Abstract
Adoptive immunotherapy with donor lymphocyte infusions (DLI) is an effective treatment for relapsed chronic myeloid leukemia (CML) after allogeneic stem cell transplantation. To identify the effector and target cell populations responsible for the elimination of the leukemic cells in vivo we developed an assay to measure the frequency of T lymphocyte precursor cells capable of suppressing leukemic progenitor cells. Target cells in this assay were CML cells that were cultured in the presence of stem cell factor, interleukin 3, granulocyte–macrophage colony-stimulating factor, granulocyte colony-stimulating factor, and erythropoietin. [3H]thymidine incorporation at day 7 represented the proliferation of the progeny of the CD34+ CML progenitor cells, and not of the more mature CD34− CML cells. Effector cells were mononuclear cells, which were used in a limiting dilution analysis to measure the frequencies of CML progenitor cell-inhibitory lymphocyte precursors (PCILp) in peripheral blood of seven patients before and after DLI for relapsed CML. In the six patients who entered complete remission, a 5- to 100-fold increase of PCILp was found during the clinical response. In the patient with resistant relapse the frequency of PCILp was <10 per ml before and after DLI. Leukemia-reactive helper T lymphocyte precursor frequencies remained unchanged after DLI. A significant increase in cytotoxic T lymphocyte precursor frequency against more mature leukemic cells was found in only two responding patients. These results indicate that T cells specifically directed against CD34+ CML progenitor cells mediate the antileukemic effect of DLI.
Allogeneic stem cell transplantation (SCT) is potentially curative in patients with chronic myeloid leukemia (CML) not only by the cytoreductive effects of irradiation and chemotherapy, but also by a graft-versus-leukemia effect (1). Clinical evidence for this effect by the immunocompetent cells in the stem cell graft is supported by a lower risk of relapse in patients with graft-versus-host disease (GvHD) after transplantation (2), and an increased risk of relapse in patients treated with a syngeneic transplant (3) or a T cell-depleted transplant (4–6). Moreover, the transfusion of lymphocytes from the original stem cell donor in patients with a cytogenetic or hematological relapse of CML after SCT results in a complete remission in 70–80% of the patients (7–12). The response rate is lower in patients with relapsed CML in accelerated phase or blast crisis (10, 12). DLI is accompanied by GvHD and bone marrow aplasia in 90% and 35–50% of the patients, respectively (10, 12).
The frequency of allo-reactive T cells in an HLA-identical donor that may react with patient leukocytes or leukemic cells is low (13–15). The development of acute GvHD and bone marrow aplasia during the responsive phase after DLI was associated with increased patient-reactive helper T lymphocyte precursor (HTLp) frequencies, as determined in a limiting dilution assay using cocultures of peripheral blood MNC after DLI and patient leukemic cells in the presence of interleukin (IL)-2 (16). These HTLp frequencies were found by measuring IL-2 production in response to restimulation with patient-derived nonleukemic B-lymphoblastoid cell lines (EBV-LCL), suggesting the recognition of a patient-specific polymorphic major histocompatibility (MHC) antigen. An increase in patient EBV-LCL reactive cytotoxic T lymphocyte precursor (CTLp) frequency after DLI was found in one responding patient. A 2-fold increase in the CTLp frequency against leukemic cells and an increase in natural killer cell activity was found in two patients with relapsed CML responding to DLI, suggesting MHC-restricted as well as non-MHC-restricted reactivity (17). Whether these relatively minor increases in HTLp and CTLp frequencies could explain the antileukemic response after DLI remained unclear.
Previously, we have generated cytotoxic T cell lines, and CD8+ and CD4+ T cell clones reactive with leukemic cells by stimulating donor T cells with patient leukemic cells (18–21). In some cases, we found T cell responses against CML progenitor cells in the absence of cytotoxicity against more mature leukemic cells (20). Because complete remissions after DLI appear to be long lasting, we hypothesized the involvement of leukemia-reactive T cells directed against the CML progenitor cells. To analyze whether such T cell responses play a role in the antileukemic effect after DLI, we developed an assay to measure inhibition of the proliferation of CML progenitor cells by cultured T cells. We report the clinical, hematological, and immunological parameters in seven consecutive patients treated with interferon (IFN)-α 2b and low doses of donor mononuclear cells (MNC) for relapsed CML after SCT. The HTLp, the CTLp, and the CML progenitor cell-inhibitory lymphocyte precursor (PCILp) frequencies in peripheral blood harvested before and at various time points after DLI were determined to identify the mechanism underlying the antileukemic responses.
MATERIALS AND METHODS
Patients.
Patients with a relapse of CML after allogeneic HLA-identical SCT were eligible for this study. A cytogenetic relapse of CML was defined by an increasing percentage of Philadelphia chromosome positive (Ph+) metaphases in consecutive karyotype analyses of the bone marrow. A hematological relapse after SCT was classified as chronic phase, accelerated phase, or blast crisis according to criteria described previously (22).
A cytogenetic remission was defined as all of 30 bone marrow metaphases analyzed were normal, a molecular remission as the absence of bcr-abl mRNA transcripts in blood and bone marrow cells as measured by reversed transcriptase–PCR.
Patients with a relapse of CML after SCT were treated with IFNα 3 × 106 units s.c. 5 days a week for at least 4 weeks before the first DLI. IFNα was discontinued in the case of a complete remission, acute GvHD ≥ grade II (23), or pancytopenia. MNC were harvested from the original bone marrow donor by leukapheresis, and 107 MNC/kg of body weight of the patient were infused. In two patients, 6 weeks after the initial dose, a second dose consisting of 3 × 107 MNC/kg was administrated.
GvHD ≥ grade II (23) was treated with methylprednisolone and/or cyclosporin A. Bone marrow aplasia was defined as a hypocellular bone marrow, dependency on platelet transfusions, the absence of reticulocytes, and granulocytes < 0.1 × 109/liter for a period of at least 2 weeks. A T cell-depleted SCT was given in case of bone marrow aplasia. Ex vivo T cell depletion of the bone marrow graft was performed by incubation of the cells with the mAb Campath-1G (IgG2b), followed by three washing procedures to remove free antibody.
Clinical Evaluation.
Blood cell and differential counts were determined at least every other week. Bone marrow aspirates were taken before treatment 6, 10, 16, and 26 weeks after DLI, or when clinically indicated. Before the start of IFNα, before DLI (time 0), and 2, 4, 6, 8, 10, 13, 16, 20, 26, and 52 weeks after DLI, peripheral blood was obtained from the patient and centrifugated over Ficoll Isopaque. MNC were harvested from the interphase and polymorphonuclear cells (PMN) from the pellet. In both fractions the presence of bcr-abl mRNA transcripts was determined by reverse transcriptase–PCR (24). Chimerism was studied by using a set of allele-specific oligonucleotides, flanking the human polymorphisms of factor IX (25), AFP (26), NGFβ (26), IL4RP2 (27), and PYNZ 22 (28). In all cases a patient- and/or donor-specific allele (29) was identified.
Phenotype analysis of MNC was performed by flowcytometry using mAbs against CD2, CD3, CD4, CD8, CD14, CD19, CD33, CD34, CD45, CD56, or T cell receptor γδ. No lymphocyte subpopulation analysis or immunological studies were performed in patients during treatment with cyclosporin A or more than 1 mg of methylprednisolone/kg per day.
Combined Determination of HTLp and CTLp Frequencies.
All cultures to determine the precursor cell frequencies from each donor-patient pair in patient peripheral blood samples at various intervals before and after DLI were performed within the same experiment to avoid inter-test variability. All leukemic MNC (CML-MNC) used as stimulator or target cells were shown to be exclusively Ph+. Thawed cells were washed twice and resuspended in complete medium, consisting of RPMI medium 1640 with 10% heat inactivated prescreened (HIV-, HBsAg- and allo-antibody negative) human serum. Using a pipetting robot (Biomek, Beckman) serial 2-fold dilutions of responder MNC from 40,000 cells/well down to 625 cells/well were cultured in 24 replicates per concentration of two 96-well microtiter plates. Each well was stimulated with 20,000 irradiated (25 Gy) patient CML-MNC. The last 24 wells contained CML-MNC only and were used as a reference. After 3 days of culture the supernatant was harvested from each well, and HTLp frequencies were analyzed by measuring IL-2 production in each well as described previously (30). To the remaining cells complete medium with 120 units/ml of IL-2 (Roussel Uclaf, Paris, France) was added. At day 7, all wells were restimulated with 10,000 irradiated CML-MNC. Twice a week half of the medium was refreshed. After 21 days of culture, half of the cells from each well was tested in a 4-hr Europium release assay as described previously (31), using CML-MNC from the patient as target cells. Wells were scored positive if the counts in that well exceeded the mean plus 3 SD of the reference wells. The other half of the cells were analyzed in the CML-PCILp assay.
CML Progenitor Cell Proliferation Assay.
Thawed, viable CML-MNC were divided into a CD34+ and a CD34− fraction by using CD34-specific immunomagnetic beads. These fractions as well as unseparated CML-MNC were cultured in progenitor cell culture medium, consisting of Iscove’s modified Dulbecco’s medium (IMDM) with 15% prescreened human serum and 50 ng/ml of stem cell factor (Amgen Biologicals), 25 ng/ml of IL-3 (Sandoz Pharmaceutical), 100 ng/ml of granulocyte–macrophage colony-stimulating factor (Sandoz), 100 ng/ml of granulocyte colony-stimulating factor (Amgen), 2 units/ml of erythropoietin (Cilag AG, Zug, Switzerland), 0.47 g/liter of human transferrin, and 5 × 10−5 mmol/liter of β-mercaptoethanol. Proliferation was measured in six replicates per concentration of serial 2-fold dilutions of unseparated, or CD34− CML-MNC (from 20,000 cells/well down to 1,250 cells/well), or CD34+ CML-MNC (from 4,000 cells/well down to 125 cells/well). After 7 days of culture, 1 μCi of [3H]thymidine-deoxyribose was added to each well and after 6 hr of culture [3H]thymidine incorporation was measured. The relative contribution of the CD34+ and CD34− fraction to the [3H]thymidine incorporation in the unseparated CML-MNC was calculated by using the percentage of CD34+ cells in the unseparated cell suspensions.
CML PCILp Assay.
As described to determine the CTLp frequencies, after 21 days of culture all wells were split, and half of the cells from each well or T cell clones were irradiated at a dose (10 Gy) that was shown to completely abrogate T cell proliferation but not to affect cytolytic activity (data not shown) and cocultured with 20,000 patient CML-MNC per well in progenitor cell culture medium. At least 24 wells containing only CML-MNC were used as a reference. After 7 days of culture the [3H]thymidine incorporation was measured. Inhibition of CML progenitor cell proliferation was calculated by using the reference wells. An individual well was scored positive if the [3H]thymidine incorporation in that well was less than the mean minus 3 SD of the reference wells. The percentage growth inhibition in a well was determined by [1 − (experimental cpm/mean cpm reference wells)] × 100%.
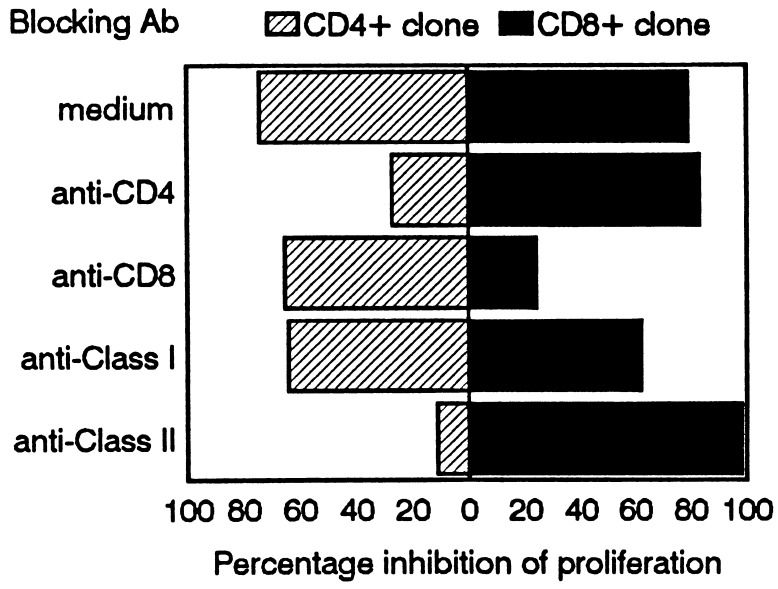
To illustrate MHC-restricted recognition in this assay, blocking studies were performed. Effector cells were preincubated with saturating concentrations of mAbs against CD4 or CD8 (RIV6 and FK18, respectively), or target CML-MNC were preincubated with mAbs against pan-HLA class I (W6.32) or pan-HLA class II (PdV 5.2) as described previously (19, 20).
Evaluation of the Data and Statistical Analysis.
We assumed single-hit kinetics and used the zero term of the Poisson equation, which predicts that when 37% of the tested wells are negative there is an average of one precursor cell per well. The HTLp, CTLp, and PCILp frequencies were calculated by using a statistical computer program (32). Correlation coefficients (r) were calculated by using the Pearson correlation coefficient.
RESULTS
Clinical Outcome.
Seven patients with a relapse of CML after SCT were treated with IFNα and MNC from the original, sex-matched, HLA-identical sibling donor (n = 4) or matched unrelated donor (n = 3) (Table 1). A molecular remission was obtained in six patients; five responded to a single transfusion of 107 MNC/kg, and one (EU) to a cumulative dosage of 4 × 107 MNC/kg. The interval from DLI to molecular remission varied from 6 to 20 weeks.
Table 1.
Patient characteristics and clinical outcome after DLI
| Patient | Donor type | SCT → DLI, months | Phase of CML at DLI | GvHD after DLI
|
DLI → CR, weeks | |
|---|---|---|---|---|---|---|
| Grade | Organ | |||||
| ES | MUD | 18 | Blast crisis | 0 | Died | |
| KK | MUD | 9 | Blast crisis | I | S | 6* |
| HG | MUD | 31 | Accelerated | III | L | 20 |
| EU | Sibling | 46 | Accelerated | IV | L,S | 20 |
| RB | Sibling | 14 | Hematological | IV | L,S | 16 |
| RV | Sibling | 12 | Hematological | II | L | 8 |
| WH | Sibling | 26 | Cytogenetic | 0 | 10 | |
MUD, matched unrelated donor; L, liver; S, skin; CR, complete remission.
*Relapse after 7 months.
Patient ES died 4 weeks after a second dose of donor MNC because of a therapy-resistant relapse. Patient KK had a second blast crisis 7 months after achieving complete remission with IFNα and DLI. Treatment with IFNα and two doses of donor MNC did not result in a second remission and 4 months later he died. Patient EU died 21 months after the DLI because of GvHD. The other patients are alive and well in continuous complete remission with a follow-up of 1–3 years GvHD > grade I after DLI was observed in all responding patients, except patient WH and KK. Patients HG and EU had a period of bone marrow aplasia, necessitating a T cell-depleted SCT, resulting in complete hematological recovery.
At relapse, before DLI, during the responsive phase, and after a complete remission was confirmed, the lymphocyte subsets in peripheral blood from all patients were determined. No significant differences were found in the relative percentage and absolute numbers of NK cells, CD4+, CD8+, or γδ T lymphocytes in each individual patient (data not shown).
Chimerism After DLI.
To analyze whether CML-MNC or more mature leukemic PMN were targets for the donor lymphocytes, patient/donor chimerism was determined in these fractions at various time points after DLI. As shown in Table 2, in three patients (EU, HG, and RV) a decrease in patient (leukemic) MNC preceded the decrease of leukemic PMN. Full donor chimerism in the MNC was present 2–6 weeks before this decrease was confirmed in PMN fraction. Fig. 1 represents the chimerism data from patient EU. Serial differential counts and FACS analysis by using anti-CD34 and anti-CD33 antibodies in patients EU and HG after DLI showed that first immature myeloid cells, followed by monocytes, and mature PMN disappeared consecutively before a period of bone marrow aplasia (data not shown).
Table 2.
Patient/donor chimerism in MNC and PMN after DLI
| Patient | Cells | Weeks after donor leukocyte infusion
|
|||||
|---|---|---|---|---|---|---|---|
| 0 | 6 | 8 | 10 | 13 | 16 | ||
| KK | MNC | M* | D | D | D | D | D |
| PMN | M | D | D | D | D | D | |
| HG | MNC | M | M | D | D | D | D |
| PMN | P | M | M | M | —† | D | |
| EU | MNC | P | P | M | M | D | D |
| PMN | P | P | P | P | M | D | |
| RB | MNC | M | M | nt | D | D | D |
| PMN | M | M | nt | D | D | D | |
| RV | MNC | M | D | D | D | nt | D |
| PMN | M | M | D | D | nt | D | |
| WH | MNC | M | M | nt | D | D | D |
| PMN | M | M | nt | D | D | D | |
nt, Not tested.
The results of chimerism analysis are given as P = patient, M = mixed, or D = donor.
Aplasia.
Figure 1.
Chimerism in the peripheral blood MNC and PMN in patient EU 0–19 weeks after DLI. Alpha-fetoprotein (AFP) polymorphism was used to identify donor (D)-specific cells (black bars); factor IX to identify patient (P)-specific cells. Complete donor chimerism in the MNC was found 14 weeks after the DLI, whereas it was present in the PMN 2 weeks later.
Leukemia-Reactive HTLp and CTLp Frequencies.
The leukemia-reactive HTLp frequencies in sibling donor peripheral blood were 0–1 per 106 MNC, and in matched unrelated donors 0 (donor HG), 22 (donor KK), and 48 (donor ES) per 106 MNC, respectively. The HTLp per ml of peripheral blood varied between 0 and 2 in patients with a relapse of CML, between 0 and 8 after IFNα, and between 0 and 12 after DLI. No correlation between clinical response and HTLp frequency was found. The leukemia-reactive CTLp frequencies in sibling donor peripheral blood varied between 0 and 14 per 106 MNC, and in the matched unrelated donors between 3 and 47 (donor KK) per 106 MNC. The number of CTLp per ml of peripheral blood at relapse, at the DLI, during clinical response, and after a molecular remission was confirmed is given in Table 3. In patient KK the number of CTLp rose from 12 before DLI to 502 per ml 2 weeks after DLI, and 79 per ml 6 months after DLI. During the second relapse the number of CTLp had dropped to 4 per ml. A moderate rise in CTLp frequency after DLI was found in one other patient (RB). No clear correlation was found between the clinical signs of GvHD and the number of circulating CTLp cells.
Table 3.
Maximal number of CTLp in peripheral blood at relapse (start IFNα), at DLI, during the clinical response, and after a molecular remission was confirmed
| Patient | Relapse | DLI | Response | Remission |
|---|---|---|---|---|
| ES | nt | 0 | 5 (NR) | — |
| KK | 8* | 12 | 502 | 4† |
| HG | 9 | 17 | 22 | 29‡ |
| EU | 5 | 5 | 5‡ | 12 |
| RB | 4 | 7 | 35 | 14 |
| RV | nt | 5 | 14 | 4 |
| WH | 0 | 2 | 0 | 0 |
NR, no response; nt, not tested.
The results are given as number of CTLp per ml of peripheral blood.
Relapse.
GvHD.
CML Progenitor Cell Proliferation Inhibition.
In a pilot study, CTL lines were generated by stimulating HLA-identical donor MNC with irradiated CML-MNC, and CD4+ CTL clones were generated by limiting dilution. Fig. 2 shows the percentage-specific lysis of CML-MNC in a 51Cr release assay and the percentage growth inhibition of CML progenitor cell proliferation by the three CD4+ CTL clones. Clone A was cytotoxic in both assays, exhibiting >20% specific lysis of leukemic cells in the 51Cr release assay and significant (>50%) proliferation inhibition of CML progenitor cells. Clone B was not cytotoxic in both assays. However, clone C gave significant proliferation inhibition of CML progenitor cells, but low cytotoxicity in the 51Cr release assay.
Figure 2.
Percentage specific lysis of patient leukemic cells in a 51Cr release assay (dotted bars) and percentage proliferation inhibition of CML progenitor cells from 104 CML-MNC by three different CTL clones at effector/target ratios of 10:1, 3:1, and 1:1. The results are given as the mean of two experiments.
To show that the CD34+ CML progenitor cells were responsible for the [3H]thymidine incorporation in the progenitor cell proliferation assay, thawed viable leukemic cells were divided in an unseparated, a CD34+, and a CD34− fraction by using immunomagnetic beads. The mean percentage of CD34+ cells was 7% in unseparated, thawed CML-MNC. Separation with immunomagnetic beads resulted in an enrichment of the CD34+ fraction up to 90%, whereas the mean percentage of CD34+ cells was less than 0.5% in the CD34− fraction. The mean [3H]thymidine incorporation of serial dilutions of unseparated CML cells, CD34+ CML cells, and CD34− CML cells of each patient after 7 days of culture were used to calculate the relative contribution of the CD34+ cells to the [3H]thymidine incorporation in the unseparated CML cells. As shown in Fig. 3, after 7 days of culture the proliferation of the CD34+ fraction was responsible for more than 90% of the proliferation in the unseparated CML cells. Blocking studies were performed by using a CD4 and CD8 positive clone. Fig. 4 shows that the inhibition of proliferation of CML progenitor cells can be blocked by antibodies against CD4 or CD8 and HLA class II or class I, respectively, illustrating HLA-restricted recognition.
Figure 3.
The proliferation of different numbers of unseparated CML-MNC, CD34+ CML progenitor cells, and CD34− CML-MNC after 7 days of culture in progenitor cell culture medium. Proliferation was measured by [3H]thymidine incorporation (cpm) during 6 hr. Shown is the proliferation of the unseparated fraction (shaded bars), the proliferation of the CD34+ fraction (filled bars), and the CD34− fraction (empty bars). The percentage of CD34+ cells was 1.9%, 6.2%, and 14.0% in patients HG, EU, and TO, respectively. In each tested concentration from each patient, the numbers of separated CD34+ and CD34− cells tested were equivalent to the numbers of these cells in the unseparated cell fraction. All experiments were done in 6-fold.
Figure 4.
MHC restricted recognition of target cells in the CML progenitor cell proliferation inhibition assay. A class II-restricted MHC antigen-specific CD4+ clone and a class I-restricted CD8+ clone were irradiated (10 Gy) and analyzed against CML-MNC at effector/target ratios of 4:1 and 1:1, respectively. Effector T cells or target CML-MNC were preincubated with control medium or antibodies against CD4, CD8, class I, or class II.
Leukemia-Reactive PCILp Frequencies.
The percentage of growth inhibition in the PCILp assay was calculated by using the [3H]thymidine incorporation of the experimental wells and the reference wells. The statistical cut-off point was >50% growth inhibition in comparison with the reference wells in all patient/donor combinations. The PCILp frequency in the matched unrelated donors was 14 (donor ES), 23 (donor KK), and 20 (donor HG) per 106 MNC. In sibling donors the PCILp frequency was 0 (donor WH), 13 (donor RB), 17 (donor RV), and 40 (donor EU) per 106 MNC. No clear correlation was found between the HTLp, CTLp, and PCILp frequencies in these donors, respectively, nor between the individual positive wells in the different assays. Phenotypic analysis of representative wells showed that both wells with predominantly CD4+ or with CD8+ cells were capable of specific inhibition of the CML progenitor cells (data not shown).
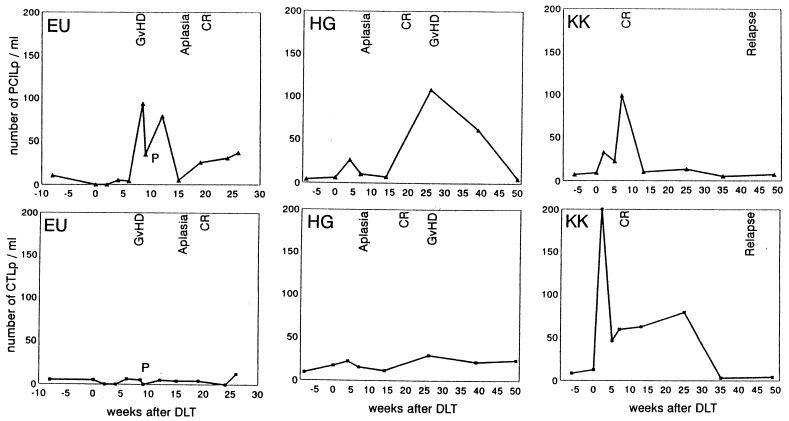
As shown in Fig. 5, a correlation was found between the number of PCILp and the clinical response. The number of PCILp per ml of patient peripheral blood at relapse, at the DLI, during the clinical response, and at the time of molecular remission is given in Table 4. In all tested patients a 5- to >100-fold increase in the number of circulating PCILp was found after DLI. After a complete remission was confirmed, the number of PCILp declined to <10/ml in all patients except EU and HG, who had persistent extensive and mild chronic GvHD, respectively.
Figure 5.
Frequencies of CML-PCILp and CTLp per ml of blood before or after DLI in patients EU, HG, and KK. Patient KK with a relapsed myeloid blast crisis entered complete remission 6 weeks after the first DLI. After 7 months a second relapse was treated unsuccessfully with IFNα and additional DLI. P indicates treatment with methylprednisolon. CR, complete remission.
Table 4.
Maximal number of PCILp at relapse (start IFNα), before DLI, during the clinical response, and after a molecular remission was confirmed
| Patient | Relapse | DLI | Response | Remission |
|---|---|---|---|---|
| ES | nt | 8 | 8 (NR) | — |
| KK | 7* | 9 | 98 | 5† |
| HG | 4 | 6 | 26 | 108‡ |
| EU | 10 | 0 | 93‡ | 36 |
| RB | 0 | 0 | 163‡ | 5 |
| RV | nt | 16 | 51‡ | 87‡ |
| WH | 0 | 0 | 29 | 0 |
NR, no response; nt, not tested.
The results are given as number of PCILp per ml of peripheral blood.
Relapse.
GvHD.
DISCUSSION
The antileukemic effect of DLI as a treatment for patients with a relapse of CML after SCT frequently is associated with GvHD or bone marrow aplasia, although an antileukemic effect also can be found in the absence of GvHD (11). To analyze the possible effector and target cells in DLI we monitored the disappearance of the leukemic cells and immunological parameters in seven consecutive patients treated for relapsed CML after SCT with IFNα and low doses of donor MNC. One patient with a cytogenetic relapse of CML had a complete molecular remission without GvHD. In contrast to the results described by Mackinnon et al. (11), four patients who responded to 107 donor MNC/kg had GvHD, but two of those patients had a matched unrelated donor.
The analysis of chimerism in the MNC and granulocytes in two patients with a hematologic relapse showed almost complete patient leukemic hematopoiesis before DLI. After DLI the leukemic cells disappeared from the MNC fraction before the more mature PMN converted to complete donor chimerism. These findings indicated that antigens on the progenitor cells and not on the mature cells were the potential target for donor lymphocytes.
Bunjes et al. (16) reported elevated HTLp frequencies during the responsive phase in five patients who achieved a molecular remission after high doses of DLI (16). In contrast to our HTLp analysis, the responder cells were cultured in IL-2, and IL-2 production was measured after 14 days in response to restimulation with patient-derived nonleukemic B-lymphoblastoid cell lines (EBV-LCL). High HTLp frequencies in four responding patients suggested the recognition of a patient-specific polymorphic MHC antigen by donor T cells. In our combined assay for leukemia-reactive HTLp and CTLp frequencies, we found no significant increase in HTLp frequency during clinical responses. Conflicting data about the patient-specific CTLp frequencies after DLI (16, 17) may be explained by differences in the stimulation protocols and days of culture. After 21 days of culture, we found no significant increase in the leukemia-reactive CTLp frequency in four responding patients, a moderate increase in one patient, and a strong increase in one patient with a myeloid blast crisis.
As we previously published (1, 20) and confirmed in this study, leukemia-reactive T cells capable of suppressing CML progenitor cells in a growth inhibition assay can be found in the absence of cytotoxicity against more mature leukemic cells in a 51Cr release assay. In this assay recognition by T cells of both leukemia-specific antigens and MHC antigens expressed on progenitor cells is detected. To analyze whether frequencies of T cell precursors directed against CML progenitor cells correlated with a clinical response after DLI, a modification of the growth inhibition assay was developed, allowing us to test CML progenitor cell growth inhibition in large numbers of wells. First, we showed that the [3H]thymidine incorporation by unseparated CML cells after 7 days of culture in medium containing stem cell factor, IL-3, granulocyte–macrophage colony-stimulating factor, granulocyte colony-stimulating factor, and erythropoietin was caused by the proliferation of CD34+ progenitor CML cells. In a pilot study we showed that CTL clones, whether or not they were cytotoxic against patient CML cells in a 51Cr release assay, could give significant inhibition of CML progenitor cells in this assay. Blocking studies illustrated MHC restricted recognition of the CML progenitor cells by the effector cells. Thus, by measuring the inhibition of proliferation of cultured CML cells in this assay, the functional activity of effector cells recognizing CD34+ CML progenitor cells can be tested.
The frequencies of PCILp correlated with the clinical response in the patients with a relapse of CML after SCT. In the responding patients a 5- to 100-fold increase in circulating PCILp was found; the highest numbers of circulating PCILp coincided with the disappearance of circulating malignant cells and the occurrence of GvHD. After obtaining complete molecular remission, PCILp frequencies diminished gradually. In patient KK with a myeloid blast crisis after SCT, a rapid molecular remission within 6 weeks coincided with elevated numbers of circulating PCILp and with high numbers of CTLp. This finding may explain the relative short interval between DLI and complete remission as has been reported in responding patients with relapsed acute myeloid leukemia (12).
In conclusion, by using this PCILp assay measuring the frequency of T cell precursors in peripheral blood that are capable of suppressing the growth of CD34+ CML progenitor cells, we demonstrated that during the responsive phase after DLI for relapsed CML after allogeneic SCT, T cell responses against CML progenitor cells probably mediate the antileukemic effect.
Acknowledgments
We thank Yvonne Bauman-Souverein for secretarial assistance, Roel de Paus and Simone van Luxemburg-Heijs for technical assistance, and Dr. S. Bhola for cytogenetic analysis. This study was supported by grants from the Dutch Cancer Society and the J. A. Cohen Institute for Radiopathology and Radiation Protection.
ABBREVIATIONS
- DLI
donor lymphocyte infusion
- CML
chronic myeloid leukemia
- SCT
stem cell transplantation
- PCILp
progenitor cell-inhibitory lymphocyte precursor
- HTLp
helper T lymphocyte precursor
- CTLp
cytotoxic T lymphocyte precursor
- MNC
mononuclear cells
- PMN
polymorphonuclear cells
- GvHD
graft versus host disease
- IL
interleukin
- MHC
major histocompatibility complex
- IFN
interferon
References
- 1.Falkenburg J H F, Smit W M, Willemze R. Immunol Rev. 1997;157:223–230. doi: 10.1111/j.1600-065x.1997.tb00985.x. [DOI] [PubMed] [Google Scholar]
- 2.Weiden P L, Flournoy N, Thomas E D, Prentice R, Fefer A, Buckner C D, Storb R. N Engl J Med. 1979;300:1068–1073. doi: 10.1056/NEJM197905103001902. [DOI] [PubMed] [Google Scholar]
- 3.Gale R P, Horowitz M M, Ash R C, Champlin R E, Goldman J M, Rimm A A, Ringden O, Stone J A V, Bortin M M. Ann Intern Med. 1994;120:646–652. doi: 10.7326/0003-4819-120-8-199404150-00004. [DOI] [PubMed] [Google Scholar]
- 4.Apperley J F, Jones L, Hale G, Waldmann H, Hows J, Rombos Y, Tsatalas C, Marcus R E, Goolden A W, Gordon Smith E C, et al. Bone Marrow Transplant. 1986;1:53–66. [PubMed] [Google Scholar]
- 5.Goldman J M, Gale R P, Horowitz M M, Bigs J C, Champlin R E, Gluckman E, Hoffmann R G, Jacobsen S J, Marmont A M, McGlave P B, et al. Ann Int Med. 1988;108:806–814. doi: 10.7326/0003-4819-108-6-806. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz M M, Gale R P, Sondel P M, Goldman J M, Kersey J, Kolb H J, Rimm A A, Ringden O, Rozman C, Speck B, et al. Blood. 1990;75:555–562. [PubMed] [Google Scholar]
- 7.Kolb H J, Mittermüller J, Clemm Ch, Holler E, Ledderlose G, Brehm G, Heim M, Wilmanns W. Blood. 1990;76:2462–2465. [PubMed] [Google Scholar]
- 8.Porter D L, Roth M S, McGarigle C, Ferrara J L M, Antin J H. N Engl J Med. 1994;330:100–106. doi: 10.1056/NEJM199401133300204. [DOI] [PubMed] [Google Scholar]
- 9.van Rhee F, Lin F, Cullis J O, Spencer A, Cross N C P, Chase A, Garicochea B, Bungey J, Barrett J, Goldman J M. Blood. 1994;83:3377–3383. [PubMed] [Google Scholar]
- 10.Kolb H J, Schattenberg A, Goldman J M, Hertenstein B, Jacobsen N, Arcese W, Ljungman P, Ferrant A, Verdonck L, Niederwieser D, et al. Blood. 1995;86:2041–2050. [PubMed] [Google Scholar]
- 11.Mackinnon S, Papadopoulos E B, Carabasi M H, Reich L, Collins N H, Boulad F, Castro-Malaspina H, Childs B H, Gillio A P, Kernan N A, et al. Blood. 1995;86:1261–1268. [PubMed] [Google Scholar]
- 12.Collins R H, Shpilberg O, Drobyski W R, Porter D L, Giralt S, Champlin R, Goodman S A, Wolff S N, Hu W, Vervaillie C, et al. J Clin Oncol. 1997;15:433–444. doi: 10.1200/JCO.1997.15.2.433. [DOI] [PubMed] [Google Scholar]
- 13.Kaminski E, Hows J, Man S, Brookes P, Mackinnon S, Hughes T, Avakian O, Goldman J M, Batchelor J R. Transplantation. 1989;48:608–613. [PubMed] [Google Scholar]
- 14.Hoffmann T, Theobald M, Bunjes D, Weiss M, Heimpel H, Heit W. Bone Marrow Transplant. 1993;12:1–8. [PubMed] [Google Scholar]
- 15.Schwarer A P, Jiang Y Z, Deacock S, Brookes P A, Barrett A J, Goldman J M, Batchelor J R, Lechler R I. Transplantation. 1994;58:1198–1203. [PubMed] [Google Scholar]
- 16.Bunjes D, Theobald M, Hertenstein B, Wiesneth M, Novotny J, Arnold R, Heimpel H. Bone Marrow Transplant. 1995;15:713–719. [PubMed] [Google Scholar]
- 17.Jiang Y Z, Cullis J O, Kanfer E J, Goldman J M, Barrett A J. Bone Marrow Transplant. 1993;11:133–138. [PubMed] [Google Scholar]
- 18.Falkenburg J H F, Faber L M, van den Elshout M, van Luxemburg-Heys S A P, Hooftman-den Otter A, Smit W M, Voogt P J, Willemze R. J Immunother. 1993;14:305–309. doi: 10.1097/00002371-199311000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Faber L M, van Luxemburg-Heys S A P, Willemze R, Falkenburg J H F. J Exp Med. 1992;176:1283–1289. doi: 10.1084/jem.176.5.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faber L M, van Luxemburg-Heys S A P, Veenhof W F J, Willemze R, Falkenburg J H F. Blood. 1995;86:2821–2828. [PubMed] [Google Scholar]
- 21.Faber L M, van Luxemburg-Heijs S A P, Rijnbeek M, Willemze R, Falkenburg J H F. Biol Blood Marrow Transplant. 1996;2:31–36. [PubMed] [Google Scholar]
- 22.Speck B, Bortin M M, Champlin R, Goldman J M, Herzig R H, McGlave P B, Messner H A, Weiner R S, Rimm A A. Lancet. 1984;i:665–668. doi: 10.1016/s0140-6736(84)92179-2. [DOI] [PubMed] [Google Scholar]
- 23.Thomas E D, Storb R, Clift R A, Fefer A, Johnson L, Neiman P E, Lesner K G, Glucksberg H, Buckner C D. N Engl J Med. 1975;292:832–843. doi: 10.1056/NEJM197504172921605. [DOI] [PubMed] [Google Scholar]
- 24.Maurer J, Janssen J W G, Thiel E, van Denderen J, Ludwig W D, Aydemir U, Heinze B, Fonatsch C, Harbott J, Reiter A, et al. Lancet. 1991;337:1055–1058. doi: 10.1016/0140-6736(91)91706-z. [DOI] [PubMed] [Google Scholar]
- 25.Bouvier D P. Nucleic Acids Res. 1990;18:5325. doi: 10.1093/nar/18.17.5325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saiki R K, Gelfand D H, Stoffel S, Scharf S J, Higuchi R, Horn G T, Mullis K B, Erlich H A. Science. 1988;239:487–491. doi: 10.1126/science.2448875. [DOI] [PubMed] [Google Scholar]
- 27.Mout R, Willemze R, Landegent J E. Nucleic Acids Res. 1991;19:3763. doi: 10.1093/nar/19.13.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolff R K, Nakamura Y, White R. Genomics. 1988;3:347–351. doi: 10.1016/0888-7543(88)90126-7. [DOI] [PubMed] [Google Scholar]
- 29.Mackinnon S, Barnett L, Bourhis J H, Black P, Heller G, O’Reilly R J. Blood. 1992;80:3235–3241. [PubMed] [Google Scholar]
- 30.Schanz U, Roelen D L, Bruning J W, Kardol M J, van Rood J J, Claas F H J. J Immunol Methods. 1994;169:221–230. doi: 10.1016/0022-1759(94)90266-6. [DOI] [PubMed] [Google Scholar]
- 31.Bouma G J, van der Meer-Prins P M W, van Bree F P M J, van Rood J J, Claas F H J. Hum Immunol. 1992;35:85–92. doi: 10.1016/0198-8859(92)90015-f. [DOI] [PubMed] [Google Scholar]
- 32.Strijbosch L W G, Buurman W A, Does R J M M, Zinken P H, Groenewegen G. J Immunol Methods. 1987;97:133–140. doi: 10.1016/0022-1759(87)90115-3. [DOI] [PubMed] [Google Scholar]