Childhood blindness is a priority of “Vision 2020—the Right to Sight,” a global initiative for the elimination of avoidable blindness (www.v2020.org), although only 1.4m blind children are included in the worldwide total of 45m blind people.1,2 There are several reasons for this. Blind children have a lifetime of blindness ahead, which affects their opportunities for education, employment, and earning potential. Early onset blindness adversely affects psychomotor, social, and emotional development. Blind children have a higher death rate than their sighted counterparts. An estimated 500 000 children become blind each year, but in developing countries up to 60% are thought to die within a year of becoming blind.2 Almost half of all blindness in children—particularly those in the poorest communities3—is due to avoidable causes that are amenable to cost effective interventions.
The prevalence of blindness is higher in developing countries because, firstly, potentially blinding conditions such as vitamin A deficiency, harmful traditional eye remedies, or cerebral malaria, which do not occur in affluent societies, are prevalent there. Secondly, preventive measures for conditions that have been controlled elsewhere such as measles, congenital rubella, or ophthalmia neonatorum are inadequate. Thirdly, facilities and skilled personnel for managing conditions needing surgery are lacking (box).4
In middle income countries the pattern of causes is mixed, with retinopathy of prematurity emerging as an important cause in Latin America and some eastern European countries.5,6 Currently unavoidable causes (the biggest group in affluent countries) include hereditary retinal dystrophies, disorders of the central nervous system, and congenital anomalies. Uncorrected refractive errors cause visual impairment and blindness in all regions, particularly myopia in south east Asia.7
Box 1 Magnitude and causes of blindness in children
The epidemiology of blindness in children reflects socioeconomic development
The prevalence and magnitude ranges from about 3/10 000 children in affluent societies (60 blind children per million total population) to 15/10 000 in the poorest communities (600 blind children per million total population)
75% of the world's blind children live in developing countries
Some 500 000 children become blind each year, most in developing countries
Blind children have a high death rate—the prevalence therefore markedly underestimates the burden2
Children younger than 5 years need targeting as this age group has the highest incidence of blindness, and early sight restoring surgery is needed to prevent amblyopia. Priorities include elimination of corneal scarring due to vitamin A deficiency, and measles (poorest communities); treatment of cataract (everywhere), screening programmes for retinopathy of prematurity (middle income countries), correction with spectacles for refractive errors (everywhere); and low vision services for children with incurable visual loss (everywhere).
About 140m children have vitamin A deficiency disorders and are at risk of blindness and increased mortality.8 Massive international and national efforts for control are in place in countries with death rates among children younger than 5 of more than 50 per 1000 live births, where vitamin A deficiency disorders are prevalent. Control encompasses promotion of breast feeding, home gardening (to increase local production of food rich in vitamin A, control of diarrhoea, fortification of food, education about nutrition, and intermittent supplementation with high dose vitamin A. Since the launch of the vitamin A global initiative in 1998 supplements are combined with immunisation. Between 1998 and 2000 about a million child deaths were prevented.9 However, the impact on blindness is more difficult to ascertain, but blind school and community studies show that corneal blindness is less common in young than in older children.10
Measles causes corneal blindness through several mechanisms, including acute vitamin A deficiency, exposure keratitis, herpes simplex keratitis, secondary infection, and harmful traditional remedies. As a result of the Expanded Programme of Immunisation, the number of cases with measles has fallen from over 4m per year in 1980 to 830 000 in 2001, and global immunisation coverage is currently 72%.11 Declining rates of measles related blindness in parallel with increasing immunisation coverage has been reported, and according to anecdotal evidence corneal ulceration after measles is now uncommon in developing countries.
The management of childhood cataract is far more complex than age related cataract and needs well trained teams at the tertiary level and long term follow up. Children with cataract need to be identified and referred promptly, and barriers overcome through health education—for example, fear that eyes are removed during surgery. In many developing countries, particularly in Africa, paediatric ophthalmology is underdeveloped, but training programmes are becoming established, particularly in India, to meet targets set by Vision 2020 of at least one trained paediatric ophthalmologist for every 50m population by 2010.2 Vision 2020 aims to reduce the global prevalence of blindness in children from the current level of 7/10 000 children to 4/10 000 by 2020. If achieved, the number of blind children would be almost halved, as the child population is projected to stabilise at 2bn over the next few years.
Excellent neonatal care can prevent retinopathy of prematurity to a large extent, but babies developing threshold disease need to be identified as treatment of this stage is highly effective at preventing visual loss.12 Screening programmes are in place in industrialised countries and are being developed in Latin America and large Asian cities.
Many children with incurable visual loss benefit from low vision services, which facilitate near vision and inclusive education. Often these services are lacking where they are most needed. Refractive errors, particularly myopia, often go undetected, and vision screening in schools with provision of affordable spectacles is another component of Vision 2020.
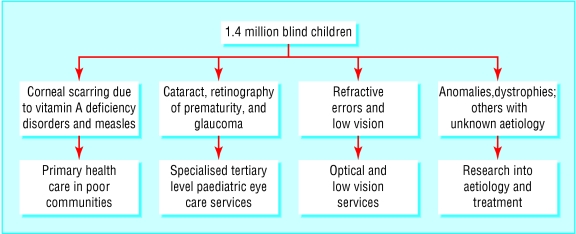
The control of blindness in children is complex, requiring community activities through to sophisticated tertiary eye care services (figure). Multidisciplinary collaboration will be required with comprehensive service delivery encompassing health promotion, specific preventive measures, optical, medical, and surgical services as well as low vision care, special education, and rehabilitation. The challenges are to ensure political commitment towards the alleviation of poverty and the development of models that are effective, replicable, sustainable, and equitable and to mobilise the additional resources required.
Figure 1.
Schematic classification of childhood blindness by control strategy
Competing interests: None declared.
References
- 1.World Health Organization. Global initiative for the elimination of avoidable blindness. Geneva: WHO, 1977. (WHO/PBL/97.61.)
- 2.World Health Organization. Preventing blindness in children: report of WHO/IAPB scientific meeting. Geneva: WHO, 2000. (WHO/PBL/00.77.)
- 3.World Bank. World development report 1993: investing in health. New York, 1993. Oxford University Press.
- 4.Gilbert C, Rahi J, Quinn G. Visual impairment and blindness in children. In: Johnson G, Minassian D, Weale W, West S, eds. Epidemiology of eye disease. 2nd ed. London: Arnold, 2003.
- 5.Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet 1997;350: 12-4. [DOI] [PubMed] [Google Scholar]
- 6.Kocur I, Kuchynka P, Rodny S, Barakova D, Schwartz EC. Causes of severe visual impairment and blindness in children attending schools for the visually handicapped in the Czech Republic. Br J Ophthalmol 2001;85: 1149-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Elimination of avoidable visual disability due to refractive errors. Geneva: WHO, 2000. (WHO/PBL/00.79.)
- 8.Sommer A, Davidson FR. Assessment and control of vitamin A deficiency: the Annecy accords. J Nutr 2002;132(9 suppl): S2845-50. [DOI] [PubMed] [Google Scholar]
- 9.Unicef. Unicef statistics. Vitamin A deficiency. www.childinfo.org/eddb/vita_a/ (accessed 8 Sep 2003).
- 10.Titiyal JS, Pal N, Murthy GVS, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol 2003;87: 941-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. WHO vaccine-preventable disease: monitoring systems. 2002 global summary. Geneva: WHO, 2002. (WHO/V&B02.20.)
- 12.Cryotherapy for Retinopathy of Prematurity Co-operative Group. Multi-center trial of cryotherapy for retinopathy of prematurity: ophthalmological outcomes at 10 years. Arch Ophthalmol 2001;119: 1, 110-1, 118. [DOI] [PubMed] [Google Scholar]