Abstract
A total of 675,626 active duty Army soldiers who were known to be at risk for deployment to the Persian Gulf were followed from 1980 through the Persian Gulf War. Hospitalization histories for the entire cohort and Health Risk Appraisal surveys for a subset of 374 soldiers were used to evaluate prewar distress, health, and behaviors. Deployers were less likely to have had any prewar hospitalizations or hospitalization for a condition commonly reported among Gulf War veterans or to report experiences of depression/suicidal ideation. Deployers reported greater satisfaction with life and relationships but displayed greater tendencies toward risk-taking, such as drunk driving, speeding, and failure to wear safety belts. Deployed veterans were more likely to receive hazardous duty pay and to be hospitalized for an injury than nondeployed Gulf War-era veterans. If distress is a predictor of postwar morbidity, it is likely attributable to experiences occurring during or after the war and not related to prewar exposures or health status. Postwar excess injury risk may be explained in part by a propensity for greater risk-taking, which was evident before and persisted throughout the war.
Introduction
Nearly 700,000 American military personnel were deployed to the Persian Gulf between August 1990 and April 1991 in support of Operations Desert Shield/Desert Storm (ODS/DS), most of them Army soldiers. Soon after these soldiers began returning to the United States, reports of unexplained illnesses and nonspecific symptoms (later termed “Gulf War illnesses”) began to surface. After nearly 10 years of research and a great deal of media attention, the cause of these problems remains elusive.
One potential, although largely unexplored, explanation for the development of Gulf War-related illnesses is the possibility that prewar characteristics (intrinsic or acquired traits) shared by soldiers deployed to the Persian Gulf differ from those of soldiers not deployed. Understanding of these differences may contribute to an improved understanding of why a variety of symptom complexes described as Gulf War-related illnesses have been reported among those soldiers who did ultimately deploy to the Persian Gulf. At a minimum, the potential confounding influence of these possible differences deserves a comprehensive evaluation in current research efforts.
The purpose of this paper is to describe the prewar demographic, occupational, and physical and mental health status of active duty Army soldiers who deployed to the Persian Gulf and to compare these characteristics with those of soldiers on active duty who did not deploy.
Background
Studies of Gulf War veterans have focused principally on postwar health outcomes. Few studies have compared the prewar experiences, health habits, and general mental and physical health status of veterans. Most significantly, few studies have explored how factors predicting deployment may confound or contribute to soldiers’ risk of developing Gulf War-related illnesses subsequent to service in the Persian Gulf. Documenting differences between soldiers based on whether they deployed or not may improve understanding of postdeployment soldier health.
Differences in demographic variables, health behaviors, risk-taking behaviors, and mental or physical health could influence a soldier’s postwar health status. Such factors could affect the chance of selection for deployment (e.g., risk-taking habits), the risk of future illness independent of deployment (e.g., cigarette smoking), and the risk of responding to the deployment experience with increased risk-taking behaviors (e.g., postwar increases in alcohol use as a coping response).
During ODS/DS, deployed soldiers did not experience significantly higher overall mortality rates than nondeployed Gulf War-era veterans or the U.S. population at large, with the exception of unintentional injury death.1 Similarly, a study of postwar mortality found that deployed Gulf War veterans were significantly more likely to die from accidents, such as motor vehicle crashes, than their nondeployed counterparts, but not from illness-related deaths.2 This suggests either risk-taking differences between deployed and nondeployed soldiers during and after the war or increased exposure to hazards. Because a veteran’s experiences during the war might contribute to the adoption of unhealthy risk-taking behaviors after the war, it is important to look for the presence of these behaviors before deployment. Otherwise, we will not be able to discern whether the war caused increases in risk-taking or whether prewar tendencies to engage in risky behaviors were in fact responsible for deployment. Similarly, suggestions that stressors or distress after service in the Persian Gulf may predict Gulf War illnesses cannot be fully evaluated without exploration of mental health or experiences of stressors before deployment.
Studies published to date have primarily measured health outcomes among individuals assigned to one or more specialized military units, often relying on small samples,3–13 among groups of veterans seeking treatment for conditions they believed to be related to service in the Persian Gulf,10,14–16 or among veteran populations drawn from a particular geographic locale.7,10,17–22 Many studies relied heavily on self-reports of symptoms and exposures, sometimes with little obvious effort to validate the reports or the measurement instrument used.7,9–13,17–22 Premorbid data on the physical and mental health status of Gulf War veterans is severely limited. There have been few population-based surveys that have examined health-related trends across the entire Army or that have been able to control for a large enough number of demographic variables to adequately assess the issue of who gets selected to deploy. This has resulted in an incomplete and potentially biased picture of the functional health status of Army Gulf War veterans and has prevented a cogent assessment of the extent to which prewar factors affect a soldier’s risk of developing Gulf War-related illnesses.
This paper expands upon existing knowledge by examining a broader range of prewar health status measures for all Army soldiers on active duty during the war, followed over a longer continuous prewar period. Also, this paper focuses specifically on the Army, a group known to be disproportionately high users of care for Gulf War health concerns.23 This study includes prospectively gathered information on a variety of mental health and risk-taking behavior measures.
Methods
Study Population
A total of 675,626 active duty Army soldiers were followed from 1980, or entry to the Army if they entered after 1980, to the beginning of ODS/DS (August 1990). Approximately 38% (N = 257,699) of these soldiers ultimately were deployed to the Persian Gulf at some time between August 1, 1990, and June 14, 1991. Although a total of 836,438 soldiers were on active duty in the U.S. Army during some portion of the Gulf War, only soldiers who remained on active duty for the full duration of ODS/DS (i.e., active duty subjects, for whom we had confirmed demographic information at three observation dates: June 1990, December 1990, and June 1991) were included in the study cohort. Out of these 836,438 soldiers, there were 160,812 who were on active duty during some portion of ODS/DS but not for the entire period, 7.5% of whom (N = 12,098) were deployed to the Persian Gulf. Because these individuals did not have the same opportunity to be deployed and were often missing prewar information, they were not included in the study population. A subanalysis of 374 members of the study population who took an Army Health Risk Appraisal (HRA) before the war began was conducted to assess differences in prewar risk-taking, self-reported experiences of stressors, and feelings related to distress or depression.
The Data
The Total Army Injury and Health Outcomes Database (TAIHOD)24,25 was used to describe the study population’s demographic, health, and behavioral characteristics. The TAIHOD joins key elements from multiple Department of Defense (DoD) administrative and health databases, linked at the individual soldier level by encrypted Social Security numbers. Components used in these analyses included demographic and occupational records, self-reported health behaviors and quality of life (HRA surveys), hospitalizations, and health evaluations from the Comprehensive Clinical Evaluation Program for Gulf War veterans (CCEPa).24,25
The TAIHOD Defense Manpower Data Center data are collected at 6-month intervals, in June and December of each year. Discharge (“loss”) files are merged to these files to provide a complete occupational history for every active duty soldier. HRAs, officially implemented by the Army in 1987 but not administered in large numbers until 1991, have been administered to a subset of the Army during routine in-processing to new work assignments, as part of periodic physical examinations or physical fitness testing, or during walk-in visits to occupational or outpatient health clinics. Sociodemographic characteristics of individuals taking the HRA were similar to those of individuals in the study population who did not take an HRA, except that HRA takers were more likely to have some education beyond high school than were those in the overall cohort (38% versus 19%, respectively). Also, enlisted soldiers who had completed an HRA were more senior than enlisted soldiers who did not complete an HRA (50% of HRA takers were E5 or above versus about 40% of those who did not take an HRA). These differences probably reflect, in part, longer time in the Army and thus greater opportunity to have been offered the HRA. Although 13% of the overall study cohort had been in the Army for 1 year or less in June 1990, only 6% of those taking the HRA had been in the service for 1 year or less. Perhaps more importantly, though, those taking the HRA were no more likely to have had a previous hospitalization than those who did not take an HRA, suggesting similar health status (data not shown).
Variables for Analysis
The main outcome measure for these analyses is deployment to the Persian Gulf. The DMDC Gulf War deployment file was used to determine if a soldier was deployed to the Gulf War theater of operations. For this analysis, deployment was defined by being sent to the Gulf War theater at any time between August 1, 1990, and June 14, 1991.
Demographic Data
Demographic information included gender, age, race, education, marital status, number of dependents, rank, total active duty service, and occupation (DoD occupational code). Demographic data from the June 1990 DMDC files were used for most analyses. For logistic regression models of prewar annual hospitalization risks, demographic data from the first observation point in each year were used.
For ease of analysis and interpretation, age is grouped as younger than 21, 21 to 25, 26 to 30, 31 to 35, 36 to 40, and older than 40 years of age. Racial or ethnic groups are described as white, black, Hispanic, Asian/Pacific Islander. Alaskan/Indian, and other. Education is coded as less than a high school degree, high school degree or equivalent (GED), some college, bachelor’s degree, any graduate education, and other. Marital status is coded as single (never married), no longer married, married with spouse not on active duty, married with spouse on active duty but not deployed to the Persian Gulf, and married with spouse on active duty and deployed to the Persian Gulf. Dependent status is coded as member only, member with one dependent, and member with two or more dependents. Military rank is coded as junior enlisted (E1–E4), senior enlisted (E5–E9), warrant officers, junior officers (O1–O3), officers (O4–O5), and senior officers (O6–O11). Total time on active duty was calculated from entry into the service until June 1990 and grouped as follows: less than 6 months, more than 6 to 12 months, more than 12 to 24 months (1–2 years), more than 24 to 60 months (2–5 years), more than 60 to 120 months (5–10 years), more than 120 to 180 months (10–15 years), more than 180 to 240 months (15–20 years), and more than 240 months (more than 20 years).
Some soldiers receive hazardous duty pay as partial compensation for their occupational exposures. Hazardous duty pay is received by flight crew, parachutists, divers, those assigned to war zones (combat pay) or foreign duty, and those exposed to environmental stressors or experimental vaccines. Hazardous duty has been linked in previous research to increased risk of injury.26 For this study, hazardous duty pay was coded as follows: not receiving hazardous duty pay, receiving one type of hazardous duty pay only, and receiving two or more types of hazardous duty pay concurrently between January 1 and June 30, 1990. Thus, hazardous duty compensation received in this period reflects exposures before ODS/DS.
Occupations were grouped using the DoD occupational codes.b DoD occupational codes are broad occupational categories composed of similar military occupational specialties. Occupational specialties available differ by rank and often by gender. The categories for enlisted personnel include infantry/gun crews, electrical equipment repair, communications/intelligence, health care, technical/allied specialists, support/administration, mechanical equipment repair, crafts workers, service/supply, and nonoccupational. Warrant and commissioned officer categories include general officer/executive, tactical operations officer, intelligence officer, engineering and maintenance officer, scientists and professionals, health care officers, administrators. supply/procurement and allied officers, and nonoccupational.
Health and Health Behaviors
The hospital and HRA components of the TAIHOD were used to document prewar health status. Hospitalizations were examined in three overlapping categories: any cause, injuries (International Classification of Diseases, 9th Revision, Clinical Modification codes 800–999), and conditions most commonly observed among Army Gulf War veterans evaluated for Gulf War-related health concerns.c Although there is no clear consensus from the medical community on what constitutes a Gulf War illness, to evaluate the incidence of prewar conditions commonly diagnosed among veterans of the war we used the 25 most frequent ICD-9-CM diagnoses (other than “healthy”) among Army veterans registered with the CCEP who received a clinical evaluation. These Gulf War-prevalent illnesses are referred to as Gulf War illnesses (GWI) throughout this text. Hospitalization with a primary diagnosis including any of these conditions was used to indicate a GWI hospitalization independent of deployment status. Any hospitalization occurring before August 1, 1990, was included for analysis, with the earliest hospitalization cases occurring in 1980. For purposes of these descriptive analyses, hospitalizations were counted once per individual in each of the three categories.
Stressors, distress, risk-taking propensity, and general mental well-being were assessed through several HRA variables. We grouped six variables assessing behavioral risk for alcohol dependence into one single index measure because intercorrelations were quite high (coefficient α = 0.763) and all of the items appear to measure risk for dependent drinking (face validity). The resultant composite alcohol use measure comprised the four CAGE items27 and two additional, similarly scaled items: “friends worry about your drinking” and “ever have a drinking problem.” The CAGE is a clinical screening tool used to identify individuals at risk for alcohol dependency. Thus, we refer to the composite variable (CAGE plus the two related items) as a potential “dependent drinking” measure. This composite item has been shown to be a better predictor of high-risk drinking and other risky behaviors than the CAGE alone.28 Survey takers missing responses to three or more of the items were excluded (18%). The remaining items were used to develop an average response. These responses were dichotomized, based on the distribution of responses for the entire population, into two categories: those with no affirmative responses (84%) versus those with one or more affirmative responses. Risky driving practices were also grouped to improve power and because any one of the three high-risk driving habits measured in the HRA could increase the risk for motor vehicle injuries–the only source of differences in mortality between Gulf War-era veterans who were deployed versus those not deployed to the Persian Gulf.2.29 This variable included drinking alcohol before driving or riding with someone who had been drinking, speeding, and seatbelt use. Very few soldiers were missing responses to any of these items (N = 6). Those who were missing responses to any of these items were excluded from the analysis. The final variable was coded as yes if the subject said he or she had done any drinking and driving or had ridden with an intoxicated driver one or more times in the past month, if he or she routinely drove more than 5 miles per hour over the speed limit, or if he or she reported using a safety belt less than 100% of the time on average.
Other variables used for analysis included feeling so overwhelmed the respondent had considered hurting himself or herself, considering suicide or experiencing prolonged depression within the past year, experiencing worries that interfered with life, problems with spouse, children, or peers, work stress, low satisfaction in current job assignment, low life satisfaction, frequent losses in the past year, and little time for relaxation. We also included self-reported daily tobacco use and weekly alcohol consumption.
Analytic Methods
Exploratory analysis was conducted using frequency distributions and χ2 tests. Continuous variables were compared using t tests. To compare prewar differences in health behaviors and experiences of stressors and distress between deployed and nondeployed cohorts. χ2 analysis was used. Multiple logistic regression analyses, with deployment as an outcome, were conducted to explore the relationships between the explanatory variables. Occupation, gender, and rank were highly correlated. Therefore, we constructed different models, selecting the most commonly deployed occupational groups in each gender-rank group for comparison purposes.
To compare differences between deployed and nondeployed cohorts in their risk for hospitalization before the war while controlling for differences in exposure potential (time in service), multivariate Cox proportional hazard models were used. Soldiers were followed from entry into the Army (or from January 1, 1980, for those who entered the Army before 1980) until their first hospitalization event occurred or until August 1, 1990 (censored date). In 1990, only hospitalizations occurring before August 1 were included for comparison, because this was 1 day before Iraq’s invasion of Kuwait and 1 week before the arrival of U.S. planes in Saudi Arabia. Thus, we hoped to reduce potential bias that might result if an individual sought hospitalization to avoid deployment.
To identify changes in risk for hospitalization as a function of time and proximity to the deployment period, logistic regression models predicting hospitalization for any cause, for injuries, and for GWI were also constructed for each year in the prewar period. Beginning in 1980, models compared rates in each year for soldiers who ultimately deployed with rates for those who did not deploy. The potentially confounding influences of gender, age, race/ethnicity, time in active military service, education, and rank were included in the models.
SAS was used to develop multivariate models and initial exploratory models.30 Bivariate associations between self-reports on the HRA and deployment status were evaluated using EpiInfo.31 Exact odds ratios, confidence intervals, and two-sided p values were used, because many of the tables included sparse cells.
Results
There were 675,626 Army soldiers on continuous active duty during ODS/DS. Thirty-eight percent (257.699) were deployed to the Persian Gulf between August 1, 1990, and June 1, 1991.
Unadjusted analyses revealed that deployers were more likely to be male. have fewer than 5 years of time in service, be younger than 25 years of age, black, single, and high school graduates, have fewer dependents, and be junior enlisted and junior officer rank than their nondeployed counterparts (Table I). Thirty-nine percent of men on active duty during the war deployed compared with 29% of women on active duty: 46% of those younger than 21 years deployed compared with 28% of those older than 35 years; and almost half of those enlisted with a grade of E1 to E4 (45%) deployed compared with 10% of officers with a grade of O6 to O11 (data not shown).
TABLE I.
UNADJUSTED ASSOCIATIONS BETWEEN THE DEMOGRAPHIC CHARACTERISTICS OF 675.626 ARMY GULF WAR-ERA VETERANS AND DEPLOYMENT TO THE PERSIAN GULF
| Deployed (N = 257.699) | Not Deployed (N = 417.927) | χ2p Values | |
|---|---|---|---|
| Gender | <0.001 | ||
| Male | 91.64% | 87.12% | |
| Female | 8.36% | 12.88% | |
| Agea | <0.001 | ||
| <21 years | 15.04% | 11.07% | |
| 21–25 years | 37.15% | 28.09% | |
| 26–30 years | 22.58% | 21.94% | |
| 31–35 years | 13.56% | 17.64% | |
| 36–40 years | 7.92% | 12.50% | |
| >40 years | 3.75% | 8.73% | |
| Race/ethnicity | <0.001 | ||
| White | 60.85% | 62.82% | |
| Black | 30.67% | 28.63% | |
| Hispanic | 4.15% | 3.96% | |
| Asian/Pacific Island | 1.43% | 1.82% | |
| Indian/Alaskan | 0.56% | 0.50% | |
| Other | 2.32% | 2.24% | |
| Educational level | <0.001 | ||
| Less than high school | 1.21% | 0.89% | |
| High school graduate/GED | 84.35% | 75.29% | |
| Alternative education | 0.03% | 0.03% | |
| Some college | 3.43% | 4.94% | |
| Bachelor’s degree | 7.75% | 10.98% | |
| Graduate degree | 2.10% | 6.67% | |
| Unknown | 1.13% | 1.22% | |
| Marital status | <0.001 | ||
| Single | 43.31% | 34.00% | |
| Married, spouse not on active duty | 49.93% | 56.98% | |
| Married, spouse on active duty and deployed | 1.95% | 0.95% | |
| Married, spouse on active duty and not deployed | 1.57% | 3.65% | |
| No longer married | 3.20% | 4.27% | |
| Unknown | 0.03% | 0.15% | |
| Dependents | <0.001 | ||
| Member only | 44.93% | 36.65% | |
| Member plus one dependent | 17.57% | 17.50% | |
| Member plus two or more dependents | 37.32% | 45.56% | |
| Unknown | 0.19% | 0.29% | |
| Rank | <0.001 | ||
| E1–E4 | 54.39% | 41.33% | |
| E5–E9 | 34.92% | 41.41% | |
| Warrant officer | 2.20% | 1.95% | |
| O1–O3 | 6.53% | 9.08% | |
| O4–O5 | 1.77% | 5.26% | |
| O6–O11 | 0.18% | 0.97% | |
| Time in Service | <0.001 | ||
| Less than 6 months | 3.99% | 4.50% | |
| 6–12 months | 10.94% | 7.89% | |
| >12–24 months | 16.31% | 10.88% | |
| >24–60 months | 31.71% | 26.20% | |
| >60–120 months | 18.34% | 20.13% | |
| >120–180 months | 11.10% | 15.59% | |
| >180–240 months | 6.31% | 11.27% | |
| >240 months | 1.26% | 3.49% | |
| Unknown | 0.03% | 0.05% | |
| Hazardous duty pay | <0.001 | ||
| No hazardous duty pay | 86.41% | 87.08% | |
| Hazardous duty pay one type | 12.81% | 12.37% | |
| Hazardous duty pay two or more types in pay period | 0.78% | 0.55% | |
| Enlisted (n = 575,942) | <0.001 | ||
| Infantry/gun crews | 27.58% | 24.34% | |
| Mechanical equipment repair | 18.99% | 13.38% | |
| Communication/intelligence | 14.01% | 14.13% | |
| Support/administration | 12.17% | 18.26% | |
| Service/supply | 11.76% | 11.15% | |
| Health care | 5.09% | 8.24% | |
| Electrical equipment repair | 4.60% | 5.29% | |
| Technical/allied specialist | 2.93% | 2.96% | |
| Craftsworkers | 2.61% | 1.77% | |
| Nonoccupational | 0.25.% | 0.44% | |
| Other | 0.01% | 0.03% | |
| Officer (n = 85.874) | <0.001 | ||
| Tactical operations officer | 40.86% | 27.02% | |
| Nonoccupational | 12.10% | 19.06% | |
| Health care officers | 12.10% | 18.91% | |
| Supply, procurement, and allied officers | 10.37% | 7.11% | |
| Engineering and maintenance officer | 10.35% | 8.54% | |
| Intelligence officer | 5.24% | 4.50% | |
| Administrators | 4.90% | 7.40% | |
| Scientists and professionals | 3.78% | 6.79% | |
| General officer/executive | 0.26% | 0.52% | |
| Other | 0.05% | 0.15% | |
| Warrant (n = 13.810) | <0.001 | ||
| Tactical operations officer | 49.09% | 37.77% | |
| Engineering and maintenance officer | 26.44% | 25.37% | |
| Supply, procurement, and allied officers | 7.76% | 7.42% | |
| Nonoccupational | 4.91% | 6.31% | |
| Intelligence officer | 4.38% | 7.34% | |
| Health care officers | 3.77% | 3.75% | |
| Administrators | 3.49% | 11.28% | |
| Scientists and professionals | 0.14% | 0.64% | |
| Other | 0.02% | 0.12% |
Values are those documented in June 1990 DMDC records.
χ2 test for trend analysis indicated a statistically significant trend of increasing risk for deployment with successively younger age groups, with the odds for deployment being more than three times greater among those younger than 21 years than for those older than 40 (p < 0.001).
Deployers were also more likely to have received hazardous duty pay before July 1990 (Table I). Deployed enlisted soldiers were more likely to be in infantry/gun crews, mechanical equipment repair, or crafts worker (e.g., plumbers, metal workers) occupations. Deployed officers were significantly more likely to belong to the tactical operations or supply and procurement, engineering and maintenance, or intelligence officer occupational group. Deployed warrant officers were significantly more likely to be in the tactical operations occupational group.
Table II shows whether the demographic characteristics described in Table I are independent predictors of deployment in multivariate logistic regression models. Because gender, rank, and occupation are highly correlated (with numerous potential occupational categories), we conducted separate subanalyses based on occupations most commonly deployed to the Persian Gulf within each gender-rank group. The results from these multivariate logistic regression models show factors explaining variation among those who deployed and those who did not deploy in occupations with the highest rates of deployment to the Persian Gulf.
TABLE II.
MULTIVARIATE LOGISTIC REGRESSION ANALYSES OF INDIVIDUAL CHARACTERISTICS RELATED TO DEPLOYMENT TO THE PERSIAN GULF BY OCCUPATION, RANK, AND GENDER GROUPS MOST OFTEN DEPLOYED TO THE PERSIAN GULF
| Infantry and Gun Crews (N = 146,864) (Male Enlisted) | Support and Administration (N = 25,248) (Female Enlisted) | Tactical Operations (N = 31,427) (Male Officer) | Health Care (N = 4,566) (Female Officer) | |
|---|---|---|---|---|
| Age | ||||
| 17–20 years | 2.5 (2.3–2.7) | 2.8 (2.2–3.5) | 3.0 (0.9–9.4) | NAa |
| 21–25 years | 2.4 (2.3–2.6) | 2.3 (1.8–2.8) | 4.3 (3.9–4.7) | 2.1 (1.6–2.7) |
| 26–30 years | 1.8 (1.6–1.9) | 1.9 (1.5–2.4) | 3.3 (3.1–3.6) | 1.4 (1.1–1.8) |
| 31–35 years | 1.4 (1.3–1.5) | 1.5 (1.2–1.8) | 2.0 (1.8–2.1) | 1.3 (1.0–1.7) |
| 36–40 years | 1.2 (1.1–1.3) | 1.1 (0.9–1.4) | 1.9 (1.7–2.1) | 1.0 (0.8–1.3) |
| >41 years | 1.0 | 1.0 | 1.0 | 1.0 |
| Race/ethnicity | ||||
| White | 1.0 | 1.0 | 1.0 | 1.0 |
| Black | 1.0 (1.0–1.0) | 1.1 (1.1–1.2) | 0.9 (0.8–1.0) | 0.9 (0.7–1.2) |
| Hispanic | 1.0 (0.9–1.0) | 1.3 (1.1–1.5) | 0.8 (0.7–1.0) | 1.0 (0.5–1.9) |
| Indian/Alaskan | 1.0 (0.9–1.2) | 1.1(0.8–1.6) | 1.1 (0.8–1.6) | 0.7 (0.2–3.2) |
| Asian/Pacific Islander | 0.9 (0.8–1.0) | 0.8 (0.7–1.0) | 0.8 (0.6–1.0) | 0.7 (0.4–1.3) |
| Other | 1.0 (0.9–1.0) | 1.1 (0.9–1.4) | 0.9 (0.7–1.1) | 0.8 (0.4–1.6) |
| Education | ||||
| Less than high school | 2.9 (1.7–4.9) | 4.7 (1.7–13.3) | 2.3 (0.4–13.8) | NA |
| High school graduate/GED | 2.8 (1.7–4.7) | 3.3 (1.4–7.6) | 3.8 (3.3–4.3) | NA |
| Alternative education | 3.0 (1.4–6.2) | NA | NA | NA |
| Some college | 1.9 (1.1–3.2) | 2.2 (1.0–5.3) | 3.0 (2.7–3.4) | NA |
| Bachelor’s degree | 2.0 (1.2–3.4) | 2.1 (0.9–5.1) | 2.1 (1.9–2.2) | 2.1 (1.8–2.5) |
| Graduate degree | 1.0 | 1.0 | 1.0 | 1.0 |
| Marital Status | ||||
| Single | 1.5 (1.5–1.5) | 1.3 (1.2–1.4) | 1.5 (1.4–1.6) | 1.4 (1.1–1.7) |
| Married, spouse not on active duty | 1.0 | 1.0 | 1.0 | 1.0 |
| Married spouse on active duty, not deployed | 0.7 (0.7–0.8) | 0.5 (0.4–0.5) | 0.9 (0.7–1.1) | 0.7 (0.5–1.0) |
| Married, spouse on active duty, deployed | 2.4 (2.0–2.9) | 2.7 (2.5–3.0) | 3.9 (2.8–5.3) | 1.9 (1.3–2.6) |
| No longer married | 1.0 (0.9–1.1) | 0.8 (0.7–0.9) | 1.0 (0.9–1.2) | 1.3 (1.0–1.7) |
| Dependents | ||||
| Member only | 1.6 (1.6–1.6) | 1.3 (1.3–1.4) | 1.7 (1.6–1.8) | 1.7 (1.4–2.1) |
| Member plus one | 1.3 (1.3–1.3) | 1.1 (1.0–1.2) | 1.6 (1.5–1.7) | 1.1 (0.9–1.5) |
| Member plus two or more | 1.0 | 1.0 | 1.0 | 1.0 |
| Rank | ||||
| E1–E4 | 1.6 (1.6–1.6) | 1.6 (1.5–1.7) | NA | NA |
| E5–E9 | 1.0 | 1.0 | NA | NA |
| O1–O3 | NA | NA | 0.8 (0.8–0.9) | 10.4 (2.5–42.2) |
| O4–O5 | NA | NA | 0.4 (0.4–0.4) | 6.3 (1.5–25.7) |
| O6–O11 | NA | NA | 1.0 | 1.0 |
| Time in service | ||||
| <6 months | 2.2 (1.9–2.4) | 4.6 (1.8–11.7) | 1.9 (1.3–2.8) | 1.0 (0.4–2.3) |
| 6–12 months | 3.2 (2.9–3.6) | 5.4 (2.1–13.5) | 5.5 (4.6–6.6) | 3.2 (1.6–6.2) |
| >12–24 months | 2.9 (2.6–3.2) | 7.0 (2.8–17.6) | 5.7 (5.0–6.5) | 3.2 (1.7–6.2) |
| >24–60 months | 2.8 (2.5–3.1) | 4.1 (1.6–10.3) | 4.5 (4.0–5.1) | 2.6 (1.4–5.0) |
| >60–120 months | 1.8 (1.7–2.1) | 3.6 (1.5–9.1) | 2.9 (2.6–3.3) | 2.5 (1.3–4.7) |
| >120–180 months | 1.6 (1.4–1.7) | 2.6 (1.0–6.4) | 2.6 (2.3–2.9) | 1.8 (0.9–3.5) |
| >180–240 months | 1.3 (1.1–1.4) | 1.8 (0.7–4.7) | 1.9 (1.6–2.1) | 1.6 (0.8–3.2) |
| >240 months | 1.0 | 1.0 | 1.0 | 1.0 |
| Hazardous duty pay | ||||
| No hazardous duty pay | 1.0 | 1.0 | 1.0 | 1.0 |
| Hazardous duty pay one type | 0.8 (0.8–0.9) | 0.8 (0.7–0.9) | 2.0 (1.8–2.21 | 0.3 (0.0–2.2) |
| Hazardous duty pay two or more types in pay period | 1.4 (1.3–1.5) | 0.2 (0.0–1.7) | 5.1 (2.9–8.8) | NA |
Values are odds ratios for deployment and 95% confidence intervals (in parentheses).
NA, No soldiers represented within these categories for the specific occupation, gender, and rank group displayed.
Factors consistently associated with deployment across all four occupations included younger age (mostly younger than 25 years), less time in service (particularly those in the service less than 5 years), having fewer than two dependents, and having a spouse on active duty who was also deployed to the Persian Gulf. Also, those with less education were more likely than their more highly educated counterparts to deploy. Enlisted male and female soldiers of lower rank were significantly more likely to be deployed than their higher-ranking counterparts. This was also true of female officers but not male officers. Male enlisted and male officers with special pay for exposure to two or more occupational hazards were more likely to deploy than males in these same occupations who had received no hazardous duty pay.
Three hundred seventy-four of the 675.626 soldiers on active duty during ODS/DS had taken an HRA before August 1, 1990. Deployers were less likely to have seriously contemplated suicide or to have experienced prolonged or repeated periods of depression within the past year (Table III). They were less likely to say that life had been so overwhelming that they had considered hurting themselves, that worries had ever interfered with their daily lives, that they were not satisfied with their lives or jobs, that they had experienced family problems or personal misfortunes, or that they never had time to relax. They were also less likely to answer affirmatively to the dependent drinking measure. Similarly, those who deployed were more likely to say that they had experienced a pleasant life change in the past year. Although the direction of these associations is consistent, we are unable to rule out the role of chance in these associations because of small sample sizes and tight control of type I and II errors.
TABLE III.
PREWAR SELF-REPORTED DEPRESSION, DISTRESS, STRESS, AND RISK-TAKING BEHAVIORS AND UNIVARIATE ASSOCIATIONS WITH DEPLOYMENT TO THE PERSIAN GULF AMONG 374 ARMY SOLDIERS COMPLETING AN HRA BEFORE AUGUST 1. 1990
| Risk Factor | Deployed (N = 106) | Nondeployed (N = 268) | Odds Ratioa | 95% Confidence Interval | Two-Tailed p Value |
|---|---|---|---|---|---|
| Reports considering suicide or experiencing prolonged/repeated periods of depression in past year (vs. never) | 20% | 31% | 0.56 | 0.31–0.99 | 0.04 |
| Reports feeling so overwhelmed with life that he or she considered hurting self in past year (vs. never) | 2% | 4% | 0.45 | 0.05–2.13 | 0.37 |
| Reports worries have interfered with daily life during past year (vs. never) | 44% | 49% | 0.83 | 0.51–1.34 | 0.42 |
| Reports having has serious problems dealing with spouse, parents, children, or friends (vs. never) | 62% | 70% | 0.70 | 0.43–1.16 | 0.14 |
| Reports feeling only somewhat or not satisfied at all with life in general (vs. mostly or totally satisfied) | 14% | 20% | 0.66 | 0.33–1.26 | 0.19 |
| Reports having experienced personal misfortune in past year (vs. none) | 53% | 61% | 0.73 | 0.45–1.18 | 0.17 |
| Reports feeling not satisfied with current job (vs. somewhat, mostly, or totally satisfied) | 67% | 72% | 0.77 | 0.44–1.37 | 0.34 |
| Reports feeling there is sometimes too much work stress (vs. never) | 73% | 68% | 1.23 | 0.72–2.12 | 0.43 |
| Reports seldom or never has time to relax (vs. sometimes or often) | 14% | 17% | 0.87 | 0.42–1.65 | 0.62 |
| Responds yes to one or more dependent drinking measures (vs. “no” to all) | 11% | 18% | 0.55 | 0.25–1.21 | 0.11 |
| Reports current smoking habits as | |||||
| Current smoker | 21% | 22% | 0.93 | 0.50–1.71 | 0.82 |
| Ex-smoker (vs. never smoked) | 21% | 22% | 0.90 | 0.48–1.65 | 0.90 |
| Reports he or she has often or sometimes experienced pleasant life change in past year (vs. seldom or never) | 62% | 39% | 1.45 | 0.89–2.37 | 0.11 |
| Reports engaging in at least one high-risk driving practice in past month or typically (vs. none)b | 53% | 46% | 1.34 | 0.83–2.16 | 0.20 |
Exact methods used to calculate odds ratios, 95% confidence intervals, and p values are described in Epilnfo.31
Reports drinking and driving one or more times in past month, or speeding more than 5 miles over the limit, or not wearing seatbelt 100% of the time.
A trend was observed suggesting that those who deployed are more likely to engage in risky behaviors, such as drinking alcohol before driving, speeding, and not wearing seatbelts while driving.
In multivariate Cox proportional hazards models (controlling for gender, age, race, education, marital status, time in service, rank, and prewar receipt of hazardous duty pay), deployed status remained significantly associated with reduced risk for hospitalization for any cause or for one of the conditions commonly documented among Gulf War veterans, although the risk differences were quite small. There was no significant difference in risk of injury hospitalization between deployed and nondeployed Gulf War-era veterans. Male gender, young age, less education, single marital status, less time in service, and receipt of two or more types of hazardours duty pay in a pay period were all significant predictors of prewar injury hospitalization (data not shown).
Figures 1 to 3 depict the association between deployment and adjusted odds of hospitalization during each year of the follow-up period. Figure 1 shows that deployers were at lower risk for hospitalizations for any cause, particularly in the period immediately before ODS/DS, even after controlling for gender, age, race/ethnicity, time on active duty, education, and rank.
Fig. 1.
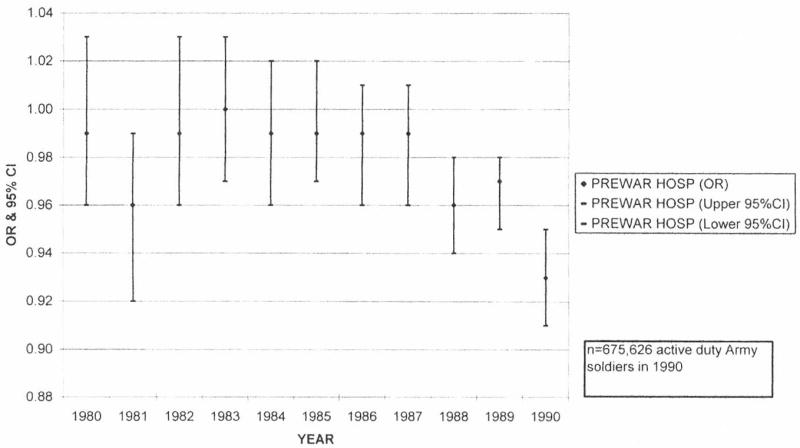
OR and 95% CI for deployment status (outcome = any prewar hospitalizations 1980–1990) controlling for gender, age, ethnicity, total time in service, education, and rank. Demographics, physical, and mental health factors associated with deployment of U.S. Army soldiers to the Persian Gulf.
Fig. 3.
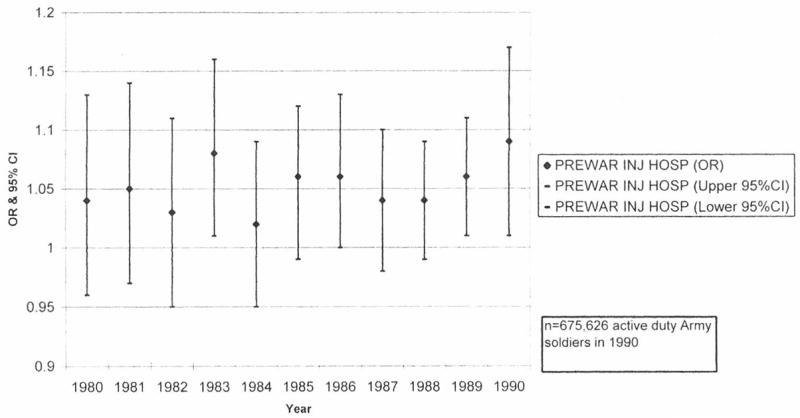
OR and 95% CI for deployment status (outcome = prewar injury hospitalizations 1980–1990) controlling for gender, age, ethnicity, total time in service, education, and rank. Demographics, physical, and mental health factors associated with deployment of U.S. Army soldiers to the Persian Gulf.
Deployed soldiers were not at greater risk for a prewar GWI hospitalization than nondeployed Gull War-era veterans. There was a largely consistent pattern of risk in the prewar period where those who ultimately deployed were actually at lower risk for a hospitalization related to any of the diagnoses most commonly seen among veterans seeking care for GWI after the war (Fig. 2).
Fig. 2.
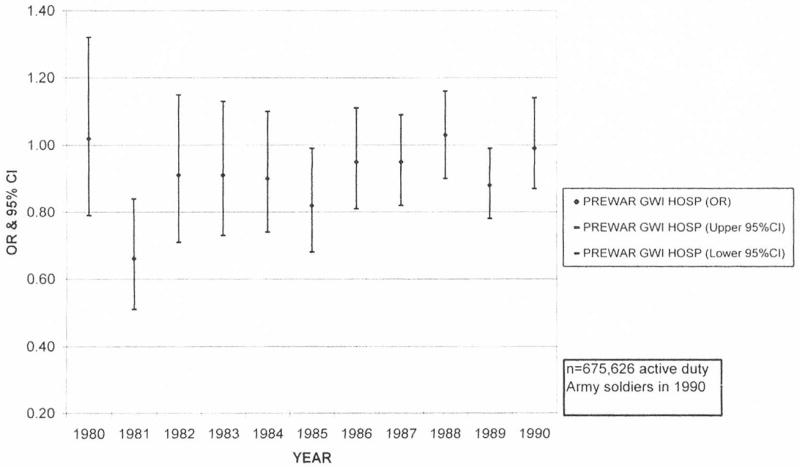
OR and 95% CI for deployment status (outcome = prewar GWI hospitalizations 1980–1990) controlling for gender, age, ethnicity, total time in service, education, and rank. Demographics, physical, and mental health factors associated with deployment of U.S. Army soldiers to the Persian Gulf.
In most years before ODS/DS, deployers were at greater risk for an injury hospitalization than were their nondeployed counterparts. This was true even after accounting for the effects of gender, age, race, time in service, education, and rank (Fig. 3). To refine this analysis, we also constructed an age-specific model including just soldiers younger than 26 years. Even among this very young cohort, injury risk in almost every year before ODS/DS was significantly higher among soldiers who ultimately deployed than among those who did not (data not shown).
Discussion
Without good prewar baseline information, it is difficult to make a cogent assessment regarding the postwar health consequences of service in the Persian Gulf. There have been relatively few studies documenting the prewar health and mental status of soldiers deployed to the Persian Gulf. The few studies that have focused on or at least briefly described differences between those who deployed and those who did not deploy to the Persian Gulf note that veterans deployed there were disproportionately male and younger than veterans deployed elsewhere.1,18,23 They were also more likely to be married than their nondeployed counterparts and differed significantly with respect to race or ethnicity, branch of service, activation status (e.g., reserve versus active duty), and grade.1,18,23 Deployed veterans were more likely to be discharged or separated from the military soon after the war, although not because of death or medical disability.23 Gray et al. also note that military personnel who were sent to the Persian Gulf had fewer prewar hospitalizations up to the point of deployment than their nondeployed counterparts, particularly in the years immediately preceding ODS/DS, similar to what we document among active duty Army personnel.23 We expand upon these earlier observations by examining a longer period and by including an assessment of prewar risk-taking differences, self-appraised distress and well-being, and by focusing on active duty Army personnel. We also expand upon the strengths of earlier studies by using a comparison group that was more restrictive than those used by many other researchers. We reduce potential bias by including only nondeployed Gulf War-era veterans who were on active duty during the entire ODS/DS period.
Our data suggest that before the war Army soldiers who ultimately deployed to the Persian Gulf were significantly healthier and happier than their nondeployed counterparts, as measured by their hospitalization histories and self-reports. They were significantly less likely to report prewar experiences of depression or suicidal ideation, and they were significantly less likely to have experienced any prewar hospitalizations and, most note-worthy, hospitalizations for conditions most prevalent among postwar Army veterans seeking care. The data also suggest that deployed personnel were happier in their personal lives (families, life events) and jobs before the war than their nondeploying counterparts. Although small sample sizes limited our ability to detect statistically significant differences in many cases between the two cohorts, the consistency of the findings across measures of satisfaction and general well-being is compelling.
There is some evidence indicating that soldiers who deployed to the Persian Gulf may have been greater risk takers before deployment and/or may have faced greater hazards than nondeployed Gulf War-era veterans. They were more likely to have received hazardous duty pay for two or more different hazardous exposures before being deployed to the Gulf War theater. These prewar differences are driven primarily by more frequent receipt of pay for parachuting or for potential exposure to hostile fire. Indeed, these attributes or experiences might make the candidates likely prospects for wartime deployment.
Other evidence for excess prewar risk-taking or risk exposure among deployers can be found in the records of prewar hospitalizations and self-reported behaviors. For most years between 1980 and 1990, annualized odds for injury hospitalizations were higher than for those not deployed, even after adjusting for potential confounders. Similarly, nonsignificant trends were observed that suggested that soldiers deployed to the Persian Gulf were also more likely to speed, drive after having had too much alcohol, or ride with someone who had consumed too much alcohol, and they were less likely to always wear seatbelts.
Those who were deployed to the Persian Gulf were significantly more likely to also have a spouse who was deployed. This may be an important modifying factor and should be considered in future studies examining risk factors for Gulf War-related illnesses. This seems particularly important given the findings of Gray et al., who note that even after controlling for several confounders married personnel were at greater risk for postwar hospitalizations for all causes.23 Perhaps those who were married are at greater risk for postwar hospitalizations because they were likely to have a spouse also deployed to the Persian Gulf. These veterans might be experiencing even greater distress because of concerns about the well-being of their deployed spouses.
There are a few potential weaknesses of this study that deserve comment. First, because the HRA program was initiated in late 1987, there are relatively few HRAs from the prewar period, with the bulk of those used in this study coming from the years 1989 and 1990. However, because we are interested in prewar experiences of stressors or distress and health habits as they relate to postwar health, the close proximity of HRA measures we do have to the start of the ODS/DS period may also be considered a strength of this study. In addition, in spite of small samples, we are still able to demonstrate a significant difference in risk for depression and suicidal ideation in the prewar period. Second, the measures of health behaviors and life quality from the HRA are self-reported and cannot be validated directly by assessment of actual practices and life stressors. However, many studies have validated self-reported behaviors and found good correspondence between actual and reported behaviors. 32–38 The use of hospitalization diagnoses common among Army CCEP registrants may reduce the generalizability of our findings because not all veterans of the Persian Gulf chose to register or receive clinical evaluation under the CCEP program. Finally, the cohort defined here includes those who were on active duty for the entire ODS/DS period. Thus, individuals who enlisted during the war or who were discharged during the war are not included.
Conclusions
It seems unlikely, given these data, that any single prewar factor, such as excess stress, distress, difficulty coping, or poor health, will completely explain the health concerns and illnesses Gulf War veterans have experienced since the war. Our results suggest that the increased distress among Gulf War veterans compared with nondeployed Gulf War-era veterans found in some studies22.39–41 is probably best understood as a consequence of' the war experience rather than as a result elevated prewar levels of distress. However, the excess postwar injury mortality may be attributable to risk-taking habits or exposures that were present before deployment and that persisted even after the war. Although there is some cohesive evidence for excess risk-taking among deployers before the war, the strength of the evidence is weak. More information is needed documenting postwar risk-taking habits, particularly longitudinal data capable of documenting changes in habits that may have occurred after deployment.
Acknowledgments
The authors thank Dr. Catherine Spino for her statistical assistance with the development and interpretation of analytic models used in this paper and Dr. Thomas Mangione for his intellectual contributions in the early planning stages of these analyses.
This study was made possible by grant DAMD17-98-1-8610 from the U.S. Army Medical Research Acquisition Activity and by grant 1 R29 AA11407-01A1 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
The contents herein are the sole responsibility of the authors and do not necessarily represent the position or the policy of the U.S. Army Medical Research Acquisition Activity, the U.S. Army, the Department of Defense, or the National Institute on Alcohol Abuse and Alcoholism. No official endorsement should be inferred.
The CCEP was established in June 1994, upon the directive of the Department of Defense, to evaluate Gulf War veterans who were concerned about their health and to facilitate treatment for the myriad complaints and conditions experienced by Gulf War veterans.
DoD 1312.1–1. Occupational Conversion Index. Enlisted/Officer/Civilian. March 1997.
Major depressive disorder. single episode (296.20): neurotic depression (300.4): tension headache (307.81): prolonged post-traumatic stress disorder (309.81): depressive disorder. not elsewhere classified (311): migraine. unspecified (346.90): essential hypertension. unspecified (401.90): allergic rhinitis. cause unspecified (477.9): asthma. unspecified (493.90): esophageal reflux. without inflammation (530.81): irritable colon. not elsewhere specified (564.1): contact dermatitis and other eczema. unspecified cause (692.9): primary localized osteoarthrosis (715.18): osteoarthrosis. unspecified whether generalized or localized (715.90): unspecified arthralgia (719.40): lower leg arthralgia (719.46): multiple-site arthralgia (719.49): lumbago. not otherwise specified (724.2): myalgia and myositis. unspecified (729.1): other insomnia (not otherwise characterized) (780.52): other and unspecified sleep apnea (780.57): malaise and fatigue (780.7): other general symptoms. which may include amnesia (retrograde). chills not otherwise specified. generalized pain. and hypothermia not related to low environmental temperature (780.9): rash and other nonspecific skin eruptions (782.1): and headache. including facial pain and other pain in the head that is not otherwise specified (784.0) (TAIHOD. May 1999).
References
- 1.Writer JV, DeFraites RF, Brundage JF. Comparative mortality among US military personnel in the Persian Gulf region and worldwide during Operations Desert Shield and Desert Storm. JAMA. 1996;275:118–21. [PubMed] [Google Scholar]
- 2.Kang HK, Bullman TA. Mortality among US veterans of the Persian Gulf War. N Engl J Med. 1996;335:1498–504. doi: 10.1056/NEJM199611143352006. [DOI] [PubMed] [Google Scholar]
- 3.Perconte ST, Wilson A, Pontius E, et al. Unit-based intervention for Gulf War soldiers surviving a SCUD missile attack: program description and Preliminary findings. J Trauma Stress. 1993;6:225–38. [Google Scholar]
- 4.Labbate LA, Snow MP. Posttraumatic stress symptoms among soldiers exposed to combat in the Persian Gulf. Hosp Community Psychiatry. 1992;43:831–3. doi: 10.1176/ps.43.8.831. [DOI] [PubMed] [Google Scholar]
- 5.Southwick SM, Morgan A, Nagy LM, et al. Trauma-related symptoms in veterans of Operation Desert Storm: a preliminary report. Am J Psychiatry. 1993;150:1524–8. doi: 10.1176/ajp.150.10.1524. [DOI] [PubMed] [Google Scholar]
- 6.Southwick SM, Morgan CA, 3rd, Darnell A, et al. Trauma-related symptoms in veterans of Operation Desert Storm: a 2-year follow-up. Am J Psychiatry. 1995;152:1150–5. doi: 10.1176/ajp.152.8.1150. [DOI] [PubMed] [Google Scholar]
- 7.Haley RW, Kurt TL, Hom J. Is there a Gulf War syndrome? Searching for syndromes by factor analysis of symptoms. JAMA. 1997;277:215–22. [PubMed] [Google Scholar]
- 8.Haley RW, Hom J, Roland PS, et al. Evaluation of neurologic function in Gulf War Veterans: a blinded case-control study. JAMA. 1997;277:223–30. [PubMed] [Google Scholar]
- 9.Haley RW, Kurt TL. Self-reported exposure to neurotoxic chemical combinations in the Gulf War: a cross-sectional epidemiologic study. JAMA. 1997;277:231–7. [PubMed] [Google Scholar]
- 10.Centers for Disease Control. Unexplained illness among Presian Gulf War veterans in an Air National Guard Unit: preliminary report–August 1990-March 1995. JAMA. 1995;274:16–7. [PubMed] [Google Scholar]
- 11.Sloan P, Arsenault L, Hilsenroth M, Harvill L, Handler L. Rorschach measures of posttraumatic stress in Persian Gulf War veterans. J Pers Assess. 1995;64:397–414. doi: 10.1207/s15327752jpa6403_1. [DOI] [PubMed] [Google Scholar]
- 12.McCarroll JE, Ursano RJ, Fullerton CS. Symptoms of posttraumatic stress disorder following recovery of war dead. Am J Psychiatry. 1993;150:1875–7. doi: 10.1176/ajp.150.12.1875. [DOI] [PubMed] [Google Scholar]
- 13.McCarroll JE, Ursano RJ, Fullerton CS. Symptoms of PTSD following recovery of war dead: 13–15-month follow-up. Am J Psychiatry. 1995;152:939–41. doi: 10.1176/ajp.152.6.939. [DOI] [PubMed] [Google Scholar]
- 14.Joseph SC. A comprehensive clinical evaluation of 20,000 Persian Gulf War veterans: Comprehensive Clinical Evaluation Program evaluation Team. Milit Med. 1997;162:149–55. [PubMed] [Google Scholar]
- 15.Murphy FM, Kang H, Dalager NA, et al. The health status of Gulf War veterans: lessons learned from the Department of veterans Affairs Health registry. Milit Med. 1999;164:327–31. [PubMed] [Google Scholar]
- 16.Amato AA, McVey A, Cha C, et al. Evaluation of neuromuscular symptoms in veterans of the Persian Gulf War. Neurology. 1997;48:4–12. doi: 10.1212/wnl.48.1.4. [DOI] [PubMed] [Google Scholar]
- 17.Stretch RH, Bliese PD, Marlowe DH, Wright KM, Knudson KH, Hoover CH. Physical health symptomatology of Gulf War-era service personnel from the states of Pennsylvania and Hawaii. Milit Med. 1995;160:131–6. [PubMed] [Google Scholar]
- 18.Stretch RH, Marlowe DH, Wright KM, Bliese PD, Knudson KH, Hoover CH. Post-traumatic stress disorder symptoms among Gulf War veterans. Milit Med. 1996;161:407–10. [PubMed] [Google Scholar]
- 19.Spencer PS, McCauley LA, Joos SK, et al. US Gulf War veterans: service periods in theater, differential exposures, and persistent unexplained illness. Portland Environmental Hazards Research Centre. Toxicol Lett. 1998;102–103:515–21. doi: 10.1016/s0378-4274(98)00258-6. [DOI] [PubMed] [Google Scholar]
- 20.Proctor SP, Heeren T, White RF, et al. Health status of Persian Gulf War veterans: self-reported symptoms. environmental exposures and the effect of stress. Int J Epidemiol. 1998;27:1000–10. doi: 10.1093/ije/27.6.1000. [DOI] [PubMed] [Google Scholar]
- 21.West L, Mercer SO, Altheimer E. Operation Desert Storm: the response of a social work outreach team. Soc Work Health Care. 1993;19:18–98. doi: 10.1300/J010v19n02_04. [DOI] [PubMed] [Google Scholar]
- 22.The lowa Persian Gulf Study Group. Self-reported illness and health status among Gulf War veterans: a population-based study. JAMA. 1997;277:238–45. [PubMed] [Google Scholar]
- 23.Gray GC, Coate BD, Anderson CM, et al. The postwar hospitalization experience of US veterans of the Persian Gulf War. N Engl J Med. 1996;335:1505–13. doi: 10.1056/NEJM199611143352007. [DOI] [PubMed] [Google Scholar]
- 24.Amoroso PJ, Swartz WG, Hoin FA, Yore MM. Total Army Injury and Health Outcomes Database: Description and Capabilities, Army report TN97-2. Natick, MA: US Army Research Institute of Environmental Medicine; February 6, 1997. [Google Scholar]
- 25.Amoroso PJ, Yore MM, Weyandt B, Jones BH. A model comprehensive research database: Total Army Injury and Health Outcomes Database. Milit Med. 1999;164(suppl):8-l–8-36. [PubMed] [Google Scholar]
- 26.Bricknell MCM, Amoroso PJ, Yore MM. What is the risk associated with being a qualified military parachutist? Occup Med. 1999;49:139–45. doi: 10.1093/occmed/49.3.139. [DOI] [PubMed] [Google Scholar]
- 27.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 28.Fertig JB, Allen JP, Cross GM. CAGE as a predictor of hazardous alcohol consumption in U.S. Army personnel. Alcohol Clin Exp Res. 1993;17:1184–7. doi: 10.1111/j.1530-0277.1993.tb05225.x. [DOI] [PubMed] [Google Scholar]
- 29.Kang H, Bullman T. Mortality among US veterans of the Gulf War: update through December 1997. Proceedings of the Conference on Federally Sponsored Gulf War Veterans Illnesses Research; Arlington, VA. June 24, 1999. [Google Scholar]
- 30.Statistical Application Software (SAS), version 6.12. Cary, NC: SAS Institute; 1996. [computer program] [Google Scholar]
- 31.EpiInfo, version 6.04b. Atlanta, GA: Centers for Disease Control and Prevention; 1997. [computer program] [Google Scholar]
- 32.Bradley KA, Bush KR, McDonell MB, Malone T, Fihn SD. Screening for problem drinking: comparison of CAGE and AUDIT. Ambulatory Care Quality Improvement Project (ACQUIP), Alcohol Use Disorders Identification Test. J Gen Intern Med. 1998;13:379–88. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82:231–5. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 34.Harris TR, Wilsnack RW, Klassen AD. Reliability of retrospective self-reports of alcohol consumption among women: data from a US national sample. J Stud Alcohol. 1994;55:309–14. doi: 10.15288/jsa.1994.55.309. [DOI] [PubMed] [Google Scholar]
- 35.Hultsch DF, Hammer M, Small BJ. Age differences in cognitive performance in later life: relationships to self-reported health and activity life style. J Gerontol. 1993;48:1–11. doi: 10.1093/geronj/48.1.p1. [DOI] [PubMed] [Google Scholar]
- 36.Polich JM. The validity of self-reports in alcoholism research. Addict Behav. 1982;7:123–32. doi: 10.1016/0306-4603(82)90037-5. [DOI] [PubMed] [Google Scholar]
- 37.Stacy AW, Widaman KF, Hays R, DiMatteo MR. Validity of self-reports of alcohol and other drug use: a multitrait-multimethod assessment. J Pers Soc Psychol. 1985;49:219–32. doi: 10.1037//0022-3514.49.1.219. [DOI] [PubMed] [Google Scholar]
- 38.Wagenaar AC, Komro KA, McGovern P, Williams CL, Perry CL. Effects of a saliva test pipeline procedure on adolescent self-reported alcohol use. Addiction. 1993;88:199–208. doi: 10.1111/j.1360-0443.1993.tb00803.x. [DOI] [PubMed] [Google Scholar]
- 39.Perconte ST, Wilson AT, Pontius EB, Dietrick AL, Spiro KJ. Psychological and war stress symptoms among deployed and non-deployed reservists following the Persian Gulf War. Milit Med. 1993;158:516–21. [PubMed] [Google Scholar]
- 40.Unwin C, Blatchley N, Coker W, et al. Health of UK servicemen who served in Persian Gulf War. Lancet. 1999;353:169–78. doi: 10.1016/S0140-6736(98)11338-7. [DOI] [PubMed] [Google Scholar]
- 41.Stretch RH, Bliese PD, Marlowe DH, Wright KM, Knudson KH, Hoover CH. Psychological health of Gulf War-era military personnel. Milit Med. 1996;161:257–61. [PubMed] [Google Scholar]


