Abstract
Background: Anxiety and depressive disorders have a significant and negative impact on quality of life. However, less is known about the effects of anxiety and depressive symptoms on quality of life. The purpose of this study was to examine the impact of anxiety and depressive symptoms on emotional and physical functioning, the effects of anxiety symptoms on functioning independent of depressive symptoms, and the effects of depressive symptoms on functioning independent of anxiety symptoms.
Method: Participants included 919 patients, recruited from 2 university-affiliated primary care clinics between May 2004 and September 2006, who completed self-report measures of anxiety symptoms, depressive symptoms, and quality of life.
Results: Almost 40% of the sample reported anxiety symptoms and 30% reported depressive symptoms. In both unadjusted and adjusted models, anxiety and depressive symptoms were significantly associated with all domains of quality of life. When anxiety and depressive symptoms were added simultaneously, both remained significant. As the severity of anxiety or depressive symptoms increased, quality of life decreased. Furthermore, patients with moderate to severe anxiety or depressive symptoms had greater impairments in most quality of life domains than patients with acute myocardial infarction, congestive heart failure, or diabetes.
Conclusion: Detection and treatment of anxiety and depressive symptoms in the primary care setting should be emphasized.
The prevalence of mental disorders is high, with reports of up to 30% in the general population.1 Anxiety and mood disorders account for the largest percentage of mental disorders by far. Results of the National Comorbidity Survey Replication indicate a 12-month prevalence of 18.1% for anxiety disorders and 9.5% for mood disorders.2 Of the people who seek treatment for anxiety and depression, the majority first go to their primary care physician (PCP).3 Nonetheless, only a small percentage of PCP visits are due to a primary psychiatric problem.4
Anxiety and depressive disorders and symptoms significantly impair functioning in a number of areas, including work functioning, social functioning, and health.5,6 In fact, quality of life among depressed adults is more impaired than that of adults with diabetes, hypertension, and chronic lung disease.7 Similarly, anxiety has been also associated with a number of negative outcomes, including decreased work productivity8; impaired work, family, and social functioning9; physical disability10,11; and even mortality.12 Furthermore, it has been demonstrated that individuals with comorbid medical illnesses and anxiety have significantly greater impairment in quality of life than patients without anxiety.13,14 Despite the fact that anxiety disorders are more common than depressive disorders and that anxiety has deleterious effects, little research has focused on the impact of anxiety and depression on functioning independent of each other, allowing for the examination of the relative contribution of each to different areas of functioning.15 Thus, there is debate as to whether the impact of anxiety on functioning is largely due to its comorbidity with depression.
One study that has looked at the independent effects of anxiety and depression on functioning in primary care patients was conducted by Olfson and colleagues.16 They found that both depression and anxiety were associated with significant impairment in multiple domains. When the presence of major depression was controlled, panic disorder remained significantly associated with impairment in work, family, and social functioning. Similar results were found for depression when controlling for anxiety. In their study, however, the measures of functioning were ones that are used primarily in psychiatric studies, making it difficult to compare the impact of anxiety and depression relative to other health conditions. In the current study, the effects of anxiety and depression on quality of life are studied in a large sample of primary care patients employing a commonly used measure of quality of life that allows for comparisons among patients with other health conditions. Furthermore, the current study focuses on anxiety and depressive symptoms rather than using DSM-IV diagnoses because patients in the primary care setting may differ in presentation of symptoms from patients in the psychiatric setting.16
The purposes of this study are (1) to examine the impact of anxiety and depressive symptoms on emotional and physical functioning, (2) to examine the effects of anxiety symptoms on functioning independent of depressive symptoms, and (3) to examine the effects of depressive symptoms on functioning independent of anxiety symptoms. It is hypothesized that impairment will worsen with increasing severity of anxiety and depressive symptoms.
METHOD
Subjects and Procedures
Participants were 919 patients recruited from 2 university-affiliated primary care offices between May 2004 and September 2006. All patients were approached by a research assistant after checking in for their appointment and were asked to complete a brief questionnaire. Participation was completely voluntary. Participants who had difficulty reading or writing were provided with assistance in completing the questionnaires. This study was approved by the Institutional Review Board of Wake Forest University School of Medicine, and all participants provided written informed consent at enrollment.
Measures
Demographics
Participants were asked to indicate their age in years, gender, race, years of education, and marital status.
Health information
Participants indicated whether or not they had been diagnosed with different health conditions, including asthma, cancer, congestive heart failure, coronary artery disease, diabetes, emphysema or chronic obstructive pulmonary disorder (COPD), heart attack, hearing loss, high blood pressure, osteoarthritis, osteoporosis, rheumatoid arthritis, or stroke.
Anxiety
Anxiety was assessed with the Beck Anxiety Inventory (BAI),17 a self-report measure consisting of 21 items that measure symptoms of anxiety (e.g., feeling nervous, heart pounding or racing). The BAI has been validated in samples of medical patients, including patients with acute myocardial infarction,18 patients with COPD,19 and older medical outpatients.20 Participants rated each symptom on a 4-point scale ranging from 0 (“not at all”) to 3 (“severely”). Responses to the individual items were then summed to create a total score. Higher scores indicated greater anxiety. Scores of 0 to 7 indicated minimal anxiety symptoms, scores of 8 to 15 indicated mild anxiety symptoms, and scores of 16 to 63 indicated moderate to severe anxiety symptoms. The internal consistency of the BAI in the current study was 0.93.
Depression
Depression was assessed with the Beck Depression Inventory (BDI),21 a 21-item measure of depressive symptoms. For each item, participants chose the statement that best reflected how they felt. Responses to the individual items were then summed, with scores ranging from 0 to 63. Scores of 0 to 10 indicated minimal depression, scores of 11 to 17 indicated mild depression, and scores of 18 to 63 indicated moderate to severe depressive symptoms. The internal consistency of the BDI in the current study was 0.92.
Functional disability
The Medical Outcomes Study Short-Form 36-Item Health Survey (SF-36)22 was used to assess functioning. The SF-36 contains 8 subscales: physical functioning, role limitations due to physical health problems, role limitations due to emotional health problems, social functioning, pain, vitality, emotional well-being, and general health perceptions. Higher scores on each scale indicated better functioning.
Analyses
Multiple regression analyses were conducted to determine the impact of anxiety and depressive symptoms on quality of life, both individually and jointly. Unadjusted models are presented first. In the adjusted models, demographic information was entered in Step 1 and health and disease-related information was entered in Step 2. In Model 1, anxiety was entered in Step 3. In Model 2, depression was entered in Step 3. Model 3 tested the independent effects of anxiety and depression by entering them simultaneously in the third step. Next, analyses of variance (ANOVAs) were conducted to examine the effects of symptom severity on quality of life. Finally, t tests were conducted to compare the quality of life in patients who reported moderate to severe anxiety or depressive symptoms with normative data from patients with acute myocardial infarction, congestive heart failure, and diabetes.22
RESULTS
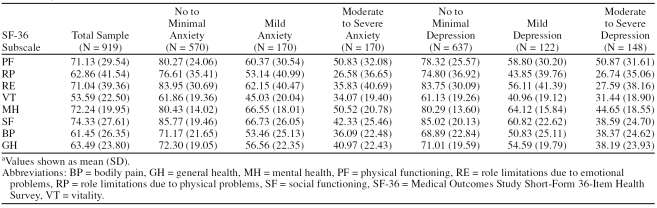
Participants ranged in age from 19 to 92 years, with a mean age of 50.32 years (SD = 16.10). The majority of the sample was female (75.2%), white (64.7%), well educated (mean = 14.12 years, SD = 3.05), and married (61.0%). The most commonly reported health conditions were high blood pressure (33.0%), osteoarthritis (30.6%), and asthma (12.1%). The mean BAI score was 8.74 (SD = 10.33); 62.6% reported no or minimal symptoms of anxiety, 18.7% reported mild anxiety symptoms, and 18.7% reported moderate to severe symptoms of anxiety. The mean BDI score was 9.12 (SD = 9.13). Incidence of depressive symptoms was slightly lower, with 70.2% reporting no or minimal symptoms of depression, 13.5% reporting mild symptoms of depression, and 16.3% reporting moderate to severe symptoms of depression. Mean scores on SF-36 subscales by level of anxiety and depressive symptoms are presented in Table 1.
Table 1.
Quality of Life, as Measured by SF-36 Subscale Scores, by Severity of Anxiety and Depressive Symptoms in Primary Care Patientsa
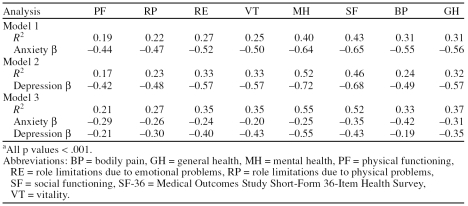
The results of the unadjusted models are presented in Table 2. Anxiety was significantly associated with all domains of quality of life (all p values < .001). The cognitive and somatic items of the BAI were summed separately and the analyses were repeated. The results were unchanged, as both the cognitive and somatic anxiety symptoms were associated with all domains of quality of life (all p values < .001; data not shown). Similarly, depression was also associated with all domains of quality of life (all p values < .001).
Table 2.
Outcomes of Unadjusted Multiple Regression Analyses Examining Anxiety and Depression Symptoms as Predictors of Quality of Life by SF-36 Subscalea
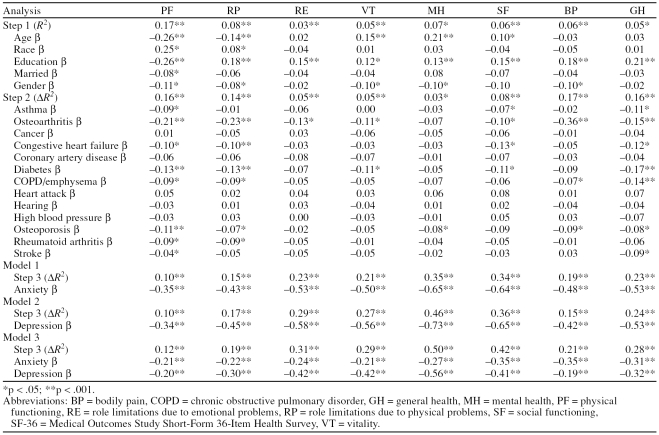
Table 3 presents the results of the multivariate analyses. Demographic factors were significantly related to quality of life. Education was related to all domains of quality of life. Being male was associated with better physical functioning, greater vitality, better mental health, less bodily pain, and fewer role limitations due to physical problems. Age had a differential relationship with quality of life: increased age was associated with greater vitality, greater mental health, and greater social functioning, but it was also associated with poorer physical functioning and more role limitations due to physical problems. Finally, race was associated with physical functioning and role limitations due to physical health, and marital status was associated with physical functioning. Similarly, the regression analyses indicated that health conditions had a significant effect on quality of life. The diseases with the greatest effects were osteoarthritis, diabetes, osteoporosis, and COPD.
Table 3.
Multiple Regression Analyses Examining Anxiety and Depression Symptoms as Predictors of Quality of Life by SF-36 Subscale, Adjusting for Demographics and Health-Related Information
In Model 1, anxiety was entered into the regression analysis after controlling for demographics and health-related conditions. Anxiety was significantly associated with all domains of quality of life and accounted for 10% to 35% of the variance. Similarly, Model 2 demonstrates that depression also had a significant effect on all domains of quality of life and accounted for 10% to 46% of the variance. Finally, in order to examine the independent effects of anxiety and depression, they were entered jointly in Model 3. Results indicate that both anxiety and depressive symptoms are significantly associated with poorer quality of life in all domains. Jointly, they accounted for 12% to 50% of the variance.
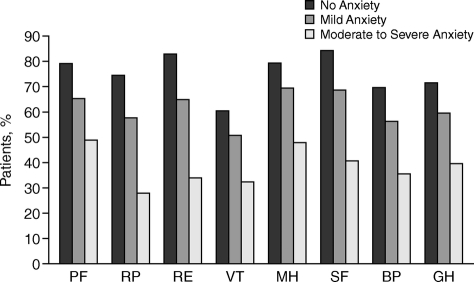
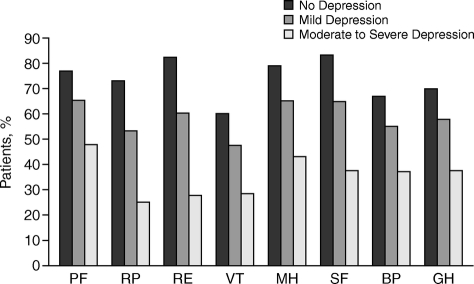
In order to examine the effects of anxiety and depressive symptom severity using established ranges for mild, moderate, and severe symptoms on quality of life, ANOVAs were conducted for each domain of quality of life after adjustment for demographics and health conditions. The findings are presented in Figures 1 and 2. For each domain of quality of life, mild symptoms of anxiety were associated with significantly greater impairment in quality of life than no anxiety symptoms, and moderate to severe anxiety symptoms were associated with greater impairment in quality of life than mild anxiety symptoms (all p values < .001). The findings were the same for depressive symptoms (all p values < .001).
Figure 1.
Relationship of Anxiety Symptom Severity and Quality of Life as Measured by SF-36 Subscales
Figure 2.
Relationship of Depressive Symptom Severity and Quality of Life as Measured by SF-36 Subscales
Finally, in order to compare the effects of anxiety and depressive symptoms on quality of life relative to other diseases, the findings of this study were compared with data from the Medical Outcomes Study (Ware et al.22) using t tests with Welch-Satterthwaite approximations of degrees of freedom. Because multiple tests were conducted, a p value of < .001 was considered significant. Relative to patients with diabetes and acute myocardial infarction, patients with moderate to severe anxiety or depressive symptoms reported significantly worse quality of life in every domain (all p values < .001). Relative to patients with congestive heart failure, patients with moderate to severe anxiety or depressive symptoms had significantly greater impairments in bodily pain, vitality, social functioning, role limitations due to emotional problems, and mental health functioning, and patients with depressive symptoms also had significantly more bodily pain (p < .001).
DISCUSSION
This study highlights the prevalence and impact of anxiety and depressive symptoms in the primary care setting. The prevalence of both anxiety and depressive symptoms in this sample was high, with almost 40% of the sample reporting anxiety symptoms and 30% reporting depressive symptoms. Furthermore, the impact of anxiety and depressive symptoms was pervasive across all domains of functioning: both anxiety and depressive symptoms were associated with poorer functioning in all domains of quality of life.
Hierarchical regression analyses were conducted to determine the effects of anxiety and depressive symptoms on 8 domains of functioning. Unadjusted analyses demonstrated that both anxiety and depressive symptoms were associated with poorer functioning in all domains. After controlling for demographic information and medical conditions, anxiety symptoms remained significantly associated with physical functioning, role limitations due to physical health problems, role limitations due to emotional health problems, social functioning, pain, vitality, emotional well-being, and general health perceptions, accounting for 10% to 35% of the variance in these domains. Similar findings were obtained for depressive symptoms, which accounted for 10% to 46% of the variance in functioning. Furthermore, individuals with moderate to severe anxiety reported similar levels of functioning across domains as individuals with moderate to severe depressive symptoms. These findings demonstrate that anxiety and depressive symptoms are associated with decreased functioning over and above that attributed to health problems.
Some have speculated that the association between anxiety and functioning is due to anxiety's high rates of comorbidity with depression.23 In the current study, this was tested by simultaneously entering both anxiety and depressive symptoms into the regression models. Although the simultaneous inclusion of anxiety and depressive symptoms into the models reduced the strength of the associations, both anxiety and depressive symptoms remained significantly associated with quality of life. Thus, anxiety and depression have a significant relationship with quality of life that is independent of the other. Furthermore, when analyzed simultaneously, anxiety and depressive symptoms have differential associations with domains of functioning. Depressive symptoms had a stronger association with role limitations due to physical and emotional problems, vitality, mental health, and social functioning than did anxiety symptoms. Conversely, anxiety symptoms had a stronger relationship with bodily pain than did depressive symptoms. One possible explanation is that there are different pathways through which anxiety and depressive symptoms affect quality of life.
The association between anxiety and depressive symptom severity and functioning was also examined. Individuals with mild levels of anxiety or depressive symptoms had worse functioning than individuals who reported no symptoms. Similarly, individuals with moderate to severe symptoms had worse functioning than individuals who reported mild levels of anxiety or depression. These findings demonstrate a clear incremental worsening of functioning with increasing severity of anxiety or depressive symptoms. This is consistent with deBeurs and colleagues,24 who found that anxiety symptoms were associated with poorer physical and social functioning, as well as with studies that have found that subsyndromal symptoms of depression are related to worse physical and emotional functioning.25,26
Normative data for the SF-36 are available for samples with significant health conditions, including congestive heart failure, diabetes, and recent myocardial infarct.22 When compared with patients with diabetes or an acute myocardial infarction, individuals with moderate to severe anxiety or depressive symptoms reported worse levels of functioning in all domains. When compared with patients with congestive heart failure, patients with moderate to severe anxiety or depressive symptoms reported worse bodily pain, vitality, social functioning, role limitations due to emotional problems, and mental health. Furthermore, patients with depressive symptoms also reported worse general health. The only area in which congestive heart failure patients reported worse functioning was in the physical functioning domain. Thus, participants with moderate to severe levels of anxiety or depressive symptoms exhibit greater decrements in functioning than patients with congestive heart failure, diabetes, and recent myocardial infarct.
These findings must be considered in light of the limitations of this study. First, anxiety and depressive symptoms rather than clinical disorders were assessed. In the primary care setting, however, rates of anxiety and depressive symptoms are higher than rates of clinical disorders,9 and, as demonstrated in this study, even mild symptoms of anxiety and depression impair quality of life. Another limitation of this study is its cross-sectional design, which precludes causal inferences.
This study provides additional support for the assessment and treatment of anxiety and depressive symptoms in the primary care setting. Prior research demonstrates that anxiety and depressive disorders are both underdetected and undertreated in the primary care setting.3,27–29
The results of the current study suggest that anxiety and depressive symptoms, even those at a mild level, are associated with declines in functioning after statistically controlling for differences in demographics and health-related conditions. Moreover, individuals with anxiety and depressive symptoms report greater impairment in functioning than people with congestive heart failure, diabetes, and myocardial infarct. Given these findings, more effective ways of assessing and treating anxiety and depressive symptoms in the primary care setting are necessary. Recent studies have demonstrated that a collaborative care model of treatment in which mental health treatment is integrated into the primary care setting can result in positive outcomes.30–33 Even when referrals to specialty mental health clinics are made and transportation is provided, patients are more likely to participate in treatment that is integrated into the primary care setting.34 Furthermore, recent studies have shown that depression is associated with nonadherence to treatment regimens.35,36 Thus, the integration of mental health services into the primary care setting may significantly enhance the number of people who are actively engaged in treatment for anxiety and depression as well as improve care for other medical problems.37
Footnotes
This work was supported by National Institute of Mental Health grant MH65281 to Dr. Brenes.
Dr. Brenes reports no financial or other affiliations that could be considered a conflict of interest relative to the subject of this article.
REFERENCES
- Kessler RC, Demler O, and Frank RG. et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005 352:2515–2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, and Demler O. et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 62:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Sherbourne CD, and Craske MG. et al. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. 2004 2230–2237. [DOI] [PubMed] [Google Scholar]
- Ansseau M, Dierick M, and Buntink F. et al. High prevalence of mental disorders in primary care. J Affect Disord. 2004 78:49–55. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- Wells KB, Stewart A, and Hays RD. et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA. 1989 262:914–919. [PubMed] [Google Scholar]
- Wells KB, Sherbourne CD. Functioning and utility of current health of patients with depression or chronic medical conditions in managed, primary care practices. Arch Gen Psychiatry. 1999;56:897–904. doi: 10.1001/archpsyc.56.10.897. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27:861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- Olfson M, Shea S, and Feder A. et al. Prevalence of anxiety, depression, and substance use disorders in an urban general medicine practice. Arch Fam Med. 2000 9:876–883. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, and Williamson J. et al. The influence of anxiety in the progression of disability. J Am Geriatr Soc. 2005 53:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes GA, Penninx BWJH, and Judd PH. et al. Anxiety, depression, and disability across the lifespan. Aging Ment Health. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenes GA, Kritchevsky S, and Mehta KM. et al. Scared to death: results from the Health, Aging, and Body Composition study. Am J Geriatr Psychiatry. 2007 15:262–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Jacobi F, and Cox BJ. et al. Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Arch Intern Med. 2006 166:2109–2116. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Wells KB, and Meredith LS. et al. Comorbid anxiety disorders and the functioning and well-being of chronically ill patients of general medical providers. Arch Gen Psychiatry. 1996 53:889–895. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, and Martire LM. et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001 9:113–135. [PubMed] [Google Scholar]
- Olfson M, Broadhead WE, and Weissman MM. et al. Subthreshold psychiatric symptoms in a primary care group practice. Arch Gen Psychiatry. 1996 53:880–886. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, and Brown G. et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 56:893–897. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Smith FA, and Blais MA. et al. Recognition and treatment of depression and anxiety in patients with acute myocardial infarction. Am J Cardiol. 2006 98:319–324. [DOI] [PubMed] [Google Scholar]
- Ferguson CJ, Stanley M, and Souchek J. et al. The utility of somatic symptoms as indicators of depression and anxiety in military veterans with chronic obstructive pulmonary disease. Depress Anxiety. 2006 23:42–49. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Arean PA. Psychometric evaluation of the Beck Anxiety Inventory with older medical patients. Psychol Assess. 1997;9:136–144. [Google Scholar]
- Beck AT, Rush AJ, and Shaw BF. et al. Cognitive therapy of depression. New York, NY: Guildford Press. 1979 [Google Scholar]
- Ware JE Jr, Kosinski M, and Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: Quality Metric Inc. 1993 [Google Scholar]
- Nisenson LG, Pepper CM, and Schwenk TL. et al. The nature and prevalence of anxiety disorders in primary care. Gen Hosp Psychiatry. 1998 20:21–28. [DOI] [PubMed] [Google Scholar]
- deBeurs E, Beekman ATF, and van Balkom AJLM. et al. Consequences of anxiety in older persons: its effect on disability, well-being and use of health services. Psychol Med. 1999 29:583–593. [DOI] [PubMed] [Google Scholar]
- Chopra MP, Zubritsky C, and Knott K. et al. Importance of subsyndromal symptoms of depression in elderly patients. Am J Geriatr Psychiatry. 2005 13:597–606. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Fisher LJ, and Dal Grande E. et al. Subsyndromal depression: prevalence, use of health services and quality of life in an Australian population. Soc Psychiatry Psychiatr Epidemiol. 2004 39:293–298. [DOI] [PubMed] [Google Scholar]
- Rost K, Zhang M, and Fortney J. et al. Persistently poor outcomes of undetected major depression in primary care. Gen Hosp Psychiatry. 1998 20:12–20. [DOI] [PubMed] [Google Scholar]
- Stanley MA, Roberts RE, and Bourland SL. et al. Anxiety disorders among older primary care patients. J Clin Geropsychol. 2001 7:105–116. [Google Scholar]
- Wells KB, Schoenbaum M, and Unutzer J. et al. Quality of care for primary care patients with depression in managed care. Arch Fam Med. 1999 8:529–536. [DOI] [PubMed] [Google Scholar]
- Craske MG, Roy-Byrne P, and Stein MB. et al. Treating panic disorder in primary care: a collaborative care intervention. Gen Hosp Psychiatry. 2002 24:148–155. [DOI] [PubMed] [Google Scholar]
- Levkoff SE, Chen H, and Herr ECM. et al. Design and sample characteristics of the PRISM-E multisite randomized trial to improve behavioral health care for the elderly. J Aging Health. 2004 16:3–27. [DOI] [PubMed] [Google Scholar]
- Rollman BL, Belnap BH, and Mazumdar S. et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Arch Gen Psychiatry. 2005 62:1332–1341. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Craske MG, and Stein MB. et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry. 2005 62:290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Coakley EH, and Zubritsky C. et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004 161:1455–1462. [DOI] [PubMed] [Google Scholar]
- Rieckmann N, Kronish IM, and Haas D. et al. Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am Heart J. 2006 152:922–927. [DOI] [PubMed] [Google Scholar]
- Smith A, Krishnan JA, and Bilderback A. et al. Depressive symptoms and adherence to asthma therapy after hospital discharge. Chest. 2006 130:1034–1038. [DOI] [PubMed] [Google Scholar]
- Dalessandro M, Conti CM, and Gambi F. et al. Antidepressant therapy can improve adherence to antiretroviral regimens among HIV-infected and depressed patients. J Clin Psychopharmacol. 2007 27:58–61. [DOI] [PubMed] [Google Scholar]