Abstract
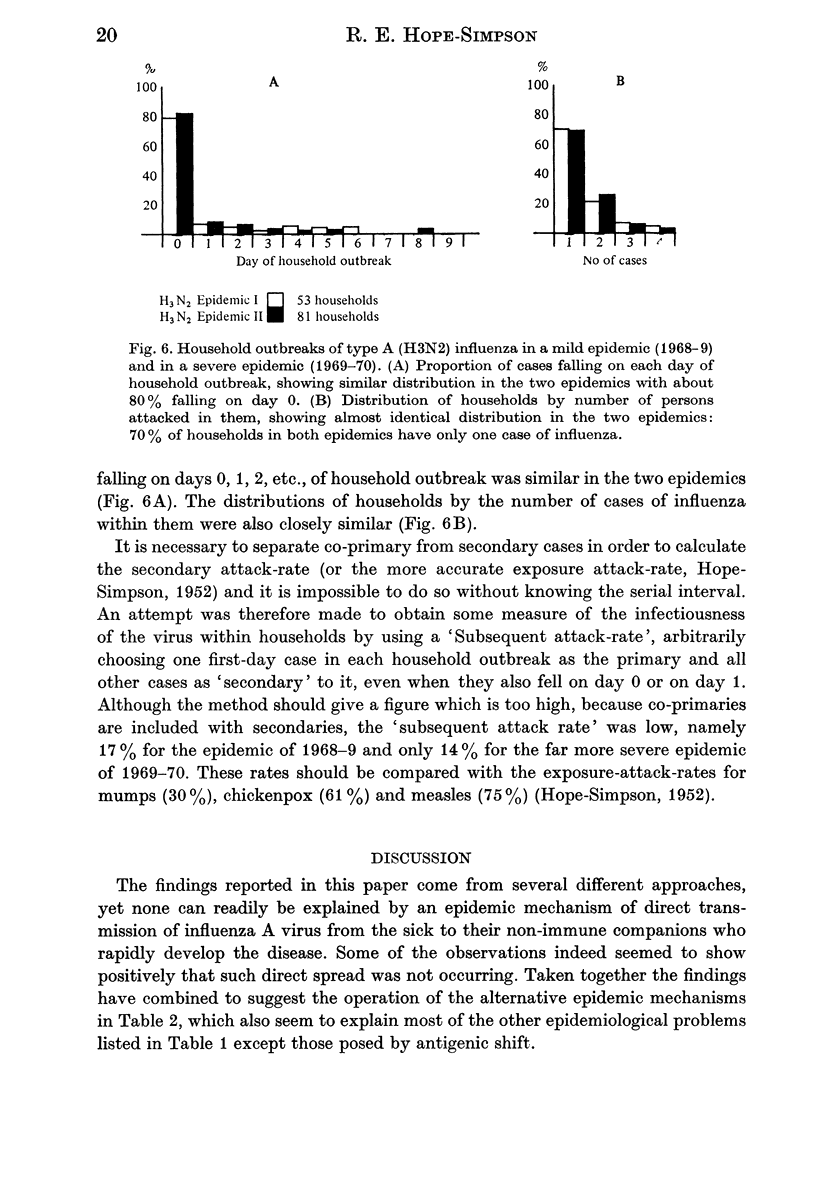
The antigenic varieties of influenza A virus isolated from 1968 to 1976 in a surveillance of a small, rather remote population were similar to those from England and Wales as a whole, despite frequent antigenic changes during the period. Household studies in the first two H3N2 influenza A epidemics found low attack rates within households, a high proportion (70%) of affected households with only one case of influenza, similar distributions of affected households in the two epidemics by the number of cases of influenza and similar distributions of the influenza cases by the day of their onset in the household outbreak. No serial interval could be demonstrated by cumulating household outbreaks. More than one minor variant was causing influenza contemporaneously in the same villages in several seasons, and different variants were on one occasion found on successive days in bedfellows. The regular occurrence of epidemics in winter was often accompanied by the disappearance of the epidemic variants and their replacement, after a virus-free interval, by new variants. These epidemiological findings seem best interpreted on the following tentative hypothesis. Influenza A sufferers do not transmit the virus during their illness; instead it rapidly becomes latent in their tissues so that they become symptomless carrier-hosts and develop specific immunity. Next season an extraneous seasonally mediated stimulus reactivates the latent virus residues so that the carrier-host becomes briefly infectious, though symptomless. Antigenic drift occurs because particles reconstituted to be identical with the progenitor virus cannot escape the specific immunity it has provoked in the carrier host. He can shed only mutants also determined by the progenitor virus. From the assortment of mutants shed by the carrier-host, his non-immune companions select that (those) which is best fitted to survive, and it rapidly causes influenzal illness. Epidemics consist largely or entirely of such persons sick with influenza caused by reactivated virus caught from symptomless carrier-hosts.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ANDREWES C. H. Epidemiology of influenza in the light of the 1951 outbreak. Proc R Soc Med. 1951 Sep;44(9):803–804. doi: 10.1177/003591575104400905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ARCHETTI I., HORSFALL F. L., Jr Persistent antigenic variation of influenza A viruses after incomplete neutralization in ovo with heterologous immune serum. J Exp Med. 1950 Nov 1;92(5):441–462. doi: 10.1084/jem.92.5.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazekas de St Groth S., Hannoun C. Sélection par pression immunologique de mutants dominants du virus de la grippe A (Hong Kong. C R Acad Sci Hebd Seances Acad Sci D. 1973 Mar 19;276(12):1917–1920. [PubMed] [Google Scholar]
- Frolov A. F., Shcherbinskaia A. M., Rybalko S. L., Gavrilov S. V., Iatel' T. P. Iavlenie dlitel'noi tsirkuliatsii virusa grippa Ao v organizme. Mikrobiol Zh. 1978 Jan-Feb;40(1):102–104. [PubMed] [Google Scholar]
- Gavrilov V. I., Asher D. M., Vyalushkina S. D., Ratushkina L. S., Zmieva R. G., Tumyan B. G. Persistent infection of continuous line of pig kidney cells with a variant of the WSN strain of influenza A 0 virus. Proc Soc Exp Biol Med. 1972 May;140(1):109–117. doi: 10.3181/00379727-140-36405. [DOI] [PubMed] [Google Scholar]
- Golubev D. B., Paramonova M. S., Medvedeva M. N., Poljakov Y. M. Influenza A2 neuraminidases and their changes during persistance of viruses in tissue cultures. Z Gesamte Hyg. 1975 Apr;21(4):324–329. [PubMed] [Google Scholar]
- Hope-Simpson R. E. First outbreak of Hong Kong influenza in a general practice population in Great Britain. A field and laboratory study. Br Med J. 1970 Jul 11;3(5714):74–77. doi: 10.1136/bmj.3.5714.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope-Simpson R. E., Higgins P. G. A respiratory virus study in Great Britain: review and evaluation. Prog Med Virol. 1969;11:354–407. [PubMed] [Google Scholar]
- ISAACS A. The 1951 influenza viruses. Proc R Soc Med. 1951 Sep;44(9):801–803. doi: 10.1177/003591575104400904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marine W. M., McGowan J. E., Jr, Thomas J. E. Influenza detection: a prospective comparison of surveillance methods and analysis of isolates. Am J Epidemiol. 1976 Sep;104(3):248–255. doi: 10.1093/oxfordjournals.aje.a112297. [DOI] [PubMed] [Google Scholar]
- Mensík J., Pospísil Z., Machatková M., Tůmová B., Franz J., Stumpa A. Adaptation of human influenza A/Hong Kong/68 (H3N2) virus to colostrum-deprived, specific-pathogen free piglets. Zentralbl Veterinarmed B. 1976 Sep;23(8):638–651. doi: 10.1111/j.1439-0450.1976.tb00702.x. [DOI] [PubMed] [Google Scholar]
- Petrescu A., Broniţki A. L., Teodosiu O., Mihail A., Popescu A., Cojiţ M., Petrişor L., Ialomiţeanu M., Mîcă C., Sferdean O. Virological study of some influenza outbreaks in the period January--March 1975. Virologie. 1976 Apr-Jun;27(2):111–114. [PubMed] [Google Scholar]
- SIMPSON R. E. H. Infectiousness of communicable diseases in the household (measles, chickenpox, and mumps). Lancet. 1952 Sep 20;2(6734):549–554. doi: 10.1016/s0140-6736(52)91357-3. [DOI] [PubMed] [Google Scholar]
- Shadrin A. S., Marinich I. G., Taros L. Y. Experimental and epidemiological estimation of seasonal and climato-geographical features of non-specific resistance of the organism to influenza. J Hyg Epidemiol Microbiol Immunol. 1977;21(2):155–161. [PubMed] [Google Scholar]
- Wallace G. W. Swine influenza and lungworms. J Infect Dis. 1977 Mar;135(3):490–492. doi: 10.1093/infdis/135.3.490. [DOI] [PubMed] [Google Scholar]
- Werner J., Schudrowitz C., Köhler H. Antigenic variation of neuraminidase of human type A influenza (H3N2) viruses isolated in Berlin (West). Zentralbl Bakteriol Orig A. 1975 Dec;233(4):440–446. [PubMed] [Google Scholar]



