Abstract
A total of 64 patients with cervical spondylotic myelopathy (CSM) were assessed in this study. Forty-two patients underwent selective expansive open-door laminoplasty (ELAP). Twenty-two patients who underwent conventional C3-7 ELAP served as controls. There were no significant differences in recovery rate of JOA scores, C2–C7 angle or cervical range of motion between two groups. Incidence of axial symptoms and segmental motor paralysis in selective ELAP was significantly lower than those in the C3-7 ELAP. Size of anterior compression mass, postoperative spinal cord positions and decompression conditions were evaluated using preoperative or postoperative MRI in 50 of 64 patients. There was a positive correlation between number of expanded laminae and maximum anterior spaces of spinal cord. Incomplete decompression was developed in three of 37 patients in selective ELAP and in two of 13 patients in C3-7ELAP. Mean size of anterior compression mass at incomplete decompression levels was significantly greater than that at complete decompression levels. Since, there was less posterior movement of the spinal cord in selective ELAP than that in C3-7ELAP, minute concerns about size of anterior compression mass is necessary to decide the number of expanded laminae. Overall, selective ELAP was less invasive and useful in reducing axial symptoms and segmental motor paralysis. This new surgical strategy was effective in improving the surgical outcomes of CSM, and short-term results were satisfactory.
Keywords: Selective cervical laminoplasty, Cervical spondylotic myelopathy, Axial symptoms, Segmental motor paralysis, Posterior shift of spinal cord
Introduction
In most patients with cervical spondylotic myelopathy (CSM), cervical laminoplasty has been performed for posterior cervical surgery. There are many variations in surgical procedure and good clinical results have been reported for many of them [11]. However, there are no clear criteria for the number of the laminae that require treatment and C3–C7 laminoplasty has been performed in most cases [3, 7, 13].
Although the long-term outcomes of the laminoplasty are stable [7,8], postoperative problems such as cervical malalignment [7], restriction of range of motion (ROM) [9], persistent axial symptoms [4] and segmental motor paralysis [1] have been reported. To prevent these problems, recent studies have attempted less invasive surgical procedures [14].
Since 2001, we have indicated selective expansive open-door laminoplasty (selective ELAP) to reduce the damage to cervical posterior elements such as muscle and facet joints. English literature dealing with selective cervical laminoplasty is scant. The purpose of this study was to evaluate the efficacy and short-term results of selective ELAP for CSM.
Materials and methods
A total of consecutive 64 patients with CSM were assessed in this study. Patients with kyphotic deformity treated with decompression in conjunction with correction were excluded.
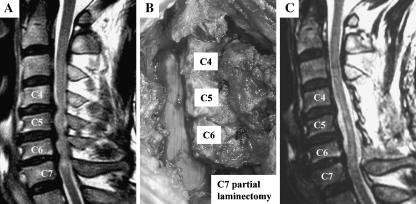
In selective ELAP, open-door laminoplasty was performed only at stenosis levels, and partial laminectomy of the upper half of lamina at the most inferior stenosis level was combined with laminoplasty. To determine the canal stenosis, magnetic resonance imaging (MRI) of cervical spine was used. The stenosis levels were defined by the disappearance of the subarachnoid space at the T2-wighted sagittal images (Fig. 1a). Forty-two patients underwent selective ELAP since 2001 and the mean follow-up period was 33 months. The mean age at the time of surgery was 62 years. The mean pre-operative Japanese Orthopaedic Association (JOA) score was 9.2 points. The mean preoperative C2–C7 angle was 19.9°. The mean cervical range of motion (ROM), which was measured as the angle between C2–C7 on plain radiographs of lateral flexion and extension, was 41.2°. The mean level of canal stenosis was 2.8 levels. Assuming that partial laminectomy was calculated at 0.5 laminae, the mean number of treated laminae was 3.2 (range 1.5–4.5).
Fig. 1.
Case presentation of selective ELAP. a Preoperative MRI shows three-level stenosis from C4/5–C6/7. The stenosis levels were defined by the disappearance of the subarachnoid space. b Intraoperative photograph. In this three levels stenosis case, the laminae from C4 to C6 laminae were opened in conjunction with upper half laminectomy of C7. c Postoperative MRI
Twenty-two patients with CSM who underwent conventional C3-7 ELAP in our hospital before 2001 served as controls and the mean follow-up period was 72 months. The mean age at the time of surgery was 64 years. The mean pre-operative JOA score was 10.4 points. The mean preoperative C2–C7 angle was 21.6°. The mean cervical ROM was 40.6°. The mean level of canal stenosis was 2.5 levels. There was no significant difference of pre-operative parameters between the two groups (Table 1).
Table 1.
Preoperative patient demographics
| Selective ELAP | C3-7ELAP | |
|---|---|---|
| Gender | Man: 28, woman: 14 | Man: 17, woman: 5 |
| Age | 62 (39–85) | 64 (39–79) |
| JOA score | 9.2 (4–14.5) | 10.4 (2.5–14.5) |
| C2–C7 angle | 19.9 ± 1.9° | 21.6 ± 4.7° |
| Range of motion | 41.2 ± 1.8° | 40.6 ± 2.9° |
| Stenosis level | 2.8 (1–4) | 2.5 (1–4) |
| Number of expanded laminae | 3.2 (1.5–4.5) | 5 |
Values are indicated as mean ± standard error and range is given in parenthesis
Surgical indication and technique for selective ELAP
The criteria of the surgical method used in the current study was as follows: anterior spinal fusion was indicated for patients with CSM in whom the spinal canal stenosis caused by anterior compression mass is one or two levels and the spinal canal is 13 mm and over. On the other hand, ELAP was indicated for patients with multilevel compression myelopathy, developmental spinal canal stenosis (less than 13 mm), or spinal canal stenosis caused by posterior elements such as the ligamentum flavum.
To determine the decompression area, MRI and plain radiographs of cervical spine were used for selective ELAP. The laminae to expand were determined as follows: from one level above the most cranial stenosis level to upper half partial laminectomy of the most caudal stenosis level. The method described below is based on three-level stenosis case from C4–C5 to C6–C7 (Fig. 1a). After longitudinally dividing the nuchal fascia in line with the mid line incision, the laminae from C4 to upper half lamina of C7 were exposed. The C3–C4 and C6–C7 interlaminar spaces were exposed and the ligamentum flavum at those levels were removed. In accordance with the so-called Hirabayashi’s open-door method, [3] open-side and hinge-side gutters were made using a high-speed drill at the C4, C5 and C6 laminae. Before the ‘open-door’ technique, the upper half laminectomy of C7 was performed leaving untouched the attachment of the semispinalis cervicis and multifidus muscle of C7. The laminae were elevated and secured to the facet joints by using sutures (Fig. 1b, c).
Surgical technique for conventional C3-7 ELAP
For conventional C3-7 ELAP, surgical procedures were performed according to Hirabayashi’s method [3].
Postoperative care
The patients of both groups were allowed to sit up or walk between 2 and 5 days after surgery with a cervical brace for 3 weeks. Isometric and isotonic muscle contraction of the posterior neck was recommended after surgery as soon as possible.
Evaluation
Clinical and radiological results were evaluated at 1 year and 2 years after surgery. Clinical recovery rates were evaluated using Japanese Orthopaedic Association (JOA) scores. Local symptoms (pain and stiffness), or so-called axial symptoms, were evaluated using an axial symptom scoring system that was developed at our institution. In this scoring system, there were four parameters (i.e., posterior neck pain, posterior neck stiffness, shoulder pain, shoulder stiffness) and each parameter was classified into four grades (i.e., none: 3, occasional mild: 2, continuous mild or occasionally severe: 1, continuously severe: 0). The analgesics utilized after surgery were also evaluated. The incidence of postoperative segmental motor paralysis, or so-called C5 palsy, was examined in both groups during the follow-up period.
Preoperative and postoperative cervical alignment was evaluated using C2–C7 angle. Cervical ROM was measured as the angle between C2–C7 on plain radiographs of lateral flexion and extension. The % ROM was calculated using the following formula: (post operative ROM/preoperative ROM) × 100.
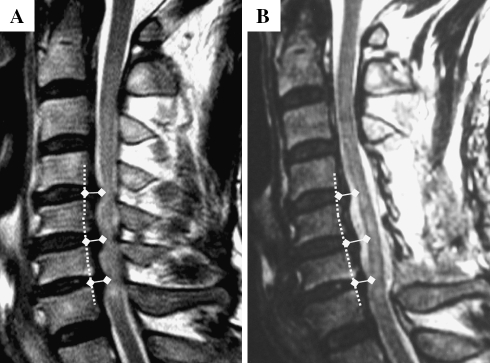
The size of anterior compression mass, postoperative spinal cord positions and decompression conditions were evaluated using preoperative or postoperative MRI in 50 of 64 patients (selective ELAP: 37, C3-7ELAP: 13), in which a quality of MRI was enough to investigate. Postoperative MRI was obtained 1–6 months after surgery. MRI of T2-weighted sagittal image was analyzed using Scion Image Beta 4.02 (Scion Co., Maryland, USA). A baseline was drawn to link the middle point of posterior vertebral body margin, and the distances from the baseline to the posterior edge of anterior compression mass (i.e., size of anterior compression mass) or to the anterior edge of spinal cord (i.e., anterior space of spinal cord) at the disc level were measured at the stenosis levels in the selective ELAP group and at all four levels in the C3-7 ELAP group (Fig. 2).
Fig. 2.
Size of anterior compression mass and anterior space of spinal cord. Figure shows C4–C6 expansive open-door laminoplasty in conjunction with C7 upper half laminectomy of three-level stenosis case. A baseline (dotted line) was drawn to link the middle point of posterior vertebral body margin and the anterior compression mass (a) and anterior space of the spinal cord (b) were measured at the disc levels
Statistical analysis
Data were expressed as the mean ± standard error. Comparisons between the selective and conventional C3-7 ELAP groups were made by a t test, a Mann–Whitney’s U test or Fisher’s exact probability test. Correlations were evaluated using Spearman’s correlation coefficient by rank test. Differences with P values of less than 0.05 were considered significant.
Results
Clinical and radiological results were shown in Table 2. There was no significant difference of the recovery rate of JOA score, C2–C7 angle and %ROM between the two groups.
Table 2.
Clinical and radiological results
| Selective ELAP | C3-7 ELAP | Statistical analysis | |
|---|---|---|---|
| Recovery rate of JOA score (1-year) | 58.7 ± 3.6% | 52.7 ± 5.8% | NS |
| Recovery rate of JOA score(2-year) | 57.7 ± 3.6% | 53.4 ± 5.0% | NS |
| Axial symptoms (1-year) | 11.5 ± 0.1 | 9.5 ± 0.5 | P < 0.001 |
| Axial symptoms (2-year) | 11.4 ± 0.1 | 10.1 ± 0.5 | P = 0.026 |
| Analgesics (1-year) | 3/42 | 8/22 | P = 0.006 |
| Analgesics (2-year) | 4/42 | 4/22 | NS |
| C5 palsy | 0/42 | 3/22 | P = 0.037 |
| C2–C7 angle (1-year) | 21.2 ± 2.0° (107%) | 21.4 ± 4.0° (99%) | NS |
| C2–C7 angle (2-year) | 20.9 ± 1.9° (105%) | 22.4 ± 3.8° (99%) | NS |
| %ROM (1-year) | 70.4 ± 5.2% | 72.3 ± 9.9% | NS |
| %ROM (2-year) | 70.6 ± 7.8% | 65.4 ± 8.9% | NS |
Post/pre-operation % are given in parenthesis
The mean axial symptoms score of 11.5 (1-year) and 11.4 (2-years) in selective ELAP group was significantly higher than those of 9.5 (1-year) and 10.1 (2-years) in C3-7 ELAP group. The analgesics utilized in the selective ELAP group were significantly less than those in C3-7 ELAP group at 1 year after surgery, but not significantly different at 2 years after surgery.
Although none of the patients in the selective ELAP group exhibited postoperative segmental motor paralysis, the paralysis developed in three of 22 patients in the C3-7 ELAP group. The incidence of segmental motor paralysis in selective ELAP group was significantly lower than that in C3-C7 ELAP group. C5, C6 and C7 palsy was developed at two-day, four-day and 1.5-month after surgery, respectively in C3-7 ELAP groups. Spontaneous recovery was observed in two cases at 5 and 6 months after surgery.
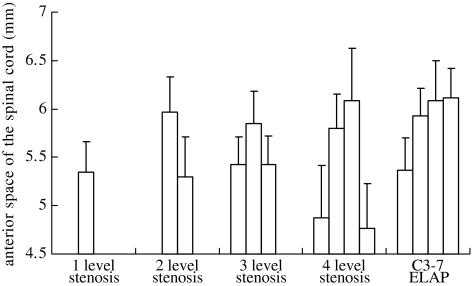
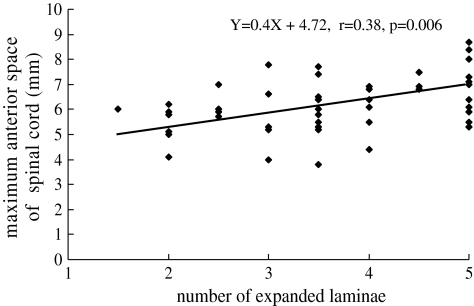
There was no significant difference of the mean size of anterior compression mass between the two groups (Table 3). The postoperative anterior space of the spinal cord was shown in Fig. 3. The anterior space of the spinal cord ranged from 3.0 to 8.7 mm, and the maximum spaces were obtained at the middle of laminoplasty. The mean value of maximum anterior space of the spinal cord was 5.5 mm in the selective ELAP group and was 5.9 mm in C3-C7 ELAP group (Table 3). The more the number of expanded laminae increased, the more the maximum anterior space of the spinal cord enlarged. There was a positive correlation between the number of expanded laminae and the maximum anterior spaces of the spinal cord (Fig. 4).
Table 3.
Preoperative and postoperative MRI findings
| Selective ELAP | C3-7 ELAP | Statistical analysis | |
|---|---|---|---|
| Anterior compression mass | 3.9 ± 0.1 mm | 3.8 ± 0.2 mm | NS |
| Maximum anterior space of spinal cord | 5.5 ± 0.1 mm | 5.9 ± 0.1 mm | P = 0.015 |
| Incomplete decompression | 3/37 | 2/13 | NS |
Fig. 3.
Anterior space of spinal cord. The anterior space of spinal cord increased in the middle position of the laminoplasty. The maximum anterior space of spinal cord showed a tendency to increase in proportion to the number of expanded laminae
Fig. 4.
Maximum anterior space of spinal cord associated with number of expanded laminae. There was a significant correlation between the maximum anterior space of spinal cord and the number of expanded laminae (r = 0.38, P = 0.006)
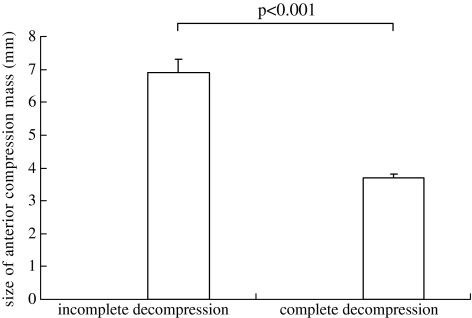
Incomplete decompression was defined as residual concave deformity of spinal cord caused by compression mass using postoperative MRI. Incomplete decompression was developed in 3 of 37 patients in the selective ELAP and in 2 of 13 patients in the C3-7ELAP group (Table 3). All of compression mass at incomplete decompression levels were 6 mm and over. The mean size of anterior compression mass at incomplete decompression level was significantly greater than that at complete decompression level (Fig. 5). However, the recovery rates of JOA scores were 64.2 ± 5.5% in incomplete decompression cases and 57.9 ± 3.0% in complete decompression cases.
Fig. 5.
Size of anterior compression mass associated with postoperative decompression condition. The mean size of anterior compression mass was 6.4 ± 0.2 mm at incomplete decompression levels and 3.7 ± 0.1 mm at complete decompression levels (P < 0.001)
Discussion
The optimal surgical treatment for multilevel cervical spinal cord compression caused by cervical spondylosis remains controversial. Anterior decompression and fusion [2, 18], laminectomy with or without fusion [5], and expansive laminoplasty [3] have all been performed to treat multilevel CSM. In Japan, laminoplasty is the most common procedure out of concern for complications [2, 18] such as dislodgement of graft bone, pseudoarthrosis, adjacent level’s stenosis, kyhotic deformity and instability.
Although satisfactory results of the laminoplasty are maintained for more than 10 years after surgery [7], several postoperative problems including neurological deterioration caused by malalignment [8], restriction of ROM [18], axial symptoms [4] and postoperative C5 palsy [1, 12] have been reported.
The common purpose of various laminoplasty procedures is to obtain the posterior movement of the spinal cord. Generally, five laminae (i.e., C3–C7) are indicated for expansion in most institutions. Before 2001, C3-7 ELAP was indicated for all patients in our institute for the purpose of obtaining sufficient posterior movement of the spinal cord. However, in a postoperative MRI of C3-7 ELAP, excessive posterior movement of the spinal cord is not unusual. Therefore, it is doubtful whether C3-7 laminoplasty, which expands five laminae, is necessary for all patients with CSM. Since 2001, we have indicated selective ELAP to reduce postoperative problems.
Although the present study has some limitations of research methodology (i.e., irregular operator or appraiser and the difference of therapeutic period between the two groups), the pre-operative parameters of both groups were almost equal between the two groups. Therefore, the study design of this study is a retrospective cohort study indicating different surgical strategies for two groups.
The results of the present study demonstrated that there was no significant difference in neurological recovery rates between the two groups. Because the mean number of the laminae managed with surgery was 3.2 in selective ELAP, this procedure was less invasive for facet joints, ligaments and muscle than conventional C3-7 ELAP.
The high incidence of a change from a preoperative lordotic alignment to a postoperative straightened or kyphotic alignment after laminoplasty has been reported [7,8]. Since there is a relationship between severe local kyphosis and poor surgical outcomes [15], maintaining the cervical alignment is one of the keys to satisfactory neurological recovery. In our results, the cervical alignments evaluated using the C2–C7 angle were maintained in both groups, in contrast to previous reports [7, 13, 18]. In the present study, cervical alignments may have been maintained in both groups because we encouraged the patients to do early active cervical exercises after surgery and the cervical brace was worn only for 3 weeks.
There are some confusing aspects about cervical ROM in the literature on laminoplasty. Some authors have asserted that limitation of ROM leads to a reduction of dynamic factors and is associated with satisfactory neurological improvement [10]. In contrast, other authors have noted the importance of preserving cervical ROM to reduce axial symptoms [6] or to maintain cervical alignment [9]. The decrease of cervical ROM was not significantly different between the two groups in the present study. That is, reducing the surgical invasion did not contribute to maintenance of cervical ROM. However, other authors of long-term follow-up studies have demonstrated a clear trend toward chronological loss of cervical ROM after laminoplasty [7, 13], so significant differences in the decrease of ROM between the selective ELAP and C3-7 ELAP may emerge at long-term follow-up.
The incidence of axial symptoms (pain or stiffness in the neck or shoulder) varies markedly [4, 17] largely because of differences in the definition of what constitutes axial symptoms or when axial symptoms are recorded. Although several studies have recently reported the importance of axial symptoms [4, 6, 14] their underlying mechanisms are not fully understood. Potential sources include the cervical disc, musculature, facet joints, spinal cord, and nerve roots [4,17]. Axial symptoms were evaluated using semi-quantitative scoring system in this study. The present study demonstrated that selective ELAP, which was less invasive for the posterior elements, could reduce the axial symptoms not only at 1 year but also at 2 years after surgery. This suggests that axial symptoms may be caused in part by musculature or facet joints.
Segmental motor paralysis, or so-called C5 palsy, is seen occasionally in patients treated with laminoplasty, and in studies in which C5 palsy is reported, the mean incidence is about 5–8% [11, 12]. It is interesting that C5 palsy was not observed after selective ELAP in the present study. Although the mechanisms underlying C5 palsy remain unclear, some possible causes (i.e., nerve root and spinal cord) have been reported [1, 12]. One of the causes of C5 palsy has been attributed to a nerve root tethering effect [16] caused by excessive posterior movement of the spinal cord after decompression. The present study demonstrated that the number of expanded laminae is correlated with the maximum anterior space of the spinal cord. Therefore, the mechanism of less incidence of C5 palsy in selective ELAP may be elucidated by less posterior movement of the spinal cord in selective ELAP than after C3-7 ELAP. All these results suggest that selective ELAP has the potential to reduce the incidence of C5 palsy. However, high incidence of C5 palsy in C3-7 ELAP may affect the statistical significance in the current study; further, a large study is necessary to evaluate the evidence.
Incomplete decompression caused by anterior compression mass developed in five patients. The size of anterior compression mass at incomplete decompression level was significantly greater than that of complete decompression level, and was 6 mm and over at all incomplete decompression levels. The results of the current study demonstrated that one of the risk factors for incomplete decompression is the size of anterior compression mass. In the selective ELAP, there was less posterior movement of the spinal cord than that in C3-7ELAP, minute concerns about the size of anterior compression mass is necessary to decide the number of expanded laminae. Therefore, in the case of anterior compression mass over 6 mm at most inferior or superior level, one more lamina is expanded in our new strategy.
Overall, selective ELAP was useful in reducing surgical invasions and postoperative problems compared with conventional C3-7 ELAP. However, further study and long-term follow-up investigations will be necessary to certify the firm evidence.
Conclusions
Selective ELAP was less invasive and useful in reducing axial symptoms and segmental motor paralysis. This new surgical strategy was effective in improving the surgical outcomes of CSM, and short-term results were satisfactory.
References
- 1.Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Hirabayashi K (2002) Segmental motor paralysis after expansive open-door laminoplasty. Spine 27:2108–2115 [DOI] [PubMed]
- 2.Edwards CC, Heller JG, Murakami H (2002) Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine 27:1168–1175 [DOI] [PubMed]
- 3.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y (1983) Expansive open-door laminoplasty for cervical stenotic myelopathy. Spine 8:693–699 [DOI] [PubMed]
- 4.Hosono N, Yonenobu K, Ono K (1996) Neck pain and shoulder pain after laminoplasty. Spine 21:1969–1973 [DOI] [PubMed]
- 5.Houten JK, Cooper PR (2003) Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of posterior longitudinal ligament: effects on cervical alignment, spinal cord compression and neurological outcome. Neurosurgery 52:1081–1087 [DOI] [PubMed]
- 6.Kawaguchi Y, Kanamori M, Ishihara H, Nobukiyo M, Seki S, Kimura T (2003) Preventive measure for axial symptoms following cervical laminoplasty. J Spinal Disord Tech 16:497–501 [DOI] [PubMed]
- 7.Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Nakamura H, Kimura T (2003) Minimum 10 years follow-up after en bloc cervical laminoplasty. Clin Orthop Relat Res 411:129–139 [DOI] [PubMed]
- 8.Kimura I, Shingu H, Nasu Y (1995) Long-term follow-up of cervical spondylotic myelopathy treated by canal-expansive laminoplasty. J Bone Joint Surg 77B:956–961 [PubMed]
- 9.Maeda T, Arizono T, Saito T, Iwamoto Y (2002) Cervical alignment, range of motion, and instability after cervical laminoplasty. Clin Orthop Relat Res 401:132–138 [DOI] [PubMed]
- 10.Morio Y, Yamamoto K, Teshima R, Nagashima H, Hagino H (2000) Clinicoradiologic study of cervical laminoplasty with posterolateral fusion or bone graft. Spine 25:190–196 [DOI] [PubMed]
- 11.Ratliff JK, Cooper PR (2003) Cervical laminoplasty: a critical review. J Neurosurg (Spine 3) 98:230–238 [DOI] [PubMed]
- 12.Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H (2003) C5 palsy after decompression surgery for cervical myelopathy: review of literature. Spine 28:2447–2451 [DOI] [PubMed]
- 13.Satomi K, Nishi Y, Kohno T, Hirabayashi K (1994) Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine 19:507–510 [DOI] [PubMed]
- 14.Shiraishi T, Fukuda K, Yato Y, Nakamura M, Ikegami T (2003) Results of skip laminectomy -mimimum 2-year follow-up study compared with open-door laminoplasty. Spine 28:2667–2672 [DOI] [PubMed]
- 15.Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M (2003) Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 28:1258–1262 [DOI] [PubMed]
- 16.Tsuzuki N, Abe R, Saiki K, Zhongshi L (1996) Extradural tethering effects as one mechanism of radiculopahty complicating posterior decompression of the cervical spinal cord. Spine 21:1839–1840 [DOI] [PubMed]
- 17.Yoshida M, Tamaki T, Kawakami M, Nakatani N, Ando M, Yamada H (2002) Dose reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty ? Spine 27:1414–1418 [DOI] [PubMed]
- 18.Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K (2001) Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy. Spine 26:1433–1448 [DOI] [PubMed]