Abstract
Sudden, precipitous improvements in depressive symptom severity have been identified as occurring among unipolar depressed individuals. These “sudden gains” have been associated with superior acute treatment outcome in several treatment modalities, including cognitive therapy. A better understanding of sudden gains may provide insight into the mechanisms of action in these and other psychotherapies. One efficacious therapy that has been overlooked in sudden gains research is interpersonal psychotherapy (IPT; Weissman et al. 2000). The present research examined the rates and concomitant features of sudden, precipitous improvements in depressive symptomotology among 185 women receiving IPT for recurrent depression. Sudden gains, defined using extant criteria for the Beck Depression Inventory, were assessed over 12 weeks of acute IPT treatment for depression and occurred for 33.5% of the sample. Sudden gains were not associated with diagnostic and demographic characteristics or with differential likelihood of achieving depression remission with IPT monotherapy during active treatment. Further, those with sudden gains were no more likely to maintain their recovery through maintenance treatment. The lack of impact of sudden gains on eventual outcome is discussed in terms of potentially disparate emphases and mechanisms of change between IPT and CBT.
Keywords: Sudden Gains, Depression, Interpersonal Psychotherapy
1. Introduction
Since 1999, researchers have become increasingly interested in the frequency, correlates, and clinical implications of sudden, precipitous improvements in unipolar depressive symptomotology. Researchers and clinicians alike have observed that depressive symptom reduction in psychotherapy is not always a gradual process (Tang & DeRubeis 1999a). Some individuals make substantial improvements in their level of depressive symptomotology over relatively short intervals during acute treatment. To date, these “sudden gains” have been identified as occurring during the active phase of treatment in a variety of psychotherapies for depression, including cognitive therapy (Tang & DeRubeis, 1999b; Tang et al 2005), brief psychodynamic therapy (Tang, Luborsky & Andrusnya 2002; Andrusnya, Luborsky, Pham & Tang, 2006), and group psychoeducational treatment (Kelly, Roberts & Ciesla, 2005). Sudden gains also occur in mental health clinic “treatment as usual” (Stiles et al., 2003), among placebo control groups (Vittengl et al., 2005) and among non-treated samples (Kelly, Roberts & Bottonari, 2007). Further, there is some evidence that individuals who experience sudden gains have better acute treatment outcomes and do better in long-term follow-up than those whose symptom improvement is more gradual (Tang & DeRubeis, 1999b; Tang, Luborsky & Andrusnya 2002; Tang, DeRubeis, Hollon, Amsterdam & Shelton, 2007; see also Grilo, Masheb, & Wilson, 2006, for related results in binge-eating disorder).
There has also been interest in determining predictors and precipitants of sudden gains. Understanding factors associated with precipitous improvements in depressive symptomotology has the potential to provide insight into the mechanisms of action of differing psychotherapies, and may suggest areas for increased therapeutic focus. This, in turn, could influence clinical practice as well as improving our understanding of the process of recovering from depression. Unfortunately, relatively little work has gone into determining precipitants of sudden gains, and some of this evidence has been mixed. Tang and DeRubeis (1999b), drawing from the theoretical underpinnings of cognitive therapy (CT), found evidence that sudden gains occurring during CT were related to pre-gain improvements in depressotypic cognitive style (Tang & DeRubeis, 1999b; Tang et al., 2005). However, others have had difficulty replicating this finding using alternate assessment methods in a CBT- oriented intervention (Kelly, Roberts & Ciesla, 2005). Further, as previously stated, sudden gains have been found to occur across several treatment modalities (Tang & DeRubeis, 1999b; Tang et al., 2002, 2005; Stiles et al., 2005; Andrusyna et al., 2006) and among samples who are not receiving active treatment (Kelly et al., 2007; Vittengl et al. 2003). This suggests that the precipitants and meaning of sudden gains in the remediation of depressive symptoms have yet to be fully understood.
The occurrence and impact of sudden gains in interpersonal psychotherapy (IPT) for depression has not been explored to date. IPT has been shown to be an efficacious treatment for depression in numerous clinical trials (DiMascio et al., 1979; Weissman et al. 1979; Elkin et al., 1989; Mufson, Weissman, Moreau et al., 1999; Mufson, Dorta, Wickramaratne, et al., 2004). In contrast to CT, which focuses on the internal thought processes of the patient, IPT focuses on improving interpersonal difficulties that are thought to exacerbate or trigger depressive symptoms. IPT seeks to identify and link interpersonal stressors or conflicts to mood symptoms and to improve interpersonal functioning to reduce depressive symptoms. Thus, the presumed mechanism of action in IPT differs from that of CBT. Examining the relative rates of sudden gains in IPT, as well as their clinical impact, may provide insight into differential therapeutic mechanisms at work in IPT and CBT.
The present paper seeks to examine the rates, correlates and clinical impact of sudden gains in IPT for depression. Because sudden gains have been identified across treatment modalities, we predicted that sudden gains would occur at a similar rate in IPT as in other treatments, or approximately 40%. Further, based on previous work in other psychotherapies, we expected that individuals who experienced sudden gains would recover more quickly and more completely compared to individuals who do not have sudden gains during acute treatment. We also explored demographic, diagnostic and other characteristics that may be associated with the occurrence of sudden gains in IPT for depression.
2. Method
2.1. Participants
The study sample consisted of 185 women with recurrent unipolar depression who participated in the acute treatment phase of an outpatient treatment study designed to evaluate the efficacy of maintenance IPT for relapse prevention (Frank et al., 2000). To be included in the study, individuals a) were in a recurrent episode of Major Depressive Disorder as determined by diagnostic interview; b) had a previous episode of depression within 130 weeks; c) had at least a 10 week period of remission between the previous and index episodes; d) were between 20 and 60 years of age; and e) scored a 15 or greater on the 17-item version of the Hamilton Rating Scale for Depression (HRSD-17; Hamilton, 1960). Women who met criteria for bipolar or psychotic spectrum disorders were excluded, as were individuals meeting full criteria for antisocial or borderline personality. Individuals with a recent history (past two years) of substance dependence were excluded as were those with serious or unstable medical illness or whose depressive symptoms were secondary to medications. Participants had to be anti-depressant free for two weeks prior to starting treatment, and those whose symptomotology required inpatient treatment were withdrawn from the study.
The goal of the acute phase of the study was to treat participants to remission with 12–24 weekly individual sessions of IPT as part of a study investigating various session frequencies of IPT as maintenance therapy for recurrent depression. Patients scoring 7 or lower on the HRSD-17 for three consecutive weeks during acute treatment were classified as remitters as soon as they met that criterion. Individuals who did not have an adequate response to IPT treatment by week 8 (with response defined as a 50% reduction in HRSD-17 score) or for whom medication was clinically indicated were offered adjunctive medication treatment. Because the primary goal of the current report was to examine sudden gains associated with IPT, patients who required adjunctive medication treatment were censored at the time of medication initiation to eliminate the possibility of including a “sudden gain” that may be attributable to the placebo effect or to the clinical efficacy associated with medication1.
Individuals in the parent trial were kept on a schedule of weekly acute IPT for 12 to 24 weeks. Patients who met remission criteria (as defined above) prior to 12 weeks were kept in weekly sessions until 12 weeks. Patients displaying depression remission at or before 12 weeks went into continuation and then maintenance treatment following week 12. In contrast, those unable to achieve depression remission received weekly acute treatment for up to 24 weeks. Individuals who met remission criteria after 12–24 sessions of IPT were placed in a continuation arm of the study, and were subsequently randomized to receive weekly, bi-weekly or monthly maintenance IPT sessions for up to 2 years. For complete details on the sample and methods, see Frank et al., 2000.
For the purpose of the present analyses, we focused attention on sudden gains occurring in the first 12 weeks of acute treatment. This allowed us to maintain a standard inter-session interval across patients regardless of remission status. Because we were interested in the impact of sudden gains on treatment outcome, participants who did not attend at least 6 sessions (i.e., did not receive a sufficient dose of psychotherapy) were excluded from the present sample. Participants were monitored for relapse using the HRSD and time (in weeks) to relapse or withdrawal from the study was recorded. In total, 92 of the original sample of 185 (approximately 50%) remitted with IPT alone and entered maintenance IPT treatment.
2.2. Statistical Methods
2.2.1. Sudden Gains Criteria
Tang and colleagues originally defined a sudden gain as a change in BDI scores between sessions that met three criteria: a) a reduction (gain) of at least 7 points, b) the gain is at least 25% of the previous score, and c) the average BDI scores for the three preceding and three following weeks differed in terms of an independent sample t-test. The intent of these criteria was that the gain be objectively large, be large relative to recent scores, and that it be large relative to individual symptom fluctuations.
Since the initial description of sudden gains, several authors have adjusted the criteria in multiple ways. Tang and colleagues (2005) suggested that criterion c could be examined by comparing the mean differences between the three preceding and three following assessments. Per Tang and colleagues, if that difference is at least 2.78 times the pooled standard deviation, then criterion c was satisfied. Similarly, Hardy et al (2005) used a change in BDI of at least 8 points and required that the t-test comparing the three preceding and three following assessments be greater than or equal to 2.50 when defining sudden gains. Kelly and colleagues (Kelly, Roberts & Ciesla, 2005) also modified the third criterion by first calculating each individual’s standard deviation across the assessments and then comparing that number to the intersession change in BDI scores. If a drop in BDI score was at least 1.5 times the individual’s standard deviation, it was considered to have met criterion c.
This modified criterion has several advantages over Tang and colleagues’ original third criterion. First, using standard deviation accounts for the non-independence of the three preceding and three following sessions (and hence violation of the assumption of independence required for the t-test). Second, it allows researchers to include sudden gains that occur very early or very late in treatment (i.e.: within three sessions of initiating of terminating treatment). This is potentially critical as there is good evidence that sudden gains occurring very early in treatment have a stronger relationship to treatment outcomes than those occurring later in treatment (Illardi & Craighead, 1994; Kelly et al, 2005; Grilo et al., 2006). Lastly, using each individual’s standard deviation accounts for that individual’s typical fluctuation in depressive symptomotology, and thus adheres to the intent of Tang’s third criterion. Research has indicated that the use of this third criterion yields rates of sudden gains that are similar to those obtained in previous work (see Kelly et al., 2005; Kelly et al. 2007).
For the present study, symptom improvement on the BDI was considered to be a sudden gain if it a) was at least 7 points, b) was at least a 25% decrease from the previous score, and c) the difference score was at least 1.5 times larger than the individual’s standard deviation across all assessments. Weekly assessments that occurred less than 4 days or more than 10 days apart were excluded from consideration for sudden gains to reduce potential overlap in symptom reporting over brief time intervals and to legitimately identify “sudden” gains. If a BDI assessment was missing, that interval was excluded from consideration for sudden gains. Due to the unknown pattern of change over a missing assessment, missing data were not extrapolated or considered as part of a contiguous time-line in the present analyses.
2.2.2. Remission Criteria
For the present analyses, remission from depression was considered to have occurred if a patient recorded a HRSD-17 score of ≤ 7 during three consecutive weeks of treatment regardless of how early this occurred in treatment. Time to remission was calculated based on the first of three weeks which satisfied the remission criteria. This method ensured that symptom improvement was relatively stable over time before determining that remission had occurred and reduces the chance that someone is included in or excluded from the remission group simply because of a good or bad week at the end of treatment2.
2.2.3. Analyses
Participants with sudden gains were compared to those without sudden gains in terms of initial demographic and clinical characteristics. Further, differences in depressive severity at visit 12 (with the last score carried forward as needed due to termination or medication initiation), remission rates, and time to treatment remission were examined. Independent sample t-tests and chi-square analyses were used to test for significant differences between sudden gainers and other participants on the variables of interest. In addition, two Kaplan-Meyer survival analyses were conducted, one to examine differential time to remission between sudden gainers and non-sudden gainers and one to determine if those with sudden gains had a differential time to recurrence during the maintenance phase of treatment compared to those without sudden gains.
2.3. Measures
2.3.1. Demographic characteristics
Demographic information collected from participants included age, ethnicity, marital status and employment status.
2.3.2. Diagnostic Assessment
Diagnostic interviews were conducted to determine current depressive status and to collect information regarding clinical features (e.g., number of previous episodes, duration of index episode). The first 39 participants included in this sample were diagnosed using the Schedule for Affective Disorders (SADS; Endicott & Spitzer, 1978) while the remaining patients were diagnosed using the Structured Clinical Interview for DSM-IV diagnosis (SCID-I; First, Spitzer, Gibbon & Williams, 1995).
2.3.3. Depressive Symptoms
Depressive symptom severity was assessed with both the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) and the Beck Depression Inventory (BDI; Beck & Steer, 1988). The HRSD is a 17-item, rater administered measure of depressive symptoms that is widely used in clinical trials. Trained independent evaluators conducted HRSD interviews. The HRSD served as the primary outcome measure for the parent study, was used to determine participant eligibility for the study, and was repeated at each visit. The BDI is a self-report assessment of depressive symptomotology with well-established psychometric properties and has been widely used in depression research. In keeping with previous work, BDI scores were used to determine the presence or absence of sudden gains.
3. Results
The average participant was 37.7 (sd=9.93) years old and had 15.0 years of education (sd=1.93). Nearly 40% of participants were married (n=73), 61 participants (33.0%) were never married, 45 (24.3%) were separated or divorced and 6 (3.2%) were widowed. Over half of the participants were employed full-time (53%) or part-time (21.1%); 11.4% identified themselves as homemakers, 3.8% were students, and the remainder was unemployed, laid off or on a leave of absence (10.7%). The majority of participants (87.6%) were Caucasian (8.6% African American, 3.8% Hispanic or of other ethnicity).
Participants were moderately depressed at the time of study entry on both the BDI (mean=25.8, sd = 6.69) and the HRSD-17 (mean = 18.3, sd = 2.85). The average age of onset of major depression was 24.6 years of age (sd=8.99, range: 7–51 years) and the average number of previous episodes was 4.94 (sd=3.94; mode=3; number of previous episodes was truncated at 9 to decrease skew). Seventy-three participants (39.5%) met criteria for melancholic depression and 21 (11.4%) met criteria for atypical depression. Forty-one (22.2%) had one or more comorbid Axis I diagnoses. Nineteen of these individuals (46.3%) had a comorbid anxiety disorder and 11 (26.8%) were diagnosed with concurrent dysthymia (double depression). Of the study sample, 104 (56.2%) achieved depression remission with IPT monotherapy, 12 (6.5%) terminated prior to remission, and 69 (37.3%) required initiation of adjunctive medication treatment (mean number of sessions prior to medication initiation = 11.1, sd = 3.8).
Based on our criteria for sudden gains, 66 sudden gains occurred to 62 participants (33.5%) within the first 12 sessions of IPT. The magnitude of the average sudden gain was 13.0 BDI points (sd=5.3). Approximately half of the sudden gains (53.0%) were reversed (giving up half of the gain subsequently) making 33 sudden gainers “reversers.” One sudden gain was maintained for 2 of the 4 participants who had multiple sudden gains.
3.1. Characteristics of sudden gainers
Those who experienced sudden gains during treatment did not differ from other participants in terms of demographic characteristics such as age, ethnicity, marital and employment status (all p’s >.32). Similarly, sudden gainers and non-sudden gainers did not differ in terms of diagnostic characteristics, such as age of onset of depression, duration of index episode, and number of previous episodes (all p’s >.08). Sudden gainers and non-sudden gainers had similar initial BDI scores at baseline (p>.71) and did not differ in terms of either rates of comorbidity overall, χ2 (1, N=185) = 0.35, p=.64 (17.7% among sudden gainers, 24.4% among non-sudden gainers), or of comorbid anxiety disorders, χ2 (1, N=185) = 0.04, p=1.0 (9.7% of sudden gainers, 10.6% of non-sudden gainers). Similarly, sudden gainers and non-sudden gainers did not differ in terms of presence or absence of melancholic depression, χ2 (1, N=184) = 2.97, p=.11 (48.4% among sudden gainers, 35.2% among non-sudden gainers), nor in terms of atypical depression, χ2 (1, N=145) = .07, p=1.00 (13.3% among sudden gainers, 15.0% among non-sudden gainers).
In terms of treatment response, sudden gainers did not remit from depression at a higher rate when compared to participants who did not have a sudden gain, χ2 (1, N=185) = 1.27, p=.27. Thirty four of 62 sudden gainers (54.8%) were categorized as achieving remission by the end of active treatment compared to 78 of 123 non-sudden gainers (63.4%) who remitted with psychotherapy alone3. Similarly, those who experienced sudden gains did not differ significantly from non-sudden gainers in terms of depressive symptomotology (17-item HRSD scores) at the 12th visit with the last score carried forward for subjects whose data were missing or censored prior to visit 12 (because of early termination or initiation of adjective medication), t(183)= .19, p=.85, n.s.
To examine the time required by sudden gainers and non-sudden gainers to achieve remission, a Kaplan-Meier survival analysis was conducted, with the HRSD as the index of remission. Individuals who experienced a sudden gain did not remit more quickly than those who did not experience a sudden gain, χ2 (1, N=185) = 0.48, p<.49. Median time to remission was estimated at 13.0 weeks for non sudden gainers (95% CI: 10.8–15.2), and 14.8 weeks for sudden gainers (95% CI: 10.7–19.0)4. Survival curves are presented in Figure 1.
Figure 1.
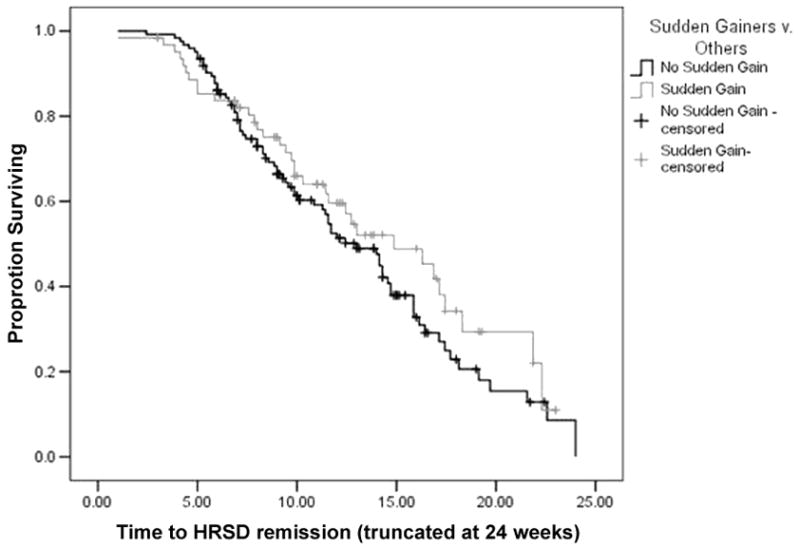
Weeks to HRSD remission.
Lastly, because sudden gains may impact longer-term treatment outcome, survival analyses were conducted on the sub-sample of participants (n=92) who entered the maintenance phase of treatment after achieving remission from depression with IPT alone. The presence of a sudden gain was not associated with time to relapse, χ2 (1, N=92) = 1.09, p<.30. Mean survival time was estimated at 89.9 weeks for non sudden gainers (95% CI: 83.4–96.4), and 83.5 weeks for sudden gainers (95% CI: 71.9–95.2). Survival curves are presented in Figure 25.
Figure 2.
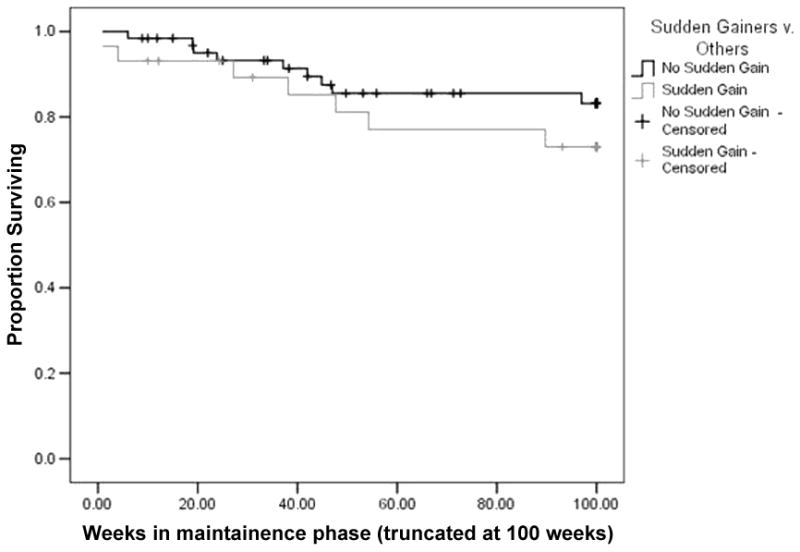
Weeks to recurrence in maintenance.
4. Discussion
The present analyses sought to examine the rate of sudden gains in IPT for depression. In addition, we sought to identify demographic and diagnostic characteristics that may be associated with sudden gains in IPT, and examined the influence of interpersonal functioning on the occurrence of sudden gains. In accordance with our hypothesis, sudden gains did occur in IPT and occurred at a rate that is consistent with rates reported in other studies. In the present study, sudden gains occurred to 33.5% of the sample. This figure is relatively consistent with data from previous work. Most other sudden gains studies show rates of sudden gains in the high 30% to low 40% range. This work adds to the growing evidence that sudden gains are a robust finding across interventions. It further reinforces the consistent finding that approximately 40% of a given depressed population experiences a sudden and precipitous improvement in symptomotology over time.
Contrary to our hypotheses we found no differences between sudden gainers and other participants in terms of baseline demographic or diagnostic characteristics. Previous work in the sudden gains area (Hardy et al., 2005; Kelly et al., 2005; see also Grilo, Masheb & Wilson, 2006, for similar null findings in CBT for binge eating) has shown inconsistent associations between demographic characteristics and sudden gains such that a clear pattern of association between baseline characteristics and sudden gains has yet to be identified. Further, sudden gainers were no more likely to achieve sustained remission from depression with IPT alone compared to those who did not experience a sudden gain.
Using a measure to determine clinical outcome that is different from the one used to determine sudden gains (i.e.: clinician-rated HRSD versus self-reported BDI) carries the benefit of reducing a potential tautology that occurs when the same measure is used to assess both sudden gains and treatment outcome. Having a sudden gain implies that the participant has enjoyed a substantial improvement in symptomotology at some point during treatment on a given measure. While having a sudden gain is neither necessary nor sufficient to cause remission, if the same measure is used to determine both sudden gains and treatment response, those with sudden gains are, by definition, more likely to remit. Thus our use of two separate measures, the HRSD-17 for outcome and the BDI to define sudden gains, represents a more conservative approach than what has been done in previous research. Nevertheless, we note that a similar pattern of findings emerged when BDI scores were used to predict outcome (see footnotes 2–4).
Contrary to hypotheses, those who had sudden gains on the BDI did not achieve remission from depression as defined by HRSD any faster than those who did not have sudden gains. Although researchers in adult depression have not generally conducted survival analyses to examine the relationship between sudden gains and time to remission, Gaynor et al. (2003) found that adolescents experiencing sudden gains remitted with psychotherapy twice as quickly as those who did not have a sudden gain (5 sessions v. 9.5 sessions). Similarly, while Tang et al. (2000) found that individuals with sudden gains during acute CBT treatment faired better in long-term follow-up, in the present data, patients who had a sudden gain during the course of acute IPT treatment had no apparent advantage during long-term maintenance. It should be noted, however, that relatively few individuals relapsed over the 2 years of maintenance therapy.
Potential explanations for the apparent lack of importance of sudden gains in IPT may be drawn from the differing theoretical rationales and putative mechanisms of IPT and CBT. In theory, CBT works to reduce depressive symptoms by teaching patients the skills required to restructure their thinking patterns so that the world can be viewed in a less pessimistic light. For some CBT patients, acquiring and applying skills in cognitive restructuring and/or making a cognitive shift may be a relatively rapid occurrence, leading to a sudden gain and potentially improving ultimate outcome. In contrast, IPT focuses on changing patterns of interpersonal function, which is likely to be a more gradual and iterative process and less under individual control than cognition. Thus, sudden gains in IPT may reflect a temporary improvement in interpersonal relationships and mood, and have less impact on eventual outcome. Alternately, those who experience sudden gains in IPT may be those whose mood is more reactive to interpersonal interactions, for better or worse. In either case, the experience of a sudden gain in IPT compared to CBT may be prompted by differing causes and may hold quite different clinical implications.
It is especially interesting to note that in previous work, Tang and colleagues (Tang, Luborsky & Andrusyna, 2002) found that sudden gains occurring during the course of supportive-expressive (SE) therapy, a derivative of psychodynamic therapy that is arguably closer in nature to IPT than is CBT, were less robust and did not predict longer term outcomes as did CBT related sudden gains. These authors suggest that SE therapy-related sudden gains are less robust due to the relative complexity of SE compared to CBT. Similarly, IPT operates by processing emotion and making adjustments to interpersonal interactions rather than using step-by-step methods to adapt cognitions as CBT does. Thus IPT is arguably more complex than CBT and sudden gains occurring in IPT may be more subject to reversal (due to either complexity or interpersonal setbacks) and have limited relationship to ultimate outcomes.
In addition, differential demand characteristics may be at work in these two therapies. In CBT, patients are praised for their ability to minimize negative affect, in both severity and duration, through the skillful use of cognitive restructuring. In IPT, patients are asked to discuss and process affective experiences as they relate to interpersonal interactions more deeply than is done in typical CBT. Thus, while CBT may prompt patients to downplay mood by focusing on cognitions surrounding affective changes, IPT emphasizes mood fluctuations, particularly those that occur in relation to interpersonal stressors. This differing set of therapeutic expectations may promote different patterns of symptom identification and reporting between the two interventions.
To our knowledge, this work represents the first examination of the sudden gains phenomenon in IPT. Further, it is among a minority of studies that examines sudden gains in terms of time to remission. Given that sudden gains and the characteristics associated with them are potentially useful for exploring mechanisms of depression (Tang et al. 1999b), it is arguably important to consider not only ultimate outcome but also treatment course.
There are, however, several limitations to the current research. First, the sample consisted exclusively of female participants with recurrent depression, limiting generalizability. Patterns and correlates of sudden gains may be different in male or mixed samples and sudden gains may have a differential impact on those with chronic depression or who are in their first episode of depression. Second, although the criteria used to define sudden gains in this study were the same as have been used in previous work (Kelly, Roberts & Ciesla, 2005; Kelly, Roberts & Bottonari, 2007), they do differ from Tang and DeRubeis’s (1999) original criteria. The criteria used here may be slightly more liberal (although rates of sudden gains are similar regardless of criteria) and may be more prone to reversal. Nevertheless, we note that follow-up analyses using the original Tang and DeRubeis’ (1999) criteria produced a similar set of study results (see Footnote 5). Last, given that the goal of the parent study was to assess IPT as a maintenance therapy for recurrent depression, medication was made an option to participants who either did not have a 50% reduction in HRSD-17 scores by week 8 with IPT alone or whose symptom profile and symptom severity warranted adjunctive medication. Although individuals were removed from the present sample at the point at which adjunctive antidepressant medication was prescribed, the sample considered here may be representative only of individuals who performed relatively well in IPT monotherapy. Future work examining the impact of sudden gains among patients treated exclusively with IPT over a longer period of time would add to our understanding of the impact of sudden gains on non-cognitive psychotherapies.
In conclusion, the present work indicates that sudden gains do occur in IPT for depression at rates similar to those found in other studies. No clear demographic or diagnostic characteristics were found to be associated with the occurrence of sudden gains. Adding to the mixed results often found in this area of research, IPT-related sudden gains do not appear to provide an advantage to sudden gainers in terms of depressive symptom severity following acute treatment or in time to remission. Sudden gains also did not provide an advantage in terms of durability of remission over time. This suggests potential mechanistic differences between IPT and CBT oriented interventions. Future work examining the pattern and impact of sudden gains in diverse psychotherapies appears to be warranted.
Acknowledgments
This work was supported by Grants MH-049115-08 and MH-16804-25. The authors would like to thank the researchers and staff who conducted the original study from which the present data are drawn, as well as the women who volunteered to participate.
Footnotes
One participant whose clinical progress suggested the addition of medication was maintained on IPT alone due to pregnancy.
Because of potential difficulties associated with using the HRSD to determine remission status but BDI scores to determine sudden gains, remission status was determined using the BDI as well. Again, individuals who scored in the non-depressed range (in this case, scores of 10 or lower) for three consecutive sessions were considered to have met remission criteria on the BDI. Time to BDI remission was calculated based on the first of three low scores.
Similarly, when the BDI was used to determine remission status, those without sudden gains were statistically similar, χ2 (1, N=185) = 0.00, p=1.00. Twenty five sudden gainers achieved BDI remission (40.3%) as did 50 non-sudden gainers (40.7%). Sudden gainers and non-sudden gainers did not differ in terms of BDI scores after 12 sessions of IPT, t(183)=.39, p=.70 (with last score carried forward for those who terminated early or had missing data at session 12).
A second survival analysis was conducted using time to BDI related remission. Again no differences were found between sudden gainers and non-sudden gainers in terms of time to remission, χ2 (1, N=185) = 0.26, p<.61. Mean time to BDI-defined remission was estimated at 16.1 weeks for non sudden gainers (95% CI: 14.5–17.4), and 16.1 weeks for sudden gainers (95% CI: 14.0–18.1).
Because of our use of an alternate third sudden gain criterion may have impacted our results, we recalculated sudden gains using Tang and DeRubeis’ original method and re-analyzed our data. Although this did result in fewer sudden gainers (50 v. 62 with 17 reversers) than our adjusted criteria, results when using Tang’s original criterion were unchanged. Sudden gainers and non-sudden gainers were not differentiable in terms of age, ethnicity, marital status, or employment status (all p’s >.30), nor did they differ in terms of any diagnostic characteristics (all p’s >.38), baseline depressive symptom severity, t(177)=.37, p=.71, remission rate, χ2(1, 185)=.93, p=.41, or HRSD-17 score at visit 12, t(183)=.19, p=.85. Further those with sudden gains calculated using Tang’s third criterion enjoyed no differential benefit in terms of time to remission, χ2(1, 185)=1.01, p=.31, or time to relapse, χ2(1, 92)=.68, p=.41, when survival analyses were conducted. Based on these results, it seems unlikely that the difference in sudden gain criteria is responsible for our findings.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Citations
- Andrusyna TP, Luborsky L, Pham T, Tang T. The mechanisms of sudden gains in Supportive-Expressive therapy for depression. Psychotherapy Research. 2006;16(5):526–536. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- DiMascio A, Klerman GL, Weissman MM, Prosoff BA, Neu C, Moore P. A control group for psychotherapy research in acute depression: One solution to ethical and methodological issues. Journal of Psychiatric Research. 1979;15:189–197. doi: 10.1016/0022-3956(79)90012-8. [DOI] [PubMed] [Google Scholar]
- Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, et al. National Institutes of Mental Health Treatment of Depression Collaborative Research Program: General effectiveness of treatments. Archives of General Psychiatry. 1989;46(11):971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: The Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Edition (SCID, Version 2.0) New York: Biometrics Research Department; 1995. [Google Scholar]
- Frank E, Grochocinski VJ, Spanier CA, Buysse DJ, Cherry CR, Houck PR, et al. Interpersonal psychotherapy and antidepressant medication: evaluation of a sequential treatment strategy in women with recurrent major depression. Journal of Clinical Psychiatry. 2000;61(1):51–57. [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurological and Neurosurgical Psychtiary. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy GE, Cahill J, Stiles WB, Ispan C, Macaskill N, Barkham M. Sudden gains in cognitive therapy for depression: A replication and extension. Journal of Consulting and Clinical Psychology. 2005;73(1):59–67. doi: 10.1037/0022-006X.73.1.59. [DOI] [PubMed] [Google Scholar]
- Gaynor ST, Weersling VR, Kolko DJ, et al. The prevalence and impact of large sudden improvements during adolescent therapy for depression: A comparison across cognitive-behavioral, family and supportive therapy. Journal of Consulting and Clinical Psychology. 2003;72(2):386–393. doi: 10.1037/0022-006x.71.2.386. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Rapid response to treatment for binge eating disorder. Journal of Consulting and Clinical Psychology. 2006;74(3):602–613. doi: 10.1037/0022-006X.74.3.602. [DOI] [PubMed] [Google Scholar]
- Kelly MAR, Roberts JE, Bottonari KA. Non-treatment related sudden gains in depression: The role of self-evaluation. Behaviour Research and Therapy. 2007;45:737–747. doi: 10.1016/j.brat.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Kelly MAR, Roberts JE, Ciesla JA. Sudden gains in cognitive behavioral treatment for depression: When do they occur and do they matter? Behavior Research and Therapy. 2005;43(6):703–714. doi: 10.1016/j.brat.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, et al. A randomized effectiveness trial of Interpersonal Psychotherapy for depressed adolescents. Archives of General Psychiatry. 2004;61(6):577–584. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of Interpersonal Psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56(6):573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- Stiles WB, Leach C, Barkham M, et al. Early sudden gains in psychotherapy under routine clinical conditions: Practice based evidence. Journal of Consulting and Clinical Psychology. 2003;71(1):14–21. [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Reconsidering rapid early response in cognitive behavioral therapy for depression. Clinical Psychology: Science and Practice. 1999a;6(3):283–284. [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999b;67(6):894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73(1):168–172. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R. Sudden gains in cognitive therapy of depression and depression relapse/recurrence. Journal of Consulting and Clinical Psychology. 2007;75(3):404–408. doi: 10.1037/0022-006X.75.3.404. [DOI] [PubMed] [Google Scholar]
- Tang TZ, Luborsky L, Andrusyna T. Sudden gains in recovering form depression: Are they also found in psychotherapies other than cognitive-behavioral therapy? Journal of Consulting and Clinical Psychology. 2002;70(2):444–447. [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Validity of sudden gains in acute phase treatment of depression. Journal of Consulting and Clinical Psychology. 2005;73(1):173–182. doi: 10.1037/0022-006X.73.1.173. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- Weissman MM, Prusoff BA, DiMascio A, Neu C, Goklaney M, Klerman GL. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. American Journal of Psychiatry. 1979;136(4B):555–558. [PubMed] [Google Scholar]


