Short abstract
Increased understanding of the anatomy of haemorrhoids has led to the development of new procedures to treat them. Among the surgical options for intractable prolapsed haemorrhoids, formal haemorrhoidectomy now competes with stapled haemorrhoidopexy, which is less painful and allows a shorter convalescence but may have a higher recurrence rate and needs further long term evaluation
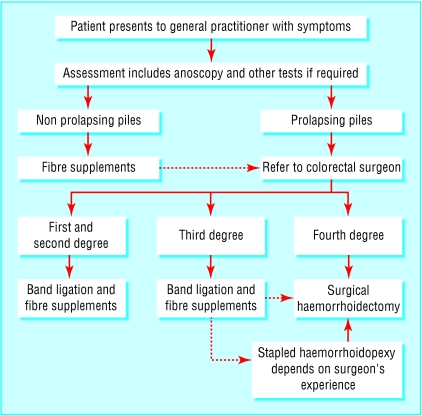
Improvements in our understanding of the anatomy of haemorrhoids have prompted the development of new and innovative methods of treatment. Unfortunately confusion still exists among lay people and doctors, who misuse the terms haemorrhoids and piles to cover a variety of complaints. This has led to estimates of prevalence varying from 4.4% among adults in the United States to 36.4% in general practice in London.1,2 This article describes the pathogenesis of haemorrhoids and management strategies (fig 1).
Fig 1.
Suggested algorithm for management of haemorrhoids (dotted arrows indicate failure of initial treatment)
Methods
We retrieved evidence based articles from the Medline database and Cochrane Library under the MESH subheading “hemorrhoid.” We included randomised controlled trials with valid end points and meta-analyses.
Pathogenesis
The anal canal has a triradiate lumen lined by three fibrovascular cushions of submucosal tissue. The cushions are suspended in the canal by a connective tissue framework derived from the internal anal sphincter and longitudinal muscle. Within each cushion is a venous plexus that is fed by arteriovenous communications. These specialised vascular structures allow for enlargement of the cushion to maintain fine continence. In health as in disease the anal cushions appear in the right anterior, right posterior, and left lateral positions.3
Fragmentation of the connective tissue supporting the cushions leads to their descent. This occurs with age and the passage of hard stools, which produce a shear force on the framework. Straining produces an increase in venous pressure and engorgement. The prolapsed cushion has an impaired venous return, which results in dilation of the plexus and venous stasis. Inflammation occurs with erosion of the cushion's epithelium, resulting in bleeding.
Haemorrhoids result from the pathological changes in prolapsed anal cushions. This mechanism was proposed as the theory of sliding anal lining3 and has superseded notions that piles were a form of varicose veins.
Classification
Internal haemorrhoids originate from the internal haemorrhoidal venous plexus above the dentate line; external haemorrhoids originate from the external plexus below the dentate line. This line lies at 2 cm from the anal verge and demarcates the transition from the upper anal canal, lined with columnar epithelium, and the lower anal canal, lined with sensate squamous epithelium. Internal haemorrhoids may be classified according to the degree of prolapse, although this may not reflect the severity of a patient's symptoms. First degree haemorrhoids bleed but do not prolapse. Second degree haemorrhoids prolapse on straining and reduce spontaneously. Third degree haemorrhoids prolapse on straining and require manual reduction. Fourth degree haemorrhoids are prolapsed and incarcerated.
Presentation and diagnosis
Symptoms vary with conditions such as pregnancy, repeated straining, or changes in diet or work patterns. Sufferers may undergo periods of remission and relapse or heightened awareness of symptoms.
Haemorrhoidal bleeding is bright red and usually noticed on wiping or in the toilet bowl. Prolapse occurs with a bowel movement and is associated with an uncomfortable sensation of fullness and incomplete evacuation; patients complain of a lump at the anal verge. Soiling may occur in third and fourth degree haemorrhoids as a result of impaired continence or production of mucus discharge. Discharge can cause perianal irritation and itching.
Fourth degree haemorrhoids may become “strangulated” and present with acute severe pain. Progressive venous engorgement and incarceration of the acutely inflamed haemorrhoid leads to thrombosis and infarction (fig 2).
Fig 2.
Thrombosed haemorrhoid
Assessment should include anoscopy and a digital examination in the left lateral position. The perianal area should be inspected for the presence of skin tags, fissures, fistulae, polyps, or tumours. Prolapsing haemorrhoids may appear at the anal verge on straining. The haemorrhoidal cushions can be viewed by using the anoscope in the left lateral, right anterior, and right posterior positions (3 o'clock, 7 o'clock, 11 o'clock positions). Haemorrhoidal size, severity of inflammation, and bleeding should be assessed.
Treatment will be guided by degree and severity of symptoms. Further evaluation of rectal bleeding is prudent in patients with alteration of bowel habit, blood mixed with stool, or with risk factors for colorectal cancer.
Conservative treatment
Dietary and lifestyle modification
Increasing intake of fibre is useful for softening motions, relieving constipation, and thus reducing straining. Fibre supplementation has been shown to reduce episodes of bleeding and discomfort in patients with internal haemorrhoids, but it does not improve the degree of prolapse. Fibre supplements can relieve the symptoms of non-prolapsing haemorrhoids, but it may take six weeks for a significant improvement.4 A high fibre diet is recommended in patients with haemorrhoidal symptoms and should be initiated by the general practitioner. Lifestyle advice on avoiding straining and reading on the toilet should be emphasised. Non-prolapsing haemorrhoids can be managed adequately in primary care with these measures.
Medical treatment
A range of ointments is available that contain local anaesthetics, mild astringents, or steroids. These agents may be used to provide short term relief from discomfort, but there is a lack of evidence to support their widespread use. They do not affect the underlying pathological changes in the anal cushions. Continuous application can cause eczema and sensitisation of the anoderm; rectal absorption can lead to systemic side effects.
Dietary supplementation with micronised semi-synthetic flavonoids is a common alternative treatment that is popular in continental Europe and the Far East. These drugs act to improve venous tone and inhibit the release of prostaglandins. As an adjunct, their use has been shown to reduce acute symptoms and secondary haemorrhage after haemorrhoidectomy.5
Outpatient treatment
Interventional procedures are performed in clinic to treat first degree haemorrhoids that do not respond to dietary modification as well as second and third degree haemorrhoids. Treatment is directed at the asensate origin of the haemorrhoid lying above the dentate line. If performed correctly these procedures should not be painful.
Rubber band ligation
The technique was originally described by Barron in 1963 and is the most commonly used outpatient treatment. Anoscopy is performed to identify the haemorrhoid's origin, which is grasped by using a forceps or suction device. A band is then applied at its base. The strangulated haemorrhoid becomes necrotic and sloughs off, while the underlying tissue undergoes fixation by fibrotic wound healing.
If the procedure is well tolerated up to three piles can be banded at one visit. This increases the risk of discomfort (29% in multiple banding versus 4.5% in single banding), vasovagal symptoms (5.2% in multiple bandings versus 0% in single bandings), and urinary symptoms (12.3% in multiple bandings versus 0% in single bandings).6 Multiple banding does not increase the risk of major complications. Injection of a local anaesthetic does not reduce the discomfort associated with multiple banding.7 If application of the first band causes discomfort then repeat sessions of single banding are advised.
In a study of 512 patients, major complications including urinary retention, rectal bleeding, pelvic sepsis, and perianal abscess occurred in 2.5% (13 patients) of procedures and required admission to hospital. Minor complications including haemorrhoid thrombosis, band displacement, mild bleeding, and formation of mucosal ulcers occurred in 4.6% (24 patients).8
Band ligation is the most effective outpatient procedure for haemorrhoids,9 providing a cure in 79% of patients with first to third degree haemorrhoids. Eighteen per cent of patients have a relapse requiring repeat banding, and 2.1% fail to respond.10 The addition of fibre supplements will increase the long term cure rate after banding.11
Injection sclerotherapy
Injection sclerotherapy is an alternative to band ligation in first and second degree haemorrhoids. Injection of phenol in oil into the pedicle leads to tissue necrosis. Rare complications include pelvic infection and impotence as a result of incorrectly sited injections. Sclerotherapy may provide a short term benefit, but long term follow up shows sustained improvements in only 28% of patients.12 After six months outcome after injection sclerotherapy is comparable to treatment with fibre supplementation alone in bleeding haemorrhoids.13
Surgery
Haemorrhoidectomy
Surgery is advised for symptomatic third degree haemorrhoids not responding to banding and for fourth degree haemorrhoids.9 Less than 10% of patients referred for specialist treatment will require surgery.14 Only symptomatic haemorrhoidal tissue should be excised (“limited haemorrhoidectomy”).15 This conserves the sensory anoderm for continence and decreases postoperative pain and anal stenosis.
In the United Kingdom the Milligan-Morgan haemorrhoidectomy is the most popular technique. This entails grasping and everting the haemorrhoid, then dissecting it off the anal sphincter. The vascular pedicle is ligated, and the wounds are left open to granulate, separated by bridges of skin and mucosa. In the United States the Ferguson haemorrhoidectomy is more popular. The haemorrhoid is exposed in the anoscope, and excision and ligation are performed in its anatomical position. The wound is closed with a continuous suture. Both methods are effective forms of treatment; in theory wound closure should offer faster healing, but this has not been shown consistently. Wound dehiscence after excision of three piles prolongs healing after closed surgery (6.9 weeks in closed operation versus 4.9 weeks in open operation).16
Traditionally patients would stay in hospital after surgery until their first postoperative bowel motion. Studies have shown that day case haemorrhoidectomy is feasible in 82% of selected patients and resulted in a high degree of satisfaction among patients.17 This requires a standardised protocol of education for patients in lowering the expectation of pain and a preoperative local anaesthetic block to reduce immediate postoperative pain. Laxatives will reduce pain during the first postoperative motion, and restricting perioperative intravenous fluid will minimise the risk of urinary retention. Successful day surgery is dependent on adequate community nursing, to encourage the appropriate use of analgesics and reassure patients; up to nine home visits may be required. The addition of prophylactic metronidazole reduces pain and convalescence after day surgery and increases patients' satisfaction.18 Surgical complications include urinary retention, secondary haemorrhage, anal stricture, infection, and impairment of continence. Some 5-10% of patients undergoing day case haemorrhoidectomy require readmission. Despite successful trials only 16% of haemorrhoidectomies in 2001-2 were performed as day case procedures.19
Stapled haemorrhoidopexy
In 1998 Longo presented the procedure for prolapsing haemorrhoids (PPH), stapled haemorrhoidopexy, as a new treatment.20 A circular stapling gun is used to excise a doughnut of mucosa from the upper anal canal and lift the haemorrhoidal cushions back within the canal. As this procedure avoids a cutaneous incision it was assumed to cause less postoperative pain and a faster recovery than conventional excision.
Randomised controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy are listed in the table. Evidence shows that stapled haemorrhoidopexy is a less painful procedure, with a shorter inpatient stay and faster return to work. In trials of day surgery stapled haemorrhoidopexy is a feasible procedure but does not show a significantly shorter convalescence compared with conventional haemorrhoidectomy. Two trials report a notably higher recurrence rate with stapled haemorrhoidopexy. Reports of persistent postoperative pain and faecal urgency in one trial could not be accounted for by surgical technique, endoanal ultrasound findings, or anorectal manometry.21 In addition pelvic sepsis and rectal perforation are rare but disastrous potential complications.
Table 1.
Randomised controlled trials comparing the procedure for prolapsing haemorrhoids and conventional haemorrhoidectomy
|
No of patients |
Clinical follow up |
Inpatient stay (days) |
Return to work (days) |
No of patients with recurrent prolapse |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Country | SH | CH | SH | CH | SH | CH | SH | CH | SH | CH |
|
Stapled v diathermy |
|||||||||||
| Cheetham et al, 2003w1 |
United Kingdom |
15 |
16 |
Median 8 months |
Trial of day surgery |
Median 10 |
Median 14 |
2 |
1 |
||
| Kairaluoma et al, 2003w2 |
Finland |
30 |
30 |
1 year |
Trial of day surgery |
Median 8 |
Median 14 |
5 |
0* |
||
| Ortiz et al, 2002w3 |
Spain |
27 |
28 |
Mean 15.9 months |
Mean 15.2 months |
NA |
NA |
Mean 3.3 |
Mean 3.8 |
7 |
0* |
| Rowsell et al, 2000w4 |
United Kingdom |
11 |
11 |
6 weeks |
Mean 1.09 |
Mean 2.82* |
Mean 8.1 |
Mean 16.9* |
NA |
NA |
|
| Ho et al, 2000w5 |
Singapore |
57 |
62 |
Mean 19.2 weeks |
Mean 18.9 weeks |
Mean 2.1 |
Mean 2 |
Mean 17.1 |
Mean 22.9* |
NA |
NA |
|
Stapled v Milligan-Morgan |
|||||||||||
| Palimento et al, 2003w6 |
Italy |
37 |
37 |
6 months |
NA |
NA |
Median 28 |
Median 34 |
NA |
NA |
|
| Smyth et al, 2003w7 (late follow up of trial by Mehigan et al, 2000w12) |
United Kingdom |
20 |
16 |
Mean 37 months |
0 |
0 |
|||||
| Brown et al, 2001w8 |
Singapore |
15 |
15 |
6 weeks |
Median 2 |
Median 2 |
NA |
NA |
0 |
0 |
|
| Ganio et al, 2001w9 |
Italy |
50 |
50 |
Mean 16 months |
Median 1 |
Median 2* |
Median 5 |
Median 13* |
3 |
2 |
|
| Shalaby and Desoky, 2001w10 |
Egypt |
100 |
100 |
95% at 1 year |
80% at 1 year |
Mean 1.1 |
Mean 2.2* |
Mean 8.2 |
Mean 53.9* |
1 |
2 |
| Pavlidis et al, 2001w11 |
Greece |
40 |
40 |
3 months |
Mean 1.7 |
Mean 3.2* |
NA |
NA |
0 |
0 |
|
| Mehigan et al, 2000w12 |
United Kingdom |
20 |
20 |
Median 136 days |
Median 125 days |
Median 1 |
Median 1 |
Median 17 |
Median 34* |
See Smyth et alw7 |
See Smyth et alw7 |
| Wilson et al, 2002w13 |
United Kingdom |
59** |
30 |
6-8 weeks |
Median 1 |
Median 1.9 |
14 (Ethicon instrument) |
18* |
NA |
NA |
|
|
Stapled v Ferguson |
|||||||||||
| Correa-Rovelo et al, 2002w14 |
Mexico |
42 |
42 |
74% at range 7-14 months |
67% at range 7-14 months |
NA |
NA |
Mean 6.1 |
Mean 15.2 |
1 |
0 |
| Hetzer et al, 2002w15 |
Switzerland |
20 |
20 |
1 year |
Mean 2.4 |
Mean 2.1 |
NA |
NA |
1 |
1 |
|
|
Stapled v hospital Leopold Bellan procedure |
|||||||||||
| Boccasanta et al, 2002w16 | Italy | 40 | 40 | Mean 20 months | Mean 20 months | Mean 2 | Mean 3* | 8 | 15* | 0 | 0 |
SH=stapled haemorrhoidopexy. CH=conventional haemorrhoidectomy. NA=not available.
Statistically significant result.
27 Autosuture/32 Ethicon stapled haemorrhoidopexy.
Additional educational resources
Review articles
Loder PB, Kamm MA, Nicholls RJ, Phillips RK. Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg 1994;81: 946-54.
Corman ML, Gravie JF, Hager T, Loudon MA, Mascagni D, Nystrom PO, et al. Stapled haemorrhoidopexy: a consensus position paper by an international working party—indications, contra-indications and technique. Colorectal Dis 2003;5: 304-10.
Guy RJ, Seow-Choen F. Septic complications after treatment of haemorrhoids. Br J Surg 2003;90: 147-5612555289.
Websites
American Society of Colon and Rectal Surgeons (www.fascrs.org/coresubjects/2001/cataldo.html)—information from a keynote lecture aimed at doctors
Association of Coloproctology of Great Britain and Ireland (www.acpgbi.org.uk/documents/consensusPPH.doc)—consensus statement on stapled haemorrhoidopexy
Information for patients
American Gastroenterological Association (www.gastro.org/public/brochures/hemorrhoids.html)—brochure for patients Prodigy (www.prodigy.nhs.uk/ClinicalGuidance/ReleasedGuidance/webBrowser/pils/PL77.htm)—leaflet with validated information for patients Merck Manual of Diagnosis and Therapy (www.merck.com/pubs/mmanual/section3/chapter35/35b.htm)—article on haemorrhoids
Summary points
Symptomatic haemorrhoids result from the fragmentation, descent, and engorgement of the anal cushions; these fibrovascular structures have a role in maintaining continence
Classification is based on the degree of prolapse and reducibility into the anal canal but may not reflect the severity of symptoms
Haemorrhoidal symptoms are very common and may mask symptoms of colorectal malignancy or inflammatory disease
Rubber band ligation augmented with a high fibre diet is the most effective outpatient treatment for symptomatic haemorrhoids
Limited open haemorrhoidectomy can be performed successfully as a day case procedure and is the gold standard treatment
Stapled haemorrhoidopexy requires further long term evaluation. Although it is less painful than haemorrhoidectomy, it does not seem to be as effective
Surgeons require formal training and experience to perform the procedure independently. In patients seeking a less painful but less effective alternative to conventional haemorrhoidectomy it may be indicated for second and third degree haemorrhoids that do not respond to banding and fourth degree haemorrhoids that are reducible under anaesthetic.22
Emergency haemorrhoidectomy
Acutely strangulated haemorrhoids occur as a result of thrombus formation resulting in gross swelling, irreducible prolapse, and severe pain. Emergency debridement is indicated and provides rapid pain relief and recovery. This has a higher early complication rate compared with elective surgery; septic complications are, however, not increased.23
Conditions requiring modified treatment
Crohn's disease
Caution has to be exerted so as not to confuse other manifestations of Crohn's with haemorrhoids. Interventional treatments should be reserved until perianal sepsis and inflammation are well controlled. In general haemorrhoid surgery should be avoided and performed only on a selective basis with antibiotic cover.
HIV infection
Conservative treatment is preferable because of the risk of septic complications after surgery, and other causes of perianal symptoms should be excluded. Patients with asymptomatic HIV infection may be treated safely and successfully by band ligation.24 There is a risk of delayed wound healing after haemorrhoidectomy in HIV-positive patients which is higher for patients with AIDS.25
Pregnancy
Symptomatic haemorrhoids are common as a result of hormonal changes and straining associated with constipation. Haemorrhoids should be managed conservatively, using laxatives and dietary fibre. Surgery for intractable disease should be delayed until the fetus is viable. Surgical excision of symptomatic tissue at this stage may be performed safely under local anaesthesia.26
Supplementary Material
Contributors: JHS wrote the section on surgery, and PJN wrote the rest of the article. PJN is the guarantor.
Competing interests: None declared.
 Extra references w1-w16 appear on bmj.com
Extra references w1-w16 appear on bmj.com
References
- 1.Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology 1990;98: 380-6. [DOI] [PubMed] [Google Scholar]
- 2.Gazet JC, Redding W, Rickett JW. The prevalence of haemorrhoids. A preliminary survey. Proc R Soc Med 1970;63(suppl): S78-80. [PMC free article] [PubMed] [Google Scholar]
- 3.Thomson WH. The nature of haemorrhoids. Br J Surg 1975;62: 542-52. [DOI] [PubMed] [Google Scholar]
- 4.Moesgaard F, Nielsen ML, Hansen JB, Knudsen JT. High-fiber diet reduces bleeding and pain in patients with hemorrhoids: a double-blind trial of Vi-Siblin. Dis Colon Rectum 1982;25: 454-6. [DOI] [PubMed] [Google Scholar]
- 5.Ho YH, Foo CL, Seow-Choen F, Goh HS. Prospective randomized controlled trial of a micronized flavonidic fraction to reduce bleeding after haemorrhoidectomy. Br J Surg 1995;82: 1034-5. [DOI] [PubMed] [Google Scholar]
- 6.Lee HH, Spencer RJ, Beart RW, Jr. Multiple hemorrhoidal bandings in a single session. Dis Colon Rectum 1994;37: 37-41. [DOI] [PubMed] [Google Scholar]
- 7.Law WL, Chu KW. Triple rubber band ligation for hemorrhoids: prospective, randomized trial of use of local anesthetic injection. Dis Colon Rectum 1999;42: 363-6. [DOI] [PubMed] [Google Scholar]
- 8.Bat L, Melzer E, Koler M, Dreznick Z, Shemesh E. Complications of rubber band ligation of symptomatic internal hemorrhoids. Dis Colon Rectum 1993;36: 287-90. [DOI] [PubMed] [Google Scholar]
- 9.MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg 1997;40: 14-7. [PMC free article] [PubMed] [Google Scholar]
- 10.Bayer I, Myslovaty B, Picovsky BM. Rubber band ligation of hemorrhoids. Convenient and economic treatment. J Clin Gastroenterol 1996;23: 50-2. [DOI] [PubMed] [Google Scholar]
- 11.Jensen SL, Harling H, Tange G, Shokouh-Amiri MH, Nielsen OV. Maintenance bran therapy for prevention of symptoms after rubber band ligation of third-degree haemorrhoids. Acta Chir Scand 1988;154: 395-8. [PubMed] [Google Scholar]
- 12.Santos G, Novell JR, Khoury G, Winslet MC, Lewis AA. Long-term results of large-dose, single-session phenol injection sclerotherapy for hemorrhoids. Dis Colon Rectum 1993;36: 958-61. [DOI] [PubMed] [Google Scholar]
- 13.Senapati A, Nicholls RJ. A randomised trial to compare the results of injection sclerotherapy with a bulk laxative alone in the treatment of bleeding haemorrhoids. Int J Colorectal Dis 1988;3: 124-6. [DOI] [PubMed] [Google Scholar]
- 14.Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum 1992;35: 477-81. [DOI] [PubMed] [Google Scholar]
- 15.Hayssen TK, Luchtefeld MA, Senagore AJ. Limited hemorrhoidectomy: results and long-term follow-up. Dis Colon Rectum 1999;42: 909-14; discussion 914-5. [DOI] [PubMed] [Google Scholar]
- 16.Ho YH, Seow-Choen F, Tan M, Leong AF. Randomized controlled trial of open and closed haemorrhoidectomy. Br J Surg 1997;84: 1729-30. [PubMed] [Google Scholar]
- 17.Hunt L, Luck AJ, Rudkin G, Hewett PJ. Day-case haemorrhoidectomy. Br J Surg 1999;86: 255-8. [DOI] [PubMed] [Google Scholar]
- 18.Carapeti EA, Kamm MA, McDonald PJ, Phillips RK. Double-blind randomised controlled trial of effect of metronidazole on pain after day-case haemorrhoidectomy. Lancet 1998;351: 169-72. [DOI] [PubMed] [Google Scholar]
- 19.Department of Health. Hospital episode statistics. London: Department of Health, 2001 2000.
- 20.Longo A. Treatment of haemorrhoids disease by reduction of mucosa and haemorrhoidal prolapse with a circular suturing device: a new procedure. In: 6th World Congress of Endoscopic Surgery. Rome, 3-6 June 1998.
- 21.Cheetham MJ, Mortensen NJ, Nystrom PO, Kamm MA, Phillips RK. Persistent pain and faecal urgency after stapled haemorrhoidectomy. Lancet 2000;356: 730-3. [DOI] [PubMed] [Google Scholar]
- 22.Corman ML, Gravie JF, Hager T, Loudon MA, Mascagni D, Nystrom PO, et al. Stapled haemorrhoidopexy: a consensus position paper by an international working party—indications, contra-indications and technique. Colorectal Dis 2003;5: 304-10. [DOI] [PubMed] [Google Scholar]
- 23.Ceulemans R, Creve U, Van Hee R, Martens C, Wuyts FL. Benefit of emergency haemorrhoidectomy: a comparison with results after elective operations. Eur J Surg 2000;166: 808-12; discussion 813. [DOI] [PubMed] [Google Scholar]
- 24.Moore BA, Fleshner PR. Rubber band ligation for hemorrhoidal disease can be safely performed in select HIV-positive patients. Dis Colon Rectum 2001;44: 1079-82. [DOI] [PubMed] [Google Scholar]
- 25.Morandi E, Merlini D, Salvaggio A, Foschi D, Trabucchi E. Prospective study of healing time after hemorrhoidectomy: influence of HIV infection, acquired immunodeficiency syndrome, and anal wound infection. Dis Colon Rectum 1999;42: 1140-4. [DOI] [PubMed] [Google Scholar]
- 26.Hulme-Moir M, Bartolo DC. Hemorrhoids. Gastroenterol Clin North Am 2001;30: 183-97. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.