Abstract
Background
Hypertensive African Americans have higher rates of coronary heart disease (CHD) than their non-Hispanic white counterparts despite having higher HDL cholesterol (HDL-C) levels and lower triglyceride levels.
Objective
The goal of the present study was to assess whether low-density lipoprotein (LDL) particle size, a correlate of the above lipid traits and a risk factor for CHD, differs between hypertensive African Americans and whites.
Methods
Participants included 1177 hypertensive African Americans from Jackson MS (60±7 years, 72.4% women) and 860 hypertensive whites from Rochester MN (58±7 years, 56.7% women). LDL particle size was measured by polyacrylamide gradient gel electrophoresis. Within each sex, we assessed whether ethnicity was significantly associated with differences in LDL particle size after adjustment for CHD risk factors (age, total cholesterol, HDL-C, triglycerides, systolic BP, diabetes, history of smoking, body mass index), statin use, and estrogen use (in women), and “lifestyle” variables (physical activity and alcohol intake).
Results
Although HDL-C levels were higher and triglyceride levels lower in African Americans, LDL particle size (adjusted for CHD risk factors) was lower (P < 0.0001) in African American men and women than in their white counterparts (mean ± SD; men, 267.6±5.2 Å vs. 270.2±4.8 Å; women 268.7±5.1 Å vs. 271.3±5.1 Å). In both sexes, African American ethnicity was associated with lower LDL particle size after adjustment for CHD risk factors, statin use and estrogen use (in women), as well as physical activity and alcohol intake.
Conclusion
Hypertensive African American men and women have lower LDL particle size than their white counterparts despite having higher HDL-C and lower triglycerides.
Keywords: low-density lipoprotein, LDL particle size, risk factors, ethnicity, hypertension
Introduction
Low-density lipoprotein (LDL) cholesterol is an important etiologic factor for atherosclerosis and the development of coronary heart disease (CHD). However, subjects may develop CHD in the setting of “normal” levels of LDL cholesterol, and assessment of the cholesterol concentration of this lipoprotein may not entirely reflect its atherogenic potential.1 Circulating LDL particles differ in size, density, composition, and atherogenic properties.2, 3 Small LDL particle size is associated with elevated levels of plasma triglycerides and low levels of high-density lipoprotein (HDL) cholesterol, a combination referred to as atherogenic dyslipidemia.4 Small LDL particle size is also associated with insulin-resistant states such as hypertension, central obesity, metabolic syndrome, and type 2 diabetes.5 A causal role for small LDL particles in the etiology of CHD is suggested by studies showing such particles to have several atherogenic characteristics including long residence time in the plasma, greater susceptibility to oxidation, increased binding affinity for intimal proteoglycans, and increased ability to cross into the subintimal space.6 Several lines of evidence, including prospective studies, indicate that small LDL particle size is a risk factor for CHD.7-10
African Americans have lower levels of triglycerides and higher levels of HDL cholesterol than do non-Hispanic whites.11 In this ethnic group, therefore, one might expect a larger LDL particle size (less atherogenic) than in non-Hispanic whites. However physical activity, diet, and alcohol intake are also known to affect LDL particle size. Haffner et al12 reported that LDL particle size was significantly higher in normotensive African Americans than in their Hispanic or non-Hispanic white counterparts. In the present study, we attempted to extend these observations to hypertensive adults and determine whether the distribution of LDL particle size differs between hypertensive African American and non-Hispanic whites, and if observed, whether the differences could be explained by measures of adiposity, insulin resistance, lipid correlates of LDL particle size, and “lifestyle” variables such as physical activity and alcohol intake. Although triglycerides are lower and HDL cholesterol is higher in African Americans,13 obesity,14 insulin resistance,15 and type 2 diabetes16 are more prevalent in African Americans than in non-Hispanic whites. We hypothesized that the greater prevalence of these risk factors in hypertensive African Americans may lead to a lower LDL particle size than in their non-Hispanic white counterparts.
Methods
Study population
Subjects included 2037 hypertensive adults participating in the Genetic Epidemiology Network of Arteriopathy (GENOA) study, a multicenter community-based study of hypertensive sibships that aims to identify genes influencing blood pressure (BP) levels and the development of target organ damage due to hypertension.17 Participants belonged to sibships with at least 2 members diagnosed with hypertension before age 60 years. Recruitment and subject characteristics in the initial phase of the GENOA study (9/1995 to 6/2001), have been previously described.13 Between December 2000 and October 2004, 1170 of the original GENOA-Rochester participants and 1350 of the original GENOA-Jackson participants returned for a second study visit to undergo measurement of conventional and novel risk factors including LDL particle size and target-organ damage phenotypes. For the present study, we excluded normotensive participants (n = 311 in Jackson and n = 305 in Rochester). We also excluded subjects missing LDL particle size or any of the other risk factor or behavioral measurements, leaving a final study sample of 1982 subjects. The study was approved by the Institutional Review Boards of the Mayo Clinic, Rochester MN and University of Mississippi, Jackson MS. Written informed consent was obtained from each participant.
Height was measured by stadiometer, weight by electronic balance, and body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Waist circumference was measured at the level of the umbilicus at the end of a relaxed exhalation. Resting systolic BP and diastolic BP were measured by trained study coordinators using random zero sphygmomanometer and cuffs appropriate for arm size. Three readings were taken in the right arm after the subject had rested in the sitting position for at least 5 minutes; the last 2 readings were averaged for the analyses. The diagnosis of hypertension was established by one of the authors (S.T.T.) based on BP levels measured at the study visit (≥140/90 mm Hg) or a prior diagnosis of hypertension and current treatment with antihypertensive medications. Metabolic syndrome was defined based on the National Cholesterol Education Program (NCEP) criteria.18 Diabetes was considered present if the subject was being treated with insulin or oral agents or had a fasting glucose level ≥ 126 mg/dL. “Ever” smoking was defined as having smoked more than 100 cigarettes. Each prescription drug recorded at the study visit was assigned a code number corresponding to the first six digits of the Medi-Span Generic Product Identifier.19 This number identifies pharmacologically equivalent drug products and was used to categorize agents with a similar therapeutic action.19
Lifestyle variables
We constructed a physical activity scale by considering the responses to questions on how many hours per day of heavy activity, moderate activity, slight activity, and sedentary activity the participant engaged in. Specifically, the physical activity score was derived as follows: 3*heavy + 2*moderate + light (hours). Alcohol intake was quantified as ounces of alcohol per month and was estimated from responses to questions on the frequency (servings per week or servings per month), and ounces per serving of: beer, wine, hard liquor, wine cooler, and sake. The ounces per month of each of these categories were then multiplied by 5%, 12%, 40%, 8%, and 15%, respectively and summed to give ounces of alcohol per month. This variable was highly skewed, and was also transformed to a log scale after adding 1, for analysis purposes.
Lipid measures and LDL particle size
Blood was drawn by venipuncture after an overnight fast, and all measurements were performed in a single core laboratory. Serum cholesterol, triglycerides, and HDL cholesterol were measured by standard enzymatic methods. LDL cholesterol was estimated using the Friedewald equation.20 Mean LDL particle size was measured by polyacrylamide gel electrophoresis as described previously.21 Two controls (mean LDL particle size 264 Å and 254 Å) were analyzed with every 10 study samples. Inter-assay coefficients of variation were 0.77% (standard deviation = 2.0 Å), and 1.46% (standard deviation = 3.7 Å), respectively.
Statistical Methods
All analyses were performed separately in men and women. Plasma triglyceride levels and alcohol intake were log transformed due to their skewed distribution. Ethnic differences in LDL particle size were assessed before and after adjustment for CHD risk factors, log triglycerides, and estrogen use (in women). In each ethnic group, we assessed the correlation of LDL particle size with the following: a) risk factors for CHD – age, total cholesterol, HDL cholesterol, log triglycerides, systolic BP, fasting blood sugar, diabetes, and metabolic syndrome; b) measures of adiposity – BMI, waist circumference, and waist-to-hip ratio; c) use of medications: statins; and estrogen replacement therapy (in women); d) lifestyle variables: physical activity and alcohol intake. Stepwise multiple linear regression models that included the above covariates as predictor variables were fit to identify significant predictors of LDL particle size in each sex. Multivariable regression analyses were also performed after excluding subjects on lipid-lowering medications and estrogen and by stratifying on diabetic status.
Because of the presence of sibships in the sample, population-averaged generalized estimating equations (GEE)22 were used to assess the possible impact of familial correlations on the relationships between predictor and outcome variables. We also preformed the multivariable analyses randomly selecting only 1 sib from each sibship.
Results
The mean ages of African American men and women were greater than in their non-Hispanic white counterparts (Table 1). Means for both systolic and diastolic BP were higher in African American men and women than in their non-Hispanic white counterparts (Table 1). In men, mean BMI, waist circumference, and waist-to-hip ratio were greater in non-Hispanic whites than in African Americans. In contrast, among women, mean BMI, waist circumference, and waist-to-hip ratio were higher in African Americans than in non-Hispanic whites. Mean fasting blood sugar was also higher in African American women than in non-Hispanic white women. The prevalence of metabolic syndrome was lower in African American men than in non-Hispanic men, but among women, no significant difference in prevalence was noted. In both sexes, the prevalence of diabetes was higher in African Americans than in non-Hispanic whites.
Table 1. Sample characteristics.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Characteristic | African American
n = 314 |
Non-Hispanic white
n = 364 |
P | African American
n = 817 |
Non-Hispanic white
n = 487 |
P |
| Age, years | 64.84 ± 8.6 | 62.17 ± 8.7 | <.0001 | 64.16 ± 8.9 | 61.28 ± 9.2 | <.0001 |
| Systolic BP, mm Hg | 140.75 ± 20.9 | 134.65 ± 15.8 | <.0001 | 143.05 ± 21.3 | 136.63 ± 17.7 | <.0001 |
| Diastolic BP, mm Hg | 82.77 ± 11.9 | 75.95 ± 9.3 | <.0001 | 79.17 ± 11.2 | 73.76 ± 9.4 | <.0001 |
| BMI, kg/m2 | 29.57 ± 4.8 | 31.03 ± 4.9 | 0.0001 | 32.86 ± 7.0 | 31.52 ± 6.8 | 0.005 |
| Waist circumference, cms | 104.71 ± 12.5 | 108.45 ± 12.4 | 0.0002 | 104.76 ± 15.1 | 98.25 ± 16.1 | <.0001 |
| Waist-to-hip ratio | 0.94 ± 0.05 | 1.00 ± 0.1 | <.0001 | 0.88 ± 0.1 | 0.86 ± 0.1 | 0.003 |
| Fasting blood glucose, mg/dL | 118.10 ± 57.4 | 111.88 ± 28.1 | 0.080 | 114.63 ± 48.2 | 105.55 ± 24.8 | <.0001 |
| Metabolic syndrome, % | 49.68 | 58.52 | 0.010 | 60.22 | 60.16 | 0.891 |
| Diabetes mellitus, % | 34.71 | 21.15 | 0.0001 | 35.86 | 18.48 | <.0001 |
| History of smoking, % | 65.61 | 62.64 | 0.262 | 30.23 | 39.63 | 0.001 |
| Alcohol, oz/month | 3.04 ±7.5 | 9.41 ±14.0 | <.0001 | 0.75 ±3.8 | 2.89 ±6.2 | <.0001 |
| Physical activity score | 10.00 ±4.1 | 13.31 ±4.8 | <.0001 | 9.49 ±3.1 | 12.41 ±4.6 | <.0001 |
| Hypertension med use, % | 88.22 | 92.86 | 0.039 | 90.94 | 93.84 | 0.056 |
| Statin use, % | 23.57 | 43.13 | <.0001 | 20.69 | 27.93 | 0.007 |
| Estrogen use, % | – | – | – | 24.6 | 43.53 | <.0001 |
BP, blood pressure; BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein
History of smoking was more prevalent in non-Hispanic white women than in African American women but was not significantly different between the men in the 2 ethnic groups. Statin use was significantly less common in African American men and women than in their non-Hispanic white counterparts. The use of estrogen replacement was significantly more common in non-Hispanic white women than in African American women (Table 1). Physical activity scores and alcohol intake were higher in non-Hispanic whites than in African Americans.
HDL cholesterol levels were higher and triglyceride levels lower in African American men and women than in their non-Hispanic white counterparts (Table 2). However, LDL particle size was lower in African American men and women than in their non-Hispanic white counterparts (Table 2). After adjustment for CHD risk factors, log triglycerides, and estrogen use (in women), ethnic differences in mean LDL particle size remained significant (mean ± SD; men, 267.6±5.2 Å vs. 270.2±4.8 Å, P < 0.0001; women 268.7±5.1 Å vs. 271.3±5.1 Å, P < 0.0001). The prevalence of LDL particle size < 270 Å (the median LDL particle size in the combined cohort) was significantly greater in African American men than in non-Hispanic white men (Table 2). After adjustment for CHD risk factors, log triglycerides, and estrogen use (in women), the prevalence of LDL particle size <270 Å was significantly greater in African American men and women than in their non-Hispanic white counterparts (men 35.2% vs. 13.8%, P < 0.0001; women 25.1% vs. 9.8%, P < 0.0001)
Table 2. Lipids and low-density lipoprotein particle size.
| African American
n = 314 |
Non-Hispanic white
n = 364 |
P | African American
n = 817 |
Non-Hispanic white
n = 487 |
P | |
|---|---|---|---|---|---|---|
| Total cholesterol, mg/dL | 191.09 ± 41.6 | 186.73 ± 30.0 | 0.221 | 205.63 ± 41.4 | 204.11 ± 34.3 | 0.507 |
| HDL cholesterol, mg/dL | 49.40 ± 15.1 | 44.42 ± 11.8 | <.0001 | 60.29 ± 17.4 | 55.68 ± 14.9 | <.0001 |
| LDL cholesterol, mg/dL | 118.59 ± 38.6 | 113.28 ± 29.1 | 0.089 | 121.61 ± 38.4 | 115.94 ± 31.9 | 0.004 |
| Triglycerides, mg/dL | 120.80 ± 76.2 | 156.48 ± 98.0 | <.0001 | 120.98 ± 67.9 | 168.36 ± 87.3 | <.0001 |
| Log triglycerides | 4.67 ± 0.5 | 4.92 ± 0.5 | <.0001 | 4.68 ± 0.5 | 5.01 ± 0.5 | <.0001 |
| LDL particle size, Å | 268.42 ± 5.6 | 269.71 ± 4.9 | 0.039 | 269.18 ± 4.9 | 270.34 ± 5.0 | 0.011 |
| LDL particle size <270 Å, % | 56.37 | 47.80 | 0.095 | 52.02 | 42.30 | 0.019 |
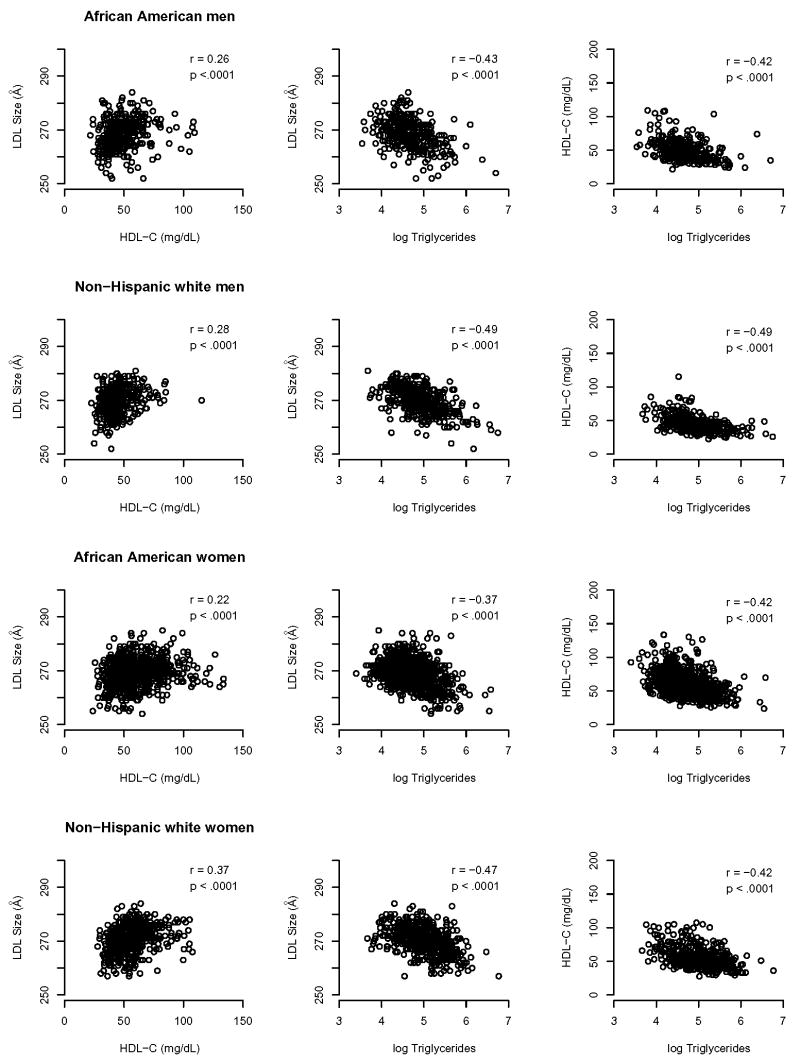
As expected, LDL particle size was significantly correlated with HDL cholesterol and log triglycerides in men and women of both ethnic groups (Figure 1, Table 3). Spearman rank correlations between LDL particle size and other variables are shown in Table 3. In men and women of both ethnic groups, LDL particle size was positively correlated with age. In addition, LDL particle size was negatively correlated with fasting blood glucose (in African American and non-Hispanic white women), BMI (in non-Hispanic white men and women), waist circumference (in non-Hispanic white men and women), and estrogen use (in African American women).
Figure 1.
Scatterplots showing correlations between LDL particle size, HDL cholesterol, and log triglycerides in hypertensive African American men and women and their non-Hispanic white counterparts.
Table 3. Spearman rank correlations (P values) between LDL particle size and selected variables.
| Characteristic | Men | Women | ||
|---|---|---|---|---|
| African American
n = 314 |
Non-Hispanic white
n = 364 |
African American
n = 817 |
Non-Hispanic white
n = 487 |
|
| Age, years | 0.38 | 0.14 | 0.26 | 0.13 |
| (<.0001) | (0.009) | (<.0001) | (0.004) | |
| Systolic BP, mm Hg | 0.04 | −0.03 | 0.04 | 0.11 |
| (0.46) | (0.53) | (0.28) | (0.02) | |
| BMI, kg/m2 | −0.09 | −0.18 | −0.01 | −0.14 |
| (0.11) | (0.0007) | (0.74) | (0.002) | |
| Waist circumference, cms | −0.04 | −0.11 | −0.003 | −0.14 |
| (0.43) | (0.04) | (0.94) | (0.002) | |
| Waist-to-hip ratio | −0.01 | −0.11 | −0.02 | −0.18 |
| (0.90) | (0.04) | (0.64) | (0.0001) | |
| Fasting blood glucose, mg/dL | −0.02 | −0.05 | −0.10 | −0.09 |
| (0.71) | (0.39) | (0.003) | (0.04) | |
| Metabolic syndrome | −0.18 | −0.26 | −0.15 | −0.36 |
| (0.001) | (<.0001) | (<.0001) | (<.0001) | |
| Diabetes | 0.10 | −0.01 | −0.05 | −0.07 |
| (0.08) | (0.79) | (0.12) | (0.13) | |
| History of smoking | −0.08 | −0.08 | −0.06 | −0.03 |
| (0.15) | (0.13) | (0.09) | (0.47) | |
| Log (alcohol, oz/month) | −0.14 | −0.03 | −0.10 | 0.05 |
| (0.01) | (0.52) | (0.005) | (0.26) | |
| Physical activity score | −0.25 | 0.02 | −0.14 | 0.06 |
| (<.0001) | (0.73) | (<.0001) | (0.16) | |
| (0.007) | (0.54) | (<.0001) | (0.32) | |
| Statin use | −0.03 | −0.02 | 0.02 | 0.02 |
| (0.58) | (0.74) | (0.63) | (0.63) | |
| Estrogen use | −0.11 | −0.0008 | ||
| — | — | (0.003) | (0.99) | |
| Total cholesterol, mg/dL | −0.21 | −0.10 | −0.14 | −0.18 |
| (<.0002) | (0.05) | (<.0001) | (<.0001) | |
| HDL cholesterol, mg/dL | 0.26 | 0.28 | 0.22 | 0.37 |
| (<.0001) | (<.0001) | (<.0001) | (<.0001) | |
| Log triglycerides | −0.43 | −0.49 | −0.37 | −0.47 |
| (<.0001) | (<.0001) | (<.0001) | (<.0001) | |
BP, blood pressure; BMI, body mass index; HDL, high-density lipoprotein
After adjustment for CHD risk factors, medication use, and lifestyle variables, African American ethnicity was associated with a lower LDL particle size in both men and women (Table 4). In addition, in men, higher total cholesterol, greater log triglycerides, lower HDL cholesterol, history of smoking, and greater physical activity were associated with smaller LDL particle size. In women, lower age, higher total cholesterol, greater log triglycerides, lower HDL cholesterol, greater physical activity, and estrogen use were associated with smaller LDL particle size (Table 4). Neither alcohol intake nor BMI had an independent association with LDL particle size in men or women in the multiple regression models. African American ethnicity was associated with lower LDL particle size even if only 1 sib from a sibship was selected for analyses, in subjects who were not on lipid lowering agents or estrogen, and in diabetics as well as non-diabetics (analyses not shown).
Table 4. LDL particle size predictors – Stepwise multivariable linear regression.
| Men, n = 678 | Women, n = 1304 | |||
|---|---|---|---|---|
| Variable | B ± SD | P | B ± SD | P |
| Age, years | 0.11 ±0.02 | <.0001 | 0.12 ±0.013 | <.0001 |
| African American ethnicity | −3.02 ±0.43 | <.0001 | −3.00 ±0.33 | <.0001 |
| HDL cholesterol, mg/dL | 0.033 ±0.015 | 0.022 | 0.044 ±0.010 | <.0001 |
| Log triglycerides | −4.11 ±0.42 | <.0001 | −3.61 ±0.34 | <.0001 |
| Total cholesterol, mg/dL | −0.014 ±0.005 | 0.007 | −0.018 ±0.004 | <.0001 |
| History of smoking | −0.91 ±0.35 | 0.010 | – | – |
| Physical activity score | −0.13 ±0.04 | 0.0004 | −0.080 ±0.032 | 0.014 |
| Estrogen use | – | – | −0.52 ±0.27 | 0.053 |
LDL, low-density lipoprotein; HDL, high-density lipoprotein
Discussion
The main finding of this study is that LDL particle size is significantly lower in African American hypertensive subjects than in their non-Hispanic white counterparts. The smaller LDL particle size in hypertensive African Americans cannot be explained by differences in HDL cholesterol and triglyceride levels and is independent of other known correlates of LDL particle size, including age, sex, and BMI.
Our findings are in contrast to previous studies reporting higher LDL particle size in African Americans than in non-Hispanic whites. In the Insulin Resistance Atherosclerosis Study, Haffner et al12 found higher LDL particle size in African Americans than in their Hispanic and non-Hispanic white counterparts. Our results also differ from those of Johnson et al23 who in a study of sedentary, overweight individuals, reported higher LDL particle size in African Americans than in whites and those of Kral et al24 who reported higher LDL particle size in asymptomatic African American siblings of persons with early-onset CHD than in their non-Hispanic white counterparts. In contrast to participants in these studies, our subjects were older, and by design, all were hypertensive.
Besides the significant differences in participant characteristics, it is important to note that Haffner et al12 found that the difference in LDL particle size between African Americans and non-Hispanic whites was not statistically significant after adjustment for age, sex, triglycerides, HDL cholesterol, fasting glucose, and insulin sensitivity. In the study by Johnson et al,23 the LDL particle size difference between the ethnic groups was no longer significant after adjustment for triglycerides. Methodologic differences in assessing LDL particle size also exist between these studies and the present study. Kral et al24 did not measure LDL particle size directly but used LDL cholesterol/apolipoprotein B ratio as a surrogate for LDL particle size.
Although African Americans are considered to be more hyperinsulinemic and insulin resistant than non-Hispanic whites,15 the prevalence of the metabolic syndrome has been reported to be lower in African Americans than in other ethnic groups.25 In our sample, the prevalence of metabolic syndrome, as defined by NCEP criteria,18 was similar in women belonging to the 2 ethnic groups and was significantly lower in African American men than in non-Hispanic white men. The lower prevalence of metabolic syndrome reported in African Americans26, 27 may be a consequence of the higher HDL and lower triglyceride levels in this ethnic group.28 However, the presence of apparently favorable levels of triglycerides and HDL cholesterol does not appear to afford protection from higher rates of CHD in African Americans.29 The use of uniform cut points to define dyslipidemia may result in missed identification of African Americans who remain at high risk for CHD.28 We found that as the number of components of the metabolic syndrome increased, LDL particle size decreased, with the lowest particle size noted in subjects with all five components of the syndrome (analyses not shown). Small LDL particle size has been found to be a marker for the metabolic syndrome in non-Hispanic whites30 and its utility as a marker of this syndrome in African Americans merits further investigation.
In contrast to the metabolic syndrome, the prevalence of diabetes in African Americans was significantly higher than in non-Hispanic whites (Table 1). In addition to adjusting for diabetic status in multivariable regression models, we performed analyses stratified on the presence of diabetes. We found that African American ethnicity was associated with lower LDL particle size in diabetics as well as non-diabetics. We also found African American ethnicity to be associated with lower LDL particle size in the normotensive siblings of the hypertensive subjects (analyses not shown). Since the normotensive participants belong to sibships ascertained on the basis of essential hypertension, they may share a genetic predisposition to metabolic abnormalities even without manifesting elevated blood pressure as a phenotype.
Our finding of ethnic differences in LDL particle size could be due to dissimilarities in unknown or unmeasured environmental factors between the 2 ethnic groups or possible genetic differences in lipoprotein metabolism. Although we adjusted for “lifestyle variables” – physical activity and alcohol use – other unmeasured environmental factors, particularly dietary habits, may confound the observed association of ethnicity and LDL particle size. Small LDL particle size clusters within families shows significant heritability,31 and segregation analyses suggest the presence of a single major gene for this trait.5 Linkage analyses suggest several candidate genes, including the LDL receptor, cholesteryl ester transfer protein, ApoA1/ApoCIII/ApoIV gene complex, and manganese superoxide dismutase.32 Variations in these and other plasma enzymes such as lipoprotein lipase and hepatic lipase that are known to modulate the composition of lipoproteins, may explain the differences in LDL particle size between the 2 ethnic groups.
A strength of the present study is the use of a uniform protocol in the 2 ethnic groups including questionnaires, anthropometric measurements, and lipid and LDL particle size measurements that were made in a single core laboratory. However, our findings should be confirmed using other available methods of measuring LDL particle size. A substantial proportion of patients were on statins, however, these drugs have not been shown to have a significant effect on LDL particle size.33 Our inferences were unchanged when we excluded patients on statins (analyses not shown).
Levels of HDL cholesterol and triglycerides do not explain the higher CHD rates in hypertensive African Americans, and it is possible that alterations in the distribution of the size of LDL or HDL particles contribute. The lower LDL particle size in hypertensive African Americans than in their non-Hispanic white counterparts may be a potential mechanism of increased cardiovascular risk in the former. A causal role for small LDL particles in the etiology of CHD is suggested by studies showing such particles to have several atherogenic characteristics including long residence time in the plasma, greater susceptibility to oxidation, increased binding affinity for intimal proteoglycans, and increased ability to cross into the subintimal space.6 Indeed, several prospective studies have shown small LDL particle size to be associated with a greater risk of CHD events.7-9
Conclusion
In conclusion, in the present study, we found that LDL particle size is lower in hypertensive African Americans than in their non-Hispanic white counterparts, despite lower triglyceride and higher HDL cholesterol levels in the former. Further confirmatory studies are needed as well as investigation to understand the pathophysiologic basis for this observation and whether the lower LDL particle size contributes to higher risk of CHD in hypertensive African Americans.
Acknowledgments
This work was supported by grants HL81331, and M01 RR00585 from the National Institutes of Health.
Abbreviations
- BMI
Body mass index
- CHD
Coronary heart disease
- HDL
High-density lipoprotein
- LDL
Low-density lipoprotein
Footnotes
No conflicts of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Iftikhar J. Kullo, Divisions of Cardiovascular Diseases, Mayo Clinic and Foundation, Rochester, MN.
M. Fuad Jan, Drexel University, Philadelphia PA.
Kent R. Bailey, Department of Biostatistics, Mayo Clinic and Foundation, Rochester, MN.
Thomas H. Mosley, Jr., University of Mississippi, Jackson MS.
Stephen T. Turner, Division of Nephrology and Hypertension, Mayo Clinic and Foundation, Rochester, MN.
References
- 1.Sniderman AD, Pedersen T, Kjekshus J. Putting low-density lipoproteins at center stage in atherogenesis. Am J Cardiol. 1997;79:64–7. doi: 10.1016/s0002-9149(96)00677-7. [DOI] [PubMed] [Google Scholar]
- 2.Krauss RM, Burke DJ. Identification of multiple subclasses of plasma low density lipoproteins in normal humans. J Lipid Res. 1982;23:97–104. [PubMed] [Google Scholar]
- 3.Otvos JD, Jeyarajah EJ, Bennett DW, Krauss RM. Development of a proton nuclear magnetic resonance spectroscopic method for determining plasma lipoprotein concentrations and subspecies distributions from a single, rapid measurement. Clin Chem. 1992;38:1632–8. [PubMed] [Google Scholar]
- 4.Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82:495–506. doi: 10.1161/01.cir.82.2.495. [DOI] [PubMed] [Google Scholar]
- 5.Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43:1363–79. doi: 10.1194/jlr.r200004-jlr200. [DOI] [PubMed] [Google Scholar]
- 6.Kullo IJ, Ballantyne CM. Conditional risk factors for atherosclerosis. Mayo Clin Proc. 2005;80:219–30. doi: 10.4065/80.2.219. [DOI] [PubMed] [Google Scholar]
- 7.Gardner CD, Fortmann SP, Krauss RM. Association of small low-density lipoprotein particles with the incidence of coronary artery disease in men and women. JAMA. 1996;276:875–81. [PubMed] [Google Scholar]
- 8.Stampfer MJ, Krauss RM, Ma J, Blanche PJ, Holl LG, Sacks FM, Hennekens CH. A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction. JAMA. 1996;276:882–8. [PubMed] [Google Scholar]
- 9.Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Despres JP. Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men. Prospective results from the Quebec Cardiovascular Study. Circulation. 1997;95:69–75. doi: 10.1161/01.cir.95.1.69. [DOI] [PubMed] [Google Scholar]
- 10.Cromwell WC, Otvos JD. Low-density lipoprotein particle number and risk for cardiovascular disease. Curr Atheroscler Rep. 2004;6:381–7. doi: 10.1007/s11883-004-0050-5. [DOI] [PubMed] [Google Scholar]
- 11.Tyroler HA, Hames CG, Krishan I, Heyden S, Cooper G, Cassel JC. Black-white differences in serum lipids and lipoproteins in Evans County. Prev Med. 1975;4:541–9. doi: 10.1016/0091-7435(75)90040-7. [DOI] [PubMed] [Google Scholar]
- 12.Haffner SM, D'Agostino R, Jr, Goff D, Howard B, Festa A, Saad MF, Mykkanen L. LDL size in African Americans, Hispanics, and non-Hispanic whites: the insulin resistance atherosclerosis study. Arterioscler Thromb Vasc Biol. 1999;19:2234–40. doi: 10.1161/01.atv.19.9.2234. [DOI] [PubMed] [Google Scholar]
- 13.O'Meara JG, Kardia SL, Armon JJ, Brown CA, Boerwinkle E, Turner ST. Ethnic and sex differences in the prevalence, treatment, and control of dyslipidemia among hypertensive adults in the GENOA study. Arch Intern Med. 2004;164:1313–8. doi: 10.1001/archinte.164.12.1313. [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–11. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 15.Haffner SM, D'Agostino R, Saad MF, Rewers M, Mykkanen L, Selby J, Howard G, Savage PJ, Hamman RF, Wagenknecht LE, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes. 1996;45:742–8. doi: 10.2337/diab.45.6.742. [DOI] [PubMed] [Google Scholar]
- 16.Lipton RB, Liao Y, Cao G, Cooper RS, McGee D. Determinants of incident non-insulin-dependent diabetes mellitus among blacks and whites in a national sample. The NHANES I Epidemiologic Follow-up Study. Am J Epidemiol. 1993;138:826–39. doi: 10.1093/oxfordjournals.aje.a116786. [DOI] [PubMed] [Google Scholar]
- 17.Boerwinkle E. Multi-Center Genetic Study of Hypertension: The Family Blood Pressure Program (FBPP) Hypertension. 2002;39:3–9. doi: 10.1161/hy1201.100415. [DOI] [PubMed] [Google Scholar]
- 18.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Medi-Span, Proprietary Concepts. Master Drug Data Base Documentation Manual. Indianapolis, Indiana; Medi-Span Inc: 1996. [Google Scholar]
- 20.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 21.Hoefner DM, Hodel SD, O'Brien JF, Branum EL, Sun D, Meissner I, McConnell JP. Development of a rapid, quantitative method for LDL subfractionation with use of the Quantimetrix Lipoprint LDL System. Clin Chem. 2001;47:266–74. [PubMed] [Google Scholar]
- 22.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 23.Johnson JL, Slentz CA, Duscha BD, Samsa GP, McCartney JS, Houmard JA, Kraus WE. Gender and racial differences in lipoprotein subclass distributions: the STRRIDE study. Atherosclerosis. 2004;176:371–7. doi: 10.1016/j.atherosclerosis.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 24.Kral BG, Becker LC, Yook RM, Blumenthal RS, Kwiterovich PO, Jr, Otvos JD, Becker DM. Racial differences in low-density lipoprotein particle size in families at high risk for premature coronary heart disease. Ethn Dis. 2001;11:325–7. [PubMed] [Google Scholar]
- 25.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 26.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003;163:427–36. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ford ES. Factor analysis and defining the metabolic syndrome. Ethn Dis. 2003;13:429–37. [PubMed] [Google Scholar]
- 28.Giannini E, Testa R. The metabolic syndrome: all criteria are equal, but some criteria are more equal than others. Arch Intern Med. 2003;163:2787–8. doi: 10.1001/archinte.163.22.2787. [DOI] [PubMed] [Google Scholar]
- 29.Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O'Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Jr, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart Disease and Stroke Statistics: 2006 Update. A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 30.Kathiresan S, Otvos JD, Sullivan LM, Keyes MJ, Schaefer EJ, Wilson PW, D'Agostino RB, Vasan RS, Robins SJ. Increased small low-density lipoprotein particle number. A prominent feature of the Metabolic Syndrome in the Framingham Heart Study. Circulation. 2005;113:20–9. doi: 10.1161/CIRCULATIONAHA.105.567107. [DOI] [PubMed] [Google Scholar]
- 31.Kullo IJ, de Andrade M, Boerwinkle E, McConnell JP, Kardia SL, Turner ST. Pleiotropic genetic effects contribute to the correlation between HDL cholesterol, triglycerides, and LDL particle size in hypertensive sibships. Am J Hypertens. 2005;18:99–103. doi: 10.1016/j.amjhyper.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Rotter JI, Bu X, Cantor RM, Warden CH, Brown J, Gray RJ, Blanche PJ, Krauss RM, Lusis AJ. Multilocus genetic determinants of LDL particle size in coronary artery disease families. Am J Hum Genet. 1996;58:585–94. [PMC free article] [PubMed] [Google Scholar]
- 33.Gaw A. Can the clinical efficacy of the HMG CoA reductase inhibitors be explained solely by their effects on LDL-cholesterol? Atherosclerosis. 1996;125:267–9. doi: 10.1016/0021-9150(96)05887-x. [DOI] [PubMed] [Google Scholar]