Abstract
Interbody fusion has become a mainstay of surgical management for lumbar fractures, tumors, spondylosis, spondylolisthesis and deformities. Over the years, it has undergone a number of metamorphoses, as novel instrumentation and approaches have arisen to reduce complications and enhance outcomes. Interbody fusion procedures are common and successful, complications are rare and most often do not involve the interbody device itself. We present here a patient who underwent an anterior L4 corpectomy with Harms cage placement and who later developed a fracture of the lumbar titanium mesh cage (TMC). This report details the presentation and management of this rare complication, as well as discusses the biomechanics underlying this rare instrumentation failure.
Keywords: Lumbar spine, Titanium mesh cage, Fracture
Introduction
Interbody fusions have become a mainstay of surgical management for lumbar fractures, tumors, spondylosis, spondylolisthesis and deformities [3, 14, 15, 20]. The technique was pioneered in the early 1930s by Capener, Burns and Mercer who mainly used it for treating tuberculosis and spondylolisthesis [22]. It has since undergone several metamorphoses, as novel instrumentation and approaches have arisen to reduce complications and enhance outcomes. Currently, numerous reports have cited high rates of radiographic and histopathologic fusion and good clinical outcomes in single-level lumbar corpectomies and fusions utilizing cylindrical titanium mesh cage (TMC) placement and pedicle screw fixation [4, 11, 12, 24, 25]. Good radiographic fusion at 24 months post-surgery has been reported to range from 47 to 100% of patients treated with TMC interbody devices [4, 8, 11, 12]. In a meta-analysis by Jacobs et al. [12], the addition of posterior versus anterior instrumentation was found to increase the average fusion rates with TMC interbody devices from 47 to 95% of patients.
Interbody fusion procedures are common and successful, complications are rare (0.4–4.5%) and most often do not involve the interbody device itself, though a review of 88 patients with BAK cages did note a 4.5% rate of significant cage migration postoperatively [1, 8, 9]. Indeed, among interbody fusion procedures, TMC-related complications are relatively uncommon, with cage subsidence being the most frequent complication and device fracture a particularly unusual postoperative complication [6]. To the author’s knowledge, only two instances have been previously reported in literature [4, 21].
We present here a patient who underwent an anterior L4 corpectomy with Harms cage placement and who later developed a fracture of the lumbar TMC. This report details the presentation and management of this rare complication, as well as discusses the biomechanics underlying this rare instrumentation failure.
Case presentation
A 20-year-old male (200 cm tall and of 98 kg weight) was admitted to a regional trauma center after a motor vehicle accident. He sustained an L4 burst fracture with canal compromise and neurologic deficits. He emergently underwent a lumbar laminectomy, decompression and stabilization from L3 through L5 with pedicle screw instrumentation and a posterior-lateral fusion. Subsequently, he was transferred to a rehabilitation center 10 weeks after his initial injury. He was reevaluated with plain X-rays and a myelogram, with a post myelogram CT. His X-rays demonstrated the instrumentation to be in good position with some degree of loss of lumbar lordosis (Fig. 1). The myelographic studies demonstrated severe canal compromise from the vertebral bony fragments. Given his lack of neurologic improvement after his initial surgery at the regional trauma center and the degree of canal compromise, it was felt that he might benefit from anterior decompression and fusion. He underwent a retroperitoneal approach, L4 vertebrectomy, decompression of the thecal sac, ventral reconstruction with a Harms titanium cage and fusion with autograft harvested from the vertebrectomy. The Harms cage was cut to the appropriate size, reinforced with rings at either end and packed with an autologous bone graft (Fig. 2). Postoperatively, he improved neurologically to his pre-injury baseline. He regained bowel and bladder function and was able to ambulate with the aid of an ankle/foot orthosis.
Fig. 1.
Lateral radiograph of the lumbar spine demonstrating fractured L4 vertebra and posterior fixation at L3 and L5
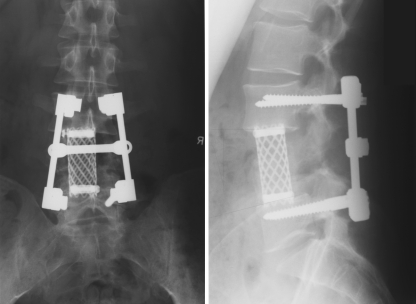
Fig. 2.
Postoperative AP and lateral X-rays showing Harms cage situated correctly in place of the L4 vertebral body
At his 12-month follow-up, his X-rays demonstrated early fusion with bone bridging from L3 through L5 anterior to the cage. His sagittal balance remained unchanged from its early postoperative state.
The patient experienced acute onset of a crepitating noise in his back, 1 month later. Radiographs obtained at that time demonstrated fracture and collapse of the Harms cage (Fig. 3). It was felt that although early evidence of fusion, anteriorly, had occurred, the patient had a posterior pseudoarthosis, with loss of normal lumbar lordosis and with subsequent stress and failure of the anterior instrumentation. Various options were discussed with the patient. The patient elected to undergo a two-stage revision: a transperitoneal removal of the fractured cage and reconstruction with a distractible cage and autograft fusion, followed by exploration of the posterior instrumentation and arthrodesis. During the anterior approach, it was noted that the cage had fractured, and two loose pieces of the cage were easily extracted. The remainder of the cage had incorporated into the endplates above and below. The remainder of the cage was removed. The anterior column was reconstructed with an expandable titanium cage. The second stage was planned to be performed in a delayed fashion. Unfortunately, the patient developed pancreatitis 6 weeks after the first stage procedure. He subsequently underwent revision of the posterolateral fusion 4 months later. He recovered from this operation uneventfully. On the 6-month follow-up, he has been doing well, with no evidence of pseudoarthosis or instrumentation failure (Fig. 4).
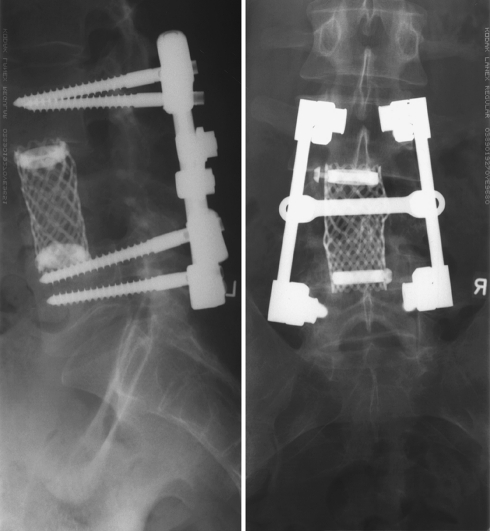
Fig. 3.
Follow-up AP and lateral X-rays displaying the previously placed Harms titanium mesh cage. Note the slight decrease in cage height and multiple fracture points in the cage
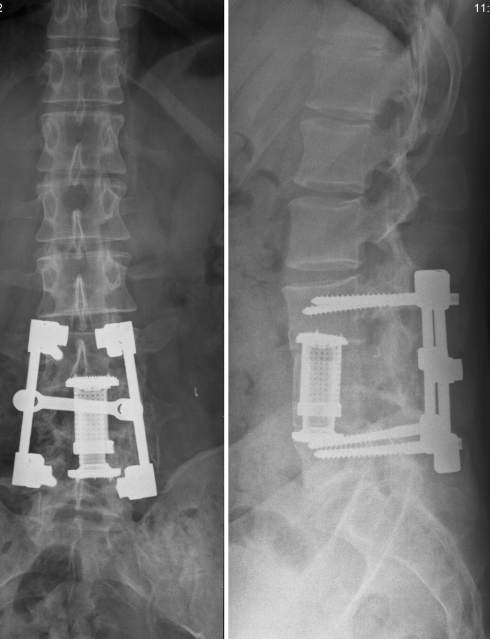
Fig. 4.
Postoperative AP and lateral X-rays following reoperation for retrieval and replacement of the fractured Harms cage. An expandable Synex® (Synthese) cage has been exchanged for the fractured titanium mesh cage
Discussion
The use of interbody devices, such as the Harms cage, has become increasingly common over the last decade. TMCs offer several advantages, including immediate anterior stabilization, re-approximation of the intervertebral disc height and obviation of bone graft harvesting from outside the surgical site [13, 19]. Additionally, they may relax bending movements on accessory instrumentation, such as anterior plating systems or posterior transpedicular fixation, by providing early anterior column support and enhancing bony fusion over time. Inevitable subsidence of the sharp edges of the cage into the adjacent endplates acts against dislocation. Such added support may actually help reduce instrumentation failure after anterior corpectomies [2, 18].
Stability
The strength of any instrumented fusion will depend in part upon the stiffness of the construct and in part upon the degree of eventual bony fusion. Several biomechanical models have investigated the strength of Harms TMCs in the lumbar spine and found it to be adequate for reconstruction of the anterior column. Testing in a calf lumbar spine model has demonstrated superior stability, regardless of anterior or posterior fixation, with the Harms cage compared to old polymethylmethacrylate (PMMA) or autograft vertebral body reconstructions [18]. When pitted against expandable and threaded interbody devices in the lumbar spine, in vitro biomechanical studies have revealed Harms TMCs to be comparable or better in load sharing and stability, though subsidence remains slightly more common among Harms cages [16, 17]. Additionally, Harms cages have been shown to support good alignment postoperatively under in vivo stresses for over 2 years in close follow-up, with good evidence of bony fusion [5].
Indeed, bony fusion rates with Harms cages are significantly higher than non-instrumented fusion rates (95–100% vs. 89.7%) [10–12, 19, 23]. Epari et al. [7] have theorized that fusion may be aided in the Harms cage and other cylindrical TMCs by their proclivity for subsidence. As the intervertebral height decreases slightly, loading on the bone graft within the cage increases, providing mechanical signals for bone growth. Histological review of bone from within the Harms cages in two different series found evidence of viable bone in 100% of cases at an average of 2 years postoperatively, attesting to the high fusion rates of these cages. In both series, though, necrotic bone was identified within the cages alongside viable tissue, indicating that fusion was yet incomplete 2 years postoperatively. Such histological evidence of still progressing fusions also occurred in patients with good radiological evidence of fusion in and around the cages [24, 25].
Prognosis/treatment
Interestingly, two previous cases of cage fracture in the lumbar spine also showed good radiological fusion around the cages, despite obvious instrumentation failure, hinting that such fractures may not be related to instability in the overall fusion, but part of the fusion process itself. In both cases, the patients were asymptomatic [4, 21].
Conclusion
This case demonstrates the above-mentioned properties of the Harms TMC. Good initial stability, very good bony healing at the ends and sides of the cage, and some necrotic bone in the middle of the cage were all observed. Like in femur fractures, where repeated minimal bending forces associated with full weight-bearing may lead to failure of fixation, the anterior fusion in this case was not able to heal fast enough to relieve the significant stresses on the cage and it finally failed. The size of the patient, as well as his high level of activity, should also be considered and undoubtedly contributed to the fracture of the Harms TMC.
The insertion technique may be questioned, as well. Gentle tapping on the cage could have inflicted minor damage to the cage structure, although in this case placement of the cage was done by impacting it on the sides with the reinforcing rings.
In patients with multiple injuries, reduction, stabilization and decompression should be done from a posterior approach. If time and patient condition allow, a posterolateral fusion is recommended. Anterior surgery is indicated when additional anterior column support or decompression of the thecal sac are needed, like in this case. This is usually performed in a staged fashion.
References
- 1.Chen L, Yang H, Tang T. Cage migration in spondylolisthesis treated with posterior lumbar interbody fusion using BAK cages. Spine. 2005;30:2171–2175. doi: 10.1097/01.brs.0000180402.50500.5b. [DOI] [PubMed] [Google Scholar]
- 2.Das K, Couldwell WT, Sava G, Taddonio RF. Use of cylindrical titanium mesh and locking plates in anterior cervical fusion. J Neurosurg. 2001;94:174–178. doi: 10.3171/spi.2001.94.1.0174. [DOI] [PubMed] [Google Scholar]
- 3.Dewald RL, Bridwell KH, Prodromas C, Rodts MF. Reconstructive spinal surgery as palliation for metastatic malignancies of the spine. Spine. 1985;10:21–26. doi: 10.1097/00007632-198501000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Dvorak MF, Kwon BK, Fisher CG, Eiserloh HL, Boyd M, Wing PC. Effectiveness of titanium mesh cylindrical cages in anterior column reconstruction after thoracic and lumbar vertebral body resection. Spine. 2003;28:902–908. doi: 10.1097/00007632-200305010-00012. [DOI] [PubMed] [Google Scholar]
- 5.Eck KR, Bridwell KH, Ungacta FF, Lapp MA, Lenke LG, Daniel Riew K. Analysis of titanium mesh cages in adults with minimum two-year follow-up. Spine. 2000;25:2407–2415. doi: 10.1097/00007632-200009150-00023. [DOI] [PubMed] [Google Scholar]
- 6.Eck KR, Lenke LG, Bridwell KH, Ungacta FF, Lapp MA, Lenke LG, Daniel Riew K. Radiographic assessment of anterior titanium mesh cages. J Spinal Disord. 2000;13:501–509. doi: 10.1097/00002517-200012000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Epari DR, Kandziora F, Duda GN. Stress shielding in box and cylinder cervical interbody fusion cage designs. Spine. 2005;30:908–914. doi: 10.1097/01.brs.0000158971.74152.b6. [DOI] [PubMed] [Google Scholar]
- 8.Freeman BJ, Licina P, Mehdian SH Posterior lumbar interbody fusion combined with instrumented postero-lateral fusion: 5-year results in 60 patients. Eur Spine J. 2000;9:42–46. doi: 10.1007/s005860050007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gill K, Blumenthal SL. Posterior lumbar interbody fusion: a 2-year follow-up of 238 patients. Acta Orthop Scand. 1993;64(Suppl 251):108–110. doi: 10.3109/17453679309160137. [DOI] [PubMed] [Google Scholar]
- 10.Hee HT, Madj ME, Holt RT, Whitecloud, Thomas S, Pienkowski D. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord. 2003;16:1–8. doi: 10.1097/00024720-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Hwang SL, Hwang YF, Lieu AS, Lin CL, Kuo TH, Su YF, Howng SL, Lee KS. Outcome analyses of interbody titanium cage fusion used in the anterior discectomy for cervical degenerative disc disease. J Spinal Disord Tech. 2005;18:326–331. doi: 10.1097/01.bsd.0000164198.30725.2d. [DOI] [PubMed] [Google Scholar]
- 12.JacobsWCH, Vreeling A, Kleuver M. Fusion for low-grade adult isthmic spondylolisthesis: a systematic review of the literature. Eur Spine J. 2005;15(4):391–402. doi: 10.1007/s00586-005-1021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanayama M, Hashimoto T, Shigenobu K, Oha F, Ishida T, Yamane S. Pitfalls of anterior cervical fusion using titanium mesh and local autograft. J Spinal Disord Tech. 2003;16:513–518. doi: 10.1097/00024720-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kaneda K, Abumi K, Fujiya M. Burst fractures with neurologic deficits of the thoracolumbar-lumbar spine: results of anterior decompression and stabilization with anterior instrumentation. Spine. 1984;9:788–95. doi: 10.1097/00007632-198411000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Kostuik JP. Anterior fixation for burst fractures of the thoracic and lumbar spine with or without neurological involvement. Spine. 1988;13:286–93. doi: 10.1097/00007632-198803000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Knop C, Lange U, Bastian L, Oeser M, Blauth M. Biomechanical compression testswith a new implant for thoracolumbar vertebral body replacement. Eur Spine J. 2001;10:30–37. doi: 10.1007/s005860000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar N, Judith MR, Kumar A, Mishra V, Robert MR. Analysis of stress distribution in lumbar interbody fusion. Spine. 2005;30:1731–1735. doi: 10.1097/01.brs.0000172160.78207.49. [DOI] [PubMed] [Google Scholar]
- 18.Lee SW, Lim TH, You JW, An HS. Biomechanical effect of anterior grafting devices on the rotational stability of spinal constructs. J Spinal Disord. 2000;13:150–155. doi: 10.1097/00002517-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Madj ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine. 1999;24:1604–1610. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 20.O’Neil J, Gardner V, Amstrong G. Treatment of tumors of the thoracic and lumbar spinal column. Clin Orthop Relat Res. 1986;227:103–112. [PubMed] [Google Scholar]
- 21.Robertson PA, Rawlinson HJ, Hadlow AT. Radiologic stability of titanium mesh cages for anterior spinal reconstruction following thoracolumbar corpectomy. J Spinal Disord Tech. 2004;17:44–52. doi: 10.1097/00024720-200402000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Sacks S. Anterior interbody fusion of the lumbar spine. J Bone Joint Surg Br. 1965;47:211–223. [PubMed] [Google Scholar]
- 23.ThalgottJS, Xiongsheng C, Giuffre JM. Single stage anterior cervical reconstruction with titanium mesh cages, local bone graft, and anterior plating. Spine J. 2003;3:294–300. doi: 10.1016/S1529-9430(02)00588-0. [DOI] [PubMed] [Google Scholar]
- 24.Togawa D, Bauer TW, Brantigan JW, Lowery GL. Bone graft incorporation in radiographically successful human intervertebral body fusion cages. Spine. 2001;26:2744–2750. doi: 10.1097/00007632-200112150-00025. [DOI] [PubMed] [Google Scholar]
- 25.Togawa D, Bauer TW, Lieberman IH, Lowery GL, Takikawa S. Histology of tissues within retrieved human titanium mesh cages. Spine. 2003;28:246–253. doi: 10.1097/00007632-200302010-00008. [DOI] [PubMed] [Google Scholar]