Abstract
Percutaneous vertebroplasty (PVP) of the axis is a challenging procedure which may be performed by a percutaneous or a transoral approach. There are few reports of PVP at the C2 level. We report a case of unstable C2 fracture treated with the percutaneous approach. The fracture was the first manifestation of multiple myeloma in a previously healthy 47-year-old woman. After local radiotherapy and chemotherapy, the fracture was still unstable and the patient had been continuously wearing a stiff cervical collar for 9 months. Complication-free PVP resulted in pain relief and stabilization and use of the cervical collar could be discontinued. At 18 months follow-up the patient remained free from pain, the fracture was stable and she had returned to work. The purpose of this article is to present the technical facts and to highlight the benefits and potential complications of the procedure. The technical characteristics of the procedure, the indication and results of the present case are discussed together with previously reported cases of PVP treatment at C2.
Keywords: C2, Multiple myeloma, Osteolytic lesion, Percutaneous vertebroplasty, Spine stabilization
Introduction
Percutaneous vertebroplasty (PVP) is a minimally invasive radiological method for the treatment of back pain related to osteoporotic vertebral compression fractures, vertebral metastases, myeloma and aggressive hemangioma. The technique was developed in France after the treatment of a patient with an aggressive hemangioma with epidural extension at C2 in 1984 [8]. The result of the treatment was reinforcement of C2 and complete pain relief. The indications for PVP were later extended to patients with osteoporotic compression fractures and vertebral metastases [4]. PVP has been reported to be an effective and safe procedure over the past 15 years [9]. PVP in the upper cervical spine may be performed by anterolateral or transoral approaches and it is technically more challenging than procedures in the thoracic and lumbar spine. The unique anatomical features and the fact that metastases predominate over osteoporosis may explain the higher risk of complications. The risk of cement leakage increases in cases of osteolytic lesions. A cement leak into the spinal canal may compromise the spinal cord or the nerve roots and lead to severe neurological deficit. Reports on PVP in the cervical spine are few, and those on PVP at C2 level are scarce [7, 11, 12, 14].
We report on PVP treatment of an unstable C2 fracture in a woman with multiple myeloma and compare our case to those reported in the literature on PVP treatment at C2. The purpose of this article is to highlight PVP as a new therapeutic option for pain relief and stabilization in the difficult management of patients with pathological fractures at C2.
Case report
A 47-year-old woman was referred to the orthopedic clinic at our hospital with a 6-week history of increasing neck pain without focal neurological symptoms. One night, a week before admission, the pain worsened as she removed a pillow under her neck. She heard a cracking noise, experienced instant pain in her neck and was not able to sustain her head. The X-ray images obtained at her local hospital demonstrated a fracture in C2 and she was referred to us for further investigation. No signs of spinal cord compression or other neurological deficit were found at the physical examination upon admission. Besides the C2 fracture, a CT scan showed an extensive osteolytic lesion (Fig. 1). MR images of the cervical spine showed a prevertebral soft tissue mass and edema (Fig. 2).
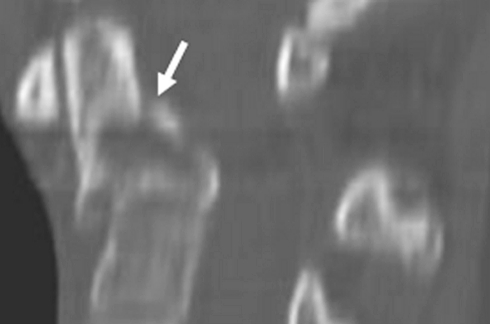
Fig. 1.
Reconstructed sagittal computed tomography image of C2 showing the extent of the osteolytic lesion through the vertebral body and part of the dens axis. A fracture (arrow) crosses the body of C2 causing ventral dislocation at the base of the dens and kyphosis at C2–C3
Fig. 2.
Sagittal T2W MR image of the cervical spine showing the extension of soft tissue mass (arrows), pre- and post-vertebral, from the body of C2. Pre-vertebral edema (asterisk) extens from C2 to C5
The patient was given a stiff cervical collar to prevent the development of neurological deficit due to the high risk of subluxation and angulation of the fracture. Osteolytic lesions on the T7, T11 and T12 vertebrae, the 8th and 12th left rib, the iliac bone and smaller lesions in other parts of the hip and in both humeri were demonstrated on the radiological work-up. Several CT-guided biopsies from C2 were inconclusive. Routine laboratory examinations showed normal peripheral blood values, s-electrolytes, including calcium, and s-creatinine. Finally, CT-guided biopsies from the affected ribs and pelvis showed infiltration of plasma cells. In the bone marrow aspirate, 20% plasma cells were found. She had no M-component in serum but showed urinary light chain excretion (3 g/24 h χ-chains) and the diagnostic criteria for multiple myeloma (MM) were fulfilled.
Hematologists and orthopedic surgeons agreed on the priority of the systemic treatment of the myeloma over the stabilization of the fracture; the cervical collar being retained during the cytostatic treatment and radiation therapy. Radiation therapy (20 Gy) was given in 5 Gy fractions to C2 and the odontoid processes together with steroids. After this treatment the pain was less intense, and the discrete paresthesia in the hands and feet that had developed during her hospital stay disappeared. She was then treated according to the Nordic myeloma program [13] with high-dose melphalan therapy and autologous stem cell support. One month after treatment the patient was in complete remission, as determined, by immune electrophoresis. The radiological follow-up (X-ray and CT scan) demonstrated persistence of the osteolytic lesion and worsening of the dislocation of the unstable C2 fracture (Fig. 3). The patient had now worn the cervical collar for a total of 9 months. She was suffering considerable discomfort and needed higher doses of analgesics and sedatives. She also experienced progressive deterioration of her quality of life. A multidisciplinary team including hematologists, an orthopedic surgeon and a neuroradiologist discussed the benefits and potential risks of surgical stabilization and PVP. A review of the facts was presented to the patient, who agreed to the PVP treatment.
Fig. 3.
Reconstructed sagittal image of a C2 CT scan 3 months after chemotherapy and local radiotherapy demonstrating progressive compression and dislocation (arrow) of the fracture
The procedure
The procedure was performed in the X-ray suite with a single-plane Philips Angiography C-arm system (Integris 5000). The patient was in the supine position and following the routines for PVP procedures at the cervical spine at our unit, under general anesthesia. A fiberoptic nasal intubation was performed to minimize movement of the neck [5]. The patient was given a prophylactic dose of an antibiotic (1.5 g of cephalosporine). The operation area with the neck slightly extended to facilitate the puncture, was sterilized and draped and local anesthesia was administered. The entry point of the puncture needle (14 gauge bevelled, Escoffier, Thonon, France) was at the edge of the mandibular angle (Fig. 4). The needle was advanced under alternative anteropostrior (AP) and lateral fluoroscopical guidance (Fig. 5) and a three-dimensional X-ray image was obtained to confirm the position of the needle (Fig. 6). The bone cement (Simplex P, Howmedica, Rutherford, NJ, USA) was prepared by mixing 20 ml of polymethyl methacrylate (PMMA) powder with 2 g tantalum powder (to increase the opacity) and 5 ml PMMA liquid. When it had reached the consistency of toothpaste, 1.5 ml of cement was injected under continuous fluoroscopy control in the lateral projection (Fig. 7).
Fig. 4.
The patient lies in supine position. The nasal intubation was performed with the patient wearing a cervical collar to prevent movements of the neck. The puncture needle is rotated during the cement injection to avoid leakage and achieve a better cement distribution in the vertebrae
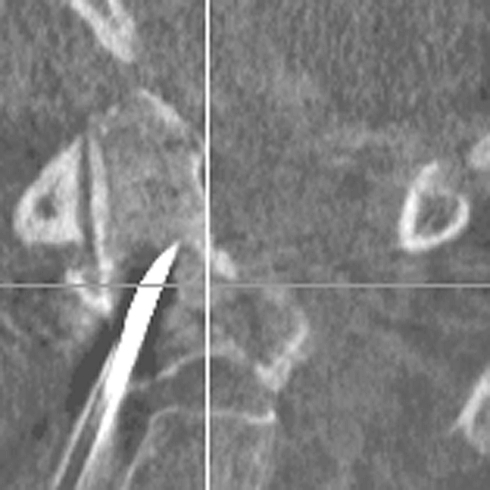
Fig. 5.
X-ray image of the puncture needle (14 G × 10 cm) in an anteroposterior view, showing how it follows an oblique anterolateral direction towards the body of C2
Fig. 6.
A 3D lateral X-ray image (orthogonal reconstruction) with the needle positioned centrally in the C2 body before cement injection
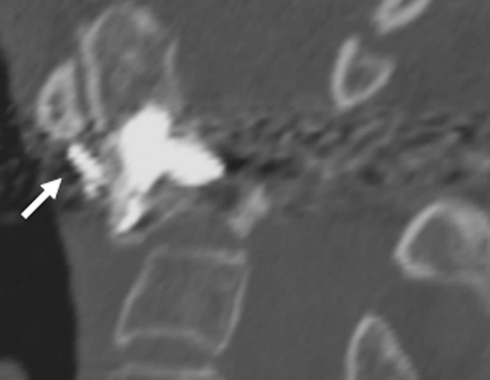
Fig. 7.
X-ray image showing a pre-vertebral cement leakage (arrow). After slight rotation of the needle, the injection was completed achieving good cement distribution in the vertebral body and part of the dens
Post-procedural care
A post-procedural CT scan was performed to evaluate the cement distribution and any possible cement leakage (Fig. 8). The patient was kept intubated and monitored overnight. No clinical complications occurred. The patient was free from pain and could be discharged from the hospital the day after PVP wearing the cervical collar.
Fig. 8.
Post-procedure CT image of the upper cervical spine. Reconstructed sagittal image on the midline shows good cement distribution over the fracture area and the osteolytic lesion in the body of C2. A small pre-vertebral cement leak can be seen (arrow). Slightly repositioning of the C2–C3 dislocation can be observed after PVP
Follow-up
A CT scan including a flexion and extension test was performed three weeks after the procedure. The examination revealed stable conditions and the cervical collar was removed. She has been given pamidronate intravenously every 4 weeks from the diagnosis to the present day. As a result of the fracture the mobility of the neck was restricted (especially extension and flexion) but it has gradually improved. At the 18-month clinical and radiological follow-up after PVP, the myeloma was still in remission, the patient remained free from pain and the fracture continued to be stable (Fig. 9a, b). The osteolytic lesion was replaced by sclerotic bone (Fig. 10a, b). She had taken up her former occupation as a florist, and experienced a remarkable improvement in her quality of life.
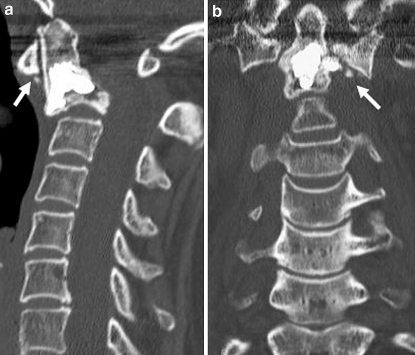
Fig. 9.
Follow-up CT images of the upper cervical spine 18 months after the PVP procedure. Reconstructed a sagittal- and b coronal images on the midline. The cement cast is unchanged. A clear osteosclerotic reaction has occurred around the cement cast
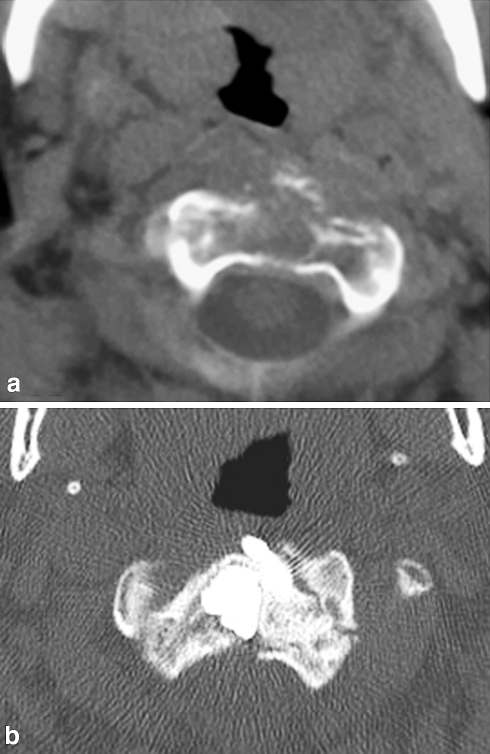
Fig. 10.
Axial CT images of the C2 vertebral body a at diagnosis and b at 18-month follow-up. The osteolytic lesion has been replaced by a sclerotic reaction increasing the reinforcement of the bone structure around the cement augmentation
Discussion
The axis is an important element of the musculoskeletal complex in the upper cervical spine. It is surrounded by a number of delicate neurological and vascular structures and controls a wide range of movements. Thus, a pathological C2 fracture is a threatening condition. Multiple myeloma and osteolytic metastases are the most frequent malignant lesions affecting the spine [3, 10]. However, the cervical spine, especially the C1 and C2 region, seems to be involved less often. In a large single-center report on PVP treatment in vertebral metastases in 117 patients (304 vertebrae) 10% were localized to the cervical region and only 2% to C2 [2]
Although there is no cure for MM, the course of the disease may be controlled with appropriate therapy and a long survival time can be expected. Severe neck and back pain and reduced mobility are the most common symptoms in patients with vertebral metastases and MM. The treatment is basically conservative, with analgesics, cytostatics, radiotherapy, reinforced corset and/or neck brace.
In patients with osteolytic lesions in the cervical spine and refractory pain, with or without fracture dislocations, different types of surgical stabilization methods have traditionally been used. The least invasive method consists of the halo-vest treatment, which can safely be performed concurrently with the medical treatment. This form of treatment may lead to bone reconstitution and stability [1]. Posterior osteosynthesis with or without decompression involves permanent fixation from occipital bone to C4 with restriction of flexion, extension, bending and rotation. The procedure has a low risk of complications, provides immediate stabilization of the C2 lesion and allows safe mobilization of the patient with a neck brace [6].
During recent years an increasing number of patients with MM and metastases have been treated with PVP [15]. This has offered rapid and long-lasting pain relief in up to 85% of cases [2, 3, 9]. However, experience in PVP treatment in the cervical spine, especially at C2 level is limited and the procedure is difficult [12].
The original approach in cervical PVP was the percutaneous anterolateral approach, and for the upper cervical spine (C1 and C2 levels) the submandibular anterolateral [12]. During percutaneous puncture the submandibular gland, the carotid and jugular vessels and the structures in the oropharyngeal region must be avoided. This is a challenging approach, but is feasible in experienced hands, and Mont’Alverne et al. [12] found this approach more suitable than the transoral approach described by Tong et al. [14].
In a literature search conducted on Medline, we found 15 cases of PVP procedures at C2. The characteristics of the patients and the procedures, indications, results, intra- and postoperative adverse events and follow-up are presented in Table 1. Only one of these patients treated with the transoral approach had MM [14]. Our patient was initially treated with a stiff cervical collar, received radiotherapy and cytostatics and after nine months her myeloma was in remission. However, the unstable osteolytic lesion at C2 had dislocated and angulated (Fig. 3). The multidisciplinary team considered PVP a better therapeutic option than surgery for the stabilization of the fracture. The procedure was performed without complications, achieving pain relief and stabilization of the fracture.
Table 1.
Characteristics of the 15 PVP procedures at C2 reported in the literature and of our own case report
| Authors/study type | Number of patients/age | Diagnosis | Indication | Approach | Anesthesia | Pain relief | Stability | Complications | Discharge | Follow-up | Discontinued use of cervical collar |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tong et al. Case report (2000) | 1/76 | Multiple myeloma | P | T | GA | Yes | No | 24 h | 6 months | 4 days after PVP | |
| Martin et al. Case report (2002) | 1/70 | Metastases | P + I | T | GA | Yes | Yes | No | No data | 8 months | Not reported |
| Gailloud et al. Case report (2002) | 1/58 | Bone cyst | P + I | T | GA | Yes | Yes | Transient dysphagia | 24 h | 18 months | Post-operatively |
| Mont’Alverne et al. Retrospective series (2005) | 12/52a (4 lost at follow-up) | Metastases | 5 P + I 3 I | p | CS | 4 (80%) | 7 (87.5%) | 1 ischemic stroke, 1 transient occipital neuralgia, 7 asymptomatic cement leaks | 24 h | 6.9 monthsa | Not reported |
| Rodriguez-Catarino et al. Case report (2006) | 1/47 | Multiple myeloma | P + I | p | CS | Yes | Yes | Asymptomatic cement leak | 24 h | 18 months | 3 weeks after PVP |
P pain, I instability, P + I = pain and instability, T transoral, p percutaneous, GA general anesthesia, CS conscious sedation
aMean value
We can only speculate whether earlier PVP treatment would have spared the patient the discomfort caused by the cervical collar for 9 months and whether could have had prevented a worsening of the fracture. However, in our case, we chose to follow the standard guidelines for treatment of MM, including radiation and chemotherapy. After 9 months the challenge of the procedure was the same, but the risk of complications was considered to be higher, since the dislocation of the fracture had increased. The fact that the osteolytic lesion persisted and the patient’s quality of life had deteriorated facilitated the decision in favor of the treatment.
The PVP procedure allows the option of preserving the mobility of the upper cervical spine. On the other hand, posterior stabilization leads to fixation from the occipital bone to the C4 vertebra, resulting in a considerable decrease in mobility. If sufficient stabilization is not achieved with PVP, the surgical option is still available.
During the past 5 years, 14 of the 350 vertebra treated with PVP at our hospital presented with metastases in the cervical spine. However, this was the first time that we had to deal with an osteolytic lesion of C2. The authors of the three case reports and the series of 12 patients treated with PVP at C2 that we found in our review are among the pioneers and are among the most experienced PVP specialists in the world. However, Mont’Alverne et al. [12] reported two severe clinical complications (16%) in their study: one patient with transient occipital neuralgia and another with an ischemic stroke. This is a higher complication rate than that reported for PVP treatment in vertebral metastases and MM.
Conclusions
Osteolytic lesions of the axis are uncommon and PVP of C2 is associated with high risk of complications. The results of the hitherto published reports and the outcome of our own patient are encouraging. PVP has shown to offer rapid and lasting pain relief and stabilization allowing rapid mobilization. PVP is a less aggressive procedure than any surgical stabilizing procedure in the upper cervical spine and does not restrict the mobility of the occipito-cervical junction. The patient can usually walk a couple of hours after treatment, and can be discharged from hospital within 24 h of the procedure. Considering the higher risk of complications of PVP in this region, it is highly recommended that the treatment be performed by an experienced specialist at a center where many PVP procedures are carried out and which has excellent radiological equipment.
References
- 1.Abitbol JJ, Botte MJ, Garfin SR, Akeson WH (1989) The treatment of multiple myeloma of the cervical spine with halo vest. J Spinal Disord Dec (4):263–267 [PubMed]
- 2.Barragan-Campos HL, Vallée JN, Lo D, Cormier E, Jean B, Rose M, Astagneau P, Chiras J. Percutaneous vertebroplasty for spinal metastases: complications. Radiology. 2006;238(1):354–362. doi: 10.1148/radiol.2381040841. [DOI] [PubMed] [Google Scholar]
- 3.Cotten A, Dewatre F, Cortet B. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200:525–530. doi: 10.1148/radiology.200.2.8685351. [DOI] [PubMed] [Google Scholar]
- 4.Deramond H, Deprestire C, Galibert P. Percutaneous ertebroplasty with polymethyl methacrylate. Technique, indications and results. Radiol Clin North Am. 1998;36(3):533–546. doi: 10.1016/S0033-8389(05)70042-7. [DOI] [PubMed] [Google Scholar]
- 5.Fuchs G, Schwarz G, Baumgartner A, Kaltenbock F, Voit-Augustin H, Planinz W. Fiberoptic intubation in 327 patients with lesions of the cervical spine. J Neurosurg Anesthesiol. 1999;11(1):11–16. doi: 10.1097/00008506-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Fung KY, Law SW. Management of malignant atlanto-axial tumours. J Orthop Surg. 2005;13(3):232–239. doi: 10.1177/230949900501300304. [DOI] [PubMed] [Google Scholar]
- 7.Gailloud P, Martin JB, Olivi A, Rűfenacht DA, Murphy KJ. Transoral vertebroplasty for a fractured C2 aneurysmal bone cyst. J Vasc Interv Radiol Mar. 2002;13(3):340–341. doi: 10.1016/S1051-0443(07)61733-3. [DOI] [PubMed] [Google Scholar]
- 8.Galibert P, Deramond H, Rosat P, Le Gards D (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33:166–168 [French] [PubMed]
- 9.Guglielmi G, Andreula C, Muto M, Gilula LA Percutaneous vertebroplasty: indications, contraindications, technique, and complications. Acta Radiol. 2005;46(3):256–268. doi: 10.1080/02841850510021049. [DOI] [PubMed] [Google Scholar]
- 10.Jenis LG, Dunn EJ, An HS. Metastatic disease of the cervical spine. A review Clin Orthop Relat Res. 1999;359:89–103. doi: 10.1097/00003086-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Martin JB, Gailloud P, Dietrich P-Y, Luciani ME, Somon T, Sappino P-A, Rűfenacht DA. Direct transoral approach to C2 for percutaneous vertebroplasty. Cardiovasc Intervent Radiol. 2002;25:517–519. doi: 10.1007/s00270-001-0122-7. [DOI] [PubMed] [Google Scholar]
- 12.Mont’Alverne F, Vallée J-N, Cormier E, Guillevin R, Barragan H, Jean B, Rose M, Chiras J. Percutaneous vertebroplasty for metastatic involvement of the axis. AJNR. 2005;26:1641–1645. [PMC free article] [PubMed] [Google Scholar]
- 13.Smith A, Wisloff F, Samson D, on behalf of the UK Myeloma Forum, Nordic Myeloma Study Group and British Committee for Standards in Haematology (2005) Guidelines on the diagnosis and management of multiple myeloma. Br Soc Haematol 132:410–451 [DOI] [PubMed]
- 14.Tong FC, Cloft HJ, Joseph GJ, Rodts GR, Dion JE. Transoral approach to cervical vertebroplasty for multiple myeloma. AJR. 2000;175:1322–1324. doi: 10.2214/ajr.175.5.1751322. [DOI] [PubMed] [Google Scholar]
- 15.Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases:indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996;199:241–247. doi: 10.1148/radiology.199.1.8633152. [DOI] [PubMed] [Google Scholar]