Abstract
Background/Objective:
Recurring annual costs of caring for patients with chronic spinal cord injury (SCI) is a large economic burden on health care systems, but information on costs of SCI care beyond the acute and initial postacute phase is sparse. The objective of this study was to establish a frame of reference and estimate of the annual direct medical costs associated with health care for a sample of patients with chronic SCI (ie, >2 years after injury).
Methods:
Patients were recruited from 3 Veterans Health Administration (VHA) SCI facilities; baseline patient information was cross-referenced to the Decision Support System (DSS) National Data Extracts (NDE) to obtain patient-specific health care costs in VHA. Descriptive statistical analysis of annual DSS-NDE cost of patients with SCI (N = 675) for fiscal year (FY) 2005 by level and completeness of injury was conducted.
Results:
Total (inpatient and outpatient) annual (FY 2005) direct medical costs for 675 patients with SCI exceeded $14.47 million or $21,450 per patient. Average annual total costs varied from $28,334 for cervical complete SCI to $16,792 for thoracic incomplete SCI. Two hundred thirty-three of the 675 patients with SCI who were hospitalized over the study period accounted for a total of 378 hospital discharges, costing in excess of $7.19 million. This approximated a cost of outpatient care received of $7.28 million for our entire sample.
Conclusions:
The comprehensive nature of health care delivery and related cost capture for people with chronic SCI in the VHA provided us the opportunity to accurately determine health care costs for this population. Future SCI postacute care cost analyses should consider case-mix adjusting patients at high risk for rehospitalization.
Keywords: Health economics, Health care costs, Spinal cord injuries, Tetraplegia, Paraplegia, Veterans Administration
INTRODUCTION
Nearly 253,000 people in the United States live with a disability related to a spinal cord injury (SCI) (1). Approximately 11,000 Americans are hospitalized for an SCI each year (2). Annual SCI costs are estimated to be $9.7 billion annually (3). The average yearly health care and living expenses vary greatly according to severity of injury, with estimated first-year injury costs ranging from $218,504 for incomplete motor function at any level to $741,425 for high tetraplegia (C1–C4) injuries (in May 2006 dollars) (4). Recurring annual cost of caring for patients with SCI is reported to be well below first-year treatment costs but is nonetheless a large economic burden on health care systems (4–8). Reported recurring costs in the United States ranged from $27,568 paraplegia to $54,400 for low tetraplegia (C5–C8) and up to $132,807 for high tetraplegia (C1–C4; in May 2006 dollars) (4).
The Veterans Health Administration (VHA) is one of the largest integrated health care systems in the United States, with more than 5 million unique patients in recent years and a large SCI population. According to the VHA Office of Public Affairs, there are nearly 44,000 eligible veterans with SCI, and the VHA provided care to 22,800 veterans with SCI and disorders who enrolled in the VHA (9). Many of these enrolled veterans choose to receive care outside of the VHA in any given year. In fiscal year (FY) 2004, the VHA SCI program accounted for approximately $716 million in direct medical costs for 18,539 enrolled veterans (VHA intranet) (10). Approximately two thirds (N = 12,257) of the 18,539 received specialized SCI programs services from the VHA in that year (9,10).
The purpose of this report is to establish a more refined frame of reference and estimate of the annual recurring direct medical costs associated with the postacute phase of care for a sample of patients with pre-existing SCI. Our population focus was patients who received specialty care at 3 VHA-designated treatment centers.
METHODS
Sources of Data
There are 23 designated SCI treatment centers in the VHA system. These 23 centers have referral regions and accept referrals from other VHA medical facilities (11). Patients were recruited from 3 designated SCI centers that are participating in a multisite SCI research program (Tampa, Augusta, and Boston VHA SCI Centers). Subjects were identified from regularly scheduled clinic visits designated as “annual evaluations” beginning in April 2004 and ending March 31, 2006. An annual evaluation was defined as “a comprehensive annual history/physical exam with specialty assessments”; offering an annual evaluation is mandated for patients with SCI in the VHA (11). The eligibility criteria were all veterans with SCI who use a wheelchair as a primary means of mobility and who had an SCI for at least 2 years. The focus of the underlying funded study was to identify patients with SCI at risk for wheelchair falls. Therefore, the eligibility criteria excluded patients with SCI injuries that did not warrant use of a wheelchair, had breaks in their use of wheelchairs because of periods of bedrest prescribed for longer than 1 month, or were ventilator-dependent patients who did not use a wheelchair as their primary means of mobility.
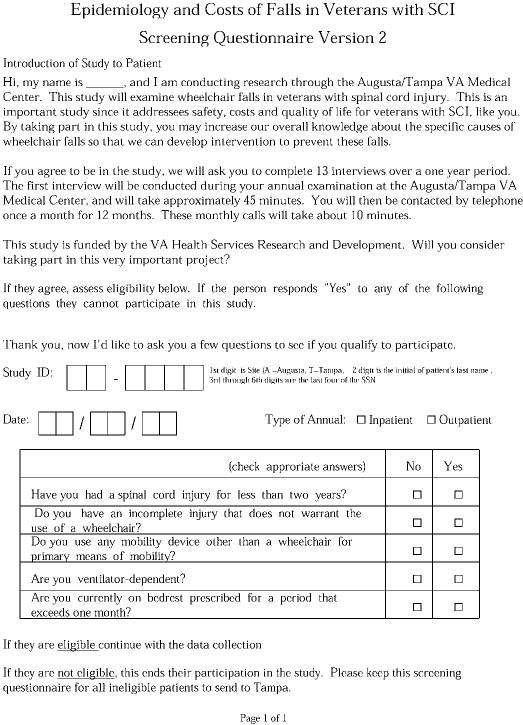
We administered a 16-page baseline survey (Figure 1) to obtain information on the level and extent of SCI injury, demographic data, and clinical information. The clinical information included data on injury level, diseases, medication use, physical activity levels, spasticity, fatigue and pain levels, alcohol consumption patterns, wheel-chair type and use patterns, and functional independence measures (FIM). The full survey is available on request from the authors. The baseline patient information was cross-referenced to the Decision Support System (DSS) National Data Extracts (NDE) to obtain patient-specific health care costs and use in the VHA. The DSS is a set of programs that uses relational databases to provide information needed by managers and clinicians, including the cost of specific patient care encounters (12). The DSS-NDE cost includes all outpatient and inpatient care costs provided or paid for by the VHA. Some examples of the costs included in the DSS-NDE are hospitalization and surgical costs, inpatient and outpatient pharmacy, radiology, laboratory, nursing care, prosthetics, rehabilitation, and nursing home care (12–14).
Figure 1. Page 1 of the 16-page screening questionnaire that was administered to potential participants in this study of the annual recurring direct medical costs associated with the postacute phase of caring for patients with pre-existing spinal cord injury. The full survey is available on request from the authors.
Statistical Analysis
We conducted a descriptive statistical analysis of the annual DSS-NDE cost of SCI patients (N = 675) for FY 2005 by level and extent of injury. Analyses were performed with SAS version 9.1 (15). This study was approved by all relevant Institutional Review Boards and complied with human subjects' protection standards.
RESULTS
Of the 1,049 patients with SCI who were asked to participate in the study, 59 refused (refusal rate of 5.6%), leaving 990 who were prescreened for eligibility (Figure 1). After implementing our eligibility criteria, 288 patients with SCI were deemed not eligible, leaving 702 patients who in turn, completed the baseline survey. The 288 patients with SCI were deemed ineligible, some for multiple reasons. In particular, 193 reported having an incomplete injury that did not warrant the use of a wheelchair; 205 used a mobility device other than a wheelchair for primary means of mobility; 40 were on bedrest prescribed for a period that exceeded 1 month; 3 were ventilator-dependent; and 39 patients had SCI for less than 2 years.
After cross-referencing the completed baseline surveys to the DSS-NDE, we retained 675 patients with SCI (mean age: 54.8 ± 12.6 [SD] years; median age, 55 years). There were 330 patients from Tampa, 319 from Augusta, and 26 from Boston. The loss of 27 patients from the analysis was because of the fact that we could not link the social security numbers from the survey instrument to the scrambled social security numbers in the DSS-NDE data at the Austin Automation Center (AAC). Our sample was 73.5% white, 22.0% black, 3.4% Hispanic, and 3.4% other or unknown. More than 95% of the sample were men, and 50.1% were married.
Overall, 47.4% of the SCI sample (N = 675) had cervical level injuries (N = 320), 45.7% were thoracic level (N = 309), and 5.9% were lumbar level (N = 46). Approximately 41.0% of the 675 SCIs were of the complete type. Patients in the study sample had very old injuries (mean duration after injury, 21.4 years; median, 20.0 years; 99% confidence interval [CI], 20.1–22.7 years). Preliminary regression analysis showed that the number of years after injury specified as a continuous or binary variable (eg, = 1 if 5–10 years after injury, = 0 otherwise) did not affect total costs in this study group; thus, costs were not described by years after injury. This was because of the lack of variation in years after injury.
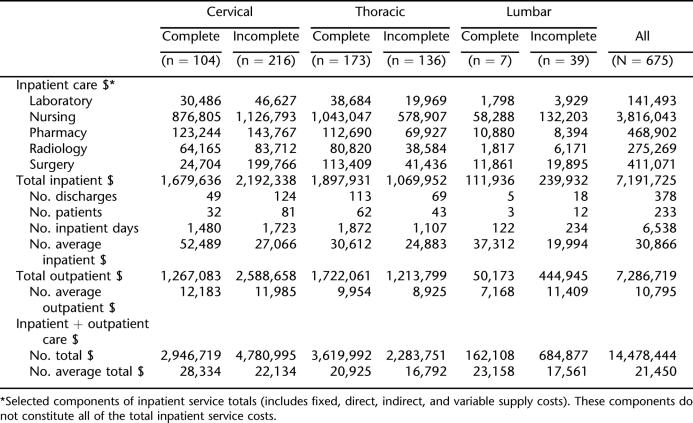
Table 1 shows the total direct medical costs for FY 2005 by level and extent of injury. The costs are displayed by selected DSS-NDE inpatient cost components, outpatient components, and total costs by the level and extent of the SCI. The nursing care inpatient cost component accounted for 53% of the total inpatient costs. Total (inpatient and outpatient) annual (FY 2005) direct medical costs for 675 patients with SCI exceeded $14.47 million or $21,450 per patient. The average annual total costs for FY 2005 ranged from $28,334 for
Table 1.
Use and Direct Health Care Costs by Level and Completeness of SCI (FY05)
Interestingly, 233 individuals who were hospitalized over the study period accounted for a total of 378 hospital discharges, costing in excess of $7.19 million. The top 5 major diagnostic categories (MDCs) for hospitalization were as follows: MDC-1 (nervous system) accounted for 90 of the 378 discharges, MDC-11 (kidney and urinary) accounted for 75 discharges, MDC-5 (circulatory) accounted for 44 discharges, MDC-6 (digestive) accounted for 43 discharges, and MDC-9 (skin, subcutaneous, and breast) accounted for 40 of the 378 hospital discharges. In all, the top 5 MDCs accounted for 292 of the 378 (77.2%) hospital discharges. The inpatient care costs were nearly equal to the cost of outpatient care received ($7.28 million) for our entire sample (N = 675). Hospitalization costs ranged from an average of $52,489 for cervical complete injuries to $19,994 for lumbar incomplete injuries. The average outpatient care costs ranged from $12,183 for cervical complete injuries to $7,168 for lumbar complete injuries (Table 1).
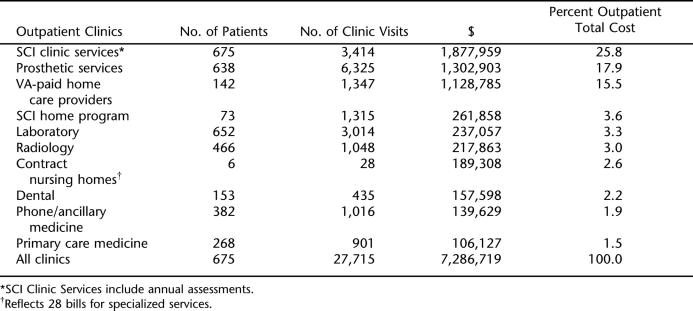
Table 2 shows the top 10 outpatient clinics by name and cost. The most costly and the most frequently visited outpatient clinics were SCI clinic and prosthetic services, respectively. Nearly 60% of the total outpatient costs were associated with 3 outpatient clinics (SCI clinic, prosthetic services, and VA-paid home care).
Table 2.
Top 10 Outpatient Clinic Costs and Uses (N = 675)
DISCUSSION
In contrast to the private sector, where care for people with chronic disabilities such as SCI (and related cost capture) is often fragmented, the VHA provides integrated and comprehensive health care services for patients with SCI. In addition, because of the VHA's sophisticated clinical and management information systems, one can accurately identify health care use and determine direct medical costs for this population. The results reported here provide data concerning the costs incurred well after the acute phase of treatment for veterans at 3 SCI centers.
Although it has been reported that significant direct medical costs are incurred in the first year of injury, people with chronic SCI may still have substantial recurring medical costs in subsequent years (4). Our findings showed that one half of the recurring total costs were associated with inpatient care. There were 378 hospital discharges for 233 of the 675 patients with SCI, with a total inpatient cost in excess of $7.19 million. One published study on the pattern of inpatient hospital use, up to 15 years after injury, among a cohort of veterans with SCI, found that the rates for the incidence of rehospitalization decreased rapidly in years 2 to 5 after injury and declined less rapidly thereafter (16). Efforts toward preventing rehospitalization should target persons with previous high use (16).
The leading cause of rehospitalization was previously reported as diseases of the genitourinary system, including urinary tract infections (UTIs) (17). Diseases of the respiratory system tended to be more likely in patients with tetraplegia (C1–C8 American Spinal Injury Association [ASIA] grades A, B, and C), whereas patients with paraplegia (T1–S5 ASIA grades A, B, and C) were more likely to be rehospitalized for pressure ulcers (17,18). Differentiating patients hospitalized from those not hospitalized, along with underlying clinical factors, is an important distinction in risk adjusting cost estimates.
Reported recurring costs in the United States ranged from $27,568 for paraplegia to $54,400 for low tetraplegia (C5–C8) and up to $132,807 for high tetraplegia (C1–C4; in May 2006 dollars) (4). In contrast, our findings were much lower when accounting for the level and extent of injury and varied from $28,334 for a cervical complete SCI to $16,792 for a thoracic incomplete SCI. However, our average costs for an incomplete motor functional injury at any level were higher at $19,820 compared with $15,313 (4).
Our findings showed that the hospitalization costs for a subset of our study sample were nearly equal to outpatient care costs for the entire sample. Because ventilator-dependent patients and those on bed rest for more than 1 month (eg, because of pressure ulcers) were not a focus of this study, it is likely that our cost estimates are lower than would have been had these relatively care-intensive subpopulations been included. These potentially high-cost patients will be the focus of a future cost and use study.
We note that our findings are based on 3 cooperating SCI centers and may not be generalizable to the rest of the VHA. Our study included 330 SCI patients from Tampa, 319 from Augusta, and 26 from Boston. In FY 2005, 871 SCI patients were treated at Tampa, 961 at Augusta, and 559 at Boston (19). According to the VHA's Allocation Resource Center (ARC) Special Disability Reports for Capacity and Planning, the average national VHA cost of a SCI disorder in FY 2005 was $24,360 for more than 12,000 unique patients with SCI (VHA intranet) (19). Our cost analysis based on levels of injury and extent were consistent with this national average cost. However, it must be noted that there is considerable variation in the average cost of care for patients with SCI by veterans integrated service network (VISN). For those VISNs with at least 400 unique patients with SCI treated in FY 2005, the average cost per patient with SCI at the VISN level ranged from $11,094 to $54,528 (VHA intranet) (19).
CONCLUSIONS
Research on the long-term costs of care for disabling injuries is important because it provides an empirical basis for policy makers to allocate resources, identifies important secondary conditions associated with the injury, and identifies particularly vulnerable subpopulations that are impacted (20). Our findings show that hospitalization costs for a subset of our study sample of patients with chronic SCI approximated the outpatient care costs for the entire sample. Future SCI postacute care cost analyses should consider case-mix adjusting patients at high risk for rehospitalization.
Footnotes
This study was supported by the Department of Veterans Affairs, Veterans Health Administration (VHA), Health Services Research & Development (HSR&D) Grant, IIR 03–003.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
REFERENCES
- University of Alabama. UAB Model SCI System. SCI facts and figures at a glance. June 2006. Available at: http://www.spinalcord.uab.edu/show.asp?durki=21446. Accessed June 7, 2007.
- Centers for Disease Control. CDC injury fact book. Available at: http://www.cdc.gov/ncipc/fact_book/25_Spinal_Cord_Injury.htm. Accessed December 6, 2006.
- Berkowitz M, O'Leary P, Kruse D, Harvey C. Spinal Cord Injury: An Analysis of Medical and Social Costs. New York: Demos Medical Publishing; 1998. [Google Scholar]
- University of Alabama. UAB Model SCI System. SCI facts and figures at a glance. Available at: http://www.spinalcord.uab.edu/show.asp?durki=19775&site=1021&return=19679. Accessed December 6, 2006.
- Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996;34:470–480. doi: 10.1038/sc.1996.81. [DOI] [PubMed] [Google Scholar]
- DeVivo MJ. Causes and costs of spinal cord injury in the United States. Spinal Cord. 1997;35:809–813. doi: 10.1038/sj.sc.3100501. [DOI] [PubMed] [Google Scholar]
- Dryden DM, Saunders LD, Rowe BH, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–525. doi: 10.1038/sj.sc.3101629. [DOI] [PubMed] [Google Scholar]
- Dryden DM, Saunders LD, Jacobs P, et al. Direct health care costs after traumatic spinal cord injury. J Trauma. 2005;59:443–449. doi: 10.1097/01.ta.0000174732.90517.df. [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs, Office of Public Affairs Media Relations. VA spinal cord injury fact sheet, May 2005. Available at: http://www1.va.gov/opa/fact/docs/spinalcfs.pdf. Accessed March 13, 2007.
- VHA. Decision support system (DSS) cost and utilization report for spinal cord injuries. Available at: http://klfmenu.med.va.gov. Accessed December 6, 2006.
- Department of Veterans Affairs, Office of Public Affairs Media Relations. Spinal cord injury system of care and procedures. VHA handbook 1176.1 Available at: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=1255. Accessed March 13, 2007.
- Health Economics Resource Center (HERC) Decision support system (DSS) user guides, presentations, and technical reports. Available at: http://www.herc.research.va.gov/data/dss.asp#Downloads. Accessed December 7, 2006.
- Health Economics Resource Center (HERC) Research guide to decision support system national cost extract 1998–2004. Available at: http://www.herc.research.va.gov/files/BOOK_413.pdf. Accessed March 13, 2007.
- Veterans Information Resource Center (VIReC) Research user guide: VHA decision support system (DSS) clinical national data extracts (NDEs) Available at: http://www.virec.research.va.gov/References/RUG/RUG-DSS00–04.pdf. Accessed December 7, 2006.
- SAS Institute. SAS Language: Reference, Versions 9. Cary, NC: SAS Institute; 2006. [Google Scholar]
- Samsa GP, Landsman PB, Hamilton B. Inpatient hospital utilization among veterans with traumatic spinal cord injury. Arch Phys Med Rehabil. 1996;77:1037–1043. doi: 10.1016/s0003-9993(96)90065-9. [DOI] [PubMed] [Google Scholar]
- Cardenas DD, Hoffman JM, Kirshblum S, et al. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–1763. doi: 10.1016/j.apmr.2004.03.016. [DOI] [PubMed] [Google Scholar]
- McKinley WO, Jackson AB, Cardenas DD, et al. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80:1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- US Department of Veterans Affairs Intranet. Special disability capacity patient reports (ARC reports) Available at: http://vaww.bdc.med.va.gov/reports/spdis/spec_disabilities05_toc.html. Accessed April 2, 2007.
- National Center for Injury Prevention and Control. CDC Injury Research Agenda. Atlanta, GA: Centers for Disease Control and Prevention; 2002. [Google Scholar]