Abstract
Objective
Research suggests that overweight and obesity are associated with depressive symptoms, particularly among women. Evidence from weight control trials suggests that higher weighing frequency is associated with greater weight loss or less weight gain. As limited data exist on the effects of self-weighing on body mass index (BMI) among overweight adults with or without depression, this study seeks to examine this issue using data from a population-based epidemiologic survey.
Methods
Data from a large population-based survey of 4,655 women ages 40-65 in the greater Seattle area, surveyed from November 2003 to February 2005, were used to examine associations of depression and weight self-monitoring with BMI. Sample-weighted regression models were used to examine associations of depression, self-weighing frequency, and BMI, with demographic factors (race/ethnicity, employment status, smoking status, age, martial status, educational attainment) entered as covariates.
Results
Regression models indicated that higher self-weighing frequency and negative depression status were independently associated with lower BMI, with no interaction observed between depression and self-weighing.
Conclusion
Frequent self-weighing appears to be associated with lower BMI in both depressed and nondepressed overweight women.
Keywords: Health behavior, depression, body mass index, women
Introduction
Rates of overweight [body mass index (BMI) > 25 kg/m2)] and obesity (BMI > 30 kg/m2) are increasing in the United States; 66% of adults are overweight and 32% are obese (Flegal et al., 2002; Hedley et al., 2004; Ogden et al., 2006). To counter these increasing rates, attention to the health impact of behavioral interventions for weight control has increased as well (Jeffery et al., 2000; Wing, 1998). Of additional concern to population health, research suggests that overweight and obesity are associated with depressive symptoms, particularly among women (Carpenter et al., 2000; Onyike et al., 2003; Simon et al., 2006).
Monitoring of daily calorie intake or physical activity behaviors has been associated with improved weight loss and maintenance (Baker & Kirschenbaum, 1998; Boutelle et al., 1999; Carels et al., 2005; Perri et al., 1989; Wadden & Letizia, 1992). Evidence from surveys of successful weight losers (McGuire et al., 1998; McGuire et al., 1999) and from behavioral weight control trials (Linde et al., 2005) suggests that greater frequency of weight self-monitoring is associated with greater weight loss or less weight gain. Among participants in a weight loss trial, more frequent self-weighing also was cross-sectionally associated with BMI at baseline (Linde et al., 2005); whether this finding applies to populations not seeking weight loss treatment has yet to be tested fully.
Daily weighing may provide feedback that can lead to favorable changes in weight regulation (Levitsky et al., 2006), but little is known about whether this feedback is associated with negative emotional states. Proponents of cognitive-behavioral interventions for weight loss recommend weekly weighing, cautioning that more frequent weighing may lead individuals to “feel disheartened by days on which there is no apparent gain or loss” (Cooper, Fairburn, & Hawker, 2003), or to “despair when the scale shows no change” (Brownell, 2004), although data to support these claims are not presented.
Studies have approached weighing in the context of mood, body image, and self-esteem in samples of normal-weight young adult volunteers (Ogden & Evans, 1996; Ogden & Whyman, 1997). In one study, participants were assigned to one of three experimental conditions: after being weighed by researchers, participants were told they were underweight, of average weight, or overweight. Mood and self-esteem ratings taken after the weighing manipulation indicated that participants in the overweight group showed increased depression and decreased self-esteem over time; the authors concluded that weighing and the normative comparisons that follow may be psychologically harmful (Ogden & Evans, 1996). Another study of normal-weight college-aged women assigned participants to either daily weighing for two weeks or weighing on the first and last days of a two-week period (the non-weighing condition) and asked them to rate their mood and self-esteem after two weeks. Results indicated that, relative to the non-weighing group, participants in the weighing group had increased self-ratings of depression and anxiety and lower ratings of self-esteem over the two weeks (Ogden & Whyman, 1997). The applicability of these studies to self-weighing recommendations in behavioral weight control is limited, however. Sample sizes in each study were small (N = 74 and 30, respectively), the first study did not employ self-weighing in its design (Ogden & Evans, 1996), and each study involved the recruitment of normal-weight young adult volunteers rather than overweight women.
Although at least two studies have addressed the question of the impact of weight self-monitoring on weight and weight control outcomes, we know of no published data on the associations of self-weighing, mood states and BMI among overweight adults. To begin to address this question, the present study examined cross-sectional associations of self-weighing frequency, depression, and BMI among adult women recruited from a health plan population for an epidemiological survey of depression and obesity.
Methods
Sample Selection
Data were taken from a survey of enrolled members of the Group Health Cooperative (GHC), a group-model prepaid health plan serving 500,000 members in Washington and northern Idaho. Member enrollment is demographically similar to the population of the Seattle area, from which the current sample was drawn, in terms of age, gender, and ethnic minority representation (Simon et al., 1996). Of these members, all women aged 40 or older are invited to complete periodic questionnaires regarding breast cancer risk factors, including height and weight; approximately 85% participate in these periodic screenings (see Taplin et al., 1990 for program details). Existing data from this Group Health Breast Cancer Screening Program (BCSP) were used to identify three strata for sampling based on self-reported BMI status from the most recently available BCSP questionnaire [BMI < 30, BMI ≥ 30, or BMI unknown (did not participate in BCSP)]. Survey eligibility was based on age (40-65), gender (women only), and GHC enrollment. The survey was designed to provide data on obesity and depression rates in a community sample of women ages 40-65; in order to over-sample women expected to have higher BMI values for subsequent recruitment into a weight loss treatment study, women who last reported BMI ≥ 30 or more were sampled at 100% (N = approximately 5207), women who last reported BMI < 30 were sampled at 12% (N = approximately 1874), and women who did not complete a screening questionnaire were sampled at 25% (N = approximately 919). This stratified sampling procedure was intended to increase the efficiency of the survey and to permit correction for differences in response rates. All analyses incorporated sampling weights (see Data Analysis below) so that results accurately reflect the entire target population. The final sample was composed of women aged 40-65, members of eight GHC clinics in the greater Seattle area, who were surveyed between November 2003 and February 2005. All study procedures were approved by the GHC institutional review board.
Procedure and Measures
All sampled participants (N = 8000) were mailed an invitation letter that described informed consent for the study and included a phone number by which to decline participation; those who did not decline were contacted by trained interviewers who conducted telephone surveys to collect data and to screen individuals for participation in a weight loss and depression treatment study conducted by the same research team. Interviewers received a total of 12 hours of general and project-specific interview training. Contact protocols for the survey required a minimum of nine contact attempts, including evening and weekend times. The survey began with a detailed informed consent procedure and included demographic data (age, race/ethnicity, marital status, educational attainment, employment status), self-reported height and weight, smoking status (current and past) dietary intake, and physical activity information.
Self-weighing frequency was assessed by asking a single item, “How often do you weigh yourself?” Response categories included never, at least once a year but not as often as once a month, 1-3 times a month, 1-6 times a week, once a day, and twice a day or more. In order to better compare the present findings with previous examinations of self-weighing frequency (Linde et al., 2005), and due to the rare report of self-weighing twice a day or more (n = 32, 0.69% of sample) categories were collapsed into never, monthly, weekly, and daily weighing frequencies.
Depression was assessed by the nine-item Patient Health Questionnaire (Spitzer et al., 1999), a self-report measure of depressive symptoms based on the DSM-IV criteria for diagnosis of major depressive disorder (American Psychiatric Association, 1994). This self-report measure has demonstrated strong agreement with structured interviews by clinicians in general medical outpatient and inpatient samples (Diez-Quevado et al., 2001; Kroenke et al., 2001; Spitzer et al., 1999), and has demonstrated validity in a representative community sample (Martin et al., 2006). The PHQ was scored for diagnosis of current major depression based on DSM-IV criteria as well as dimensionally (range = 0-27 for all nine items). A diagnosis of major depression required responses of “more than half the time” or “nearly all the time” to one of the two core symptoms (depressed mood or loss of interest) as well as five additional symptoms. Depression status was coded as negative (did not meet criteria and PHQ < 10), symptomatic (did not meet criteria but PHQ > 10) or positive (met DSM-IV criteria according to PHQ).
Data Analysis
All analyses were conducted using SAS/STAT® software, Version 9.1. To account for stratified sampling procedures and differential response rates across strata, all analyses incorporated sampling weights (Cochran, 1977) using SAS SURVEYFREQ, SURVEYMEANS, AND SURVEYREG procedures. Sample-weighted means and frequencies were calculated for demographics and variables of interest (BMI, depression status, self-weighing). Regression models were used to examine associations of depression, self-weighing frequency, and BMI, with demographic factors (race/ethnicity, employment status, smoking status, age, martial status, educational attainment) entered as covariates. Two-tailed tests of significance were used to interpret all findings.
Results
Sample Description
Of 8,000 potential participants mailed invitation letters, 442 were found to be ineligible (due to having died or no longer having GHC health plan coverage). Of the remaining 7558 eligible women, 865 could not be reached by telephone and 2033 declined to participate, resulting in 4660 women (62% of those eligible) who completed a telephone survey. Data from an additional five women were excluded due to outlying height or weight variables that could not be verified for accuracy. Available data on nonresponders indicate that, compared to those who completed a survey, women who declined participation or who could not be reached were younger [51.8 vs. 52.4 years, t(7998) = -4.06, p < 0.0001] and had lower average BMI [33.3 vs. 34.0 kg/m2, t(5532) = -3.95, p < 0.0001].
Among those who completed a survey, sample weighted mean age was 52.1 years, sample weighted mean BMI was 28.3 kg/m2 (standard error = 0.11; 95% confidence interval = 28.11-28.54; range = 15.81-74.88), 65.8% were married, 66.5% had completed at least 2 years of college, and 70.0% were employed. Nearly 4% were of Hispanic origin, and 82.4% were white. Thirty-seven percent reported never weighing themselves, 27% reported weighing themselves monthly, 24% reported weighing themselves weekly, and 12% reported weighing themselves daily. Weighted prevalence of current major depression was 5.1%; an additional 7.8% had a PHQ score greater than 10, suggesting moderate symptoms.
Table 1 presents mean BMI values by depression and self-weighing frequency categories; values are adjusted to reflect sampling weights. Results of weighted chi-square analyses [χ2(6) = 27.72, p < 0.05] and the unadjusted correlation between depression status and self-weighing (r = -0.04, p < 0.01) were statistically significant (see Figure 1). The association between depression and self-weighing was no longer statistically significant after adjusting for BMI [Wald χ2(3) = 6.82, p > 0.05); r = -0.02, p > 0.10].
Table 1.
Body mass index (kilograms/meters2) by depression and self-weighing frequency categories among women ages 40-65 surveyed in Seattle, Washington from November 2003-February 2005.
| Variable | N | Mean | SE |
|---|---|---|---|
| Depression Status | |||
| Not depressed, PHQ < 10 | 3895 | 27.79 | 0.11 |
| Major Depression criteria not met, PHQ > 10 | 466 | 32.07 | 0.56 |
| Major Depression criteria met | 276 | 32.10 | 0.54 |
| Weighing Frequency | |||
| Never | 1692 | 29.05 | 0.21 |
| Monthly | 1296 | 28.58 | 0.21 |
| Weekly | 1130 | 27.80 | 0.21 |
| Daily | 484 | 26.85 | 0.24 |
Note. All means are adjusted to reflect sampling weights. PHQ = Patient Health Questionnaire; a score > 10 indicates the presence of moderate depressive symptoms. SE = standard error of the mean.
Figure 1.
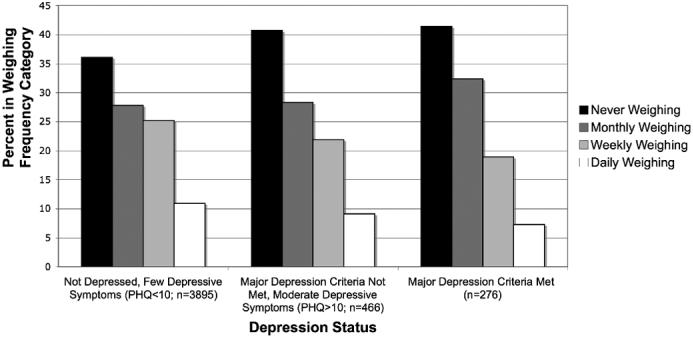
Percent of sample in each weighing frequency category by depression status category. Sample sizes are adjusted to reflect sampling weights. PHQ = Patient Health Questionnaire; a score > 10 indicates the presence of moderate depressive symptoms. Subjects were women ages 40-65 surveyed in Seattle, Washington from November 2003-February 2005.
Associations of Depression and Self-Weighing Frequency with BMI
An initial regression of depression, self-weighing frequency, and their interaction on BMI was examined; no other covariates were considered in this initial model. Depression was positively related and self-weighing frequency was negatively related to BMI [F(2, 4,590) = 39.53 and F(3, 4,590) = 7.16, p < 0.0001]; however, the depression by self-weighing interaction term was not statistically significant [F(6, 4,590) = 0.73, p = 0.63]. Thus, only main effects were considered further in a weighted regression model examining the associations of depression and self-weighing frequency on BMI.
Results of the regression of depression status (three categories, as presented in Figure 1) and self-weighing frequency (four categories, as presented in Figure 1) on BMI, adjusting for demographic factors (age, marital status, education level, race/ethnicity, employment status, smoking history, current smoking) are presented in Tables 2 and 3. The overall model was statistically significant [F(14, 4,578) = 19.63, p < 0.0001] and accounted for 10.2% of the variance in BMI. After adjustment for demographic variables, the absence of depression [F(2, 4,578) = 29.78, p < 0.0001] and greater self-weighing frequency [F(3, 4,578) = 6.95, p = 0.0001] were independently associated with lower BMI; results are comparable with those from the initial unadjusted model noted above. Comparisons of weighted, adjusted means presented in Table 3 suggest that daily weighing frequency, more so than weekly or monthly frequency, and the absence of depressive symptoms (compared to those with PHQ > 10 or those with major depression) are associated with lower average BMI.
Table 2.
Weighted regression of depression and self-weighing frequency on body mass index (kilograms/meters2) among women ages 40-65 surveyed in Seattle, Washington from November 2003-February 2005.
| Predictor | B | SE B | p |
|---|---|---|---|
| Depression Status (Major Depression criteria met=reference) | |||
| Not depressed, PHQ < 10 | -5.47 | 0.66 | <.0001 |
| Major Depression criteria not met, PHQ > 10 | 0.14 | 0.92 | .89 |
| Self-Weighing Frequency (Daily=reference) | |||
| Never | 4.23 | 0.38 | <.0001 |
| Monthly | 3.71 | 0.37 | .0002 |
| Weekly | 2.13 | 0.38 | .03 |
Note. N = 4581 due to missing values. Table entries represent unstandardized regression coefficients (B). PHQ = Patient Health Questionnaire; a score > 10 indicates the presence of moderate depressive symptoms. SE = standard error of the regression coefficient. Model is adjusted to reflect sampling weights and includes demographic covariates (age, marital status, education level, race/ethnicity, employment status) and smoking status (current or ever).
Table 3.
Mean adjusted body mass index (kilograms/meters2) by depression status and weighing frequency among women ages 40-65 surveyed in Seattle, Washington from November 2003-February 2005.
| Predictor | n | Adjusted Mean Body Mass Index | SE |
|---|---|---|---|
| Depression Status1 | |||
| Not depressed, PHQ < 10 | 4020 | 27.74a | 1.19 |
| Major Depression criteria not met, PHQ > 10 | 356 | 31.49b | 1.35 |
| Major Depression criteria met | 235 | 31.36b | 1.32 |
| Weighing Frequency2 | |||
| Never | 1693 | 30.86a | 1.19 |
| Monthly | 1241 | 30.62a,b | 1.23 |
| Weekly | 1119 | 30.06b | 1.25 |
| Daily | 559 | 29.24c | 1.27 |
Note. N = 4581 due to missing values. Means and sample sizes for predictor categories (n) are adjusted to reflect sampling weights; as such, sample sizes within each category sum to greater than 100% of the total sample. PHQ = Patient Health Questionnaire; a score > 10 indicates the presence of moderate depressive symptoms. SE = standard error of the mean. Within each predictor group, means with different superscripts are significantly different, p<.05.
Adjusted for weighing frequency and demographic covariates.
Adjusted for depression status and demographic covariates.
Discussion
In this sample of women over 40 enrolled in a health plan, higher self-weighing frequency and absence of depressive symptoms were independently associated with lower BMI. In a replication of findings that have been observed in national surveys of U.S. adults (Carpenter et al., 2000; Onyike et al., 2003; Simon et al., 2006), depression and body weight were cross-sectionally associated in the present sample, suggesting that the current regional sample may be comparable to the broader population with respect to these variables. The association between self-weighing and BMI replicates that observed in a smaller, mixed-gender sample of overweight adults seeking weight loss (Linde et al., 2005). In addition, comparisons of weighted, adjusted means (see Table 3) suggest that daily weighing frequency, more so than monthly or weekly frequency is associated with lower BMI on average, which is congruent with data from population-based surveys of successful weight control (McGuire et al., 1998; McGuire et al., 1999) and from clinic and community-based studies of overweight adults engaged in weight control trials (Linde et al., 2005). These findings suggest that the association between self-weighing and BMI may be applicable to broader samples than those who self-select into weight control trials. The lack of indication in the literature of a differential effect of self-weighing in men versus women (Linde et al., 2005) suggests that the current findings in a sample of women only may be applicable to adult men as well.
Our findings suggest no strong evidence, at least cross-sectionally, that frequent self-weighing and depression are associated in adult women. An observed, unadjusted cross-sectional association between depression and self-weighing was no longer statistically significant after adjusting for BMI, suggesting that BMI contributes to the shared variance between the two variables.
An interaction between depression and self-weighing as related to weight outcomes was not observed, suggesting that the recommendation for regular self-monitoring of weight appears to apply equally well to adults regardless of depression status. As these data are cross-sectional, longitudinal data are needed to better understand causal pathways between weighing frequency and depression in terms of the potential implications for weight loss program recommendations that currently suggest weekly weighing only due to concerns about adverse impact on mood (e.g., Brownell, 2004; Cooper et al., 2003).
Study Limitations and Strengths
One limitation of this study is a reliance on self-report for variables of interest. Although body weights and self-weighing frequencies were obtained by self-report, an examination of self-reported versus measured weights in a subset of participants from this same dataset (Jeffery et al., under review) did not detect any systematic bias in weight reporting between depressed and nondepressed women, and the correlation between self-reported and measured weights was substantial (r = 0.92). We know of no evidence to indicate differential bias in self-reports of weighing frequency by depression status. In addition, the survey response rate (62% of 8000 contacted for the study) and the restricted geographical area from which the sample was drawn (the Washington-Idaho region) may limit our ability to generalize to the broader U.S. or global populations, as might the statistically significant differences between nonresponders and responders in terms of age and BMI. However, these differences are not of a large magnitude (0.6 years for age, 0.7 kg/m2 for BMI) and may owe statistical significance in part to the large sample size. Taken together, the large sample size and the consistency of these results with previous findings in studies that evaluated self-weighing and weight associations using measured body weights (Levitsky et al., 2006; Linde et al., 2005) suggests that the present findings are sound.
Conclusions
Results from this study suggest that, after adjusting for BMI, there is no significant association between depressed mood and self-monitoring of body weight in a community-based sample of adult women. Given that obesity and depression are positively associated and that self-weighing protects against weight gain, the possibility that frequent weighing among those interested in weight control might improve mood as it improves weight should be explored. Future studies should examine the causal links between depression or related cognitive factors and the effectiveness of frequent self-weighing during weight control.
Acknowledgments
This research was supported by National Institute of Mental Health grant R01-MH068127 (G. Simon, PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. fourth edition American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Baker RC, Kirschenbaum DS. Weight control during the holidays: Highly consistent self-monitoring as a potentially useful coping mechanism. Health Psychol. 1998;17:367–370. doi: 10.1037//0278-6133.17.4.367. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME. How can obese weight controllers minimize weight gain during the high risk holiday season? By self-monitoring very consistently. Health Psychol. 1999;18:364–368. doi: 10.1037//0278-6133.18.4.364. [DOI] [PubMed] [Google Scholar]
- Brownell KD. The LEARN program for weight management. tenth edition American Health Publishing Company; Dallas, TX: 2004. [Google Scholar]
- Carels RA, Darby LA, Rydin S, Douglass OM, Cacciapaglia HM, O’Brien WH. The relationship between self-monitoring, outcome expectations, difficulties with eating and exercise, and physical activity and weight loss treatment outcomes. Ann. Behav. Med. 2005;30:182–190. doi: 10.1207/s15324796abm3003_2. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicidal ideation, and suicide attempts: results from a general population survey. Am. J. Public Health. 2000;90:251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran W. Sampling techniques. Wiley; New York: 1977. [Google Scholar]
- Cooper Z, Fairburn CG, Hawker DM. Cognitive-behavioral treatment of obesity: a clinician’s guide. The Guilford Press; New York: 2003. [Google Scholar]
- Diez-Quevado C, Rangin T, Sanchez-Planell L, Kroenke K, Spitzer R. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom. Med. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: Current status. Health Psychol. 2000;19(Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, Williams J. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitsky DA, Garay J, Nausbaum M, Neighbors L, DellaValle DM. Monitoring weight daily blocks the freshman weight gain: A model for combating the epidemic of obesity. Int. J. Obesity. 2006;30:1003–1010. doi: 10.1038/sj.ijo.0803221. [DOI] [PubMed] [Google Scholar]
- Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30:210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Hill JO. Behavioral strategies of individuals who have maintained long-term weight losses. Obes. Res. 1999;7:334–341. doi: 10.1002/j.1550-8528.1999.tb00416.x. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Seagle HM, Hill JO. Long-term maintenance of weight loss: Do people who lose weight through various weight loss methods use different behaviors to maintain their weight? Int. J. Obesity. 1998;22:572–577. doi: 10.1038/sj.ijo.0800627. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United Statues, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ogden J, Evans C. The problem with weighing: Effects on mood, self-esteem and body image. Int. J. Obesity. 1996;20:272–277. [PubMed] [Google Scholar]
- Ogden J, Whyman C. The effect of repeated weighing on psychological state. Eur. Eat. Disord. Rev. 1997;5:121–130. [Google Scholar]
- Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am. J. Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, Patti ET, McCann KL. Effect of length of treatment on weight loss. J. Consult. Clin. Psychol. 1989;57:450–452. [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Barlow W, Pabiniak C, Wagner E. Predictors of chronic benzodiadepine use in a health maintenance organization sample. J. Clin. Epidemiol. 1996;49:1067–1073. doi: 10.1016/0895-4356(96)00139-4. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch. Gen. Psychiat. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Taplin S, Thompson R, Schintzer F, Anderman C, Immanuel V. Revisions in the risk-based Breast Cancer Screening Program at Group Health Cooperative. Cancer. 1990;66:812–818. doi: 10.1002/1097-0142(19900815)66:4<812::aid-cncr2820660436>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Wadden T, Letizia K. Predictors of attrition and weight loss in patients treated by moderate and severe caloric restriction. In: Wadden T, Vanitallie T, editors. Treatment of the Seriously Obese Patient. Guilford; New York, Guilford: 1992. pp. 383–410. [Google Scholar]
- Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bouchard C, James WPT, editors. Handbook of Obesity. Marcel Dekker; New York: 1998. pp. 855–878. [Google Scholar]


