Abstract
Background. A 29-year-old woman who presented with fatigue and jaundice was found to have an obstructing mass at the bifurcation of the bile duct. The patient underwent a successful left hepatectomy with resection of the bile duct bifurcation and a reconstruction with a right hepaticojejunostomy. Pathology revealed an atypical carcinoid tumour of the left extrahepatic bile duct, with perineural and lymphatic invasion. The patient subsequently developed multiple metastases in the remaining liver. Methods. In the absence of extrahepatic disease, the patient underwent a successful liver transplant. Results. Two years later she remains disease-free. Discussion. To our knowledge this is the first report of a biliary carcinoid treated with hepatectomy and finally with liver transplantation, with excellent results. The biological behaviour of these rare tumours mandates aggressive surgical management.
Keywords: Carcinoid metastases, liver transplantation
Introduction
Over 95% of extrahepatic bile duct (EHBD) malignancies are adenocarcinomas, while only 0.2–0.3% are carcinoid tumors 1. To date there have been 31 cases of adult extrahepatic bile duct carcinoids reported in the literature. Of them, only two were treated with liver transplantation, one for liver failure due to liver replacement by tumour 3, while the other was transplanted for apparent cholangiocarcinoma 2.
This report consists of a case of a primary carcinoid of the proximal bile ducts, initially treated by partial hepatectomy and ultimately treated by liver transplantation for intrahepatic recurrence.
Case report
A 29-year-old female presented with a 3-month history of progressive fatigue, pruritus, dark urine and pale stools. She had marked jaundice, but no hepatosplenomegaly, abdominal mass or lymphadenopathy. Investigations revealed conjugated hyperbilirubinaemia, elevated alkaline phosphatase and mildly elevated liver enzymes. Ultrasonography (US) demonstrated a normal common bile duct (CBD), no CBD stones, but a dilated left hepatic duct and a bile duct bifurcation mass. Computed tomography (CT) scan confirmed a mass at the CBD bifurcation with proximal left-sided bile duct dilatation, confirmed by percutaneous transhepatic cholangiogram (PTC). During the cholangiogram an external-internal biliary stent was placed. A PTC-guided core biopsy showed poorly differentiated adenocarcinoma. An en bloc resection of the left liver, the caudate lobe, the CBD and its bifurcation was performed. Biliary continuity was established by a right hepaticojejunostomy.
The tumour involved the entire extrahepatic segment of the left hepatic duct, including the bifurcation and invaded into the adjacent liver, forming a 2.8-cm mass in the liver parenchyma. The resection margins were free of tumour, and all the sampled lymph nodes were free of metastasis. Histology showed an atypical carcinoid of the left hepatic duct, i.e. lowgrade malignant neuroendocrine neoplasm (with immunoreactivity to chromogranin A and synaptophysin), with focal perineural and lymphatic invasion (Figures 1 and 2).
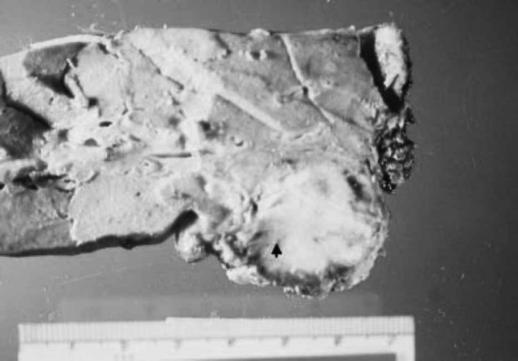
Figure 1. .
Gross specimen showing tumour invasion into adjacent liver parenchyma (bold arrow).
Figure 2. .
Light microscopy (H&E×100) showing lymphatic invasion (bold arrow).
Postoperatively a somatostatin nuclear scan did not demonstrate any disease. One year after hepatectomy, serum biochemistry showed a rising alanine transferase. US and CT scans revealed intrahepatic bile duct dilatation and magnetic resonance imaging (MRI) showed extensive intrahepatic metastatic disease. A complete metastatic workup was undertaken, including positron emission tomography (PET scan), which revealed metastatic foci only in the liver.
The patient underwent a successful orthotopic liver transplantation (OLT) 2 weeks later. The explant showed multiple nodules with extension to the hilar area and to the right adrenal gland, which was removed en bloc. All lymph nodes were negative for metastasis. Currently she is 2 years post transplant, with no evidence of disease recurrence on MRI.
Discussion
Pilz described the first carcinoid arising from the common bile duct in 1961. Since then only 31 adult cases of EHBD carcinoids have been described.
The biological behaviour of these tumours; i.e. slow growing and local spread, mandates an aggressive surgical approach, the only chance for a cure. All patients undergoing a "curative" resection were alive and recurrence-free during the last follow-up 4, which was not true for patients undergoing non-curative resection.
This is the first case described in the literature of a successful liver transplantation for bile duct carcinoid metastatic to the liver following initial tumour resection.
When curative resection is not possible, young patients without extrahepatic disease should be considered for liver transplantation. Presently, this is the only curative option for these patients.
Acknowledgments
G.N.T. was supported by the Gertrude Nemiroff Eliesen Memorial Award, McGill University Health Center Research Institute.
References
- 1.Albores-Saavedra J, Henson DE, Klimstra DS, Armed Forces Institute of Pathology (US), Universities Associated for Research and Education in Pathology.Tumors of the Gallbladder, Extrahepatic Bile Ducts, and Ampulla of Vater. Washington: Armed Forces Institute of Pathology, 2000(available from the American Registry of Pathology, Armed Forces Institute of Pathology). [Google Scholar]
- 2.Turrion VS, Salas C, Alvira LG, Jimenez M, Lucena JL, Ardaiz J. Carcinoid tumour of the common bile duct: an exceptional indication for liver transplantation. Transplant Proc. 2002;34:264. doi: 10.1016/s0041-1345(01)02754-3. [DOI] [PubMed] [Google Scholar]
- 3.Hao L, Friedman AL, Navarro VJ, West B, Robert ME. Carcinoid tumor of the common bile duct producing gastrin and serotonin. J Clin Gastroenterol. 1996;23:63. doi: 10.1097/00004836-199607000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Ross AC, Hurley JB, Hay WB, Rusnak CH, Petrunia DM. Carcinoids of the common bile duct: a case report and literature review. Can J Surg. 1999;42:59. [PMC free article] [PubMed] [Google Scholar]