Abstract
Context: To determine if testing environment affects Balance Error Scoring System (BESS) scores in healthy collegiate baseball players.
Design: Experimental, randomized, repeated-measures design with a sample of convenience.
Setting: Uncontrolled sideline and controlled locker room baseball environments.
Patients or Other Participants: A total of 21 healthy collegiate baseball players (age = 20.1 ± 1.4 years, height = 185.1 ± 6.8 cm, mass = 86.3 ± 9.5 kg) with no history of head injury within the last 12 months, no lower extremity injuries reported within the past 2 months that caused them to miss 1 or more days of practice or game time, and no history of otitis media, Parkinson disease, or Meniere disease.
Main Outcome Measure(s): Participants performed the BESS test in 2 environments, controlled locker room and uncontrolled sideline, in 2 testing sessions 1 week apart during the baseball preseason. The BESS scores were evaluated for each of the 6 conditions and total score across the testing sessions. Separate, paired-samples t tests with Bonferroni adjustment (P < .008) were used to examine differences between testing environments for each BESS subcategory and total score. Cohen d tests were calculated to evaluate effect sizes and relative change.
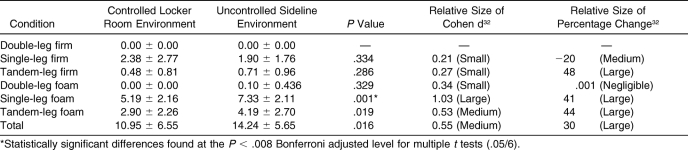
Results: Significant group mean differences were found between testing environments for single-leg foam stance (P = .001), with higher scores reported for the uncontrolled sideline environment (7.33 ± 2.11 errors) compared with the controlled clinical environment (5.19 ± 2.16 errors). Medium to large effect sizes (0.53 to 1.03) were also found for single-leg foam, tandem foam, and total BESS scores, with relative increases (worse scores) of 30% to 44% in the sideline environment compared with the clinical environment.
Conclusions: The BESS performance was impaired when participants were tested in a sideline environment compared with a clinical environment. Baseline testing for postural control using the BESS should be conducted in the setting or environment in which testing after injury will most likely be conducted.
Keywords: concussion, attention, environment, postural control
Key Points
Performance on the Balance Error Scoring System was impaired when healthy participants were tested on the sideline versus in the clinical environment.
Baseline testing for postural control using the Balance Error Scoring System should be conducted in the setting or environment in which postinjury testing will most likely take place.
Sport-related concussions can produce catastrophic or debilitative injuries if proper initial management is not provided.1–3 Individuals suspected of sustaining a sport-related concussion require a sound, evidence-based plan for proper immediate assessment and objective criteria for an informed return-to-play decision.4 Proactive approaches to the prevention of adverse consequences in managing mild head injuries have led to the formation of various preseason baseline protocols to develop objective criteria for the difficult clinical return-to-play decision process. The examination of baseline information relative to neuropsychological testing,5–10 symptoms,11–13 and postural control14–17 has been proposed to improve the sports medicine clinician's ability to make objective return-to-play decisions during both sideline and follow-up assessments.
Objective sideline assessment of mild head injury (MHI) includes the use of symptom checklists,12,13 cognitive tests,10 and postural control tests.18 Various methods of postural stability analyses have been proposed for assessing mild head injury, yet few of these tests can be used for immediate sideline assessment of MHI. The Balance Error Scoring System (BESS) was developed as a standardized, objective assessment tool for the clinical sideline assessment of postural control.18 The BESS uses 3 stances (double, single, and tandem), on both firm and foam surfaces, and was found to have an intratester reliability coefficient ranging from .78 to .96.15,17,19 The primary objective of the BESS is to provide clinicians with an immediate measure of postural control when assessing a patient with a potential MHI during a sideline clinical evaluation.
Concern about the applicability of standardized tests conducted in a controlled clinical environment as compared with an uncontrolled sideline environment has been previously reported in the literature.20 The effects of environment have been evaluated on 5 cognitive tests in both sideline and clinical evaluations in healthy collegiate lacrosse players, showing that a controlled clinical environment had minimal effect compared with an uncontrolled sideline environment.20 It was theorized that the healthy individuals could selectively screen distracting stimuli and perform cognitive tests similarly in both clinical and sideline environments. The question arises as to whether the effect of a sideline environment during a postural control assessment influences baseline scores.
Attention plays an integral role in postural control.21 Researchers22–24 using dual-task testing paradigms have reported detrimental effects with increased attentional demands when evaluating postural control. Although many investigators22–28 have studied the relationship between attention and balance, minimal research has been performed to determine if environment and external factors affect postural stability scores in collegiate athletes. The 2004 National Athletic Trainers' Association position statement on management of sport-related concussion stated, “… baseline postural-stability testing should be considered.”4 Thus, collecting valid and reliable objective BESS scores is important when comparing baseline scores with sideline scores during on-field MHI evaluations.
Our purpose was to determine if balance performance on BESS testing in an on-field, uncontrolled baseball environment differed compared with BESS testing in a controlled, locker room environment during preseason baseline testing of healthy collegiate baseball players. We hypothesized that the open, uncontrolled baseball field environment would result in increased (worse) BESS scores compared with a closed, controlled locker room environment in a preseason baseline test across each of the 6 BESS subcategories and the total BESS score.
METHODS
Subjects
Twenty-one uninjured National Collegiate Athletic Association Division I collegiate baseball players (age = 20.1 ± 1.4 years, height = 185.1 ± 6.8 cm, mass = 86.3 ± 9.5 kg) volunteered to participate in the study. Participants were randomly assigned to either the uncontrolled sideline group first (n = 13) or controlled clinical group first (n = 8). All participants completed the same BESS protocol in both types of environments during 2 sessions separated by 1 week (±1 day). Subjects were excluded if they had sustained a head injury within 12 months of the study or had medical conditions that may have adversely affected their postural control (eg, otitis media, Parkinson disease, or Meniere disease) or any lower extremity injuries within 2 months of the study that caused them to miss 1 or more days of practice or game time. Before agreeing to participate, all subjects read and signed an informed consent form approved by the institutional review board, which also approved the study.
Procedures
The BESS test18 comprises six 20-second conditions: double leg, single leg, and tandem (heel-to-toe) stances on a firm surface and then repeated on a foam-type surface. Subjects performed double-leg, single-leg, and tandem stances on an AstroTurf (Dalton, GA) carpeted, rubberized floor mat (firm) and again on a 46 × 43 × 13-cm3 block of medium-density Airex (Alcan Airex, Aargau, Switzerland) pad (foam). The firm surface was a portable AstroTurf carpeted floor mat (eg, baseball batting cage surface) that was used in both the sideline and clinical environments. The purpose of using the AstroTurf mat in both settings was to control the effects of different surface and shoe interactions (eg, concrete surface interaction with baseball shoes) on BESS test performance, thus avoiding the addition of another potential independent variable confounder to the research design. Single-leg dominance was defined subjectively as the leg the subject would use to kick a ball the farthest. The single-leg stance was performed on the nondominant leg, whereas the tandem stance required the nondominant leg to be positioned behind the dominant foot.15,17–19 The double-leg stance conditions consisted of the subject's standing with feet together. All subjects wore standard, team-issued baseball Nike Air Diamond Trainer (Nike, Inc, Beaverton, OR) soft stud shoes for all testing conditions. We decided to use footwear for all baseline testing because this would closely mimic the real-world application of BESS testing during a sideline situation.
Both testing sessions were conducted during regularly scheduled baseball practices during the beginning of the regular season. The clinical environment sessions were conducted in a closed, controlled environment with the investigator and subject present in a quiet locker room with no disruptions from external stimuli. The sideline environment evaluations were conducted in a baseball dugout during live batting practice and intersquad competition with no control of external stimuli. Typical external stimuli in the sideline environment consisted of coaches' instructions, players talking, batted balls, and the sound of the ball hitting the glove.
Participants were instructed to assume the required BESS condition stance by placing their hands on the iliac crests and keeping the head up and facing forward and eyes closed. An error was counted by the investigator if the subject (1) opened the eyes, (2) stepped, stumbled, or fell out of the test position, (3) removed the hands from the hips, (4) moved the hip into more than 30° of flexion or abduction, (5) lifted the toes or heels from the test surface, or (6) remained out of the test position for longer than 5 seconds. Subjects were instructed to make any necessary adjustments if they lost their balance and return to the testing position as quickly as possible. Instructions given to subjects were to “maintain their balance and not commit any balance errors” for both tests, without specific verbal instructions regarding the goal of evaluating environment, yet information concerning the goal of evaluating environmental effects on BESS testing was included in the informed consent information; thus, they were not completely blinded to the purpose of the study. One trial for each test was used, as per previously reported BESS testing studies,18,19,29–31 with a standardized order consisting of double-leg firm, single-leg firm, tandem firm, double-leg foam, single-leg foam, and tandem foam with use of a stopwatch to evaluate each of the 20-second tests. A minimum score of zero errors and a maximum score of 10 errors was possible for each of the 6 testing conditions, and the total score was calculated by adding the scores from the subcategories. A maximum of 10 errors per condition was assigned to individuals who could not complete the testing condition due to high error rates and their desire to terminate the testing. We selected the maximum value of 10 to limit the effects of eliminating data; inaccurate scores could be due to smaller numbers of errors when, in fact, these subjects had the worst scores. We imposed a limit of 10 to account for 1 error per 2 seconds of time. Higher BESS scores are postulated to be associated with decreased postural control. Subject scoring was determined by the same investigator (B.C.B.) for each testing session. Intratester reliability was not assessed for the BESS test investigator, yet he was expertly trained by an instructor (J.A.O.) who had a vast amount of experience with BESS testing and was required to undergo competency testing before the study.
Data Analysis
Mean BESS scores and SDs were calculated for each of the 6 conditions and the total BESS score for each of the testing environments. Data were analyzed using SPSS software (version 12.0; SPSS Inc, Chicago, IL) to evaluate environmental differences in BESS scores. Seven separate, paired-samples t tests were used to determine whether differences existed among the 6 conditions and the total BESS scores for the clinical and sideline testing environments. Alpha levels of statistical significance were set at P ≤ .05 a priori, with a Bonferroni correction (.05/6) resulting in an adjusted alpha level of P ≤ .008. The Bonferroni adjustment was determined for 6 tests because one of the conditions resulted in zero means and variances; thus, a proper statistical analysis was not required. Additionally, effect size analyses were conducted using the Cohen d for t tests calculated using HyperStat online software (http://davidmlane.com/hyperstat/analysisf.html) according to Thalheimer and Cook's 2002 analysis.32 We selected the effect size of the Cohen d and the percentage of relative change from treatment to comparison conditions to evaluate the magnitude of the effects of the uncontrolled sideline environment, which was considered the treatment condition.
RESULTS
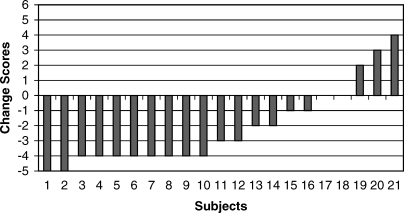
Mean scores for each of the 6 conditions and total scores for both testing environments are reported in the Table. Significant group mean differences were found between testing environments for single-leg foam (t20 = 3.731, P = .001) scores, with higher (worse) scores reported in the uncontrolled sideline environment (7.33 ± 2.11 errors) compared with the controlled locker room environment (5.19 ± 2.16 errors). Analysis of the Cohen d effect size (Table) showed large effect sizes for the single-leg foam testing environment, with a large relative percentage change (41%) resulting in the BESS scores becoming worse in the uncontrolled sideline environment. No significant differences were noted with any of the other conditions across the testing settings with the Bonferroni adjusted P value of ≤ .008. Total BESS scores (t20 = 2.637, P = .016) and tandem-leg foam stance (t20 = 2.556, P = .019) did not satisfy Bonferroni adjusted statistical significance levels, yet evaluation of effect sizes showed medium effects (0.55 and 0.53) with large relative percentage changes (30% and 44%, respectively) across both conditions. The tandem-leg foam stance and total BESS resulted in worse scores in the uncontrolled sideline environment (4.19 ± 2.70 errors and 14.24 ± 5.65 errors, respectively) compared with the controlled locker room environment (2.90 ± 2.26 errors and 10.95 ± 6.55 errors, respectively). Subjective analysis of individual change scores (difference scores between testing environments) showed that 16 participants scored better while testing in the clinical environment, compared with 3 participants who scored better while testing in the sideline environment. Scores for 2 participants did not change for the single-leg foam condition BESS (Figure).
Balance Error Scoring System Scores by Testing Environment (Mean ± SD).
Ranked individual change scores for Balance Error Scoring System (BESS) single-leg foam scores from uncontrolled (sideline) to controlled (locker room) environment. *Negative scores indicate that subjects performed worse on the BESS single-leg foam condition in the uncontrolled sideline environment than in the controlled locker room environment.
DISCUSSION
The main findings of this study indicate that healthy collegiate baseball players performed significantly worse (ie, had higher BESS scores) in an uncontrolled sideline environment compared with a controlled clinical environment for the single-leg foam condition. Additionally, medium to large effect sizes were noted for total, single-leg foam, and tandem stances, with large relative percentage changes from the controlled clinical environment to the uncontrolled sideline environment. These results support our initial hypothesis that testing environment does affect total BESS scores. We also found that subjects scored worse on the 2 purportedly harder BESS test conditions (single-leg foam and tandem-leg foam). Therefore, initial findings from this study show that uncontrolled sideline environments with increased external stimuli attentional demands negatively affected BESS performance in healthy college-aged baseball players.
In the 2004 National Athletic Trainers' Association position statement,4 Guskiewicz et al stated that “when performing baseline testing, a suitable testing environment eliminates all distractions that could alter the baseline performance.” The difficulty in conducting a sideline evaluation during the course of a game or practice is that a “suitable environment free of distractions” is not always a clinical reality. Individuals are often evaluated for postural stability during a clinical evaluation on the sidelines due to time constraints, field supervision demands, and lack of a suitable, distraction-free environment. Thus, our main finding suggesting that the uncontrolled sideline environment adversely affects postural stability BESS scores for single-leg foam is a critical issue when comparing baseline performance with sideline performance after potential injury.
Repeat administration of the BESS warrants concern for possible practice or learning effects that can influence test score results. Valovich et al29 reported that high school athletes scored significantly fewer errors on repeated administration of BESS testing 7 days after baseline, indicating a possible practice effect, but no learning effect was found when 30 days separated the tests. A concern with repeated test administration is increased test familiarity obscuring the results, yet an additional consideration is the type of testing environment used during repeated tests. We evaluated the effects of BESS scores in 2 sessions separated by 1 week. Practice effects may have influenced some of the results, yet Valovich McLeod et al19 noted a practice effect after 3 test administrations before a 1-week assessment. Nonetheless, we should think about the effects of repeat administration of the BESS across days and within similar testing environments because a known and regulated environment (eg, sideline baseball practice) is much different than a closely contested game event that alters motivation to return to play.
In addition to our findings on the effects of environment on BESS performance, we must also consider the effects of fatigue when evaluating factors that influence BESS scores. Wilkins et al30 found that performance in a controlled clinical laboratory environment resulted in decreased total BESS scores after a 20-minute fatigue protocol. Susco et al31 also found that BESS scores were adversely affected by fatigue immediately after exertion, yet baseline levels were achieved within 20 minutes of cessation of activity. Most sideline testing for MHI occurs in athletes who have sustained some form of fatigue while performing during practice or a game, reflecting the need to carefully evaluate BESS scores obtained during a non-fatigued clinical laboratory situation and be cautious when comparing them to an immediate sideline MHI assessment. Sports medicine clinicians should expect to see an increase in BESS scores during a sideline evaluation due to environmental influences, especially during fatigued states, yet future researchers should evaluate these effects in individuals who have either sustained MHI or possess a history of MHI.
Most authors investigating attention and balance have compared the relationship between dual-task paradigms and their effects on cognitive factors in the control of balance.22,25 Redfern et al23 reported that attention is involved in sensory integration, particularly in rejecting conflicting sensory information, during standing postural control in younger and older adults. Woollacott and Shumway-Cook25 hypothesized that if 2 tasks are performed together and 1 requires more than the total attentional capacity, the performance on 1 task will be diminished. Subjects in our study were required to stand as still as possible with their sole focus of attention on maintaining postural control with minimal accessory movements from the original stance position. The uncontrolled external stimuli present during sideline testing unfavorably influenced attentional control, causing BESS scores to be worse. Catena et al33 recently reported altered balance control after a gait evaluation while performing an attention test. They noted that individuals with concussions displayed signs of postural instability with increasing attentional demands, thus further reflecting how external stimuli may negatively affect individuals during a balance test. Because the task was singular in the work of Catena et al,33 with the focus of attention on maintaining postural control, future research using a true dual-task paradigm may be beneficial to understanding the effects of environmental stimuli on postural control.
Onate et al20 reported no significant differences between clinical and sideline testing environments when evaluating cognitive test performance. The conclusion was that clinicians can administer cognitive tests in an uncontrolled sideline environment and expect similar results to those found in a controlled clinical environment. One of the main differences in the findings of the influence of environment on postural control testing using the BESS test is the effect of attentional focus. Neuropsychological cognitive tests require that the subject direct attention to 1 cognitive task, with minimal time to respond to external stimuli. The BESS test for postural control consists of six 20-second tests, leaving ample opportunity for an individual to be influenced by external stimuli (eg, noise, temperature, motivation) and have balance disrupted. The BESS test requires that the subject focus on many factors (eg, hands on hips, not falling, staying in original stance position) during the task, and adding external stimuli seems to disrupt the ability to control movements, increasing the task difficulty. Additionally, our test subjects were healthy individuals involved in a baseline preseason screening assessment; testing individuals with MHI in different environments may result in different findings. Because MHI disrupts the ability to balance and focus attention,15,33–35 we theorize that the effects of a sideline testing environment would be further compounded in individuals with a recent MHI. We would expect BESS scores to be much higher than baseline scores conducted in both sideline and clinical testing environments.
One limitation to this study is the fact that the participants were a small, convenient sample of healthy, college-aged baseball players. First, the incidence of concussion in baseball players is relatively low compared with football, soccer, and wrestling athletes. Second, the a priori power was estimated to be in the 200 range for the multiple comparisons made, and our sample size was grossly underpowered. Even with the small sample size, significant results were demonstrated in the single-leg foam condition. Individual change score analysis revealed that 16 of the 21 subjects (76%) scored fewer total BESS errors in the clinical environment, with 10 of those 16 (63%) subjects scoring at least 4 more BESS error points during the single-leg foam stance in the sideline environment than in the clinical locker room setting. This finding may indicate that some individuals are unable to focus on the postural control task without distraction from external stimuli, or it may reflect more external disturbances for some individuals during the sideline testing scenario. Study results may differ when analyzing different types of athletes (eg, football, soccer, wrestling) in their particular environments and during different types of events (eg, practice versus game). Future testing of the effects of sport-specific environments must be considered when evaluating differences in BESS scores in various environments. A clinical reality is that the sideline testing environment often differs on both a day-to-day and minute-to-minute basis; thus, rigidly controlling the clinical sideline testing environment may improve scientific reliability at the cost of clinical validity. An additional note concerning the BESS testing scenario we used is that we altered the stance environment relative to traditional BESS testing protocols. Our subjects performed all tests with footwear, standardized baseball shoes, trying to replicate the on-field testing scenario as much as possible. We also standardized the floor surface with an AstroTurf mat, based on initial pilot testing with the Airex pad foam surface and the concrete surface used in the dugout during the on-field testing. Future testing should be conducted to determine if the shoe-surface interaction influences BESS testing in a sideline environment, yet we also feel that a small AstroTurf mat and footwear can be easily replicated in an on-field environment at minimal cost.
Certified athletic trainers and other sports medicine clinicians should be aware of the setting in which baseline BESS testing is performed. Consistent environmental settings should be used for both baseline and follow-up testing after concussion. Our results show that clinicians need to know that BESS scores may increase (worsen) when athletes are tested in a sideline environment as compared with a distraction-controlled baseline environment. Caution is always warranted when clinicians evaluate MHIs; recognizing the possible influence of external stimuli and testing environment allows clinicians to make better judgments based on baseline testing information. Future authors should investigate various sporting environments in practices and games, testing in different environmental conditions (eg, cold versus hot temperatures), and the effect of footwear and ankle or knee bracing or taping on BESS scores. Individuals suspected of MHI should always be managed cautiously, following objective, evidence-based protocols, to make better informed clinical decisions. The role of testing environment should be a consideration when evaluating an individual with MHI for postural control using the BESS test. We recommend that baseline testing for postural control using the BESS test be conducted in the setting or environment in which testing after injury will most likely be conducted.
REFERENCES
- Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Inj. 2005;19:85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, McCrea M, Marshall SW. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2549–2555. doi: 10.1001/jama.290.19.2549. et al. [DOI] [PubMed] [Google Scholar]
- Mori T, Katayama Y, Kawamata T. Acute hemispheric swelling associated with thin subdural hematomas: pathophysiology of repetitive head injury in sports. Acta Neurochir Suppl. 2006;96:40–43. doi: 10.1007/3-211-30714-1_10. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, Bruce SL, Cantu RC. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39:280–297. et al. [PMC free article] [PubMed] [Google Scholar]
- Belanger HG, Vanderploeg RD. The neuropsychological impact of sports-related concussion: a meta-analysis. J Int Neuropsychol Soc. 2005;11:345–357. doi: 10.1017/s1355617705050411. [DOI] [PubMed] [Google Scholar]
- Collins MW, Iverson GL, Lovell MR, McKeag DB, Norwig J, Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med. 2003;13:222–229. doi: 10.1097/00042752-200307000-00005. [DOI] [PubMed] [Google Scholar]
- Erlanger DM, Saliba E, Barth JT, Almquist J, Webright W, Freeman J. Monitoring resolution of postconcussion symptoms in athletes: preliminary results of a Web-based neuropsychological test protocol. J Athl Train. 2001;36:280–287. [PMC free article] [PubMed] [Google Scholar]
- Killiam C, Cautin RL, Santucci AC. Assessing the enduring residual neuropsychological effects of head trauma in college athletes who participate in contact sports. Arch Clin Neuropsychol. 2005;20:599–611. doi: 10.1016/j.acn.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Iverson GL, Brooks BL, Collins MW, Lovell MR. Tracking neuropsychological recovery following concussion in sport. Brain Inj. 2006;20:245–252. doi: 10.1080/02699050500487910. [DOI] [PubMed] [Google Scholar]
- McCrea M, Kelly JP, Randolph C. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13:27–35. doi: 10.1097/00001199-199804000-00005. et al. [DOI] [PubMed] [Google Scholar]
- Eyres S, Carey A, Gilworth G, Neumann V, Tennant A. Construct validity and reliability of the Rivermead Post-Concussion Symptoms Questionnaire. Clin Rehabil. 2005;19:878–887. doi: 10.1191/0269215505cr905oa. [DOI] [PubMed] [Google Scholar]
- Piland SG, Motl RW, Guskiewicz KM, McCrea M, Ferrara MS. Structural validity of a self-report concussion-related symptom scale. Med Sci Sports Exerc. 2006;38:27–32. doi: 10.1249/01.mss.0000183186.98212.d5. [DOI] [PubMed] [Google Scholar]
- Piland SG, Motl RW, Ferrera MS, Peterson CL. Evidence for the factorial and construct validity of a self-report concussion symptoms scale. J Athl Train. 2003;38:104–112. [PMC free article] [PubMed] [Google Scholar]
- Guskiewicz KM. Assessment of postural stability following sport-related concussion. Curr Sports Med Rep. 2003;2:24–30. doi: 10.1249/00149619-200302000-00006. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36:263–273. [PMC free article] [PubMed] [Google Scholar]
- Oliaro S, Anderson S, Hooker D. Management of cerebral concussion in sports: the athletic trainer's perspective. J Athl Train. 2001;36:257–262. [PMC free article] [PubMed] [Google Scholar]
- Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35:19–25. [PMC free article] [PubMed] [Google Scholar]
- Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8:71–82. [Google Scholar]
- Valovich McLeod TC, Perrin DH, Guskiewicz KM, Shultz SJ, Diamond R, Gansneder BM. Serial administration of clinical concussion assessment and learning effects in healthy young athletes. Clin J Sport Med. 2004;14:287–295. doi: 10.1097/00042752-200409000-00007. [DOI] [PubMed] [Google Scholar]
- Onate JA, Guskiewicz KM, Riemann BL, Prentice WE. A comparison of sideline versus clinical cognitive test performance in collegiate athletes. J Athl Train. 2000;35:155–160. [PMC free article] [PubMed] [Google Scholar]
- McCollum G, Shupert CL, Nashner LM. Organizing sensory information for postural control in altered sensory environments. J Theor Biol. 1996;180:257–270. doi: 10.1006/jtbi.1996.0101. [DOI] [PubMed] [Google Scholar]
- Parker TM, Osternig LR, Lee HJ, Donkelaar P, Chou LS. The effect of divided attention on gait stability following concussion. Clin Biomech (Bristol, Avon) 2005;20:389–395. doi: 10.1016/j.clinbiomech.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Redfern MS, Jennings JR, Martin C, Furman JM. Attention influences sensory integration for postural control in older adults. Gait Posture. 2001;14:211–216. doi: 10.1016/s0966-6362(01)00144-8. [DOI] [PubMed] [Google Scholar]
- Huxhold O, Li S, Schmiedek F, Lindenberger U. Dual-tasking postural control: aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res Bull. 2006;6:294–305. doi: 10.1016/j.brainresbull.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture. 2002;16:1–14. doi: 10.1016/s0966-6362(01)00156-4. [DOI] [PubMed] [Google Scholar]
- Landers MR, Wulf G, Wallmann HW, Guadagnoli MA. An external focus of attention attenuates balance impairment in patients with Parkinson's disease who have a fall history. Physiotherapy. 2005;91:152–158. [Google Scholar]
- Weeks DL, Forget R, Mouchnino L, Gravel D, Bourbonnais D. Interaction between attention demanding motor and cognitive tasks and static postural stability. Gerontology. 2003;49:225–232. doi: 10.1159/000070402. [DOI] [PubMed] [Google Scholar]
- Rankin JK, Woollacott MH, Shumway-Cook A, Brown LA. Cognitive influence on postural stability: a neuromuscular analysis in young and older adults. J Gerontol A Biol Sci Med Sci. 2000;55:M112–M119. doi: 10.1093/gerona/55.3.m112. [DOI] [PubMed] [Google Scholar]
- Valovich TC, Perrin DH, Gansneder BM. Repeat administration elicits a practice effect with the Balance Error Scoring System but not with the standardized assessment of concussion in high school athletes. J Athl Train. 2003;38:51–56. [PMC free article] [PubMed] [Google Scholar]
- Wilkins JC, Valovich McLeod TC, Perrin DH, Gansneder BM. Performance on the Balance Error Scoring System decreases after fatigue. J Athl Train. 2004;39:156–161. [PMC free article] [PubMed] [Google Scholar]
- Susco TM, Valovich McLeod TC, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the Balance Error Scoring System. J Athl Train. 2004;39:241–246. [PMC free article] [PubMed] [Google Scholar]
- Thalheimer W, Cook S. How to calculate effect sizes from published research articles: a simplified methodology. Available at: http://work-learning.com/effect_sizes.htm. Accessed February 1, 2007.
- Catena RD, van Donkelaar P, Chou LS. Altered balance control following concussion is better detected with an attention test during gait. Gait Posture. 2006;25:406–411. doi: 10.1016/j.gaitpost.2006.05.006. [DOI] [PubMed] [Google Scholar]
- McCrea M, Guskiewicz KM, Marshall SW. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2556–2563. doi: 10.1001/jama.290.19.2556. et al. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, Perrin DH, Gansneder BM. Effect of mild head injury on postural stability in athletes. J Athl Train. 1996;31:300–306. [PMC free article] [PubMed] [Google Scholar]