Abstract
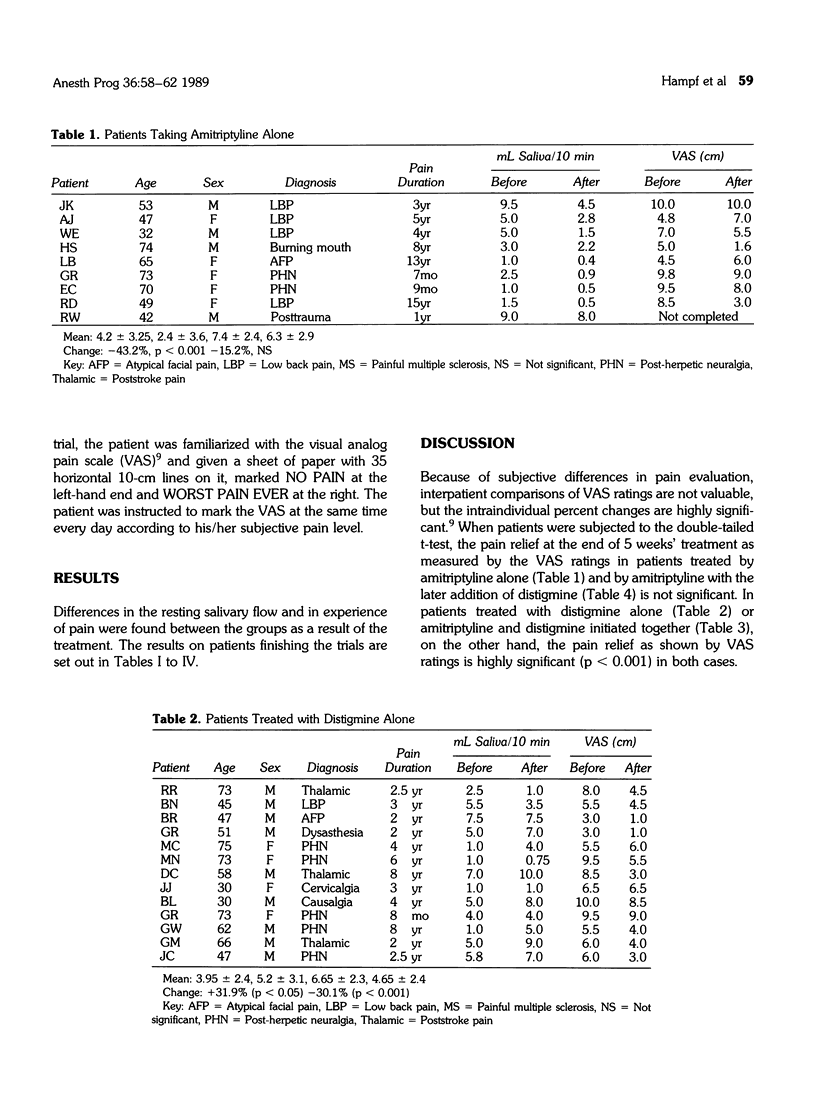
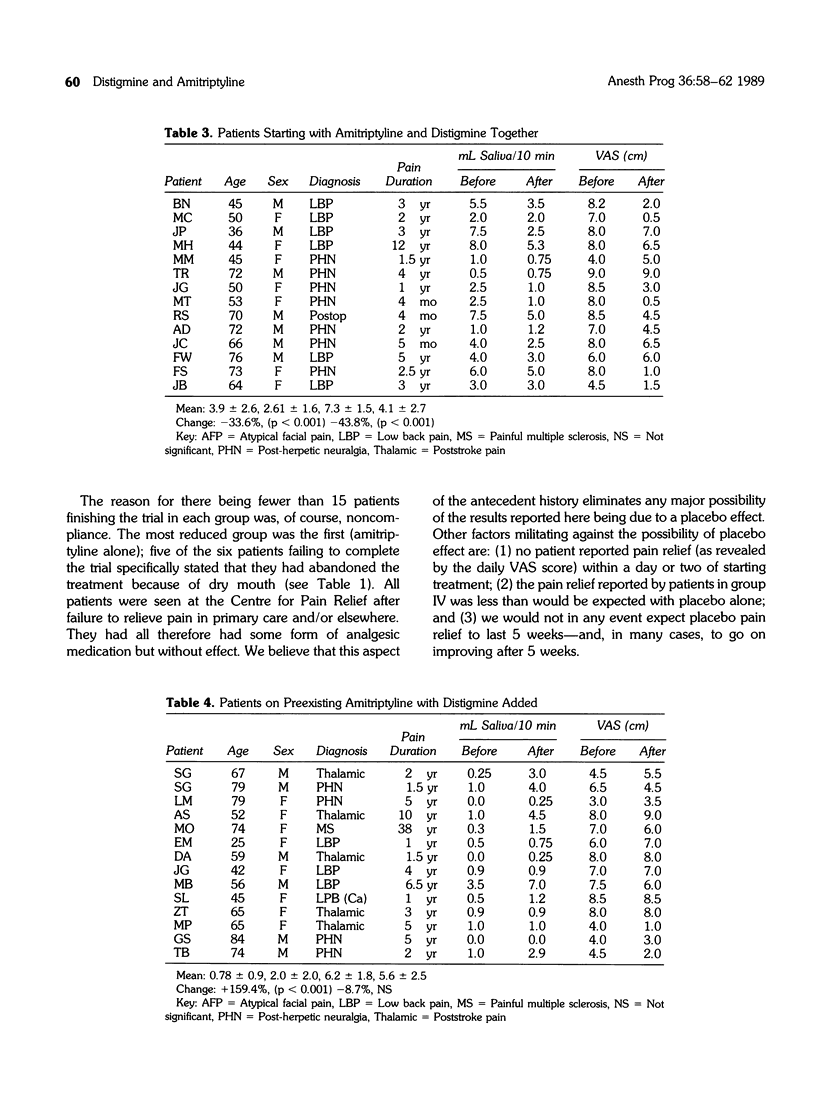
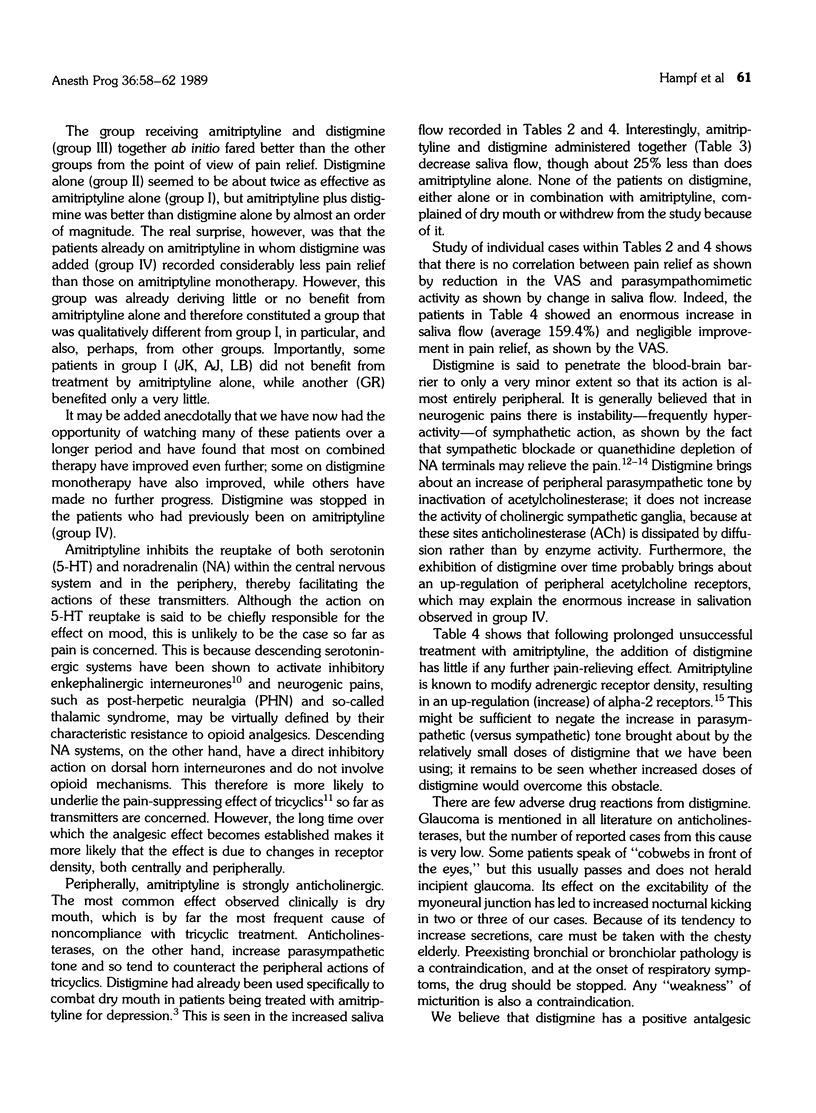
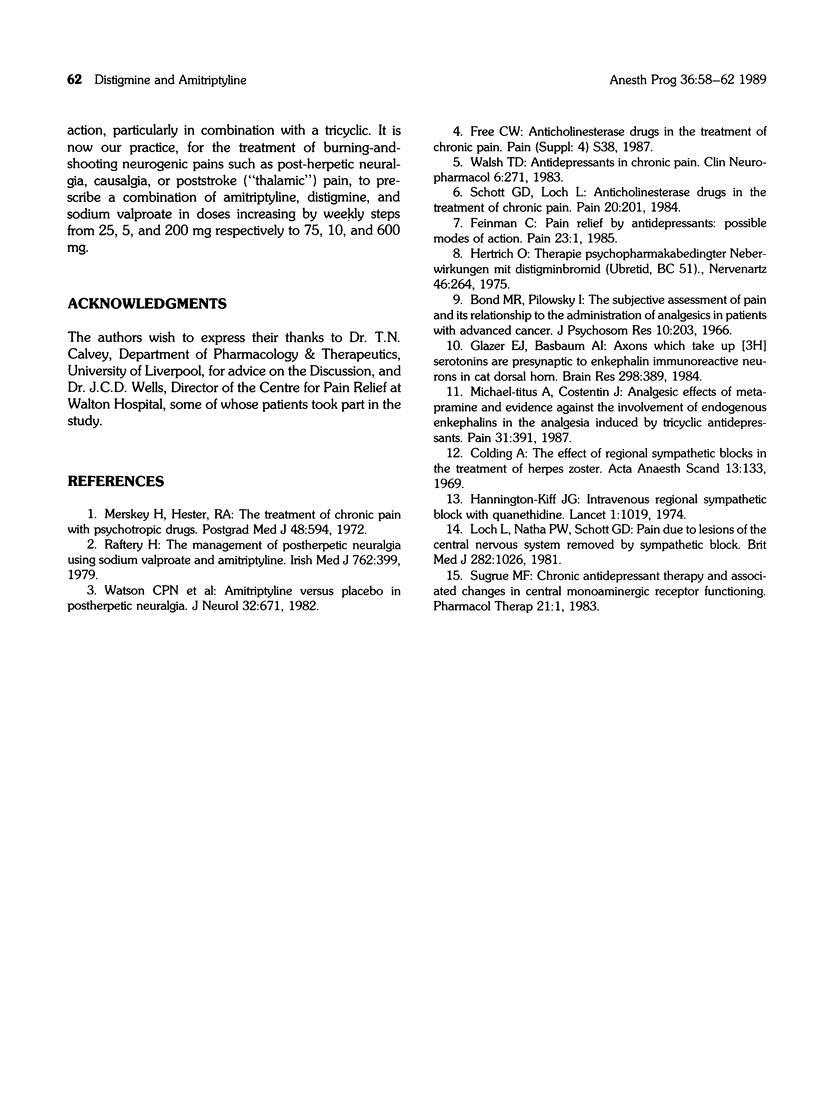
Sixty-five patients attending a pain relief clinic were randomly allocated to treatment for 5 weeks with amitriptyline alone, distigmine alone, amitriptyline and distigmine started together, or addition of distigmine to preexisting treatment with amitriptyline. Forty-eight patients successfully completed the trial; the most common cause for withdrawal was dry mouth in the amitriptyline-alone group. Two parameters were measured: Pain intensity was measured at the beginning and end of the treatment, and the saliva flow was measured at the beginning and the end of the treatment. At the end of 5 weeks, treatment with a combination of amitriptyline (75 mg/day) and distigmine (10 mg/day) resulted in a 43% reduction of pain and no subjectively noticeable mouth dryness. Distigmine alone also decreased pain and increased saliva flow, sometimes to the point of discomfort, whereas amitriptyline alone, in this particular series, did not significantly reduce pain and produced unpleasant mouth dryness. The addition of distigmine to preexisting (and ineffective) amitriptyline treatment failed to relieve pain. We therefore conclude that a combination of amitriptyline and distigmine (both given ab initio) may be a useful therapy for chronic pain.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bond M. R., Pilowsky I. Subjective assessment of pain and its relationship to the administration of analgesics in patients with advanced cancer. J Psychosom Res. 1966 Sep;10(2):203–208. doi: 10.1016/0022-3999(66)90064-x. [DOI] [PubMed] [Google Scholar]
- Feinmann C. Pain relief by antidepressants: possible modes of action. Pain. 1985 Sep;23(1):1–8. doi: 10.1016/0304-3959(85)90223-4. [DOI] [PubMed] [Google Scholar]
- Hannington-Kiff J. G. Intravenous regional sympathetic block with guanethidine. Lancet. 1974 May 25;1(7865):1019–1020. doi: 10.1016/s0140-6736(74)90418-8. [DOI] [PubMed] [Google Scholar]
- Hertrich O. Therapie psychopharmakabedingter Nebenwirkungen mit Distigminbromid (UBRETID, BC 51) Nervenarzt. 1976 May;46(5):264–267. [PubMed] [Google Scholar]
- Loh L., Nathan P. W., Schott G. D. Pain due to lesions of central nervous system removed by sympathetic block. Br Med J (Clin Res Ed) 1981 Mar 28;282(6269):1026–1028. doi: 10.1136/bmj.282.6269.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merskey H., Hester R. A. The treatment of chronic pain with psychotropic drugs. Postgrad Med J. 1972 Oct;48(564):594–598. doi: 10.1136/pgmj.48.564.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael-Titus A., Costentin J. Analgesic effects of metapramine and evidence against the involvement of endogenous enkephalins in the analgesia induced by tricyclic antidepressants. Pain. 1987 Dec;31(3):391–400. doi: 10.1016/0304-3959(87)90167-9. [DOI] [PubMed] [Google Scholar]
- Schott G. D., Loh L. Anticholinesterase drugs in the treatment of chronic pain. Pain. 1984 Oct;20(2):201–206. doi: 10.1016/0304-3959(84)90101-5. [DOI] [PubMed] [Google Scholar]
- Sugrue M. F. Chronic antidepressant therapy and associated changes in central monoaminergic receptor functioning. Pharmacol Ther. 1983;21(1):1–33. doi: 10.1016/0163-7258(83)90065-7. [DOI] [PubMed] [Google Scholar]
- Walsh T. D. Antidepressants in chronic pain. Clin Neuropharmacol. 1983;6(4):271–295. [PubMed] [Google Scholar]



