Abstract
Objective
We sought to test whether variations across regions in end-of-life (EOL) treatment intensity are associated with regional differences in patient preferences for EOL care.
Research Design
Dual-language (English/Spanish) survey conducted March to October 2005, either by mail or computer-assisted telephone questionnaire, among a probability sample of 3480 Medicare part A and/or B eligible beneficiaries in the 20% denominator file, age 65 or older on July 1, 2003. Data collected included demographics, health status, and general preferences for medical care in the event the respondent had a serious illness and less than 1 year to live. EOL concerns and preferences were regressed on hospital referral region EOL spending, a validated measure of treatment intensity.
Results
A total of 2515 Medicare beneficiaries completed the survey (65% response rate). In analyses adjusted for age, sex, race/ethnicity, education, financial strain, and health status, there were no differences by spending in concern about getting too little treatment (39.6% in lowest spending quintile, Q1; 41.2% in highest, Q5; P value for trend, 0.637) or too much treatment (44.2% Q1, 45.1% Q5; P = 0.797) at the end of life, preference for spending their last days in a hospital (8.4% Q1, 8.5% Q5; P = 0.965), for potentially life-prolonging drugs that made them feel worse all the time (14.4% Q1, 16.5% Q5; P = 0.326), for palliative drugs, even if they might be life-shortening (77.7% Q1, 73.4% Q5; P = 0.138), for mechanical ventilation if it would extend their life by 1 month (21% Q1, 21.4% Q5; P = 0.870) or by 1 week (12.1% Q1, 11.7%; P = 0.875).
Conclusions
Medicare beneficiaries generally prefer treatment focused on palliation rather than life-extension. Differences in preferences are unlikely to explain regional variations in EOL spending.
Keywords: Medicare, health care costs, physician’s practice patterns, terminal care, patient satisfaction
There are wide variations in health care expenditures across regions in the United States.1 For example, Medicare expenditures in the last 6 months of life vary dramatically across hospital referral regions in the United States, ranging from a low of $8,366 per beneficiary in Grand Junction, Colorado, to a high of $21,123 in McAllen, Texas. Variations in end-of-life (EOL) spending reflect markedly different patterns of resource use at the end of life and not health differences among this group of very ill patients near death. In 2003, the mean number of days in the intensive care unit (ICU) in the last 6 months of life in Grand Junction was 1 day, compared with 5.6 days in McAllen, and 16.7% of Grand Junction beneficiaries died in an acute care hospital, compared with 45.1% in McAllen.1
Previous studies have shown that regions with greater overall EOL spending do not have better outcomes; mortality, quality of care, and patient satisfaction among cohorts of patients with common serious conditions are sometimes worse,2,3 as are perceptions of the quality of EOL care among bereaved family members.4 In contrast, higher spending regions do have a greater regional supply of specialists,5 hospital and ICU beds,6–9 and other technologies.10,11 Physicians who practice in high-intensity regions have a greater tendency to recommend tests, referrals, and treatments for patients described in structured vignettes and are less likely to refer to hospice.12,13 It is unknown whether these differences in supply and physician practice style reflect differences in preferences for treatment among patients who reside in these high-spending regions. Yet, the policy prescriptions for addressing these regional variations depend critically on whether they are the consequence of differences across regions in patient preferences, the consequence of physician “enthusiasm” or “supplier-induced demand,” or other factors related to the supply of health care capacity.14–16
We sought to determine whether EOL treatment preferences vary across regions with differing levels of EOL treatment intensity. We used a cross-sectional survey of Medicare beneficiaries to ascertain preferences and average Medicare spending for patients in their last 6 months of life living in the respondents’ hospital referral region of residence as the measure of intensity. The central hypothesis of our study was that preferences for greater intensity of medical treatment in the event of a terminal illness would be positively associated with higher levels of regional intensity. Under the null hypothesis, in which regional preferences do not vary by regional intensity, there will be no relationship between individual beneficiaries’ preferences and the EOL spending of the region in which they reside.
METHODS
Study Population
The sampling frame was all Medicare beneficiaries in the Centers for Medicare and Medicaid 20% denominator file who were age 65 or older on July 1, 2003, alive, and entitled to part A, part B, or both, between July 1, 2003, and June 30, 2004, and residents of a US hospital referral region in 2003 and 2004 (N = 6,384,199). We drew a simple random sample of 4000 from this frame, obtained names and addresses from the Centers for Medicare and Medicaid Services (CMS), and identified telephone numbers from an electronic telephone matching service and directory assistance for a dual-mode survey (telephone administration followed by mailing a questionnaire to all for whom we could not obtain a telephone number or who had not responded by telephone). Exclusion criteria upon contact included those who were deceased or institutionalized.
Survey
Development
We designed the survey instrument to assess beneficiaries’ preferences for tests, treatments, and referrals for common health care conditions and their general concerns, goals, and preferences for care in the event of a terminal illness, in addition to sociodemographics, health status, social networks, perceptions of health care quality, and access to and use of health services in the previous 12 months. A nearly final version of the instrument was cognitively tested with 15 seniors in intensive one-on-one interviews to test construct validity and to make sure we were asking questions that people consistently can understand and can answer. The computer-assisted telephone interview (CATI) then underwent pilot testing with 20 seniors. We audiotaped and behavior-coded the pilot interviews for interviewer-respondent interaction to identify questions that were difficult to administer in a standardized format or that were difficulut for respondents to understand and revised the survey accordingly.
Administration
This dual-language, mixed-mode survey was fielded between March and October 2005. Bilingual (English/Spanish) telephone interviewers were available for those who preferred to be interviewed in Spanish. If we could not contact the beneficiary by phone after a minimum of 6 call attempts to administer the CATI, we mailed a dual-language, Canadian-style questionnaire that paralleled the telephone interview, along with a 5-dollar cash incentive. A thank you/reminder postcard was mailed 2 weeks later and mail nonrespondents were sent a replacement questionnaire packet (without a cash incentive) about 4 weeks after the initial mailing.
Measures
Local Health Care Intensity
We used a previously derived Medicare spending measure, the End-of-Life Expenditure Index, as our measure of local intensity. This measure is calculated as average per capita spending (as determined by standardized national prices) on hospital and physician services provided to Medicare fee-for-service beneficiaries age 65 and older during their last 6 months of life, adjusted for age, sex, and race. It reflects the component of local Medicare spending that is attributable to the overall quantity of medical services provided, not to local differences in illness or price.2,3 For the remainder of the article, we will refer to this measure as “EOL spending.” We assigned each respondent to 1 of 306 hospital referral regions based upon their zip code of residence. We then used each hospital referral region’s 2000–2003 EOL spending to assign the respondent to 1 of 5 quintiles: Q1: $8,366–$12,350, Q2: $12,351–$13,682, Q3: $13,683–$14,686, Q4: $14,687–$16,280, and Q5: $16,281–$21,123. We report EOL spending, last 6 month hospital days, ICU days, proportion of decedents seeing more than 10 different doctors, and proportion who died in an acute care hospital in each of these 5 quintiles in Table 1.
TABLE 1.
Differences in 2000 Medicare Spending and Resource Use, by Quintile of EOL Spending*
| Quintile of EOL Spending
|
|||||
|---|---|---|---|---|---|
| 1 (Lowest) | 2 | 3 | 4 | 5 (Highest) | |
| Per-capita EOL spending† | $11,337 | $13,155 | $14,175 | $15,449 | $17,772 |
| Service use, last 6 mo of life | |||||
| Inpatient days | 7.7 | 9.9 | 10.6 | 11.3 | 14.4 |
| ICU days | 2.0 | 2.7 | 3.0 | 3.5 | 4.9 |
| Physician visits | 18.6 | 24.2 | 26.3 | 31.0 | 43.4 |
| >10 different MDs, % | 18.9 | 24.5 | 26.8 | 30.5 | 42.0 |
| Died in hospital, % | 25.4 | 29.8 | 31.1 | 30.9 | 34.4 |
Data from the Dartmouth Atlas.
Age-sex-race and price-adjusted mean Medicare spending on hospital and physician services among beneficiaries in their last 6 mo of life, also known as the End-of-Life Expenditure Index (EOL-EI).
Medicare Beneficiaries’ EOL Concerns, Goals, and Preferences
We used responses to 6 survey questions to create 7 dichotomous outcome variables for the current study (Table 2). When dichotomizing responses, we treated answers other than “yes” or “no” (eg, “not concerned” or “I don’t know”) as missing data. Outcomes included concern about receiving too little medical treatment in the last year of life or receiving too much medical treatment, preference for dying in an acute care hospital, for life-prolonging drugs with side-effects, for palliative drugs with potential for life-shortening, and for mechanical ventilation. Item nonresponse was less than 1% among eligible respondents for each outcome measure.
TABLE 2.
Survey Questions, Response Options, and Associated Study Outcome Variable
| Introduction: The next set of questions is about care a patient may receive during the last months of life. Remember, you can skip any questions you don’t want to answer. Suppose that you had a very serious illness. Imagine that no one knew exactly how long you would live, but your doctors said you almost certainly would live less than 1 yr. | |
| Survey Question and Response Options | Outcome Variable |
| Q E9. In that situation, would you be more concerned that you would receive too little medical treatment or too much medical treatment? [too little,* too much, not concerned, don’t know†] | Too little |
| Q E9. In that situation, would you be more concerned that you would receive too little medical treatment or too much medical treatment? [too little, too much,* not concerned, don’t know†] | Too much |
| Q E10. If that illness got worse, where would you like to spend your last days—in a hospital, a nursing home, or at home? [hospital†, nursing home, home, don’t know‡] | Hospital |
| Q E11. To deal with that illness, do you think you would want drugs that would make you feel worse all the time but might prolong your life? [yes†, no, don’t know‡] | Prolong |
| Q E12. If you reached the point at which you were feeling bad all the time, would you want drugs that would make you feel better, even if they might shorten your life? [yes,* no, don’t know†] | Palliate |
| Q E13. If you needed a respirator to stay alive, and it would extend your life for a week, would you want to be put on a respirator? [yes,* no, don’t know†] | Mechanical Ventilation (MV) 1 wk |
| Respondents who answered no to Q E13, above, were asked: Q E14. If it would extend your life for a month, would you want to be put on a ventilator? [yes,* no, don’t know‡] | Mechanical Ventilation (MV) 1 mo |
The underlined option indicates the option used to create the outcome variable.
“Not concerned” and “don’t know” responses were treated as missing data for regression models.
Covariates
In addition to questions about EOL concerns and preferences, the survey collected extensive information about beneficiary attributes. Covariates in our analyses included the respondent’s age, sex, race/ethnicity, education, whether the beneficiary reported financial strain, and 3 self-reported health status measures.
Statistical Analysis
We display results according to quintile of intensity; however, all reported tests for trend are based on logisitic regression in which the independent variable is the EOL spending in the beneficiary’s hospital referral region of residence (expressed as a continuous variable, the mean per capita EOL spending dollar value in the hospital referral region) and the dependent variable is the beneficiary’s (dichotomized) response. Although our primary hypothesis is related to measuring whether patient preferences help to determine regional differences in EOL treatment intensity (spending), our statistical analysis includes EOL spending as the independent variable because it is measured accurately. Patient preferences (measured at the patient level) are the dependent variables. Thus, our statistical tests reflect an association between EOL spending and patient preferences, rather than the causal effect of patient preferences on EOL spending.
We performed multivariable logistic regression for each of the 7 outcomes, with EOL spending in the beneficiary’s hospital referral region of residence as the exposure (expressed as a continuous variable), adjusting for age, sex, race/ethnicity, education, financial strain, and health status. We also used an ordered logistic regression for the first survey question (Table 2) with a 3-level dependent variable: too little, not concerned, too much. We created an index of responses to each survey question (worry about too little medical treatment, preference for hospital death, life prolonging drugs, avoiding life-shortening palliative drugs, and wanting mechanical ventilation for 1 week and 1 month’s life extension) where a desire for the more intensive option increased the index by one. We then used linear regression to explore the relationship between EOL spending and the summed index, adjusting for age, sex, race/ethnicity, education, financial strain, and health status.
All multivariable regressions use the Huber/White/sandwich estimator of variance to adjust standard errors for clustering of respondents within hospital referral regions. We performed all statistical analyses using STATA 9.1 (Stata-Corp, College Station, TX).
Human Subjects and Role of the Funding Sources
The study was approved by the the Committee for the Protection of Human Subjects at Dartmouth Medical School and the Institutional Review Board (IRB) of the University of Massachusetts Boston and deemed exempt from the requirement for written informed consent. The data analysis plan was similarly considered exempt by the University of Pittsburgh IRB. This study was reviewed by the CMS to ensure protection of beneficiary confidentiality. The authors had full independence from the funding agency, the National Institute on Aging, and CMS in the design, conduct, analysis, and reporting and all authors had full access to the primary data.
RESULTS
Sample Characteristics
We attempted to contact 4000 beneficiaries, 160 of whom were discovered to be ineligible (dead or institutionalized). Of the eligible 3840, a total of 2515 responded for a 65% response rate (completed interviews divided by the number of eligible sample members, including refusals and all cases of unknown eligibility). Of those, 1384 (55%) responded by telephone (mean completion time, 22 minutes) and 1130 (45%) by mail (1 responded in a mixed format). Approximately 6% of the sample (n = 222) actively refused participation. Other reasons for nonresponse included those who were unable to complete the interview because of cognitive or physical debility (n = 59), language barrier (n = 3), and those who could not be contacted by phone and did not respond to 2 waves of mailings (n = 1041).
The oldest old (85+), nonwhites, and those with no doctor visits in the preceding year were the least likely to respond by telephone. With the addition of the mail mode, the final group of respondents looked more like the total sample than the group of respondents that would have resulted based on telephone alone.
The mean age of respondents was 75.6 (SD 6.6), 42.2% were men, 85.0% non-Hispanic white, 6.3% black, 4.6% Hispanic, 4.2% other race, 20.8% had not completed high school, 29.8% reported financial issues were very important in deciding whether to obtain medical care, 28.0% were in fair or poor health, 14.0% in fair or poor mental/emotional health, and 56.3% reported having physical or medical conditions that often cause pain or discomfort (Table 3). Compared with the group of beneficiaries from which our simple random sample of 4000 was selected, the respondents had a similar distribution of sex and education (using zip code-level Census imputation), but fewer persons age 85+ (9.7% vs. 14.7%) and blacks (6.3% vs. 8.1%); Hispanic ethnicity data from the enrollment file is not strictly comparable to our survey self-report data.
TABLE 3.
Sample Characteristics
| Characteristic | Sample n/N (%)* |
|---|---|
| Age 65–69 | 526/2471 (21.3) |
| Age 70–74 | 671/2471 (27.2) |
| Age 75–79 | 588/2471 (23.8) |
| Age 80–84 | 443/2471 (17.9) |
| Age 85 or older | 243/2471 (9.8) |
| Male | 1048/2483 (42.2) |
| Non-Hispanic white† | 2105/2478 (85.0) |
| Black† | 157/2478 (6.3) |
| Hispanic† | 113/2478 (4.6) |
| Other race/ethnicity† | 103/2478 (4.2) |
| No high school diploma | 511/2461 (20.8) |
| Financial strain‡ | 736/2473 (29.8) |
| Fair or poor general health | 691/2465 (28.0) |
| Fair or poor mental/emotional health | 347/2476 (14.0) |
| Pain or discomfort often | 1385/2462 (56.3) |
Nonmissing responses from the overall sample of 2515.
We categorized self-reported race and ethnicity into mutually exclusive groups of non-Hispanic white, black, Hispanic, or “other,” assigning multi-racial or ethic respondents using the hierarchy: black > Hispanic > other (Asian, Native Hawaiian or Pacific Islander, American Indian/Alaskan Indian/Alaskan Native, or Other) > non-Hispanic white. If respondents endorsed a racial category but had missing data for Hispanic ethnicity, we assumed they were non-Hispanic; this included 28 blacks, 100 whites, and 14 “others.”
We categorized respondents as having financial strain if they indicated that financial issues were “very important” in deciding whether to obtain medical care.
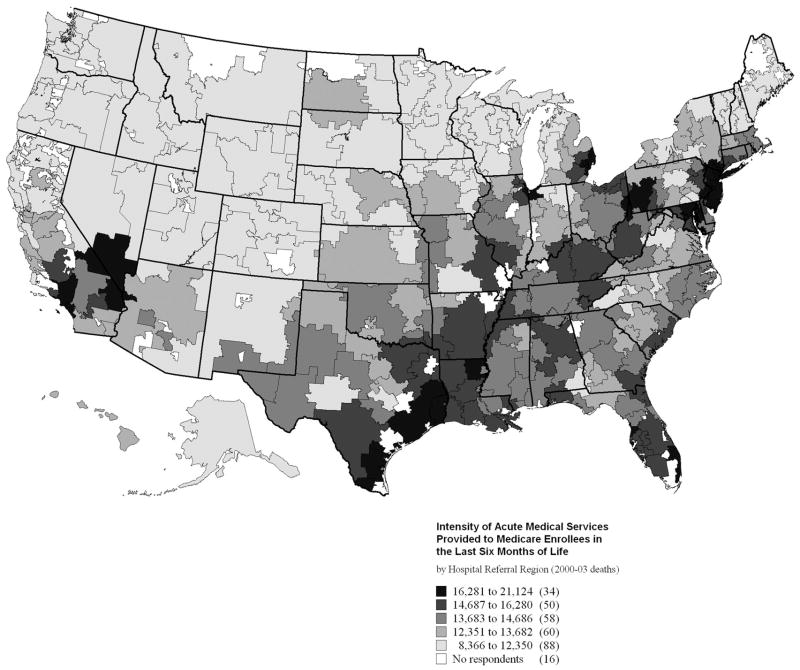
Survey respondents included beneficiaries from 290 of the 306 US hospital referral regions (Fig. 1). Roughly 20% of beneficiaries were drawn from hospital referral regions (HRRs) in each of the EOL spending quintiles (Table 4). Across these quintiles, the distribution of age, sex, financial strain, and health status were similar. In contrast, black race, Hispanic ethnicity, and lower educational achievement were not uniformly distributed; there was a greater prevalence of these characteristics in some of the higher intensity regions.
FIGURE 1.
Intensity of acute medical services provided to Medicare enrollees in the last 6 months of life, by hospital referral region (2000–2003). HRRs are color-coded by the mean per-capita Medicare spending in dollars on hospital and physician services among fee-for-service beneficiaries in their last 6 months of life who reside in the HRR. Thirty-four HRRs contributed to the highest qunitile of spending (depicted in black) and 88 HRRs contributed to the lowest quintile (depicted in lightest gray). There were no study respondents from 16 of 306 total HRRs (depicted in white).
TABLE 4.
Characteristics of Respondents by EOL Spending Quintile
| Quintile of End-of-Life Spending* |
||||||
|---|---|---|---|---|---|---|
| Characteristic | 1 (Lowest) (n = 542) | 2 (n = 474) | 3 (n = 468) | 4 (n = 492) | 5 (Highest) (n 3 539) | χ2P |
| Age 85 or older, % | 10.5 | 9.9 | 8.0 | 8.7 | 11.7 | 0.326 |
| Male, % | 44.3 | 41.4 | 42.6 | 42.9 | 39.9 | 0.656 |
| Non-Hispanic white, % | 91.4 | 86.7 | 83.8 | 86.0 | 77.0 | <0.0001 |
| Black, % | 1.1 | 4.5 | 8.4 | 7.2 | 10.6 | <0.0001 |
| Hispanic, % | 3.4 | 3.6 | 4.3 | 3.7 | 7.5 | 0.006 |
| Other, % | 4.1 | 5.1 | 3.5 | 3.1 | 4.9 | 0.414 |
| No high school diploma, % | 15.9 | 21.9 | 22.3 | 23.1 | 21.1 | 0.036 |
| Financial strain, % | 29.7 | 29.5 | 30.3 | 29.6 | 29.8 | 0.999 |
| Fair or poor general health, % | 26.4 | 31.3 | 26.3 | 29.0 | 27.5 | 0.386 |
| Fair or poor mental/emotional health, % | 12.4 | 16.6 | 16.0 | 13.2 | 12.4 | 0.163 |
| Pain or discomfort often | 56.4 | 57.5 | 56.8 | 56.7 | 54.1 | 0.846 |
Respondents resided in 1 of 290 (of 306 possible) US HRRs. The number of respondents in each of these HRRs ranged from 1 to 61. Each respondent’s HRR of residence was categorized into 1 of 5 quintiles of EOL spending based upon 2000–2003 per-capita Medicare spending on hospital and physician services among beneficiaries in their last 6 months in that HRR. Spending ranges, by quartile are: Q1 (lowest): $8,366–$12,350, Q2: $12,351–$13,682, Q3: $13,683–$14,686, Q4: $14,687–$16,280, and Q5 (highest): $16,281–$21,123.
EOL Concerns and Preferences
Faced with a hypothetical terminal illness, the respondents were almost evenly split between those who were concerned about getting too little treatment (40.4%) and those who were concerned about too much treatment (45.0%); the remainder were unconcerned (6.3%) or did not know (8.3%). Most preferred to spend their last days at home (86.0%) rather than in a hospital (9.1%) or nursing home (4.9%). Most did not want potentially life-prolonging drugs that made them feel worse all the time (83.9%), although a significant minority did (16.1%). Most wanted palliative drugs, even if they might be life-shortening (71.7%); 24.3% did not and 4.0% did not know. Most (87.4%) would not want to be put on a ventilator to gain 1 week’s life extension, but even if the gain were 1 month, 77.4% would still not want mechanical ventilation.
EOL Concerns and Preferences by EOL Spending
In crude analyses, there were no difference in respondents’ EOL treatment concerns and preferences by EOL spending with 1 exception: respondents in the lower quinitles of regional intensity were more likely to want palliative drugs that might be life-shortening (Q1 = 79.9%, Q2 = 75.5%, Q3 = 75%, Q4 = 68%, Q5 = 74.5%, P = 0.012; Fig. 2, left panel). In multivariable analyses adjusted for age, sex, race/ethnicity, education, financial strain, self-reported overall health, mental/emotional health, and frequent pain/discomfort, this difference was no longer statistically significant (Q1 = 77.7%, Q2 = 76.5%, Q3 = 75.9%, Q4 = 75.0%, Q5 = 73.4%, P = 0.138; Fig. 2, right panel).
FIGURE 2.
Proportion of beneficiaries living in regions with differing levels of EOL spending reporting particular EOL treatment concerns and preferences. Crude (left panel) and adjusted (right panel) results are presented. Responses are summarized by quintile of EOL spending, but P values are drawn from models with hospital referral region-level EOL spending entered as a continuous dollar figure, not a categorical variable. *Adjusted for age, sex, race/ethnicity, education, financial strain, and health status. MV indicates mechanical ventilation.
Findings were unchanged when respondents’ answers to the survey question about worry regarding the amount of medical care they would receive in the last year of life was modeled as a three-level ordinal variable: too little, not concerned, too much (crude P = 0.381, adjusted P = 0.911).
Among the 1595 respondents with no missing data for all 6 survey questions, the mean number of endorsements of the more intensive response was 1.31 (SD = 1.08, range, 0–5), and EOL spending in the respondent’s hospital referral region of residence was not associated with number of endorsed items (crude P = 0.094, adjusted P = 0.451).
DISCUSSION
Among a national sample of Medicare beneficiaries older than the age of 65, most prefer treatment focused on palliation rather than life-extension. We did not find a pattern of greater concern about receiving too little medical treatment, less concern about receiving too much medical treatment, preference for spending one’s last days in a hospital, for life-prolonging drugs despite side-effects, and for mechanical ventilation to achieve 1 week’s and 1 month’s life extension across respondents living in regions with progressively greater EOL spending. The observed relationship between respondents’ preferences for avoiding potentially life-shortening palliative drugs and greater spending regions was explained by the confounding effect of race/ethnicity. Taken together, the lack of cross-sectional association between preferences and spending in our study is unsupportive of the hypothesis that differences in preferences explain regional variations in EOL spending.
It is perhaps unsurprising that we did not find a relationship between individual patient preferences and local practice patterns, since the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (SUPPORT) demonstrated that preferences are seldom correctly ascertained,17 let alone heeded.6 However, unlike SUPPORT, we did not correlate actual treatment received with stated preferences. Our findings of lack of cross-sectional association using regional aggregate spending does not refute causality, and further, are potentially subject to the ecological fallacy. That is, although there is an association in aggregate, this association may not exist at the individual level.
Another limitation is the reliance upon a hypothetical scenario. Both the certainty of the prognosis and physicians’ willingness to articulate it may be unrealistic. Furthermore, we ascertained stated, not revealed preferences. It is possible that in the event of an actual life-threatening illness, individuals in higher intensity regions might behave differently than they indicated in response to the hypothetical scenario. Younger, healthier Medicare beneficiaries may not have sufficient experience with EOL decision making to reliably predict their preferences; to address this concern, we restricted the analysis only to respondents 75 or older, and our findings were unchanged. Furthermore, we adjusted all analyses for 3 health status measures, none of which were statistically significant predictors of any of the outcomes in our full models. Nonetheless, these remain important concerns because preferences are not entirely stable over time,18 particularly for those in declining health.19
The particular survey items were intentionally oversimplified to gain insight into broad concerns, goals, and preferences, rather than to anticipate particular treatment choices, and, as such were not as nuanced as required for advance care planning.20 With regard to the question about mechanical ventilation, we did not specify to the respondents the circumstances of their 1 week or 1 month’s life extension; some may have anticipated the reprieve to be lived in good health, while others may have understood the extension to be while still on the ventilator.
There was statistically significant pairwise correlation (with Bonferroni correction) for 10 of 21 outcome pairs. Not surprisingly, similar questions were highly correlated, for example between mechanical ventilation for 1 week and mechanical ventilation for 1 month (r = 0.75, P < 0.001), whereas others were less closely correlated, for example, between between mechanical ventilation for 1 week and worry about “too little” medical treatment (r = −0.11, P < 0.001). We sought a pattern of differences across all 7 outcomes, and indeed found neither a pattern nor significant differences on any single outcome. Some might argue that the lack of a difference on the responses to the questions regarding worry about getting too much or too little treatment indicates that respondents actually are getting just the kind of treatment they want across regions with differing spending levels. (Otherwise they’d be worried about getting too much in the higher spending regions.) Such an inference, however, would be inconsistent with the responses to the questions about specific services, which suggested that preferences and values for EOL care differ little across regions. Perhaps respondents are similar across regions in their values and preferences, but they observe only the intensity of care in their own region, and thus have little basis for judging what is “too much” or “too little.”
The EOL spending measure is based upon hospital and physician services only. It is possible systematic bias exists because of the exclusion of spending from other Medicare benefit cateories, such as hospice, home health, skilled nursing, and long-term acute care, if there is a greater likelihood of substitution of these services for acute care services in lower spending regions. Indeed, as shown by Pritchard and by Virnig, nursing home bed and hospice availability and use are inversely correlated with hospital as the place of death. On the other hand, nursing home bed availability is positively correlated with hospital bed availability and use more generally.8 Ultimately, this systematic bias is unlikely given the high correlation between hospital referral region-level EOL spending and hospital referral region-level overall spending (year 2000 r = 0.82, P < 0.0001). Indeed, during the last 2 decades, the substitution of these services has displaced the use of hospital acute care services at the end of life, but has not decreased the growth of total EOL Medicare expenditures.21,22
Finally, there was a 35% nonresponse rate to our survey. Although there was not a greater rate of nonresponse in the higher quintiles, it is still theoretically possible that selection bias produced the observed null result. For this to have occurred, beneficiaries preferring more intensive care would have had to be systematically more likely to be nonresponders in the higher intensity regions than in the lower intensity regions, which seems unlikely.
In summary, the results of this survey do not support the hypothesis that observed regional variations in EOL spending are attributable to differences in goals and preferences for care among residents of those regions. Longitudinal study of patients, their preferences, and their health care utilization is a natural next step in disconfirming this hypothesis.
Acknowledgments
We thank Renee Mentnech at CMS for identifying the study sample and for comments on the manuscript and Judith Lave at the University of Pittsburgh for her feedback on several versions of the manuscript.
Supported by National Institute on Aging (NIA) grant PO1 AG19783. Dr. Barnato was supported by NIA career-development grant K08 AG021921.
Footnotes
Presented at the Society of General Internal Medicine Annual Meeting in Los Angeles, CA on April 28, 2006.
References
- 1.Wennberg JE, Cooper M. [Accessed January 2, 2007];The Dartmouth Atlas of Health Care. Available at: www.dartmouthatlas.org.
- 2.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 3.Fisher ES, Wennberg DE, Stukel TA, et al. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 4.Teno JM, Mor V, Ward N, et al. Bereaved family member perceptions of quality of end-of-life care in U.S. regions with high and low usage of intensive care unit care. J Am Geriatr Soc. 2005;53:1905–1911. doi: 10.1111/j.1532-5415.2005.53563.x. [DOI] [PubMed] [Google Scholar]
- 5.Welch WP, Miller ME, Welch HG, et al. Geographic variation in expenditures for physicians’ services in the United States [see comments] N Engl J Med. 1993;328:621–627. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- 6.Pritchard RS, Fisher ES, Teno JM, et al. Influence of patient preferences and local health system characteristics on the place of death. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Risks and Outcomes of Treatment [see comments] J Am Geriatr Soc. 1998;46:1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- 7.Wennberg JE, Freeman JL, Shelton RM, et al. Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989;321:1168–1173. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]
- 8.Fisher ES, Wennberg JE, Stukel TA, et al. Hospital readmission rates for cohorts of Medicare beneficiaries in Boston and New Haven. [see comments] N Engl J Med. 1994;331:989–995. doi: 10.1056/NEJM199410133311506. [DOI] [PubMed] [Google Scholar]
- 9.Strauss MJ, LoGerfo JP, Yeltatzie JA, et al. Rationing of intensive care unit services. An everyday occurrence. JAMA. 1986;255:1143–1146. [PubMed] [Google Scholar]
- 10.Gatsonis CA, Epstein AM, Newhouse JP, et al. Variations in the utilization of coronary angiography for elderly patients with an acute myocardial infarction. An analysis using hierarchical logistic regression. Med Care. 1995;33:625–642. doi: 10.1097/00005650-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 11.McClellan M. Uncertainty, health-care technologies, and health-care choices. Am Econ Rev. 1995;85:38–44. [PubMed] [Google Scholar]
- 12.Sirovich BE, Gottlieb DJ, Welch HG, et al. Variation in the tendency of primary care physicians to intervene. Arch Intern Med. 2005;165:2252–2256. doi: 10.1001/archinte.165.19.2252. [DOI] [PubMed] [Google Scholar]
- 13.Sirovich BE, Gallagher P, Wennberg DE, et al. Does local health care spending reflect the decisions made my individual physicians? [abstract] J General Intern Med. 2005;20(Suppl 1):77. [Google Scholar]
- 14.Wennberg JE, Barnes BA, Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med. 1982;16:811–824. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- 15.Grytten J, Sorensen R. Type of contract and supplier-induced demand for primary physicians in Norway. J Health Econ. 2001;20:379–393. doi: 10.1016/s0167-6296(00)00087-4. [DOI] [PubMed] [Google Scholar]
- 16.Skinner JS, Wennberg JE. Regional inequality in Medicare spending: the key to Medicare reform. In: Garber AM, editor. Frontiers in Health Policy. Vol. 3. Cambridge, MA: MIT Press; 2000. [Google Scholar]
- 17.SUPPORT Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 18.Kohut N, Sam M, O’Rourke K, et al. Stability of treatment preferences: although most preferences do not change, most people change some of their preferences. J Clin Ethics. 1997;8:124–135. [PubMed] [Google Scholar]
- 19.Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890–895. doi: 10.1001/archinte.166.8.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 21.Barnato AE, McClellan MB, Kagay CR, et al. Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res. 2004;39:363–375. doi: 10.1111/j.1475-6773.2004.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garber AM, MaCurdy T, McClellan M. Medical care at the end of life: diseases, treatment patterns, and costs. In: Garber AM, editor. Frontiers in Health Policy Research. Vol. 2. Cambridge, MA: MIT Press; 1999. [Google Scholar]