Abstract
Presacral region is one of the difficult regions for drainage of abscess as the approaches described for this carry a lot of morbidities. Transpedicular approach is described for the drainage of presacral abscess. Further, tuberculous abscess as a cause of cauda equina syndrome is reported. Patient had complete neurological recovery within weeks of drainage of abscess. Transpedicular drainage of presacral abscess is a safer option for recently developed neurological deficit. Late presentation may need anterior approach, which is associated with increased morbidity.
Keywords: Presacral abscess, Transpedicular drainage
Introduction
Lumbosacral tuberculosis can lead to the formation of a presacral abscess. Drainage of the abscess is indicated if it is causing pressure symptoms or if it is not regressing on antituberculous treatment. Presacral region is one of the difficult regions for the drainage of abscess, as the approaches described for it carry a lot of morbidities. Anterior abdominal approach is most commonly used for the drainage of presacral abscess [3]. High sacral excision preserving both S2 roots is another approach that can lead to presacral space and potentially be utilized for the drainage of presacral abscess [4]. Interventional radiology has reported several innovative low morbidity approaches like transgluteal, transrectal, transvaginal and precoccygeal routes followed by placement of catheter for drainage [9, 11]. Transpedicular approach has been reported in the literature for the management of pyogenic discitis [1, 5] and for taking a biopsy from a presacral mass [10]. Here, a simple method of early drainage of presacral abscess through transpedicular approach is described.
Case report
A 34-year-old man presented with a history of pain in lower back for 8 months. Pain was progressive in nature, constant, increased on movements and reduced on rest. He also complained of urinary hesitancy for the last 1 month. There was no history of any constitutional symptoms. Clinical examination revealed an angular kyphosis at L5 S1. Tenderness was observed on palpation. Motor examination revealed reduced dorsiflexion at bilateral ankle joint (bilateral tibialis anterior, extensor and flexor hallucis longus and tendoachillis all had power 3/5) and 30–40% subjective loss of light touch and pinprick in L5 to S5 dermatomes in both the limbs. Babinski’s sign was negative.
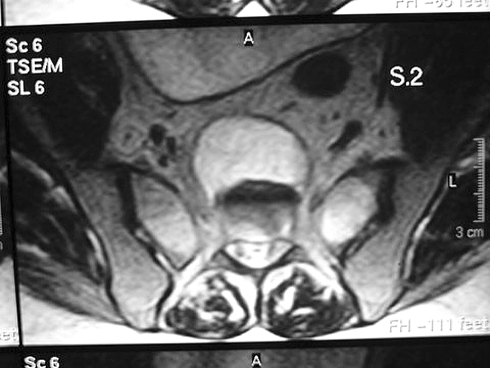
Radiographs were taken which revealed normal findings. Magnetic resonance imaging was performed, and destruction of L5 and S1 vertebrae was seen along with a loss of disc space. Presacral and epidural collection was present (Figs. 1, 2). Screening of the remaining spine revealed a skip lesion of the dorsal spine.
Fig. 1.
Sagittal section showing large presacral abscess
Fig. 2.
Transverse section showing large collection of pus
Treatment was started for the patient with a first-line antituberculous oral drugs (Isoniazide 5 mg/kg, Rifampcin 10 mg/kg, Ethambutol 15 mg/kg, Pyrazinamide 25 mg/kg; patient’s weight was 70 kg) and advised strict bed rest.
Patient reported 2 weeks after initiation of the treatment with retention of urine, further loss of power (reduced to 1/5 in above muscle groups) and sensory deficit in light touch and a pinprick of 70–80% from L5 to S5 dermatomes. Anal tone was absent. Ankle jerk was absent in both the limbs.
As the neurological level and clinical findings correlated with the lumbosacral lesion, diagnosis of cauda equina syndrome was made and the patient was prepared for decompression.
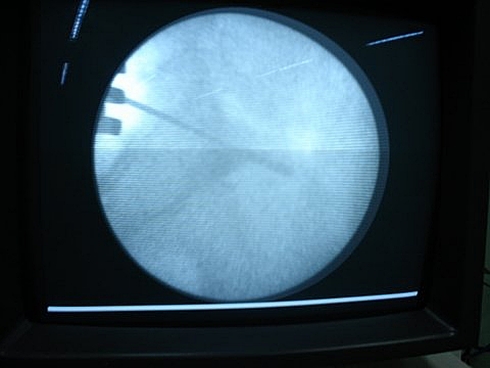
Under fluoroscopic guidance, guide wires were inserted along the S1 pedicles in a similar manner to pedicle screw insertion (Fig. 3). Drill bits measuring 3.2 mm were inserted along the same path up to anterior sacral cortex. Path was enlarged by larger sized blunt curettes and progressed 0.5 cm anterior to anterior sacral body into abscess. Abscess was drained; cavity was washed by irrigation through infant feeding tube along the same tract.
Fig. 3.
Guide wire insertion under image intensifier
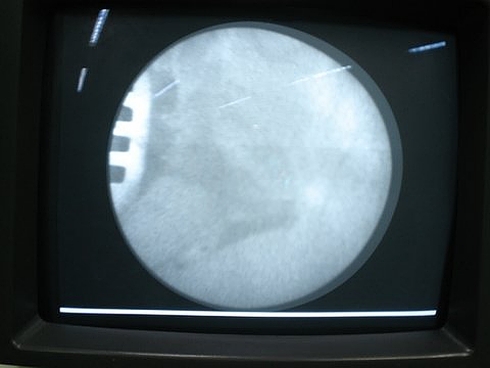
Completeness of drainage was further confirmed by injecting radio opaque dye and seeing it filling the cavity on fluoroscopy (Fig. 4). On washing the dye, cavity disappeared. Dorsal spine lesion was also stabilized by posterior pedicle screw fixation and bone grafting, as patient wanted early mobilization.
Fig. 4.
Dye seen filling the empty abscess cavity
Antituberculous treatment was continued postoperatively and the patient recovered his bladder/bowel control within 2 days. He had recovery of all motor power and sensations by 2 weeks postoperatively. Acid Fast Bacillus staining for tuberculous bacteria was positive in the pus evacuated during surgery. At 1-year follow-up, the patient was asymptomatic and is off the antituberculous treatment after normalization of inflammatory markers.
Discussion
Tuberculous abscess resolves on most occasions on antituberculous drug therapy. However, failure of improvement or deterioration in neurological status on ATT is an indication of surgical decompression. Cauda equina is rarely reported to be involved by tuberculosis and this is the second case report in the world literature of this sort [6]. Cauda equina is a surgical emergency, and early drainage is important for early recovery of bladder/bowel control [7, 8]. In fact, Kennedy et al. [7] studied several factors responsible for a successful outcome in cauda equina, and were of opinion that early diagnosis and early decompression are the most important predictors of a successful outcome.
Kapoor et al. [6] reported one such case of cauda equina being caused by tuberculous involvement of posterior elements, and reported improvement in neurological status by laminectomy.
Involvement of anterior elements causes pus to accumulate in pre- and paravertebral space. This pus can then travel through intervertebral foramen and cause pressure over cauda equina nerve roots. Rarely, pus may accumulate posteriorly after involvement of posterior part of body and posterior longitudinal ligament. However, this seems unlikely to be the mechanism in our case as posterior vertebral body is spared.
Buyukbebeci et al. [3] reported a case of lumbosacral tuberculosis with presacral abscess, which was drained by anterior route.
In this case, since anterior elements were involved, laminectomy would have led to increased instability. Further, anterior abdominal approach carries a lot of morbidity. In view of recent onset of deficit, it was decided to drain the abscess through transpedicular approach, which is much easier and without much morbidity. However, risks of failure to recover and need to undergo second stage major surgery for anterior decompression were explained to the patient. Success in this case was also because of the fact that pressure on cord was due to abscess and not granulation tissue. Had the surgery been delayed and granulation tissue formed, decompression of the cord would not have been possible by only draining the abscess.
Anterior approach is associated with the dangers of vascular or neural damage [2]. Hence this approach carries a lot of morbidities.
Presacral route has been described for excision of presacral tumors, but can be associated with major morbidity [4]. It can cause perianal anesthesia after resection of lower sacral vertebrae. Further, resection of lower sacral vertebrae can be associated with difficulty in reclining and seating due to the loss of sacral support. Preservation of S2 roots is essential for preserving the anal tone. Even though this approach can give access to presacral space, it carries much more morbidity for drainage of an abscess.
A transpedicular sacral approach is a simple alternative. By using fluoroscopic guidance, this approach can be directed towards the abscess. By just perforating the anterior cortex, any danger of vascular damage of anterior vessels is minimized. Enlargement of the path and perforation of abscess cavity by blunt curettes further protect the anterior structures.
Completeness of drainage was confirmed by injecting the iodinated radio opaque contrast into the cavity. On injecting into the cavity, a well-defined cavity was formed. On easy drainage of presacral abscess irrigation of the cavity, contrast was completely washed off denoting the absence of any remaining pus within the cavity. As is well demonstrated by this report, early drainage of pus even in the presence of neurological deficit can lead to neurological improvement.
A similar approach has been previously described for biopsy of a presacral mass [10] and for the treatment of pyogenic spondylodiscitis [1, 5]. But this is the first time in the world literature that this approach is being described for the drainage of presacral abscess, which is such a common complication of a common disease in developing countries. Success by this approach depends on early surgery when pressure from pus is the cause of deficit. Delay can lead to granulation tissue formation, and patient may need anterior abdominal approach in such cases.
Conclusion
Early drainage of presacral abscess by transpedicular route is a safer option for a recently developed neurological deficit. Late presentation may need anterior approach, which is associated with increased morbidity.
References
- 1.Arya S, Crow WN, Hadjipaviou AG, Nauta HJ, Borowski AM, Vierra LA, Walser E. Percutaneous transpedicular management of discitis. J Vasc Interv Radiol. 1996;7(6):921–927. doi: 10.1016/S1051-0443(96)70871-0. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi C, Ballard JL, Abou-Zamzam AM, Teruya TH, Abu-Assal ML. Anterior retroperitoneal lumbosacral spine exposure: operative technique and results. Ann Vasc Surg. 2003;17(2):137–142. doi: 10.1007/s10016-001-0396-x. [DOI] [PubMed] [Google Scholar]
- 3.Buyukbebeci O, Karkurum G, Gulec A, Erbagci A. Tuberculous osteomyelitis of the lumbosacral region: a spinal epidural abscess with presacral extension. Arch Orthop Trauma Surg. 2004;124(5):246–248. doi: 10.1007/s00402-004-0660-y. [DOI] [PubMed] [Google Scholar]
- 4.Gennari L, Azzarelli A, Quagliuolo V. A posterior approach for the excision of sacral chordoma. J Bone Joint Surg Br. 1987;69(4):565–568. doi: 10.1302/0301-620X.69B4.3611160. [DOI] [PubMed] [Google Scholar]
- 5.Hadjipavlou AG, Katonis PK, Gaitanis IN, Muffoletto AJ, Tzermiadianos MN, Crow W. Percutaneous transpedicular discectomy and drainage in pyogenic spondylodiscitis. Eur Spine J. 2004;13(8):707–713. doi: 10.1007/s00586-004-0699-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kapoor SK, Garg V, Dhaon BK, Jindal M. Tuberculosis of the posterior vertebral elements: a rare cause of compression of the cauda equina. A case report. J Bone Joint Surg Am. 2005;87(2):391–394. doi: 10.2106/JBJS.2928pp. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy JG, Soffe KE, McGrath A, Stephens MM, Walsh MG, McManus F. Predictors of outcome in cauda equina syndrome. Eur Spine J. 1999;8(4):317–322. doi: 10.1007/s005860050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mangialardi R, Mastorillo G, Minoia L, Garofalo R, Conserva F, Solarino GB. Lumbar disc herniation and cauda equina syndrome. Considerations on a pathology with different clinical manifestations. Chir Organi Mov. 2002;87(1):35–42. [PubMed] [Google Scholar]
- 9.Michalson AE, Brown BP, Warnock NG, Simonson TM. Presacral abscesses: percutaneous transperineal drainage with use of bone landmarks and fluoroscopic guidance. Radiology. 1994;190(2):574–575. doi: 10.1148/radiology.190.2.8284420. [DOI] [PubMed] [Google Scholar]
- 10.Rapport RL, 2nd, Ferguson GS. Dorsal approach to presacral biopsy: technical case report. Neurosurgery. 1997;40(5):1087–1088. doi: 10.1097/00006123-199705000-00040. [DOI] [PubMed] [Google Scholar]
- 11.Trambert JJ. Percutaneous interventions in the presacral space: CT-guided precoccygeal approach—early experience. Radiology. 1999;213(3):901–904. doi: 10.1148/radiology.213.3.r99dc15901. [DOI] [PubMed] [Google Scholar]