Abstract
Background
Intrauterine fetal death is a major problem in obstetrics particularly in developing countries such as Uganda. Induction of labour in cases of fetal death using the available method of oxytocin is often difficult, expensive and frustrating.
Objectives
To compare the effectiveness of vaginal misoprostol and intravenous oxytocin in induction of labour in women with intrauterine fetal death
Methods
One hundred and twenty mothers were allocated in a randomised controlled way to one of the two induction groups. Oxytocin infusion was titrated based on patient response. The starting dose was 50mcg (1/4 tablet) in misoprostol group and the dose was doubled every six hours till effective contractions were achieved. The two groups were compared for induction to delivery intervals, costs of the drugs and their safety during induction.
Results
The success rate within 48 hours of induction was 100% in the misoprostol group and 96.7% in oxytocin group. The mean induction to delivery time was significantly longer in the oxytocin group compared with the misoprostol group (23.3 versus 12.4 hours; p= 0.004). In the gestational age before 28 weeks, the induction to delivery interval in oxytocin group, was more than twice that used in misoprostol. However beyond 28 weeks, there was no significant difference.
Women with intact membranes had induction to delivery interval of 27.9 hours in the oxytocin group and 14.7 hours in the misoprostol group (p=0.002). When the membranes were ruptured, the values were 10.5 and 8.5 hours respectively (p=0.6). The induction to delivery time in cases with Bishop's score < 6 was 29.8 hours in the oxytocin group and 15.9 hours in misoprostol group (p=0.001). The corresponding values for Bishop's scores ≥ 6 were 10 and 7.9 hours respectively (p=0.6). The majority of patients in misoprostol group (62%), required less than one tablet for successful induction. Misoprostol was cheaper (0.65 USD than oxytocin (7.86 USD)
Retained placenta occurred in only 3.3% of the patients in the misoprostol group. There were no cases of ruptured uterus in both groups.
Conclusion
Intravaginal misoprostol is more effective and cheaper than intravenous oxytocin for inducing labour in patients with intrauterine fetal death.
Introduction
Intrauterine fetal death is a common obstetric problem particularly in developing countries such as Uganda. The department of Obstetrics and Gynaecology, in Mulago hospital the national referral and teaching hospital, receives most of the cases of intrauterine fetal death (IUFD). These represent about 1.3–1.67% of the 22000 deliveries conducted annually at this hospital. However, there is a shortage of human resources particularly doctors and midwives and facilities are limited.
Therefore induction of labour becomes a problem especially in fetal death which usually occurs early in pregnancy1. Myometrial responsiveness to oxytocin begins at about 20 weeks gestation and increase with advancing gestational age. Oxytocin infusion has been the method available for induction in Mulago hospital and was accepted as safe and effective when used judiciously. Unfortunately in a developing country, the cost of drugs, storage, accessibility, administration and supervision during induction makes the use of this drug difficult and frustrating. There are some prostaglandins on the market such as dinoprostone but they are quite expensive and cannot routinely be used in our hospitals.
Misoprostol, a synthetic analogue of prostaglandin E1, has been found to have several uses in Obstetrics and Gynaecology,2 and was tried in induction of labour in countries with similar settings as Uganda 3,4. However, no studies had ever been done on the effectiveness of oxytocin in induction of labour in Uganda. Misoprostol is inexpensive, stable at room temperature, easy to administer and does not require direct supervision during induction5. Unfortunately, the drug is not registered in Uganda and the purpose of this study was to compare the cost effectiveness of misoprotol with that of intravenous oxytocin with a view to introducing it in obstetric care.
Methods
The study design was a clinical trial using two known drugs and the setting was in the labour wards in Mulago hospital, the national referral hospital. The inclusion criteria included mothers who presented with confirmed intra uterine fetal death above 18 weeks of gestation and who gave informed consent.
Mothers with IUFD who had gone into labour, or had any contraindication to induction of labour or refused to participate were excluded.
A sample size of 60 in each group would be adequate to detect a difference of 7.4 minutes between oxytocin and misoprostol for the mean interval from administration of the drug to delivery, with 80% power and 95% confidence interval.
One hundred and twenty mothers with confirmed fetal death and gestation age 18–40 weeks, were recruited. They were randomly allocated to one of the two drug groups using computer-generated random numbers.
The oxytocin infusion was given in 500ml of 5% dextrose with different starting doses depending on the parity. The infusion rate was increased every 30 minutes, the maximum infusion rate was 40milli International Units per minute and if no effective contractions were noted, a new infusion with double the original dose was re-instituted. If labour was not established within 48 hours of induction, this was regarded as failed induction and the drug administration stopped. This also applied in the misoprostol group.
Misoprostol used was in 200mcg tablets which were easily cut into quadrants with a blade, each containing 50mcg. The starting dose for all mothers was 50mcg and this was doubled every 6 hours till effective contractions were established. The tablet was wetted with a drop of water for injection and inserted in the posterior vaginal fornix using a Cusco's speculum and a wooden spatula. The results were analyzed using EPI-Info version 6 statistical package. Data was summarized using means, standard deviation and frequency tables. The student's t test was used for the significance between induction to delivery intervals and a p < 0.05 was considered significant.
Results
The age was 18–40 years with mean age of 25.85 (SD 3. 6.25). Twenty six percent of the mothers were primigravida, 64.2% para 1–4, while only 10% were para 5 and above.
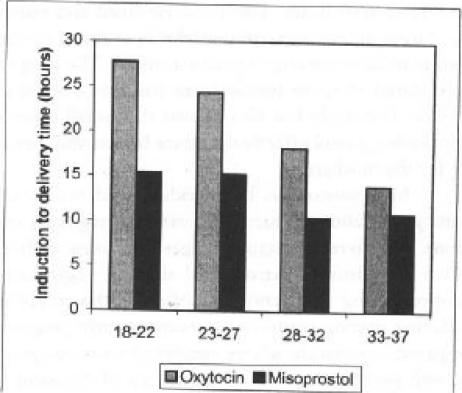
There was 100% success rate in the misoprostol group and 96.7% in the oxytocin group. The mean induction to delivery intervals were affected by the gestational age. The earlier the gestation the longer it took, using either drug, particularly before 28 weeks. However the interval in the oxytocin group was almost twice that in misoprostol group at these gestations. Beyond 33 weeks to term, there was little difference between the two drugs (See table 2).
Table 2.
Average induction to delivery intervals in hours: Mothers with Intra-uterine fetal deaths in Mulago Hospital
| Item | Oxytocin | Misprostol | P. Value |
| All patients | 23.3 | 12.4 | 0.004 |
| Intact membranes | 27.9 | 14.7 | 0.002 |
| Ruptured membranes | 10.5 | 8.5 | 0.6 (ns) |
| Bishop's score < 6 (ns) |
29.8 | 15.9 | 0.001 |
| Bishop's score ≥6 | 10.0 | 7.9 | 0.6 (ns) |
NS = P value not significant
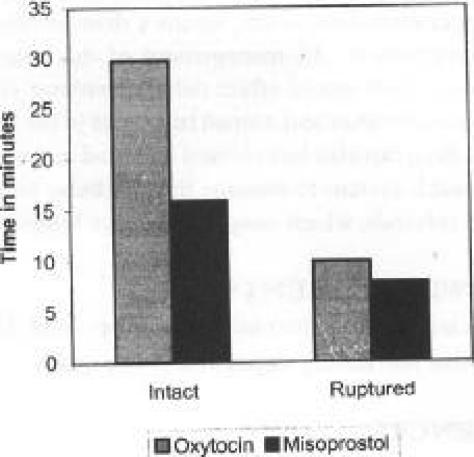
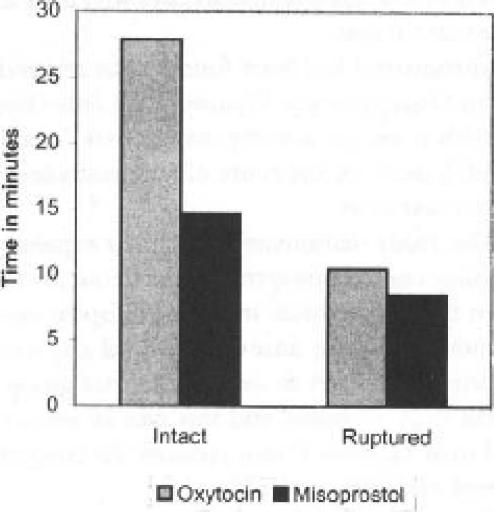
This interval was also influenced by membrane status and cervical status (Bishop's score) as shown in table 2 and figure 2.
Figure 2.
Induction-delivery time by cervical score and drug used and Bishop's score
The majority (53%) of patients presented to hospital one week or more after they realised loss of fetal movements while 17.5% reported within 24 hours of loss of fetal movements. However it was not easy to determine with certainty the actual time of fetal death. (See table 1)
Table 1.
Number of days from cessation of featal movements to induction
| Days | Method | Total | ||||
| Oxytocin | misoprostol | |||||
| ≤ 1 | 15 | 25.0% | 6 | 10.0% | 21 | 17.5% |
| 2–6 | 23 | 38.3% | 12 | 20.0% | 35 | 29.2% |
| 7–14 | 13 | 21.7% | 21 | 35.0% | 34 | 28.3% |
| ≥ 14 | 9 | 15.0% | 21 | 35.0% | 30 | 25.0% |
| Total | 60 | 100.0% | 60 | 100.0% | 120 | 100% |
The figure shows that in both ruptured and unruptured membranes, the mean time from induction to delivery was shorter in those patients induced with misoprostol. There was significant difference (p<0.002) with shorter time in the misoprostol group and longer time in oxytocin group, that is 14.7 hours and 27.9 hours respectively in the intact membranes. Where the membranes were ruptured, there was no significant difference (p=0.6) in induction to delivery time, that is 8.5 hours and 10.5 hours for the misoprostol and oxytocin group respectively.
When the cervix was unripe (Bishop's score <6), there was a significant difference (p=0.001) in the mean induction to delivery interval. This was 29.8 hours in the oxytocin group and 15.9 hours in the misoprostol group. However there was no significant difference (p=0.6) in time for Bishop's scores of ≥6. In the oxytocin group it was 10 hours while in the misoprostol group it was 7.9 hours.
The figure shows that the earlier the gestation age, the longer was the induction to delivery interval using either drug. The mean intervals were longer for oxytocin compared to misoprostol particularly before 28 weeks of gestation and beyond 33 weeks to term there was little difference.
The majority of patients required less than one tablet of misoprostol and the maximum dose of 750mcg (3 and ¼ tablets) was needed by only 3 patients. The mean cost of the drug in the misoprostol was 0.65USdollars (range 0.14–2.51USdollars) while in the oxytocin group it was 7.86 USdollars (range 3.6 – 23.9 USdollars) and the difference was statistically significant (p<0.05). There were very few complications associated with the drugs. There were no cases of uterine rupture even among patients with previous Caesarean section scars. The side effects noted were mainly nausea, vomiting, shivering and pyrexia especially with misoprostol but these were transient.
Discussion
The study has demonstrated that use of vaginal misoprostol is an efficient method of labour induction in patients with intrauterine fetal death. The costs involved and nursing time during induction were remarkably reduced as compared to induction using oxytocin infusion. The drug was easily stored at room temperature and was easy to administer. The study has also shown that small doses of vaginal misoprostol effectively induce labour and they are safe for the mothers.
Misoprostol has been widely used for cervical ripening and labour induction in various pregnancy conditions, at different gestational ages and using different routes of administration and dosing regimens6. Misoprostol has dual action of softening the cervix and producing uterine contractions even in early pregnancy compared to oxytocin whose sensitivity increases gradually with gestation age. This makes use of oxytocin for induction of labour before 28 weeks difficult7. Therefore it would necessitate several attempts at induction, which is costly and frustrating.
Misoprostol is absorbed rapidly when administered orally, vaginally, rectally or intracervically. The vaginal route is advantageous because peak levels are reached slowly and sustained for long and this is associated with fewer gastrointestinal side effects8,9.
Induction of labour in a woman with an unripe cervix often results in prolonged and difficult labour. This may result in failed induction or require use of another oxytocic agent or delivery by Caesarean section. However misoprostol has been found to be effective in women with unfavorable cervices compared with oxytocin. This was similar to other randomized clinical trials addressing the efficacy of misoprostol as a cervical ripening agent11.
The membrane status at the beginning of induction influences the outcome of induction. Labour is usually longer in cases of intact membranes compared to ruptured ones. Several studies have been done in cases of premature rupture of membranes and labour induction11–14. In this study, it was noted that the misoprostol group had shorter labour even in cases of intact membranes as compared to the oxytocin group.
Among patients with previous Caesarean deliveries, the incidence of uterine rupture is greater than in spontaneous labour cases. There has been considerable concern about association between misoprostol induction and previous uterine scars15. This is even worse in countries where resources for monitoring patients are scarce. Many studies were tried using misoprostol in induction of labour in patients with previous Caesarean scars and analysis of twelve studies,14,15 found the incidence of uterine rupture to be less than 6%. However, there were no cases of uterine rupture in the current study. Therefore vaginal misoprostol might be a potential safe alternative for induction in previous caesarean deliveries who have an indication for trial of scar.
Misoprostol has been found to be relatively safe in its use in Obstetrics and Gynaecology. Side effects associated with it are gastrointestinal and are usually dose related and depend on the route of administration. However they are transient.
The study demonstrated that the expense of induction using vaginal misoprostol was about 25–36 times lower than that of oxytocin infusion. Hospital expenses, nursing and monitoring time and hospital stay were less. The majority of women in the misoprostol group delivered in less than 12 hours and this was an advantage to them and their families. It also reduced the congestion in labour ward and lying-in wards.
The administration of oxytocin using an infusion pump easily allows precise control of the flow rate and accurate minute to minute control. However this was not used in the study because they are expensive and not easily accessible. Therefore all the titration was done manually with a midwife at the bedside. The cost of oxytocin infusion was not as high as in other studies16.
Conclusion
Misoprostol is cheaper and more effective than oxytocin in cervical ripening and induction of labour in patients with intrauterine fetal death. Therefore the use of misoprostol in Uganda, for induction of labour particularly in intrauterine fetal death, means a dramatic change and improvement in the management of this obstetric complication. This would effect delivery without straining the limited facilities and human resources in the health units. The drug can also be accessed and tried in the lower levels of health system to manage the condition to avoid delays and referrals, which congest the large hospitals.
Fig. 1.
Induction-delivery interval by membrane status and drug
Figure 3.
Induction-delivery interval by gestation age and drug used
Table 3.
The dosages of misoprostol used and their costs
| Dose (mcg) | Number of women | Cost (US dollars) |
| 50 | 27 (44%) | 0.14 |
| 100 | 6 (10%) | 0.28 |
| 150 | 5 (8%) | 0.42 |
| 250 | 10 (17%) | 0.70 |
| 350 | 4 (7%) | 0.98 |
| 550 | 5 (8%) | 1.26 |
| 750 | 3 (6%) | 2.51 |
Acknowledgements
To Associate Prof. Florence Mirembe and Dr. J. Byamugisha for kindly supervising the study.
References
- 1.Bugalho A, Bergstrom S. Induction of labour by vaginal misoprostol. Acta Obstet Gynecol Scand. 1999;78:653–654. [PubMed] [Google Scholar]
- 2.Bugalho A, Machungo F, Bique C. Induction of labour with intravaginal misoprostol in intrauterine fetal death. Am J Obstet Gynecol. 1994;171:538–541. doi: 10.1016/0002-9378(94)90295-x. [DOI] [PubMed] [Google Scholar]
- 3.Choy-Hee I, Raynor BD. Misoprostol in induction of labour in women with prior Caesarean section. Am J Obstet Gynecol. 2000;182:S15. doi: 10.1067/mob.2001.115177. [DOI] [PubMed] [Google Scholar]
- 4.Cunha M, Bugalho A, Bergstrom S, et al. Induction of labour by vaginal misoprostol in patients with previous caesarean delivery. Acta Obstet Gynecol Scand. 1999;78:653–654. [PubMed] [Google Scholar]
- 5.Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93:275–280. doi: 10.1016/s0029-7844(98)00436-0. [DOI] [PubMed] [Google Scholar]
- 6.Fernando A. Pharmacology of oxytocin and prostaglandins. Clin Obstet Gynecol. 2000;43(3):453–468. doi: 10.1097/00003081-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Hofmeyr GJ. Vaginal misoprostol for cervical ripening and labour induction in late pregnancy. The Cochrane library issue. 1999;2:1–18. [Google Scholar]
- 8.Jing S. Use of misoprostol in Obstetrics and Gynaecology. Obstet Gynecol Surv. 2000;55(8):503–509. doi: 10.1097/00006254-200008000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Ngai SW, Chan YM, Lam WS, et al. Labour characteristics and uterine activity: Misoprostol compared with oxytocin at term with prelabor rupture of membranes. Br J Obstet Gynecol. 2000;107(2):222–227. doi: 10.1111/j.1471-0528.2000.tb11693.x. [DOI] [PubMed] [Google Scholar]
- 10.Sanchez-Ramos L, Chen AH, Kaunitz AM, et al. Labour induction with intravaginal misoprostol in term premature rupture of membranes: A randomized study. Obstet Gynecol. 1997;89:909–912. doi: 10.1016/s0029-7844(97)00113-0. [DOI] [PubMed] [Google Scholar]
- 11.Sanchez-Ramos L, Kaunitz AM, Delke, et al. Labour induction with the PG. E1 methyl analogue misoprostol versus oxytocin. Obstet Gynecol. 1993;81:332–336. [PubMed] [Google Scholar]
- 12.Stubbs TM. Oxytocin for labour induction. Clin Obstet Gynecol. 2000;43(3):489–493. doi: 10.1097/00003081-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Thomas N, Longo SA, Rumney PJ, et al. Intravaginal misoprostol in prelabor rupture of membranes. Am J Obstet Gynecol. 2000;182:S136. [Google Scholar]
- 14.Thompson AJ. Elective induction of labour. Why, when and why? The Obstetrician and Gynaecologist. 1999 Jul;1:20–25. [Google Scholar]
- 15.Wing DA. Labour induction with misoprostol. Am J Obstet Gynecol. 1999;181:339–345. doi: 10.1016/s0002-9378(99)70558-2. [DOI] [PubMed] [Google Scholar]
- 16.Zieman M, Fong SK, Benowitz NL, et al. Absorption kinetics of misoprostol with oral or vaginal administration. Obstet Gynecol. 1997;90:88–92. doi: 10.1016/S0029-7844(97)00111-7. [DOI] [PubMed] [Google Scholar]