Abstract
Background
Refractive errors are a known cause of visual impairment and may cause blindness worldwide. In children, refractive errors may prevent those afflicted from progressing with their studies. In Uganda, like in many developing countries, there is no established vision-screening programme for children on commencement of school, such that those with early onset of such errors will have many years of poor vision. Over all, there is limited information on refractive errors among children in Africa.
Objective
To determine the prevalence of refractive errors among school children attending lower primary in Kampala district; the frequency of the various types of refractive errors, and their relationship to sexuality and ethnicity.
Design
A cross-sectional descriptive study.
Setting
Kampala district., Uganda
Patients
A total of 623 children aged between 6 and 9 years had a visual acuity testing done at school using the same protocol; of these 301 (48.3%) were boys and 322 (51.7%) girls.
Results
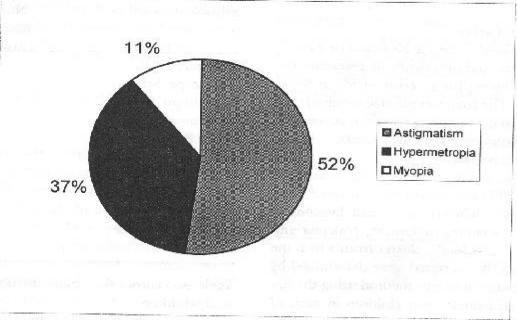
Seventy-three children had a significant refractive error of ±0.50 or worse in one or both eyes, giving a prevalence of 11.6% and the commonest single refractive error was astigmatism which accounted for 52% of all errors. This was followed by hypermetropia, and myopia was the least common.
Conclusion
Significant refractive errors occur among primary school children aged 6 to 9 years at a prevalence of approximately 12%. Therefore, there is a need to have regular and simple vision testing in primary school children at least at the commencement of school so as to defect those who may suffer from these disabilities.
Introduction
Children with learning and behavioral disabilities are often brought to an ophthalmologist for evaluation to see whether an ocular disorder is responsible for the disability. However, children who get such an opportunity are few, and only those whose disabilities are so severe as to be noticed by the parent or the teacher that are brought to anophthalmologist.
Very few schools in Uganda ensure that children are screened for visual disorders or disability before joining school. The problem is further compounded by the fact that there are few eye health care workers in Uganda and these few are not equally distributed.
The presence of a significant refractive error or other eye anomaly of vision will impair the visual and learning abilities of such a child. In the Global Initiative 2020 for the elimination of avoidable blindness, refractive errors have been emphasized together with other ocular disorders such as cataracts, trachoma and onchocerciasis.1 The Refractive Error Study in Children (RESC) has been formed under this Initiative to try and assess the prevalence of refractive errors in children2.
Materials and Methods
Study design
This was a cross-sectional descriptive study in which lower primary school children were screened for refractive errors.
Inclusion criteria
Primary school children aged 6 to 9 years whose parents had endorsed informed consent by signing a consent form. The study was carried out at Makerere University, department of Ophthalmology.
Exclusion criteria
Children who were unwilling to undergo the examination due to fear, even through the parents had authorized the examination. Children who were sick or those who were on medication for some other ailment; some drugs have ocular effect.
Ethical issues
Permission to carry out this study was sought for, and obtained from, the Faculty of Medicine Research and Ethics Committee. Each participating school was visited at least two weeks before the screening day, and permission to do the study sought from the headmaster/headmistress. In all the schools permission was readily granted. A letter explaining the purpose of the intended study, and what would actually be done was attached to parental informed consent form and given to each of the lower primary school children to take to their parents. Only children who returned duly signed consent forms, and who were willing to take part were recruited. Parents who required further explanation before consenting for their children to participate in the study were invited to attend the particular school on the screening day. Only one mother turned up, and after a few questions and answer session, she consented for her daughter to participate.
Sampling and sample size
Sample size was calculated using the Kish and Leslie's formula, using the expected prevalence of refractive errors of 18.5 3, and allowing for an error of 5% at 95% confidence interval. The total sample size required was 649. This was a multistage sampling and representation in the clusters was proportional to the number of children in the sampled clusters.
A census list for all the primary schools in Kampala district for the year 2000 enrollment was obtained from the city education office. The census list had divisions of the city (Central, Kawempe, Makindye, Nakawa and Rubaga). Each division formed a cluster from which the number of children to be recruited were determined by the probability proportional to size method using the figures of enrollment of primary two children in each of the five divisions. This was the first phase of the multi-stage sampling.
The second phase was the selection of schools from each division for the study. Two schools were selected per division using simple random sampling.
The third phase was the recruitment of children aged between 6 and 9 years from each participating school. The class register was used, and systematic random sampling was done.
Data collection
Personal details of each participating child were recorded on a form, and then the child underwent a standard ophthalmic examination, and all findings recorded. Refraction was done using retinoscopy after 1% cyclopentolate eye drops had been instilled in the eyes at least half an hour previously. Only children who had a visual acuity of less than 6/6 in at least one eye underwent retinoscopy.
Data analysis
Data was entered into a computerised database-using the CDC-WHO package EPI-INFO, and results of analysis are presented in the form of tables.
Results
Six hundred and forty-nine children aged between 6 and 9 were given consent forms to take to their parents. Out of these 623 returned signed consent forms, giving a response of 96%. These 623 children were all examined.
Table one shows the number of children examined in each of the ten schools during the study period.
Table 1.
The number of children examined in each of the 10 schools in May and July 2000.
| School | Number of Children examined for refractive error |
| Makerere P/S | 56 |
| Kawempe Mbogo | 58 |
| Kyambogo P/S | 47 |
| MurchisonBay | 62 |
| Police P/S | 81 |
| Bbunga | 58 |
| Kitebi P/S | 93 |
| Namungoona | 48 |
| Nakivubo | 73 |
| KCC Kamwokya | 49 |
| Total | 623 |
Table two shows the ethnic distribution among the 623 study children.
Table 2.
The ethnic distribution among the 623 children
| Tribe | Absolute no. | Relative freq.(%) |
| Acholi | 20 | 3.2 |
| Alur | 12 | 1.9 |
| Adhola | 17 | 2.7 |
| Baganda | 360 | 57.8 |
| Bagwere | 8 | 1.3 |
| Bakiga | 17 | 2.7 |
| Banyankole | 30 | 4.8 |
| Banyarwanda | 7 | 1.1 |
| Banyoro | 11 | 1.8 |
| Basoga | 30 | 4.8 |
| Batoro | 17 | 2.7 |
| Langi | 21 | 3.4 |
| Lugbara | 15 | 2.4 |
| Madi | 4 | 0.2 |
| Bagisu | 10 | 1.6 |
| Itesot | 44 | 7.1 |
| Total | 623 | 100.0 |
None of the children in the study had ever had correction for a refractive error; therefore none was wearing spectacles.
Seventy-five children had a visual acuity of 6/12 or worse in at least one eye. Five of these had a squint; one had a shrunken right eyeball with a 100% loss of vision in that eye. Seventy three children had a visual acuity of 6/12 or worse in one or both eyes, giving a refractive error prevalence of 11.6%
The commonest refractive error was astigmatism with 38 (52%) children, followed by hypermetropia with 27 (37%) children, and myopia with 8 (11%) children. (See figure 1).
Figure 1.
Frequency of the types of refractive errors, Kampala in May and July 2000
Table 3 shows the age distribution of the 75 children who had a visual acuity of 6/12 or worse in at least one eye. The older a child gets between the age of 6 and 9 the commoner the refractive error becomes.
Table 3.
Age distribution of the 75 children who had refraction and fundoscopy
| Age | No. | Relative Freq. (%) |
| 6 | 6 | 8.0 |
| 7 | 17 | 22.8 |
| 8 | 28 | 37.3 |
| 9 | 24 | 32.0 |
| Total | 75 | 100 |
Two children had abnormalities of the retina with juvenile macular degenerations, and early optic atrophy- respectively
Discussion
The prevalence rate of a significant refractive error of 11.6% in this study is lower than that obtained by Chen et al 4 carried out on 6 and 7 year olds, which was 18.5. This could be due to possible racial differences in the two study groups. However, the prevalence of 11.6 of this study makes interesting comparison with the studies of Proslan et al in Baltimore, USA 5, and Kazuhiro in Japan, where the respective prevalence were 8.2 and 10.4 6.
Astitmatism was the most frequent refractive error, accounting for 52% of all the errors, followed by hpermetropia, with myopia as the least frequent refractive error. These finding contrasts with results done elsewhere, for example Kalikivayi et al found that among Indian children hypermetropia was the commonest refractive error, and it accounted for 23% of all errors 7. Astigmatism was cause number two, followed by myopia. In Kazuhiro's study myopia was the commonest refractive error among Japanes children and it accounted for 58% of all errors followed by astigmatism (26%), with hypermetropia as the least common (13%). Other studies done elsewhere showed that there might be substantial variability in the relationship between refractive error and distance vision. There were patients with normal uncorrected vision but substantial refractive error, and other cases with little refractive error but reduced vision that improved with corrections 8,9,10.
Two children who had retinal abnormalities had an average visual loss of approximately 60%. They were referred to the school for children who are visually handicapped. Their Vision is most likely going to deteriorate as they grow.
This study has clearly illustrated the need to screen young children regularly or at least on first attending school. This will enable identification of those with visual disability so that corrective measures may be recommended at the earliest time possible.
References
- 1.World Health Organisations, Geneva, author. Global Initiative for the Elimination of Avoidable Blindness. Geneva: WHO/PBL/97.61; [Google Scholar]
- 2.Ande-Deminique, Leon BE Research study group, author. More Research needed to Assess the magnitude of Refractive Errors Worldwide. Journal of Community Ehe Health, Vision 2020 The Right to Sight. 2000;13(33) [PMC free article] [PubMed] [Google Scholar]
- 3.Maul E, Bairoso S, Munoz SR, Zhao J, et al. Refractive Error Study in Children: Results from La florida. Am J Ophthalmol. 2002;129(4):445–454. doi: 10.1016/s0002-9394(99)00454-7. [DOI] [PubMed] [Google Scholar]
- 4.Chen P, Chnag R, et al. Restrospective study on prevalence of Refractive Errors in 6 and 7 year old in Santa Monic, USA. Opthalmol. 1996;103:1661–1669. [Google Scholar]
- 5.Proslan M, Novak C. The Baltimore Vision Screening Project. Trop Med Int Health. 1996:314–319. [Google Scholar]
- 6.Kazuhiro H. Ophthalmol. Vol. 25. Kyoto Japan: 1978. Refractive Errors among Japanese School children XXIII Cong; pp. 1207–1211. [Google Scholar]
- 7.Kalikivayi et al., author Determination of the Prevalence of Visual Impairment due to Refractive Errors and other ocular. Diseases in Lower middle class School
- 8.Negrel AD, Naul L, pokharel GP, Zhao J, Ellwein LB. Refractive error study I children: sampling and measuring methods for a multi-county Survey. Am J Ophthalmol. 2000;129:421–426. doi: 10.1016/s0002-9394(99)00455-9. [DOI] [PubMed] [Google Scholar]
- 9.Gilbert E, Anderson L, Dandona L, Foster A. prevalence of visual impairment in children a review of available data. Ophthalmol Epidemiol. 1999;6:73–82. doi: 10.1076/opep.6.1.73.1571. [DOI] [PubMed] [Google Scholar]
- 10.Pokharel GP, Regmi G, Shrestha 8k negrel AD, Euwein LB. Prevalence of blindness and cataract surgery in Nepal. Br J Ophthalmol. 1998;82:600–605. doi: 10.1136/bjo.82.6.600. [DOI] [PMC free article] [PubMed] [Google Scholar]