 46 | 37.1 | 101 | Orlistat 120 mg three times daily (n=668); placebo (n=224) | 31/41 | 2.5-3.3 MJ/day deficit diet; exercise counselling’ food diary |
| Derosaw5 | 50 with dyslipidaemia, 1 year follow-up (Italy) | 52 | 31.9 | 95 | Orlistat 120 mg three times daily (n=27); placebo (n=23) | 7/0 | 6.3 MJ/day deficit diet |
| Finerw6 | 228 followed for 1 year (UK) | 41 | 36.8 | 98 | Orlistat 120 mg three times daily (n=114); placebo (n=114) | 36/42 | 2.5-3.8 MJ/day deficit diet |
| Hauptmanw7 | 635 followed for 1 year and a second weight maintenance year (US) | 42 | 36 | 101 | Orlistat 60 mg three times daily (n=213); orlistat 120 mg three times daily (n=210); placebo (n=212) | 28/28/42 | 5.0-6.3 MJ/day diet; exercise; food diary; educational video |
| Hollanderw8 | 322 with type 2 diabetes, 1 year follow-up (US) | 55 | 34.3 | 100 | Orlistat 120 mg three times daily (n=63); placebo (n=159) | 15/28 | 2.1 MJ/day deficit diet |
| Kelleyw9 | 550 with type 2 diabetes, 1 year follow-up (US) | 58 | 35.7 | 102 | Orlistat 120 mg three times daily (n=274); placebo (n=276) | 50/54 | 2.5-3.3 MJ/day deficit diet; exercise counselling; food records |
| Krempfw10 | 696 followed for 18 months (France) | 41 | 36.1 | 97 | Orlistat 120 mg three times daily (n=346); placebo (n=350) | 35/43 | 20% energy reduced diet, increased by 10% if weight stable; food diary |
| Lindgardew11 | 376 with type 2 diabetes, hypertension or dyslipidaemia, 1 year follow-up (Sweden) | 53 | 33.2 | 96 | Orlistat 120 mg three times daily (n=190); placebo (n=186) | 16/12 | 2.5-3.8 MJ/day deficit diet; exercise; educational package |
| Milesw12 | 156 with type 2 diabetes receiving oral hypoglycaemics, 1 year follow-up (US and Canada) | 53 | 35.4 | 102 | Orlistat 120 mg three times daily (n=255); placebo (n=261) | 35/44 | 2.5-3.3 MJ/day deficit diet; exercise |
| Rossnerw13 | 729 followed for 1 year and a second weight maintenance year (Europe) | 44 | 35.1 | 98 | Orlistat 120 mg three times daily (n=244); placebo (n=243) | 26/35 | 2.5 MJ/day deficit diet; food diary |
| Sjostromw14 | 688 followed for 1 year and a second weight maintenance year (Europe) | 45 | 36.1 | 100 | Orlistat 120 mg three times daily (n=345); placebo (n=343) | 17/20 | 2.5-3.8 MJ/day deficit diet |
| Swinburnw15 | 339 with ≥1 cardiovascular risk factor, 1 year follow-up (Australia and New Zealand) | 52 | 37.8 | 87 | Orlistat 120 mg three times daily (n=170); placebo (n=169) | 22/19 | Diet and exercise counselling |
| XENDOSw16 | 3305 patients (21% with impaired glucose tolerance), 4 year follow-up (Sweden) | 43 | 37.3 | 111 | Orlistat 120 mg three times daily (n=1650); placebo (n=1655) | 48/66 | 3.3 MJ/day deficit diet; exercise counselling |
Table 2.
Included studies on effect of sibutramine on weight loss
| Study population | Mean age (years) | Mean BMI | Mean weight (kg) | Comparison | Attrition (% drug/placebo) | Cointerventions | ||
|---|---|---|---|---|---|---|---|---|
| Apfelbaumw17 | 205 underwent 4 week very low calorie diet, those who lost ≥6 kg (n=160) randomised to treatment or placebo, 1 year follow-up (France) | 38 | 35.5 | 104 | Sibutramine 10 mg daily (n=352); placebo (n=78) | 34/42 | Diet counselling | |
| Haunerw18 | 362 from primary care, 54 week follow-up (Germany) | 43 | 35.3 | 100 | Sibutramine 15 mg daily (n=180); placebo (n=182) | 40/48 | 2.1-4.2 MJ/day deficit diet; exercise; food diary | |
| Jamesw19 | 605 receiving sibutramine 5 mg daily and diet for 6 months, those who lost 5% of weight (n=467) randomised to treatment or placebo, 18 month follow-up (Europe) | 41 | 36.7 | 102 | Sibutramine 10-20 mg daily (n=352); placebo (n=115) | 15/28 | 2.5 MJ/day deficit diet; exercise counselling | |
| Kaukuaw20 | 236 with type 2 diabetes, 1 year follow-up (Finland) | 53 | 35.7 | 99 | Sibutramine 15 mg daily (n=114); placebo (n=122) | 11/11 | 2.9 MJ/day deficit diet | |
| Mathus-Vliegenw21 | 221 receiving very low calorie diet for 3 months. Those who lost ≥10% of weight (n=189) randomised to treatment or placebo, 18 months follow-up (Dutch) | 43 | 36.6 | 105 | Sibutramine 10-15 mg daily (n=94); placebo (n=95) | 35/39 | 2.5 MJ/day deficit diet | |
| McMahon 2000w22 | 224 with controlled hypertension, 1 year follow-up (36% African-American; US) | 53 | 34.3 | 97 | Sibutramine 20 mg daily (n=170); placebo (n=169) | 22/19 | Diet counselling | |
| McMahon 2002w23 | 220 with controlled hypertension. 1 year follow-up (US) | 51 | 33.9 | 98 | Sibutramine 20 mg daily (n=146); placebo (n=74) | 42/51 | Diet counselling | |
| McNultyw24 | 194 with type 2 diabetes, | 1 year follow-up (UK, Canada, France, Belgium) | 49 | 36.6 | 103 | Sibutramine 15 mg daily (n=68); placebo (n=62) | 28/21 | Diet counselling |
| Sanchez-Reyesw25 | 86 with type 2 diabetes treated with sulfonylureas, 1 year follow-up (Mexico) | 44 | 35.1 | 98 | Sibutramine 10 mg daily (n=44); placebo (n=42) | 45/45 | Diet and exercise counselling | |
| Smithw26 | 485 from primary care, 1 year follow-up (UK) | 42 | 32.7 | 87 | Sibutramine 10 mg daily (n=161); sibutramine 15 mg daily (n=161); placebo (n=161) | 42/49/51 | Diet counselling |
Table 3.
Included studies on effect of rimonabant on weight loss
| Study population | Mean age (years) | Mean BMI | Mean weight (kg) | Comparison | Attrition (% drug/placebo) | Cointerventions | |
|---|---|---|---|---|---|---|---|
| RIO-Diabetesw27 | 1047 with type 2 diabetes receiving oral hypoglycaemics, 1 year follow-up (11 countries) | 56 | 34.2 | 98 | Rimonabant 5 mg daily (n=358); rimonabant 20 mg daily (n=339); placebo (n=348) | 35/32/34 | 2.5 MJ/day deficit diet; exercise counselling |
| RIO-Europew30 | 1507 with hypertension (41%) or dyslipidaemia (61%), 1 year follow-up (Europe and US) | 45 | 36 | 101 | Rimonabant 5 mg daily (n=603); rimonabant 20 mg daily (n=599); placebo (n=305) | 39/37/42 | 2.5 MJ/day deficit diet; exercise counselling |
| RIO-Lipidsw29 | 1036 patients with untreated dyslipidaemia, 1 year follow-up (Europe and North America) | 48 | 34 | 98 | Rimonabant 5 mg daily (n=346); rimonabant 20 mg daily (n=345); placebo (n=342) | 36/40/37 | 2.5 MJ/day deficit diet |
| RIO-North Americaw28 | 3045 patients with hypertension (30%) or dyslipidaemia (63%). 2 year follow-up (Europe and US) | 45 | 37.6 | 104 | Rimonabant 5 mg daily (n=1216); rimonabant 20 mg daily (n=1222); placebo (n=607) | 49/45/49 | 2.5 MJ/day deficit diet; exercise counselling |
Nine orlistat studies limited enrolment to higher risk populations: four recruited patients with type 2 diabetesw2 w8 w9 w12 and five enrolled obese patients with at least one cardiovascular risk factor (hypertension, dyslipidaemia, diabetes, or impaired glucose tolerance).w1 w3 w5 w11 w15 In the largest study, which used orlistat (Xenical in the prevention of diabetes in obese subjects, XENDOS), 21% of patients had impaired glucose tolerance.w16
Two sibutramine studies limited enrolment to patients with hypertension with controlled blood pressurew22 w23 and three enrolled patients with type 2 diabetes.w20 w24 w25
One rimonabant study enrolled patients with dyslipidaemia (rimonabant in obesity (RIO)-lipids),w29 one enrolled patients with diabetes (rimonabant in obesity-diabetes),w27 and the other two commonly included patients with dyslipidaemia or hypertension (rimonabant in obesity-Europe; rimonabant in obesity-North America).w28 w30
Interventions
Twenty seven studies (16 orlistat, seven sibutramine, and four rimonabant) were weight loss trials, in which drug treatment was used in conjunction with a weight loss diet for one to four years. Of these, one rimonabant and four orlistat studies also contained a second weight maintenance year.w4 w7 w13 w14 w30 The three remaining sibutramine trials were weight maintenance studies, in which randomisation was performed after a one to six month induction phase with reduced energy intake.w17 w19 w21 A standardised, low fat, low energy diet and encouragement to exercise were the main cointerventions in most weight loss studies.
Inclusion and exclusion criteria
Trials generally enrolled selected patients with few comorbidities who were able to adhere to a run-in phase protocol. Patients had similar demographic profiles across trials of all three drugs: about two thirds to three quarters of participants were women, about 90% were white, mean age was 45-50 years, mean weight was about 100 kg, and mean body mass index was 35-36 (class 2 obesity).7
In most studies exclusion criteria were obesity of endocrine origin, uncontrolled hypertension, treatment with drugs affecting body weight, pregnancy or lactation, relevant psychiatric or medical illness, previous bariatric surgery, and considerable weight loss before screening.
Methodological quality
Studies were all of similar quality,7 and the most important methodological limitation was high attrition rates, which averaged 30% for orlistat studies and 40% for sibutramine and rimonabant studies. The most common reasons for premature withdrawal were refusal of treatment, loss to follow-up, and adverse effects. Most studies did not describe the randomisation process or comment on allocation concealment. No study specifically mentioned blinding of outcome assessors. All studies reported eligibility criteria, and cointerventions were similar in intervention and control arms. Although all included studies described using an intention to treat analysis, the validity of this approach was compromised by the high attrition rates. Because there was little variation in quality and weight loss results, we did not perform sensitivity analyses according to study quality.
Secondary end points were inconsistently reported, sometimes in only a subgroup of patients, or were not reported in an extractable manner. Our analysis includes only those data that were extractable from a given study.
Heterogeneity
Significant heterogeneity (I2 ≥50%) was present in several anthropometric outcomes but was not judged to be clinically relevant. Substantial heterogeneity (I2 >80%) was also present when we pooled the effects of orlistat and rimonabant on glycaemic control. For orlistat, this heterogeneity was attenuated and did not seem clinically relevant when we limited pooling to patients with diabetes alone. For rimonabant, we have reported glycaemic control results only for the single trial involving patients with type 2 diabetes.
Outcomes
The number of patients included in a given endpoint analysis may be lower that the overall total number of patients studied because we extracted data only for the highest dose of a given drug and the end point may not have been reported at all or not reported in an extractable manner. None of the trials reported total mortality, cardiovascular morbidity, and cardiovascular mortality as end points.
Orlistat
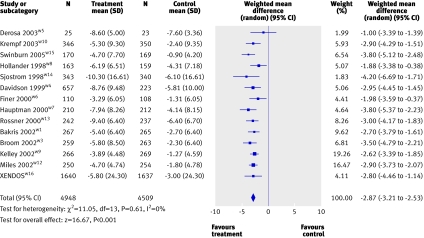
Body weight—Orlistat reduced weight by 2.9 kg (95% confidence interval 2.5 kg to 3.2 kg; 15 studies; fig 2) or 2.9% (2.5% to 3.4%; 13 studies) more than placebo and increased the absolute percentage of participants achieving 5% and 10% weight loss thresholds by 21% (54% v 33%; 18% to 24%; 14 studies) and 12% (26% v 14%; 9% to 14%; 13 studies), respectively (table 4). Placebo subtracted weight loss was 2.6% (2.1% to 3.2%; five studies) or 2.3 kg (1.6 kg to 3.0 kg; four studies) in patients with diabetes receiving orlistat. In the four studies with a second year of weight maintenance, both orlistat and placebo arms showed similar amounts of weight regain, though the weight differential observed after the weight loss phase was preserved.w4 w7 w13 w14
Fig 2 Placebo subtracted weight reduction (kg) with orlistat
Table 4.
Summary of outcomes in studies of orlistat
| Outcome | No of studies (sample size) | Weighted mean difference or risk difference (active minus placebo) (95% CI) |
|---|---|---|
| Change in weight (kg) | 15 (9833) | −2.87 (−3.21 to −2.53) |
| Change in weight (%) | 13 (6196) | −2.93 (−3.35 to −2.50) |
| 5% responders (absolute % difference) | 14 (9389) | 0.21* (0.18 to 0.24) |
| 10% responders (absolute % difference) | 13 (8857) | 0.12* (0.09 to 0.14) |
| Change in: | ||
| Waist circumference (cm) | 9 (4631) | −2.06 (−2.86 to −1.26) |
| BMI | 3 (1276) | −1.05 (−1.40 to −0.71) |
| Systolic blood pressure (mm Hg) | 13 (6965) | −1.52 (−2.19 to −0.86) |
| Diastolic blood pressure (mm Hg) | 12 (8322) | −1.38 (−2.03 to −0.74) |
| Total cholesterol (mmol/l) | 13 (5206) | −0.32 (−0.37 to −0.28) |
| Low density lipoprotein cholesterol (mmol/l) | 13 (5206) | −0.26 (−0.30 to −0.22) |
| High density lipoprotein cholesterol (mmol/l) | 11 (4152) | −0.03 (−0.04 to −0.02) |
| Triglycerides (mmol/l) | 11 (4456) | −0.03 (−0.12 to 0.07) |
| Weight in those with diabetes (%) | 5 (1678) | −2.61 (−3.06 to −2.17) |
| Weight in those with diabetes (kg) | 4 (1737) | −2.30 (−3.00 to −1.60) |
| Fasting glucose in those with diabetes (mmol/l) | 5 (1678) | −1.03 (−1.49 to −0.57) |
| Haemoglobin A1C in those with diabetes (%) | 5 (1678) | −0.38* (−0.59 to −0.18) |
| Overall gastrointestinal adverse events (%) | 14 (8938) | 0.24* (0.20 to 0.29) |
| Faecal incontinence (%) | 4 (1636) | 0.06* (0.05 to 0.08) |
| Discontinuation because of gastrointestinal side effects (%) | 12 (5994) | 0.02 (0.01 to 0.03) |
*Risk difference. All other calculations represent weighted mean difference.
Secondary end points—Orlistat reduced the incidence of type 2 diabetes from 9.0% to 6.2% (hazard ratio 0.63; 95% confidence interval 0.46 to 0.86) in one four year trial.w16 This benefit was observed primarily in patients with impaired glucose tolerance at baseline. Compared with placebo, orlistat also significantly reduced waist circumference, body mass index, systolic blood pressure, diastolic blood pressure, fasting glucose and haemoglobin A1C concentrations in patients with diabetes, and total cholesterol, low density lipoprotein cholesterol, and high density lipoprotein cholesterol concentrations (table 4). Fasting glucose concentrations were significantly reduced (P<0.05) in four of six studies that did not exclusively enrol patients with type 2 diabetes. There was no significant difference between orlistat and placebo in triglyceride concentrations or the change in Framingham cardiovascular risk score.w15
Adverse effects—Patients receiving orlistat were more likely to experience gastrointestinal adverse events and to discontinue because of this (table 4). The most commonly reported gastrointestinal events were fatty/oily stool, faecal urgency, and oily spotting, each occurring at frequency rates of 15% to 30% in most studies. Although concentrations of fat soluble vitamins were reportedly lowered, no study reported clinically relevant vitamin deficiency. Patients receiving orlistat were routinely advised to take daily multivitamins.
Sibutramine
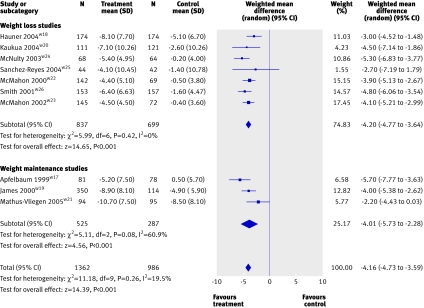
Weight loss—Patients receiving sibutramine lost 4.2 kg (3.6 kg to 4.7 kg; eight studies; fig 3) or 4.3% (3.7% to 5.0%; 10 studies) more weight than those taking placebo. In addition, sibutramine treatment increased the absolute percentage of 5% and 10% responders by 32% (55% v 27%; 27% to 37%; seven studies) and 18% (28% v 10%; 11% to 25%; seven studies), respectively (table 5). Placebo subtracted weight losses in patients with diabetes were 5.0% (3.8% to 6.2%) or 4.9 kg (3.6 kg to 6.2 kg). About 10-30% more sibutramine patients achieved successful weight maintenance compared with placebo (successful weight maintenance defined as maintaining 80-100% of the initial weight loss). This was significant (P<0.05) in all three studies but we did not combine data because of differing definitions of weight maintenance between studies.w17 w19 w21
Fig 3 Placebo subtracted weight reduction (kg) with sibutramine
Table 5.
Summary of outcomes in studies of sibutramine
| Outcome | No of studies (sample size) | Weighted mean difference or risk difference (active minus placebo) (95% CI) |
|---|---|---|
| Change in weight (kg) | 10 (2348) | −4.16 (−4.73 to −3.59) |
| Change in weight (%) | 8 (1725) | −4.34 (−5.01 to −3.67) |
| 5% responders (absolute % difference) | 7 (1464) | 0.32* (0.27 to 0.37) |
| 10% responders (absolute % difference) | 7 (1464) | 0.18* (0.11 to 0.25) |
| Change in: | ||
| Waist circumference (cm) | 8 (1837) | −3.99 (−4.70 to −3.28) |
| BMI | 5 (956) | −1.54 (−1.79 to −1.30) |
| Weight in those with diabetes (%) | 3 (450) | −4.99 (−3.78 to −6.20) |
| Weight in those with diabetes (kg) | 3 (450) | −4.91 (−3.64 to −6.18) |
| Systolic blood pressure (mm Hg) | 7 (1906) | 1.69 (0.11 to 3.28) |
| Diastolic blood pressure (mm Hg) | 7 (1906) | 2.42 (1.51 to 3.32) |
| High density lipoprotein cholesterol (mmol/l) | 5 (977) | 0.04 (0.01 to 0.08) |
| Triglycerides (mmol/l) | 4 (785) | −0.18 (−0.30 to −0.07) |
| Heart rate (beats/minute) | 7 (1658) | 4.53 (3.49 to 5.57) |
*Risk difference. All other calculations represent weighted mean difference.
Secondary end points—Treatment with sibutramine significantly reduced body mass index, waist circumference, and triglyceride concentrations and increased concentrations of high density lipoprotein cholesterol (table 5). Change in glycaemic variables and concentrations of low density lipoprotein cholesterol and total cholesterol were inconsistently reported and, when reported, were not significantly different from values in the placebo group in any study.
Adverse effects—Compared with placebo, sibutramine increased systolic blood pressure by 1.7 mm Hg (0.1 mm Hg to 3.3 mm Hg; seven studies), diastolic blood pressure by 2.4 mm Hg (1.5 mm Hg to 3.3 mm Hg; seven studies), and pulse rate by 4.5 beats/min (3.5 beats/min to 5.6 beats/min; seven studies) (table 5). Insomnia, nausea, dry mouth, and constipation were more common in patients receiving sibutramine, occurring at frequency rates of 7-20%.
Rimonabant
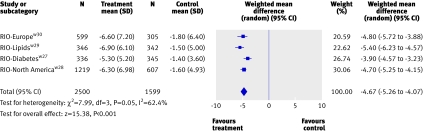
Weight loss—Patients receiving rimonabant lost 4.7 kg (4.1 kg to 5.3 kg; four studies; fig 4) more weight than those taking placebo. The average weight loss was 3.9 kg (3.2 kg to 4.6 kg) in the rimonabant in obesity-diabetes trial.w27 Rimonabant treatment also significantly increased the placebo subtracted absolute percentage of 5% and 10% responders by 33% (51% v 18%; 29% to 37%; four studies) and 19% (26% v 7%; 15% to 23%; seven studies), respectively (table 6). During the weight maintenance phase of the rimonabant in obesity-North America study, patients treated with rimonabant maintained the weight differential observed in the weight loss phase of the study.w30
Fig 4 Placebo subtracted weight reduction (kg) with rimonabant
Table 6.
Summary of outcomes for rimonabant
| Outcome | No of studies (sample size) | Weighted mean difference or risk difference (active minus placebo) (95% CI) |
|---|---|---|
| Change in weight (kg) | 4 (4099) | −4.67 (−5.26 to −4.07) |
| 5% responders (absolute % difference) | 4 (4099) | 0.33* (0.29. 0.37) |
| 10% responders (absolute % difference) | 4 (4099) | 0.19* (0.15 to 0.23) |
| Change in: | ||
| Waist circumference (cm) | 4 (4098) | −3.89 (−4.47 to −3.30) |
| Systolic blood pressure (mm Hg) | 3 (2273) | −1.78 (−2.81 to −0.76) |
| Diastolic blood pressure (mm Hg) | 3 (2273) | −1.23 (−1.93 to −0.54) |
| Total cholesterol (mmol/l) | 3 (2223) | −0.04 (−0.11 to 0.03) |
| Low density lipoprotein cholesterol (mmol/l) | 3 (2223) | −0.05 (−0.12 to 0.01) |
| High density lipoprotein cholesterol (mmol/l) | 4 (4050) | 0.10 (0.08 to 0.11) |
| Triglycerides (mmol/l) | 4 (4049) | −0.24 (−0.30 to −0.17) |
| Weight in those with diabetes (kg) | 1 (1047) | −3.90 (−4.57 to −3.23) |
| Haemoglobin A1C in those with diabetes (%) | 1 (1047) | −0.70 (−0.84 to −0.56) |
| Fasting glucose in those with diabetes (mmol/l) | 1 (1047) | −0.97 (−1.30 to −0.64) |
| Discontinuation because of adverse event (absolute % difference) | 4 (4105) | 0.06* (0.05 to 0.08) |
| Serious adverse event (absolute % difference) | 4 (4105) | 0.02* (0.00 to 0.03) |
| Psychiatric disorders (absolute % difference) | 4 (4105) | 0.03* (0.02 to 0.05) |
*Risk difference. All other calculations represent weighted mean difference.
Secondary end points—Rimonabant significantly reduced placebo subtracted waist circumference, systolic blood pressure, diastolic blood pressure, and triglyceride concentrations and increased high density lipoprotein cholesterol concentrations (table 6). Fasting glucose and haemoglobin A1C concentrations were significantly reduced in the rimonabant in obesity-diabetes studyw27 but not in the other rimonabant in obesity studies (table 6). Low density lipoprotein cholesterol and total cholesterol concentrations were not significantly reduced compared with placebo.
Adverse effects—The most worrying adverse effect was an increased incidence of psychiatric disorders (depression, anxiety, irritability, aggression), which occurred in 6% of patients receiving rimonabant and was 3% (2% to 5%; four studies) more likely in patients receiving rimonabant compared with placebo (table 6).
Discussion
Our meta-analysis of one to four year randomised controlled trials of orlistat, sibutramine, and rimonabant in adults showed that each drug results in average placebo subtracted weight reductions of less than 5 kg. We found no data on the effect of these agents on mortality or cardiovascular morbidity. Weight maintenance studies for each drug reported similar amounts of weight regained in active and placebo arms, such that the original weight differential between groups was maintained. We found differing effects on secondary end points and adverse effect profiles. These updated results are consistent with the results of previous reviews8 12,13,14,15 but more precisely define the long term effects of current agents on weight and secondary end points and describe each drug’s unique adverse effect profile.
Limitations
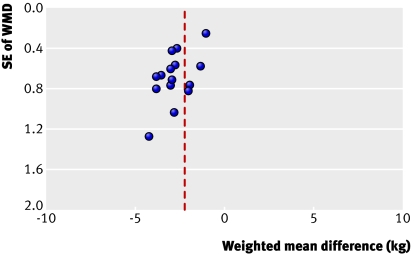
There are several limitations to this meta-analysis. Firstly, all studies showed a positive effect of treatment on weight loss, which raises the possibility of publication bias. A funnel plot of orlistat studies indicates that we might have underestimated the impact of all types of small studies (positive, negative, or neutral) in this meta-analysis (fig 5).7 There were too few sibutramine and rimonabant studies to warrant generation of funnel plots. Nearly all trials were funded by pharmaceutical companies, which may increase the likelihood of positive results.16 Secondly, most patients studied were non-elderly and white and extrapolation to other populations should be made with caution. Thirdly, we found statistical heterogeneity when we quantitatively pooled several outcomes. This was addressed by using a random effects meta-analysis and by not combining outcomes when the heterogeneity was thought to be clinically relevant. As we did not have access to data on individual patients, we could not perform meta-regression analysis to further investigate the cause of the observed heterogeneity. Differences in populations of patients, cointerventions, trial duration, and drug dose were probably all contributing factors. Fourthly, our analysis includes only those data that were extractable from a given study and studies may have reported full results only for end points that significantly differed from placebo.
Fig 5 Funnel plot of orlistat studies for weight loss
Synthesis of findings
Previous studies have shown that people with diabetes find it more difficult to lose weight, possibly because of the underlying disease state or because medications used to treat diabetes tend to increase weight.2 17 We found that studies enrolling patients with diabetes reported slightly smaller amounts of weight loss with orlistat and rimonabant, a finding not seen with sibutramine. Despite this finding, both orlistat and rimonabant improved glycaemic variables in patients with diabetes, whereas sibutramine did not. The underlying reasons for this and the clinical relevance are unclear. One potential contributor to improved glycaemic control with rimonabant is an increase in adiponectin.w29 Further data are needed, ideally from head to head clinical trials of all three agents, before more definitive conclusions can be made.
Even though studies preselected patients for their ability to adhere to and to tolerate treatment, attrition rates were high, compromising the internal validity of many studies. It is difficult to compensate for such high attrition rates by using any form of analysis. A recent study using Canadian provincial administrative data reported persistence rates with orlistat and sibutramine of less than 10% at one year and less than 2% at two years.18 Lack of adherence to treatment seems to be a major factor limiting the efficacy and effectiveness of anti-obesity drugs.
The observed increase in blood pressure and heart rate with sibutramine are of potential concern, and blood pressure should be monitored during treatment. The increased incidence of mood disorders with rimonabant indicates careful surveillance, particularly because psychiatric illness commonly coexists with obesity.2 As the patients enrolled in the rimonabant trials were carefully screened to exclude those with major psychiatric disease, the risk of mood disorders with rimonabant might be underestimated.
The decision to prescribe an anti-obesity drug involves careful assessment of the risks and benefits. The average amount of weight lost is modest, lower than the 5-10% placebo subtracted target recommended by current guidelines,3 19 20 and most patients will remain considerably obese or overweight even with drug treatment. Current anti-obesity drugs are costly (in the UK around £40-55 (€57-79, $83-114) for 28 days’ treatment), each drug has associated adverse effects, and the ultimate effect on cardiovascular morbidity and mortality remains unknown. Balanced against these factors are the potential for modest improvements in the cardiovascular risk profile, which varies according to each drug, the possibility that the patient will be among those who have a good response (that is, 5-10% weight loss or more), and accumulating evidence that even modest amounts of weight loss (5-10%) are beneficial, particularly in patients at risk of developing type 2 diabetes.21 Guidelines from the National Institute for Health and Clinical Excellence (NICE) recommend discontinuation of drug treatment if a 5% threshold in weight loss has not been reached by three months.19
In the absence of definitive data to show that one particular drug is more effective than another,3 initial treatment can be guided by the patient’s preference, local drug costs, drug availability, drug plan coverage, and the patient’s comorbidities and adverse effect profiles (table 7). Studying morbidity and mortality end points is vital to confirming a favourable benefit:risk ratio for anti-obesity drugs because drugs that improve surrogate end points, such as weight loss, may not ultimately improve more clinically relevant outcomes.22 Similarly, the clinical relevance of the reduction in incidence of diabetes observed with orlistat is uncertain, and further study is required to determine if a true preventive effect, as opposed to a delaying or masking effect, is occurring.23 Trials evaluating the effect of sibutramine and rimonabant on cardiovascular morbidity and mortality end points are ongoing and are detailed elsewhere.3 Methodologically rigorous studies powered to examine such end points are clearly required to better inform future use of anti-obesity drugs as adjuncts to lifestyle modification in improving the health status and quality of life in overweight and obese patients.
Table 7.
Prescribing summary for orlistat, sibutramine, and rimonabant
| Drug | Standard dose | Potentially useful in | Avoid in | Comments |
|---|---|---|---|---|
| Orlistat | 120 mg three times daily | Pre-diabetes, diabetes, raised low density lipoprotein cholesterol, hypertension, pre-existing cardiovascular disease | Malabsorption or chronic gastrointestinal disease | Prescribe concurrent multivitamin. Half strength available over counter in US |
| Sibutramine | 10-15 mg once daily | When lack of satiety is major barrier to weight reduction, dyslipidaemia (high triglyceride/low high density lipoprotein cholesterol) | Uncontrolled hypertension, tachycardia, pre-existing cardiovascular disease | Monitor blood pressure |
| Rimonabant | 20 mg once daily | Dyslipidaemia (high triglyceride/low high density lipoprotein cholesterol), diabetes, metabolic syndrome, hypertension | History of psychiatric illness, liver impairment | Monitor for mood disorders |
What is already known on this topic
Previous meta-analyses examining the long term efficacy of anti-obesity drugs have been limited to orlistat and sibutramine
Average weight losses were less than 5 kg and some cardiovascular risk factors improved, but attrition rates were relatively high
What this study adds
Rimonabant, sibutramine, and orlistat modestly reduce weight (less than 5 kg) and have differing effects on cardiovascular risk factors and differing side effect profiles
There are no data evaluating the effect of anti-obesity drugs on morbidity or mortality end points, although studies are now ongoing
Supplementary Material
This paper is based on a recently updated Cochrane review that is currently undergoing peer review. The conclusions of this review represent the opinions of review authors, and are not necessarily shared by the Cochrane Collaboration.
Contributors: RP was responsible for conception and design, data extraction, and data analysis, cowrote the initial and final drafts, and is guarantor. DR performed data extraction and analysis and co-wrote the initial and final drafts. SKL, CC, and DCWL performed data extraction or data interpretation and cowrote the final draft.
Funding: None.
Competing interests: DCWL has received consulting and speaker fees, research grants, and travel assistance from makers of anti-obesity drugs.
Ethical approval: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Haslam DW, James WPT. Obesity. Lancet 2005;366:1197-209. [DOI] [PubMed] [Google Scholar]
- 2.Lau DCW, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ 2007;176:S1-130. www.cmaj.ca/cgi/content/full/176/8/S1/DC1 [DOI] [PMC free article] [PubMed]
- 3.Padwal RS, Majumdar SR. Drug treatments for obesity: orlistat, sibutramine and rimonabant. Lancet 2007;369:71-7. [DOI] [PubMed] [Google Scholar]
- 4.IMS Health. Obesity: new products on the horizon 2007. www.imshealth.com/web/end/0,3150,64576068_63872702_78348467,00.html
- 5.Lau DCW. Synopsis of the 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ 2007;176:1103-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995;332:621-8. [DOI] [PubMed] [Google Scholar]
- 7.Padwal R, Rucker D, Li SK, Curioni C, Lau DCW. Long-term pharmacotherapy for obesity and overweight. Cochrane Database Syst Rev (in press). [DOI] [PMC free article] [PubMed]
- 8.Padwal R, Li SK, Lau DCW. Long-term pharmacotherapy for obesity and overweight. Cochrane Database Syst Rev 2003;(4):CD004094. [DOI] [PubMed] [Google Scholar]
- 9.Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998;51:1235-31. [DOI] [PubMed] [Google Scholar]
- 10.Juni P, Smith GD, Altman DG. Assessing the quality of randomised controlled trials. In: Egger M, Smith GD, Altman DG, eds. Systematic reviews in health care 2nd ed. London: BMJ Publishing, 2001:87-108. [DOI] [PMC free article] [PubMed]
- 11.Higgins J, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curioni C, Andre C. Rimonabant for overweight or obesity. Cochrane Database Syst Rev 2006;(4):CD006162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Z, Maglione M, Tu W, Mojica W, Arterburn D, Shugarman LR, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med 2005;142:532-46. [DOI] [PubMed] [Google Scholar]
- 14.O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G. The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment. Health Technol Assess 2002;6:1-97. [DOI] [PubMed] [Google Scholar]
- 15.O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G. A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity. Health Technol Assess 2001;5:1-81. [DOI] [PubMed] [Google Scholar]
- 16.Lexchin J, Bero LA, Djulbegovic B, Clark O. Pharmaceutical industry sponsorship and research outcome and quality: systematic review. BMJ 2003;326:1167-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wing RR, Marcus MD, Epstein LH, Salata R. Type II diabetic subjects lose less weight than their overweight nondiabetic spouses. Diabetes Care 1987;10:563-6. [DOI] [PubMed] [Google Scholar]
- 18.Padwal R, Kezouh A, Levine M, Etminan M. Long-term persistence with orlistat and sibutramine in a population-based cohort. Int J Obes (Lond) 2007;31:1567-70. [DOI] [PubMed] [Google Scholar]
- 19.National Institute for Health and Clinical Excellence. CG43 obesity: full guideline, section 1—introduction, methods and recommendations 2006. http://guidance.nice.org.uk/CG43/guidance/section1/word/English
- 20.Colman E. Anorectics on trial. A half-century of federal regulation of prescription appetite suppressants. Ann Intern Med 2005;143:380-5. [DOI] [PubMed] [Google Scholar]
- 21.Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: a systematic review and meta-analysis. BMJ 2007;334:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padwal RS. Antiobesity drug therapy: a call for more rigorous endpoint evaluation. Therapy 2007;4:221-6. [Google Scholar]
- 23.Padwal R, Majumdar SR, Johnson JA, Varney J, McAlister FA. A systematic review of drug therapy to delay or prevent type 2 diabetes. Diabetes Care 2005;28:736-44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.