Abstract
Osteoid osteoma (OO) of the cervical spine is frequently located close to the vertebral artery, spinal cord, or nerve roots and complete surgical excision is sometimes difficult by a limited approach and more extended surgery can require spinal fusion. Percutaneous radiofrequency coagulation (PRC) has demonstrated efficacy in the treatment of OO of the pelvis and limbs however, its role in the cervical spine is still nuclear. The Authors present a series of nine cases of OO of the cervical spine, six treated with surgical excision and three with PRC. No neurological or vascular complications occurred in both series. One case of the surgical series had only partial relief of persistent pain for 1 year due to incomplete excision, but is doing well 4 years after surgery. All the other surgical cases had complete relief of symptoms immediately after surgery and are symptom-free 3–10 years later. Two cases of PRC had complete relief of symptoms 24–48 h after surgery and are symptom-free 2 and 3 years later. One case of recurrent OO after surgery and treated with PRC with a reduced dose improved only, and still requires anti-inflammatory drugs 2 years after the procedure. Our still limited experience suggests that PRC can be safely performed in local anaesthesia with the patient awake, enabling to check for signs and symptoms of possible neurological injury. PRC can substitute extensive posterior approaches and reconstructions for OO of the posterior arch and joint pillar.
Keywords: Osteoid osteoma, Cervical spine, Percutaneous radiofrequency coagulation, Bone tumors, Cervical spine fusion
Introduction
Osteoid Osteoma (OO) is localized in the cervical spine in 4% of cases, representing 40% of the cases affecting the vertebral column [4, 8]. Frequent localization in the immediate vicinity of vertebral artery [10], of the spinal cord, and/or the nerve roots often renders its excision difficult and risky through an mini-invasive approach [14, 18] (Fig. 1). Percutaneous radiofrequency coagulation (PRC) has shown to be effective in the treatment of OO of the hip and limbs [3, 7, 15, 17], but its role in the treatment of vertebral and above all cervical localizations is still unclear, because of the limited number of cases reported and coagulation in the vicinity of nervous and vascular structures is risky [3, 14]. The goal of our study is to introduce our experience in the treatment of osteoid osteoma of the cervical spine with surgical therapy and percutaneous radiofrequency coagulation.
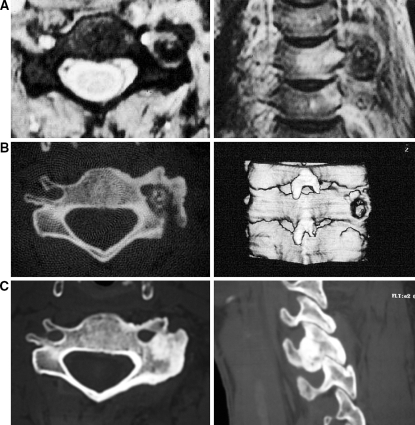
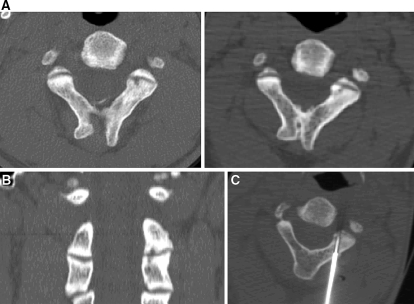
Fig. 1.
a Male 24 years old with OO of the C5 joint pillar in relation to the vertebral artery. b CT scan control 2 months after partial excision through a posterior approach with a mini-access using an operating microscope: residue at approximately midway of the lesion. c CT scan control 4 years after surgical treatment: complete ossification of the lesion. The patient is without symptoms
Materials and methods
Our series included nine cases of OO of the cervical column, six males and three females, with an age comprised between 20 and 44 years (average 28 years). Six cases were treated with surgical excision and three with PRC. All cases were studied with CT scans, MRIs, scintigraphy with 99 technetium and the constant clinical-radiographic observations are typical of osteoid osteoma [4, 8]. In all cases surgically treated, histological examination confirmed the clinical-radiographic diagnosis. In the cases treated with PRC, biopsies were not taken [1].
Of the three cases operated, one localized at the vertebral body (C4) and two at the transverse process (C5 and C6) (Fig. 2), were treated with excision through an anterior approach [8, 13].
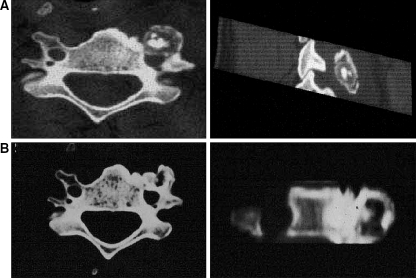
Fig. 2.
a Male 32 years old with OO of the transverse process of C% in relation to the vertebral artery. b Control 10 years after complete excision of the nidus: peripheral ossification of the lesion. The patient is without symptoms
Three cases localized at the joint pedicle were treated with simple excision through a posterior mini-access with the use of an operating microscope (C5) (Fig. 1), and two (C5 and C6) were treated with an extended posterior excision with a demolition of the joint pillar and posterior fusion fixed with plates (Fig. 3).
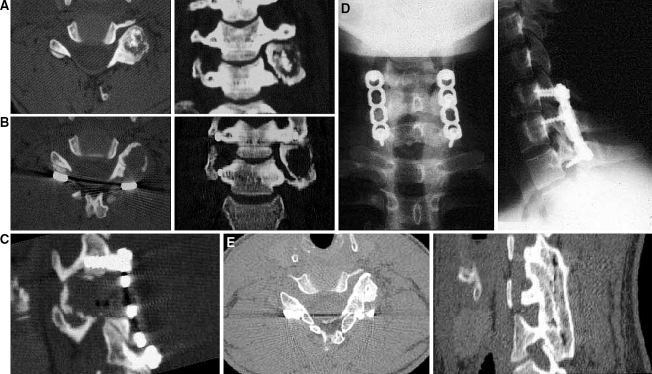
Fig. 3.
a Male 28 years old with OO of the C6 joint pillar. b CT scan controllo after complete excision of the nidus with a posterior fusion of C5–C7 using plates. c Particular of a parasagittal reconstruction showing extensive demolition of the joint pillar. d Radiographic control of the positioning of the plates. e–f Ossification of the lesion and fusion of the arthrodesis 7 years after treatment
Of the series treated with PRC, two cases at the spinous process (C2) (Fig. 4) and of the joint pillar (C3) (Fig. 5), were treated in local anesthesia with 2% carbocaine 2% and deep sedation with zemifentanil, with an intralesional temperature of 90°C for 18 min. In the third case, localized at the body of C3, was a recurrence after surgical excision with PRC with general anesthesia requested by the patient, interrupting the procedure every 3–5 min in order to control somatosensory effects caused that cannot be recorded during the activity of cauterization: for this reason, the dosage considered to be effective (18 min at 90°C) was not reached.
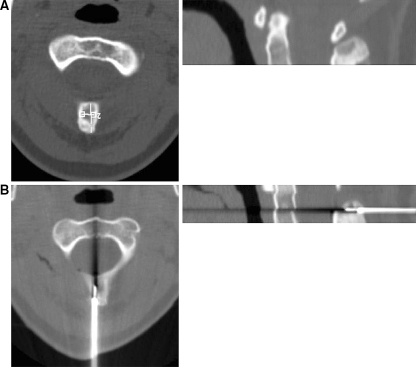
Fig. 4.
a Female 20 years old with OO of the spinal apophysis of C2. b Positioning of the cauterization needle. The patient is without symptoms 2 years after treatment
Fig. 5.
a, b Male 29 years old with OO of the joint apophysis of C3. c Positioning of the cauterization needle. The patient is without symptoms 3 years after treatment
The instrumentation used for PRC is the bioptic needle set of the Bonopty company (Radii MS, Hupsala, Sweden) comprising of a trochar of 14G, a drill with an eccentric tip and a 20G bioptic needle; the generator utilized is a RFG-3C, cauterization needle SMK 15 (length 145 mm bore 0.35 mm) and a disposable 20 G cannula with a 10–15 mm active tip manufactured by Radionics (Burlington BUT, USA).
The positioning of the cauterization needle in the nidus of the OO was performed with a guided CT approach with a series of continuous scans of 1 mm and two-dimensional reconstructions [1, 15, 16]. Two dispersive cauterizations were utilized and usually placed cranial to the lesion in order to reduce the spread of radiofrequency towards the mobile structures [2].
All the cases were controlled after 2–10 years (average 5.5 years).
No vascular and/or neurological complications were observed in our series.
Results
Of the cases operated, the patient treated with a microsurgical approach (Fig. 1a) had a partial improvement in pain, due to an incomplete excision of the nidus (Fig. 1b) with slight pain and persistent neck rigidity for 1 year. Subsequently, pain disappeared, and the CT scan taken at 4 years showed complete ossification of the residual OO excised (Fig. 1c).
All the other surgically treated cases had an immediate alleviation of pain and are asymptomatic 3–10 years after surgery. Complete (Fig. 3e) or incomplete (Fig. 2b) ossification of the lesion, and fusion of the arthrodesis (Fig. 3e), were performed, was seen radiographically.
The two cases treated with PRC with an adequate dose (18 min at 90°C), had resolution of pain 24–48 h after treatment and are asymptomatic after 2 and 3 years.
The case of post-operative recurrence treated in general anesthesia with PRC at a reduced dose only improved, with the need to assume anti-cox2 drugs at 2 years after treatment.
No important morphologic variations after PRC were seen radiographically during the short period of observation.
Discussion
Complete surgical excision of the osteoid osteoma through a limited approach [5, 12] is rather difficult: there are numerous published observations that these result in “premature recurrences” due to an incomplete excision of the lesion [14, 18] (Fig. 1). In these cases, the natural history of the OO [4], that can also evolve spontaneously, but unpredictable healing can indicate therapeutic suspension (Fig. 1), but persisting intense pain can require reintervention.
Frequent localization in the joint-peduncle area [12] can require extensive excision of the OO, with an interruption of the spinal column and arthrodesis [6] (Fig. 3), resulting in a limitation of mobility of the spinal column secondary to fusion (Fig. 3d, g). For similar biomechanical reasons, surgical resection of the C2 spinous process, in the case treated with PRC (Fig. 4), can also present a problem of secondary instability.
Percutaneous radiofrequency coagulation in our still limited experience has demonstrated to be effective and secure, performing the procedure in local anesthesia with deep sedation that maintains regional sensitivity and possibly enables the patient to indicate an irradiation of pain or anomalous pain, and to monitor neurological functions. In the literature, the heat dosage applied to the apex of the cauterization needle for the treatment of localized OO throughout is 4 min at 90°C [11, 15] or 6 min at 90°C [9, 17], with a success rate of approximately 90%.
At the beginning of our experience, we applied PRC at 90°C for 4 min with a high percentage of failures (40%). We therefore gradually increased the time of application, reaching 18 min at 90°C, an amount that we proposed as an “effective dose”. We believe that in the case of PRC performed with a partial result, was due to the low dosage reached. In this context, we believe to be able to assert that general anesthesia is contraindicated due to the impossibility to monitor neurological functions along with the necessity to interrupt the procedure periodically in order to control spinal function with potential somatosensory effects caused. The repeated interruptions do not enable to reach the effective dose that we recommend.
Conclusions
Our study, although with the limitations of a small casuistry and rarity of the pathology, indicates that PRC in the treatment of cervical osteoid osteoma is equally effective to surgery with respect to the control of symptoms. Frequent localization in the posterior arch presents the problem of secondary instability with surgical excision. Extensive and unbalanced approaches require associated posterior fusion. PRC can replace extensive surgical approaches for OO of the posterior arch and of the joint pillar, obtaining remission of the symptoms with a mini-invasive technique that has demonstrated to be applicable also in vicinity of noble and fragile structures such as the vertebral artery, spinal cord and nerve roots. The highlights of this technique include: local anesthesia, direct control of the neurological functions, meticulous execution of the technique, i.e., cauterization positioning, dispersed cauterization, duration of the application, and cauterization temperatures.
Footnotes
Read at the 21st “Annual Meeting of the Clinical Spine Research Society—European Section”, Rome, 16–17 June 2005. Authors’ declaration: This study complies with the current laws of the country in which it was performed inclusive of ethics approval.
References
- 1.Albisinni U, Rimondi E,Malaguti MC, Ciminari R (2004) Radiofrequency thermoablation in the treatment of osteoid osteoma (letter). Radiology 232:304–305 [DOI] [PubMed]
- 2.Albisinni U, Rimondi E, Malaguti MC, Ciminari R (2004) A comment on CT-guided radiofrequency thermal ablation of osteoid osteoma (letter). AJR 183:538–539 [DOI] [PubMed]
- 3.Barei P, Loreau G, Scarborough MT, Neel MD (2000) Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Rel Res 373:115–124 [DOI] [PubMed]
- 4.Campanacci M (1990) Bone and soft tissue tumors. Aulo Gaggi, Bologna, pp 355–374
- 5.De Praeter MP, Dua G, Seynaeve PC, Vermeersch DG, Klaes RL (1999) Occipital pain in osteoid osteoma of the atlas. A report of two cases. Spine 24:912–914 [DOI] [PubMed]
- 6.Faraj A, Byrne P, Mehdian H (1998) Osteoid osteoma of the lateral mass of C5. Should excision be combinated with fusion? Eur Spine J 7:242–245 [DOI] [PMC free article] [PubMed]
- 7.Ghanem J, Collet LM, Kharrat K, Samaha E, Deramon M, Mertl P, Dagher F (2003) Percutaneous radiofrequency coagulation of osteoid osteoma in children and adolescents. J Ped Orthop B 12:244–252 [DOI] [PubMed]
- 8.Giunti A, Laus M (1991) Le radiocolopatie spinali. Aulo Gaggi, Bologna, pp 212–215
- 9.Hadjipavlou AG, Lander PH, Marchesi D, Katonis PG, Gaitanis IN (2003) Minimally invasive surgery for ablation of osteoid osteoma of the spine. Spine 22:E472–E477 [DOI] [PubMed]
- 10.Laus M. Zappoli FA, Malaguti MC, Alfonso C (1997) Surgery of primary bone tumors close to the vertebral artery. XIII Meeting Cervical Spine Research Society, European Section, Burgenstock Estate, Switzerland 26–28 June 1997, Abstract book, pp 31
- 11.Lindner NJ, Ozaki J, Roedl R, Gosheger G, Winkelmann W, Wortler K (2001) Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg 83B:391–396 [DOI] [PubMed]
- 12.Matsuura M, Nakamura H, Inoue Y, Yamano (2000) Osteoid osteoma of the cervical spine depicted as dumbbell tumor by MRI. Eur Spine J 9:426–429 [DOI] [PMC free article] [PubMed]
- 13.Molloy S, Saifuddin A, Allibone J, Taylor BA (2002) Excision of an osteoid osteoma from the body of the axis through an anterior approach. Eur Spine J 11:599–601 [DOI] [PubMed]
- 14.Ozaki T, Liljeqvist U, Hillmann A, Halm H, Lindner N, Gosheger G, Winkelmann W (2002) Osteoid osteoma and osteoblastoma of the spine: experience with 22 patients. Clin Orthop Rel Res 357:394–402 [DOI] [PubMed]
- 15.Pinto CH, Taminiau AHM, Vanderschueren GM, Hogendoorn PC, Bloen JL, Obermann WR (2002) Technical consideration in CT-guided radiofrequency thermal ablation of osteoid osteoma: tricks of the trade. AJR 1633:1642 [DOI] [PubMed]
- 16.Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ (2003) Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology 229:171–175 [DOI] [PubMed]
- 17.Rosenthal D, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC (1998) Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg 80A:815–821 [DOI] [PubMed]
- 18.The Cervical Spine Research Society (1998) The cervical spine, 3rd edn. Lippincott, New York, pp 634–635