Abstract
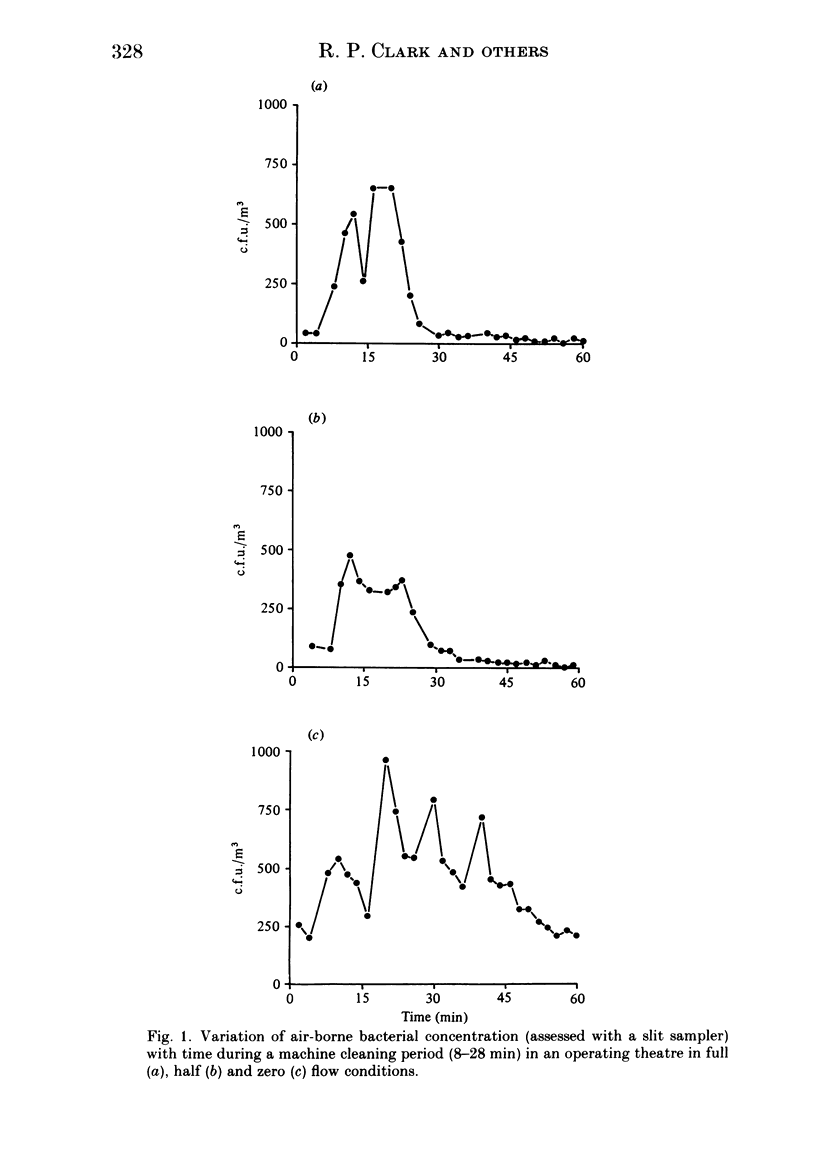
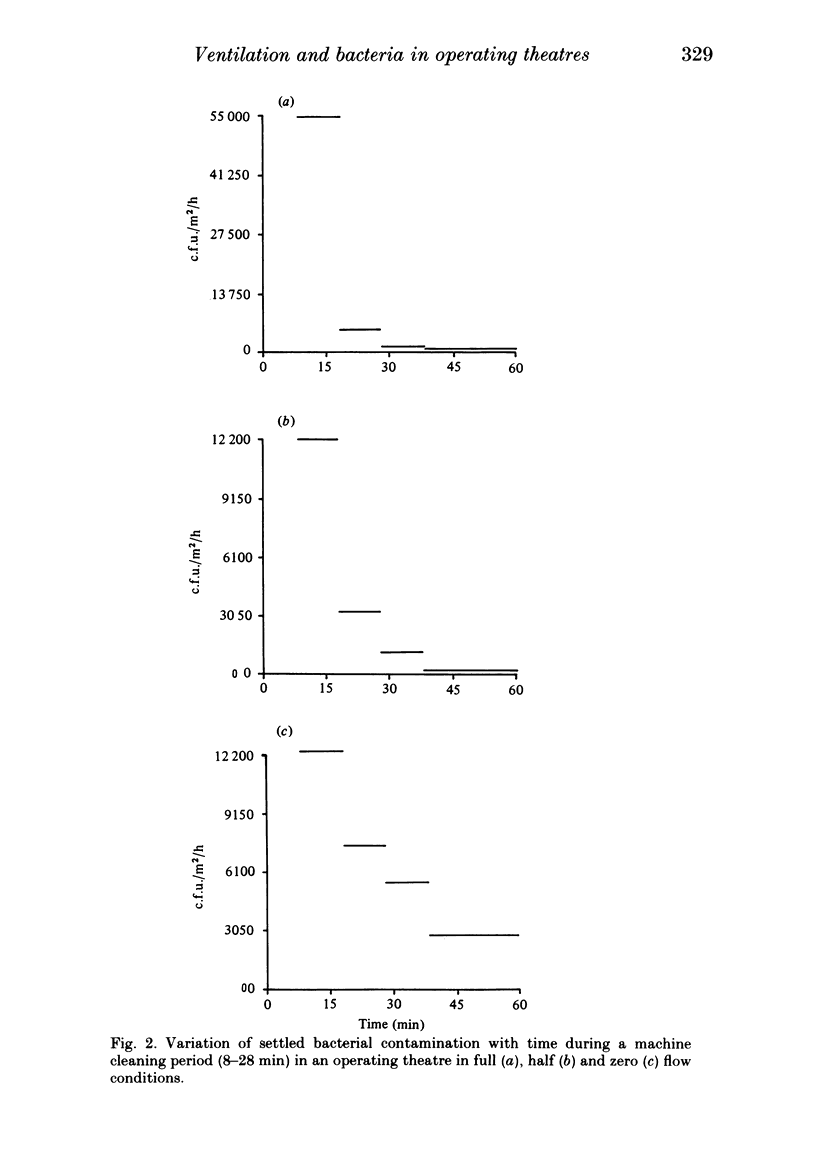
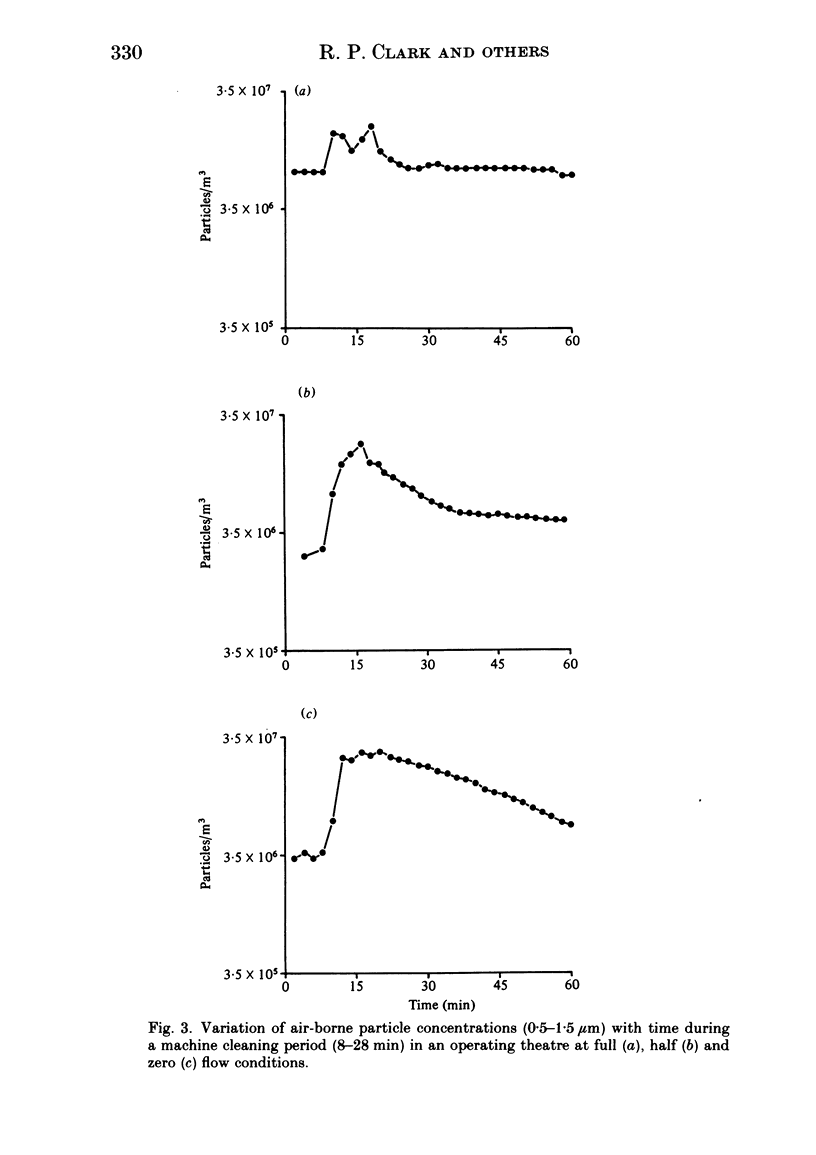
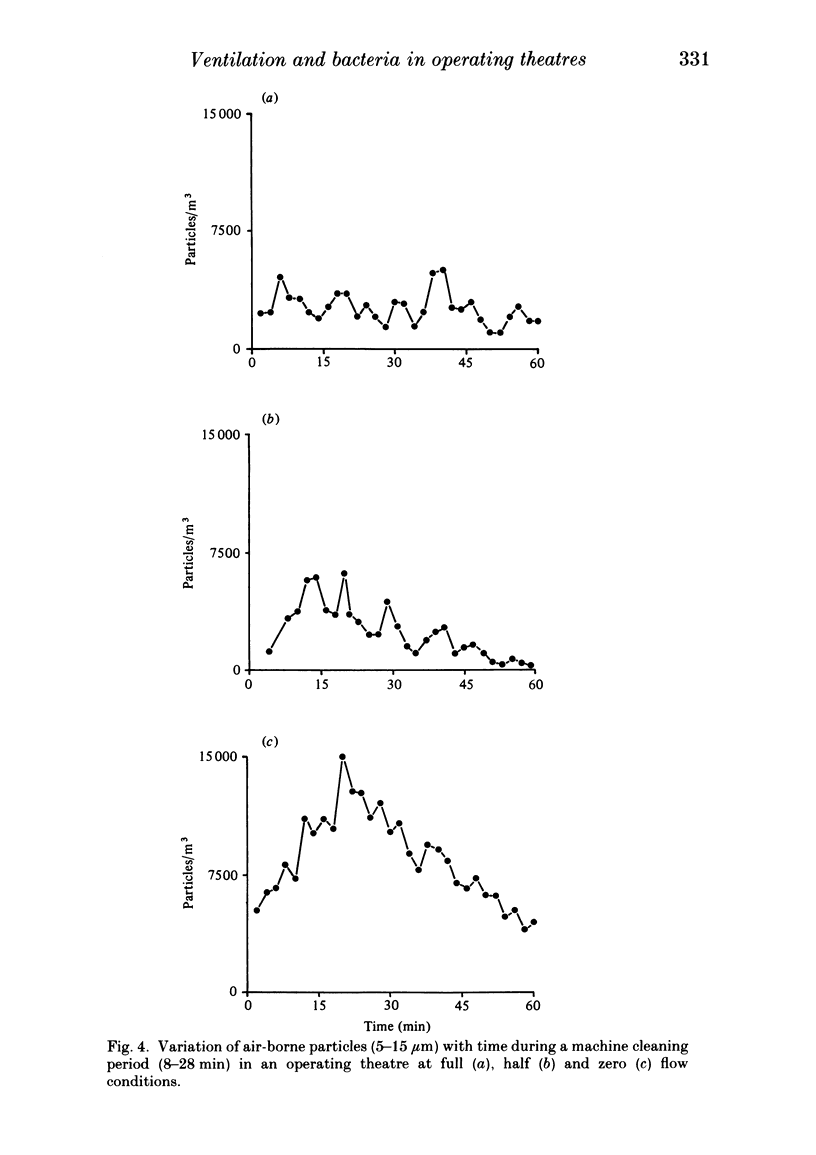
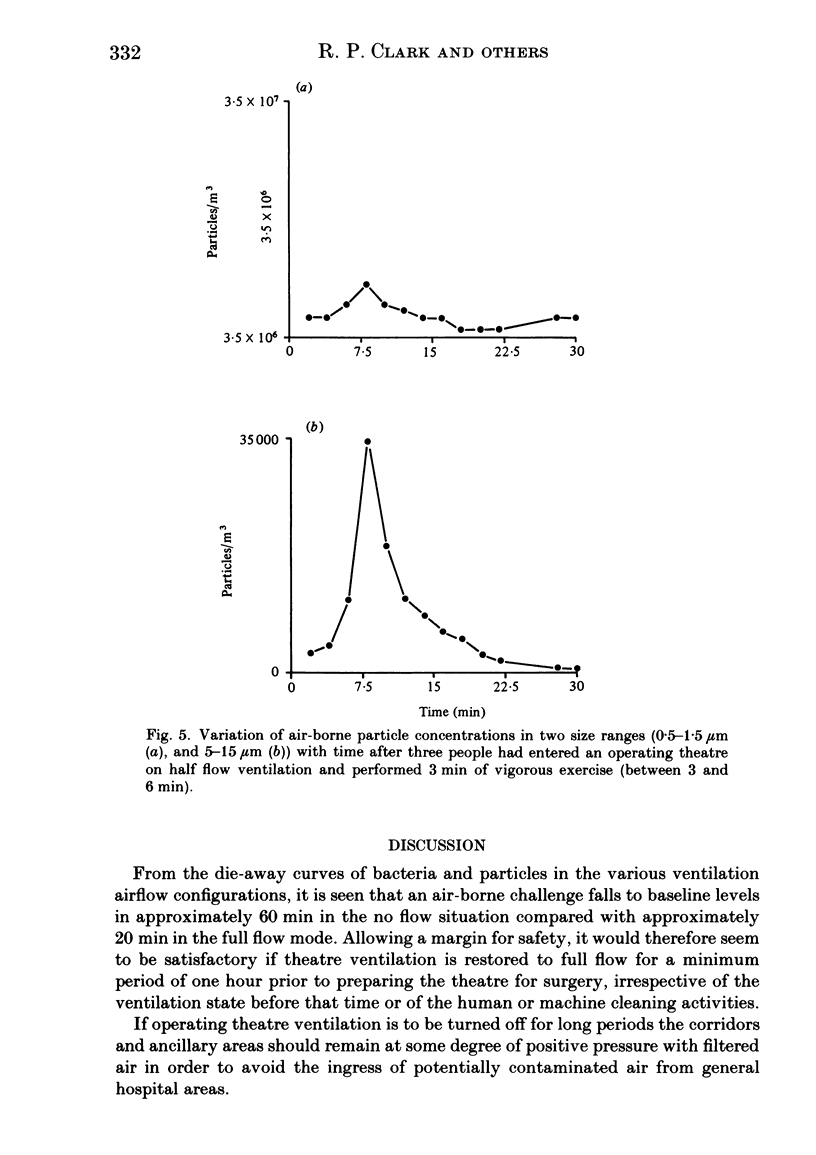
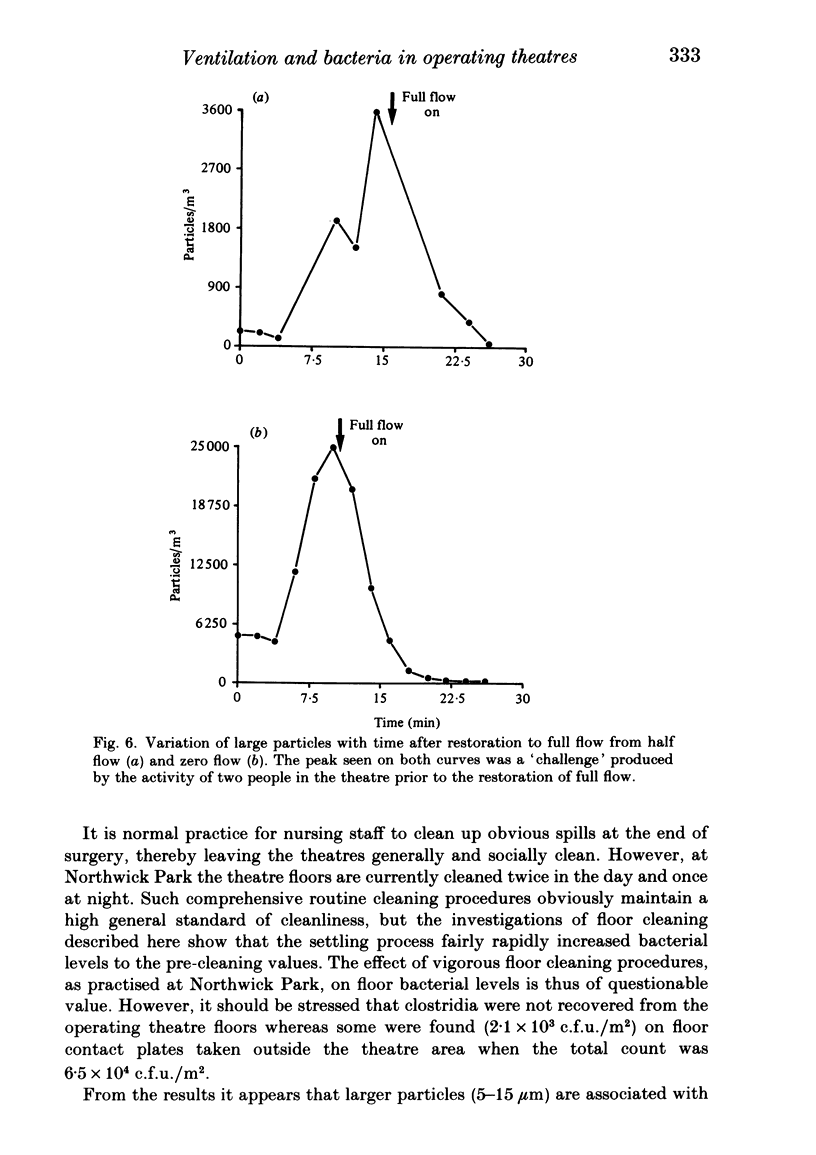
Concentrations of air-borne bacteria and particles have been measured in turbulently ventilated operating theatres in full flow, half flow and zero flow conditions. Increased air-borne challenge produced by human activity and by mechanical cleaning procedures is demonstrated: die-away of this contamination is shown to be related to the ventilation rate. Ventilation can be reduced or turned off at night and during weekends, and cleaning can also be carried out, without increased risk of infection if full flow is restored one hour prior to preparation for surgery. Areas surrounding the theatres should remain at positive pressure with regard to the general hospital environment during low or no flow periods. The implementation of such energy-saving policies will substantially reduce theatre running costs without introducing infection hazards.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Lidwell O. M. Airborne bacteria and surgical infection. Am J Med. 1981 Mar;70(3):693–697. doi: 10.1016/0002-9343(81)90598-2. [DOI] [PubMed] [Google Scholar]
- Lidwell O. M., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Airborne contamination of wounds in joint replacement operations: the relationship to sepsis rates. J Hosp Infect. 1983 Jun;4(2):111–131. doi: 10.1016/0195-6701(83)90041-5. [DOI] [PubMed] [Google Scholar]


