Abstract
Background
About 100,000 children die annually from severe malaria in Uganda and more than 75% of health unit based deaths occur within 24 hours of admission. Most of these deaths are associated with poor resuscitation systems, delays within the units by health workers and lack of essential drugs and supplies.
Objective
To describe the manifestations and quality of care children with severe malaria receive in Mulago Hospital Paediatric emergency unit and evaluate its impact on outcome.
Methods
A cohort of 784 children with severe malaria was recruited at admission and followed up. Selected measures of quality were the exposure factor and death, the outcome measure.
Results
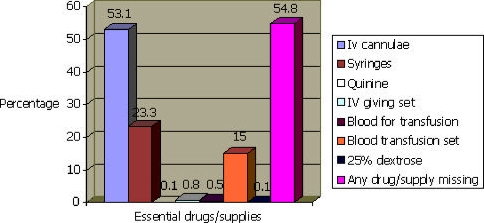
Only 22.5% of the children were brought at night. The commonest defining manifestations were severe anaemia (39.4%), respiratory distress (17.1%), multiple generalized convulsions (13.3%), hypoglycaemia (11.4%) and cerebral malaria (7.2%). Over 50% lacked an essential drug or supply needed for resuscitation and 23.4% were seen within 1 hour of arrival. Commonly lacking items were intravenous cannulae (53.1%) syringes (23.3%) and blood transfusion sets (15.0%). Children brought at night took a shorter time before being seen by a doctor (1.9 SD 2.4 vs 2.5 SD 2.0 hours, p=0.002), received the first dose of quinine earlier (4.1 SD 3.2 vs 5.2 SD 3.2 hours, p<0.0001), fewer lacked essential drugs and supplies (45% vs 57.9%, p=0.003) and fewer died (0.6% vs 3.8%, p=0.028). Children who lacked an item for resuscitation took 30 minutes longer to receive the first dose of quinine. Caretaker satisfaction was predictive of mortality in the unit.
Conclusions
Quality of care for severe malaria in Mulago paediatric emergency unit is still poor although nighttime services are comparatively better. Caretakers buy at least one resuscitation item in over 50% of cases and their level of satisfaction is predictive of mortality.
Recommendations
The unit should set targets for quality improvement to include increased staffing and supplies, a time limit within which children should be seen and measures of decongestion. Determination of blood sugar in patients with severe malaria should be made a basic requirement.
Background
Malaria continues to be a public health problem with over 1 million child deaths annually. In Uganda, 70,000 – 110,00 children die annually. 1,2 Most of these deaths are a result of severe malaria especially that which presents with altered consciousness, severe anaemia and/or respiratory distress3. A big proportion of deaths occur in health units where children are taken for treatment. Over 75% of the health unit based deaths occur within 24hours of admission and many may be preventable.4,5,6 Any attempts at reducing health unit deaths and saving children should therefore be aimed at improving the quality of care in the emergency units. Observations in many Ugandan hospitals show that unnecessary delays exist within emergency units in attending to sick children and essential resuscitation measures are often lacking. There is no systematic documentation of these problems yet addressing them may reduce mortality. This study describes the manifestations, quality of care and outcome of treatment of severe malaria in Mulago hospital Paediatric emergency unit.
Methods
Study Design
This was a cohort study. The study population was children ages 0 – 12 years presenting with severe malaria to Mulago hospital Paediatric emergency unit.
Study site
Mulago hospital is a 1500 bed National referral hospital in Uganda and a teaching hospital for Makerere University Medical School. It also serves as a district hospital for Kampala and surrounding areas. Its Paediatric emergency unit admits an average of 50 children (age 0 – 12 years) daily for over night observation and management before those who need continued care are sent to the main paediatric wards.
Inclusion criteria
Children with any of the manifestations of severe malaria using a modification of the 1990 World Health Organization (WHO) criteria for severe malaria by Marsh at el3, who were admitted to the unit during the study period and whose caretakers gave consent were included.
Exclusion criteria
Children who were found to have an additional diagnosis apart from malaria were excluded.
Sample size determination
The exposure factors were selected measures of quality that were thought to be worst during night presentation. The outcome measure was death within 24 hours of admission. Assuming a 6% case fatality among those who present during day, a relative risk of 2.0 at 95% confidence, 80% power and a ratio of day presentation to night presentation as 1.5:1, a sample of 474 children presenting during day and 316 presenting at night was planned for.
Data collection
Children with severe malaria, who fulfilled the inclusion criteria were consecutively enrolled and followed up for 24 hours unless death occurs. Upon arrival at the emergency unit, the triage nurse irrespective of the type of illness consecutively registered all sick children in the unit attendance book. The time of arrival to the unit was concurrently recorded on the child's registration card and on a nurses' record form that was handed over to the research assistant. Attending physicians recorded the time each child was seen before taking a history and performing a physical examination. A minimum package of laboratory investigations that included a blood smear for malaria parasites, haemoglobin, and blood sugar level was performed. Cerebral spinal fluid examination was done if a diagnosis of cerebral malaria was entertained. The blood films were stained with field's stain, the haemoglobin determined using Drabkins method and blood glucose determined with a glucometer (Sure Step, USA Inc). This information was recorded on case record forms. The treatment nurses then recorded the time when the first dose of quinine was given and any item required for resuscitation but was unavailable. Treatment was provided according to the hospital's guidelines (Acute care unit guidelines, un published).
Presentation between 7:00 pm and 7:00 am was considered presentation at night. After a night in the emergency unit, the outcome was documented. Some children thought by the examining doctor to have improved were discharged. The rest were transferred to the main Paediatric wards. The outcome after 24 hours was recorded for each child and the final outcome documented at discharge or death to complete the study.
Quinine, oxygen, normal saline, 5% dextrose, 25 or 50% dextrose, blood for transfusion, blood transfusion sets, intravenous cannulae, intravenous fluid giving sets, and syringes were considered the minimum drugs and supplies needed to resuscitate children presenting with severe malaria. If any item was missing in the unit and the caretaker was able to buy it from a nearby pharmacy, a prescription to this effect was made and a record taken by the study nurse. After a child had been started on intravenous quinine and stabilized, and at most within 24 hours in the unit, caretakers were asked by the research assistant to comment on the quality of care they received. Caretakers who lost children before stabilization made their comments at the time of collecting the death certificates. A caretaker was said to be satisfied with the service offered if s/he rated it as good or very good on a scale of very poor, poor, fair, good and very good.
Permission to conduct the study was sought from Makerere University Faculty of Medicine Adhoc Research Committee and informed consent was obtained from caretakers of all children before enrollment.
Data analysis
Data entry was done using Epi Data 2.1a and analyzed with SPSS 10 statistical software packages. The Chi-square test was used to test for significance of association between death within the emergency room and the presence of inadequate supplies during resuscitation. The relative risk and p value were used as measures of significance. A p value < 0.05 was considered significant. A child was said to have received quality clinical care if s/he was seen by a doctor within 1 hour of arrival, received the first dose of quinine within 2 hours, all drugs and supplies needed for emergency resuscitation were available and the caretaker was satisfied with the quality clinical care received.
Results
Demographic characteristics
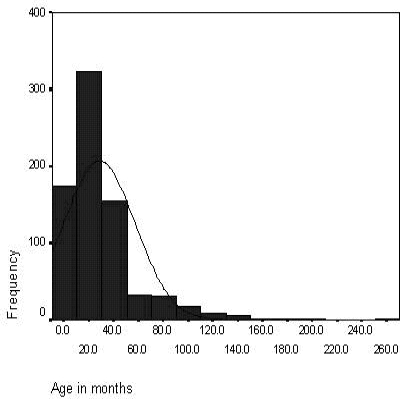
Between April 22nd to June 30th 2003, 784 children with severe malaria were admitted to the unit. Most (77.5%) were brought during day compared to only 22.5% at night. The male: female ratio was 1.2:1 with males accounting for 54.9% of the admissions. The mean age was 30.1 months and the median age 18.0 (inter quartile range 10.0 – 36.0) months. Majority of the children were less than 4 years old. (Figure I) Over 90% came from the districts of Kampala, Mukono, Wakiso, Mpigi, and Luwero, districts surrounding Kampala where Mulago is located. Most caretakers (67.7%) had attended some primary education, although only half of these had gone beyond primary four.
Figure I.
Age distribution of children with manifestations of severe malaria
Presenting symptoms
Fever, vomiting, cough and convulsions were the commonest symptoms. (Table I) Symptoms like headache and muscle aches commonly described in adults were rarely reported. Reported cases were from older children. On the other hand, diarrhoea was reported in a quarter of the children. In almost all cases, the duration of fever approximated that of the illness and this was about two and half days. Although fever, cough and vomiting were the commonest symptoms, mothers acted fast and brought the children to the unit if they had convulsions or mental confusion (Table I).
Table I.
Symptoms in children with severe malaria
| Symptoms | Percentage with symptoms symptoms (n=784) |
Mean duration of symptoms in hours (range) |
| Fever | 97.7 | 110.5 (5.0 – 720) |
| Vomiting | 65.4 | 62.1 (2.0 – 336) |
| Cough | 48.9 | 116.2 (0.5 – 720) |
| Convulsions | 37.4 | 18.6 (0.1 – 168) |
| Diarrhoea | 22.7 | 75.9 (0.5 – 434) |
| Weakness | 12.9 | 38.1 (5.0 – 168) |
| Difficult breathing | 8.9 | 47.8 (0.0 – 168) |
| Headache | 5.2 | 85.2 (16 – 336) |
| Bloody/tea colour urine | 2.7 | 33.0 (24.0 – 72) |
| Mental confusion | 2.2 | 16.6 (1.0 – 72) |
| Joint pains | 1.5 | 44.8 (18.0 – 96) |
| Muscle aches | 0.9 | 52.8 (0.0 – 96) |
Manifestations of severe malaria
Using a modification of the WHO 1990 criteria for severe malaria by Marsh at el3, the children were categorized as either having defining or supporting criteria for severe malaria. The commonest defining manifestations were severe anaemia, respiratory distress, multiple generalized convulsions, hypoglycaemia and cerebral malaria. (Table II)
Table II.
Manifestations of severe malaria in patients in Mulago Paediatric emergency unit
| Manifestations of severe malaria |
% of patients with manifestation (n = 784) |
Mortality in children who had manifestation |
Mortality in children who did not have the manifestation |
P value |
| Defining manifestations of severe malaria | ||||
| Severe anaemia (Hb < 5 g/dl) |
39.4 | 4.8 | 3.6 | 0.142 |
| Respiratory distress (tachypnoea & flaring of alae nasi, chest in drawing or deep breathing) |
17.1 | 7.8 | 2.1 | 0.003 |
| Multiple convulsions (≥2 in 24hr) |
13.3 | 7.6 | 3.1 | 0.073 |
| Hypoglycaemia (Blood sugar < 40mg/dl) |
11.4 | 7.1 | 3.2 | 0.238 |
| Cerebral malaria (BCS1 0–2) | 7.2 | 19.6 | 1.7 | < 0.0001 |
| Haemoglobinuria | 2.7 | 5.9 | 3.6 | 0.736 |
| Spontaneous bleeding | 0.3 | 0 | 3.7 | 0.940 |
| Supporting manifestations of severe malaria | ||||
| Hyperpyrexia (axillary temp > 39.5°C) |
22.5 | 4.3 | 2.8 | 0.326 |
| Impaired consciousness (BCS 3,4) |
10.3 | 11.7 | 1.9 | <0.0001 |
| Jaundice | 11.6 | 7.3 | 2.5 | 0.047 |
| Prostration (Unable to sit, stand or feed) |
10.7 | 8.3 | 3.1 | 0.125 |
| Hyperparasitaemia (Parasite density > 250,000/µl) |
8.6 | 4.6 | 2.9 | 0.682 |
The total inpatient mortality was 3.1%. Of the 23 cases of death, 5 (21.7%) occurred within 1 hour of arrival to hospital. A total of 17 deaths (73.9%) occurred in the emergency room and the remaining soon after transfer to the main Paediatric wards but all within 24 hours. Cerebral malaria accounted for 47% of these deaths. Different degrees of impairment of consciousness, respiratory distress, multiple generalized convulsions and jaundice were significantly associated with the occurrence of death. In almost all cases, the presence of any of the manifestations of severe malaria relatively increased the resulting mortality.
Although provided for in the hospitals' guidelines for the work up of children with severe malaria, the emergency unit does not routinely offer blood glucose level determination. The study therefore provided this service and was able to demonstrate hypoglycaemia in 11.4% of the children. Similarly, renal function is not routinely assessed nor urine input/output recorded for children with severe malaria. We were therefore unable to determine the prevalence of renal failure. However, 3 children definitely had renal problems. All 3 were anuric for more than 24 hours despite adequate rehydration and fluid challenge. They all regained normal urine outputs over the next 72 hours.
Care received during day and at night
Most patients were brought to the emergency unit during day and only 22.5% were brought at night. The mean distance from hospital was similar in the two groups. Altogether, 24.3% of the children were seen within 1 hour of arrival and 11.9% received their first dose of quinine within 2 hours. The time taken to see a doctor upon arrival, time to receive the first dose of quinine, presence of essential supplies and mortality were significantly better among children who presented at night when compared to day presentation. (Table III) In general, over 90% of the caretakers considered the services they received either as good or very good. The assessment of the caretakers was: very good (28.4%), good (62.9%), fair (8.4%) and poor (0.3%). These assessments were similar during day or night except all the patients who thought the services were poor came during day.
Table III.
A comparison of care received during day and at night
| Variable | Presentation at night |
Presentation during day |
P value |
| Mean distance to hospital (km) | 11.2(SD 16.8) | 11.6(SD 20.3 | 0.844 |
| Time taken to be seen by a doctor (hrs) | 1.9(SD 2.4) | 2.5(SD 2.0) | 0.002 |
| Time to receive first dose of quinine (hrs) | 4.1(SD 3.2) | 5.2(SD 3.2) | <0.001 |
| Unable to perform Haemoglobin test | 35.0 | 31.8 | 0.556 |
| Unable to perform blood smear for malaria parasites |
3.0 | 6.1 | 0.324* |
| Mortality (%) | 0.6 | 3.8 | 0.028 |
| Any essential drug or supply missing (%) | 45.0 | ||
| 57.9 | 0.004* | ||
| Percentage of caretakers satisfied with care received |
93.4 | 90.8 | 0.345 |
Fischer's exact test
During the study period, a particular problem was noted with tests for haemoglobin. The reagent for the test was often lacking. In as many as 30% of patients, the unit was unable to perform haemoglobin tests resulting in some severely anaemic patients being transfused without determining their haemoglobin levels.
Essential drugs and supplies missing in the emergency unit
Quinine, oxygen, normal saline, 5% dextrose, 25 or 50% dextrose, blood for transfusion, blood transfusion sets, intravenous cannulae, intravenous fluid giving sets, and syringes were considered the minimum drugs and supplies needed to resuscitate children presenting with severe malaria. If any of these items was needed to resuscitate a child and was not available, it was regarded as missing. Overall, 54.8% of the children had at least one item needed for their resuscitation missing in the emergency room. The most frequently missing items were intravenous cannulae (53.1%), syringes (23.3%) and blood transfusion sets (15%).1 There were significant differences in the percentages of children who presented during day with resuscitation items missing and those who came at night. (Table III) Figure II illustrates missing essential drugs and supplies.
Figure II.
Essential drugs and supplies missing in the emergency unit
In almost all cases, oxygen, normal saline and 5% dextrose were available when needed. With the exception of blood, the caretakers bought the missing essential drugs/supplies from nearby pharmacies. There was no significant association between lack of any essential supply and the occurrence of death; 2.8% of the children who lacked essential resuscitation supplies died compared to 3.5% of those who did not (OR 0.79 95% CI 0.35 – 1.82).
Selected measures of quality of care and outcome of severe malaria
A child was considered to have received quality care if a doctor attended to her/him within 1 hour of arrival, received the first dose of quinine within 2 hours, all essential drugs and supplies needed for his/her resuscitation were available, and the caretaker felt the service rendered was good or very good. Over 90% of the caretakers were satisfied with the services but less than half of the children had all the essential items available.
The relationship between these measures of quality and outcome of severe malaria is shown in table IV. Cases where services were considered good or very good had a significantly low mortality; 0.9 vs 16.9%, RR 0.05 (0.02 – 0.12). The level of education did not influence the rating a caretaker gave for the service (p = 0.303).
Table IV.
Selected measures of quality of care and outcome of severe malaria in Mulago Paediatric emergency unit
| Measures of quality | Percentage of children in who quality was achieved |
Mortality in group where quality was achieved (%) |
Mortality in group where quality was not achieved (%) |
P value |
| Child seen by a doctor | 23.4 | |||
| within 1 hour of arrival (%) | (N=653) | 5.2 | 2.2 | 0.091* |
| Child received first dose | 11.9 | |||
| of quinine within 2 hrs (%) | (N=715) | 3.7 | 2.5 | 0.472* |
| Did not lack essential drugs or supplies during emergency |
45.2 | |||
| care (%) | (N=784) | 2.8 | 3.5 | 0.673* |
| Caretaker considered services | 91.3 | |||
| good or very good (%) | (N=739) | 0.9 | 16.9 | <0.0001* |
Fischer's exact test
Aspects of the clinical assessment of patients by clinicians were poor. Important measurements like the blood pressure, though provided for in the management protocol, were not performed in the majority of children. Some children were transfused before determining the haemoglobin level. Renal function was not assessed in almost all children. For purposes of care and documentation, these areas need improvement.
Suggestions for quality improvement
Most caretakers (85.5%) either expressed appreciation or had no comments for improving the quality of services. The remaining 14.5% offered some suggestions as shown in Figure III.
An area of particular concern was staff discipline; caretakers were concerned about staff spending time on non-patient care related activities. Minimizing delays and offering faster services were recommended.
Discussion
Healthcare consumers use emergency units and services to gauge the quality of care they receive. This study looked at some measures of quality considered critical in resuscitation of severely ill children and satisfaction of caretakers of children in the management of severe malaria.
Severe malaria develops rapidly from uncomplicated disease. The mean duration of illness at admission of only two and half days is similar to findings in previous studies.8 The strategy of giving children anti malarial drugs within 24 hours to avert disease progression should therefore be emphasized.9 It was however sad to note that severe malaria developed despite pre-admission Chloroquine in > 50% of cases! The high Chloroquine resistance described in areas around Kampala may explain this10 and supports the view that Chloroquine alone may not be useful for uncomplicated malaria.
As expected in a malaria endemic area, severe anaemia was the commonest defining feature.11 The percentage of those with cerebral malaria was rather low3 although the distribution of other manifestations was within expected limits.3 Of particular importance was the 11.4% prevalence of hypoglycaemia since this unit does not routinely perform tests for blood sugar though it is provided for in the protocol. Similarly, blood pressure measurements were often not performed making it difficult to assess circulatory failure adequately. Children with this severe manifestation of malaria may die without any attempts to correct possible shock. It is time blood glucose assessment and blood pressure measurement in children with severe malaria is enforced in the unit.
Different degrees of impairment of consciousness, respiratory distress, multiple generalized convulsions and jaundice were significantly associated with death. The prominence of the associations between impairment of consciousness and respiratory distress on one hand and death on another confirms the high risk these two clinical features subject children to.3,12 The most interesting results however were those that demonstrated that patients appear to receive better services at night. This was the exact opposite of our initial hypothesis. The relatively small numbers of patients at night are seen quickly and started on specific malaria treatment resulting in significant reductions in mortality. This finding strengthens the view that with more hands in the emergency room especially during day, mortality in the unit can be reduced.
The unit fails the test of attending to children within 1 hour of arrival. Less than 25% of the children were seen within 1 hour and less than half of this received the first dose of quinine in 2 hours! This is an area that needs to be addressed urgently. The time taken to receive the first dose of quinine was further delayed by another 30 minutes among those who had to go and buy resuscitation materials. A steady supply of these resuscitation materials will cut down the time to onset of specific treatment with quinine. Firm action and commitment are needed to achieve these concerns. There was a slightly higher mortality among patients who passed the quality tests of being seen within 1 hour or receiving quinine within 2 hours. The most likely reason for this was that they were very sick children with poor prognosis in who resuscitation attempts failed despite early intervention by attending physicians. Haemoglobin level determination brought to light another problem of supplies. This basic test could not be done in over 30% of those who needed it because of lack of reagents. Several severely anaemic children were transfused on the basis of clinical observation. A mechanism should be put in place to plan for and ensure a steady supply of such important yet basic reagents.
Despite the gleam picture painted by the ratings of the measures of quality set in this study, the good news was the assessment by caretakers. Over 90% were satisfied with the care given to their children rating it either as good or very good and this was not influenced by the level of education a of caretaker. There was a significant correlation between the occurrence of death and services being considered poor. It is possible that caretakers who lost children would feel that not enough was done to save their children and rate the service poor. This assumption may be valid in cases where children died within a few hours of admission and questions on caretaker satisfaction with care were asked after the death of their children.
The caretakers also offered several suggestions for quality improvement. Most centred round increased availability and steady supply of essential materials, more staff, faster services, reduction in delays, enforcement of discipline among the staff, decongesting the unit and offering explanations to patients. These should be areas the unit should address as quality improvement processes are initiated as they bear directly to what clients feel.
Acknowledgements
We thank all caretakers of our patients and the patients themselves. May the souls of the 23 who died rest in peace. We thank the doctors and nurses in the emergency unit for their tireless effort in filling the case record forms, the laboratory staff and data entry staff.
The study received financial support from Makerere University Faculty of Medicine/Sida Sarec Research Grant and the Child Health and Development Centre/TORCH Project Novice Research grant.
References
- 1.Malaria: Know the facts. Quarterly Bulletin of the World Health Organization (WHO) Lagos, Nigeria. 1998;13(1):6–7. [Google Scholar]
- 2.Ministry of Health, author. Extend of the malaria problem; mortality and morbidity in Uganda malaria control policy. 2000. pp. 3–5. [Google Scholar]
- 3.Marsh K, Forster D, Waruiru C, et al. Indicators of life threatening malaria in African Children. New England Journal of Medicine. 1995;332(21):1399–1404. doi: 10.1056/NEJM199505253322102. [DOI] [PubMed] [Google Scholar]
- 4.Molyneux ME, Taylor TE, Wirima JJ, Borgstein A. Clinical features and prognostic indicators in paediatric cerebral malaria; a study of 131, comatose Malawian children. Quarterly Journal of Medicine. 1989;265:441–459. [PubMed] [Google Scholar]
- 5.World Health Organization, author. Severe falciparum malaria. Transactions of Royal Society Tropical Medicine Hygiene. 2000;94(supplement 1):1–45. [PubMed] [Google Scholar]
- 6.John CC, Idro R. Cerebral malaria in children. Infections in Medicine. 2003;20:53–58. [Google Scholar]
- 7.Rudolf MCJ, Levene MI, editors. Acute Diarrhoea in Paediatrics and Child Health. Blackwell Science; 2000. pp. 160–162. [Google Scholar]
- 8.Greenwood B, Bradley AK, Greenwood AM, et al. Mortality and morbidity from malaria among children in a rural area of the Gambia, West Africa. Transactions of Royal Society of Tropical Medicine Hygiene. 1987;81:474–486. doi: 10.1016/0035-9203(87)90170-2. [DOI] [PubMed] [Google Scholar]
- 9.MOH - Uganda, UNICEF, WHO, author. Joint draft proposal on Home management of fever in Uganda. 2001
- 10.Kamya MR, Dorsey G, Gasasira A, et al. The comparative efficacy of chloroquine and sulfadoxine-pyrimethamine for the treatment of uncomplicated falciparum malaria in Kampala-Uganda. Transactions of Royal Society of Tropical Medicine Hygiene. 2001;95:50–55. doi: 10.1016/s0035-9203(01)90331-1. [DOI] [PubMed] [Google Scholar]
- 11.Modiano D, Sirima BS, Sawadogo A, et al. Severe malaria in Burkina Faso: urban and rural environment. Parasitologica. 1999;41:251–254. [PubMed] [Google Scholar]
- 12.Idro R. Severe malaria anaemia in childhood cerebral malaria is associated with profound coma. African Health Sciences. 2003;3:15–18. [PMC free article] [PubMed] [Google Scholar]