Abstract
The restriction of the resident physician work week to 80 hours has had dramatic affects on resident education and life-style. While effects on mood, psychological distress, and burn-out have been studied, the resultant changes in tangible quality of life have received little attention. birth rate was considered a measurable, relevant outcome. The resident marital and parental status by duty month was collected from a single orthopaedic surgical residency program for the four academic years preceding and following the implementation of the 80-hour work week. the number of births to residents during these periods were also tallied. The relative prevalence of positive marital status changed very little between residents in the two time durations from 66 to 71 percent, but parental status increased from 27 to 43 percent. The number of births per married resident duty year also increased from 0.23 pre-restrictions to 0.32 post-restrictions. While the individual decisions involved in generating these observed changes are complex and difficult to entirely decipher, it is thought that an increased perception of life-control within the work-hour restrictions may have prompted the dramatic changes in birth rate among resident families.
INTRODUCTION
The restriction of the resident physician work week to no more than 80 hours, mandated by the Accreditation Council of Graduate Medical Education (ACGME) beginning in July 2003, was expected to dramatically affect a number of aspects of resident education. However, some of the anticipated benefits and detriments of the policy enforcement have not been clearly demonstrable.1-4 Dramatic effects on resident physician life-style were also anticipated from the corollary mandate for at least 88 hours of non-hospital time. These effects have yet received minimal attention in the literature.
The impetus behind the ACGME restrictions was the desire to protect patients from the medical errors that can result from sleep-deprived physician decision-making. It remains to be proven whether or not work-hours restrictions have accomplished this noble goal of decreased fatigue-related medical error.2,4
Some of the anticipated side-effects of work-hour restrictions related to resident quality of life. It was also conjectured that work-hours restrictions during training may change the specialty and subspecialty choices made by graduating medical students;4,5 that perhaps the brutal rigor of the training programs of certain surgical disciplines may have previously deterred some candidates who will no longer avoid these specialties now that training work-hours are controlled.
Quality of life is an extremely difficult entity to measure among residents in training. One of the major challenges is the potential confounding force of a change in the complement of residency programs. If truly different people are filling the positions, they will naturally have different behaviors and different attitudes toward what an 80-hour work week means in terms of time for family, hobbies, recreation, etc.
For this pilot study, we hypothesized that the number of births per month per married resident has increased since the implementation of work-hours restrictions. While the actual time necessary to conceive a child is minimal in comparison to an 80-hour or even 120-hour work week, the decision to do so usually follows a perception that successful family life is possible within the confines of the married couple's current schedule constraints.
METHODS
The residency records of the Department of Orthopaedics and Rehabilitation at the University of Iowa were reviewed, along with personal memory, to identify the marital status of every resident in the first four years post-work-hours-restriction, spanning from July 2003 through June 2007, and the last four years pre-work-hours-restrictions, spanning from July 1999 through June 2003. Common-law and formal marriages were not distinguished. Residents who spent less than a full five years in the program were included, as all numbers ultimately included the denominator of residency duty months. First through fifth post-graduate years were included.
Children born were counted for birth occurring during the pre- and post- time periods noted above. Births were anticipated for the final 5 months of the post- time period, under the assumption that pregnancies far enough along to permit birth in the next 5 months are already publicly recognized in the small and friendly community of residents. Only children born to known resident families were included. No attempt was made to measure or estimate actual conception events as these are necessarily private. Specifically, no data regarding children conceived out of wed-lock (formal or functional) were collected. Data regarding pregnancies ending in miscarriage or abortion were also not collected. Number of children born was felt to be a maximally concrete variable to measure. Children born immediately before or after the periods in question were not counted. Children born immediately before or after a resident's months of resident duty in the Department were also not counted.
RESULTS
Twenty-four births to resident families occurred in the four years following ACGME restriction of resident work hours (Figure 1). Fifteen births occurred in the four years preceding these work hour restrictions (Figure 1). The denominator for these births changed, however, as the number of residents per class increased in the years following work hour restriction implementation. A total of 1188 months of resident duty were served during the four years preceding work hours restriction and 1260 months following. The number of births per year of resident duty increased from 0.15 to 0.22. Otherwise stated, there were 79 months of resident duty per birth prior to work hours restrictions and 53 months of duty per birth afterward.
Figure 1.
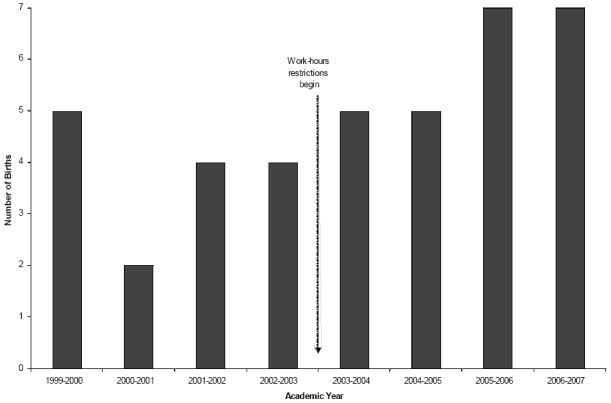
The number of births to orthopaedic surgical resident families during the four years preceding and following the implementation of the 80-hour work week.
More residents in the four years post-restrictions were married, with 892 married resident duty months following restrictions versus 781 married resident duty months in the four years pre-restrictions. The number of births per year of resident duty while married also increased from 0.23 to 0.32. This is a 40 percent increase in birth rate among married residents following the ACGME mandate. This correlates with 52 months of married resident duty per birth pre-restrictions and 37 months post-restrictions.
Residents did not appear to have children earlier or later in residency before or after the ACGME restrictions were mandated, averaging 2.73 and 2.79 years into residency at the time of birth pre- and post-restrictions, respectively (Figure 2). However, between the increased birth rate and the increased number of post-restriction residents with children born prior to the beginning of residency, the prevalence of positive parental status underwent a 60 percent increase after work-hours restrictions were mandated (Figure 3).
Figure 2.
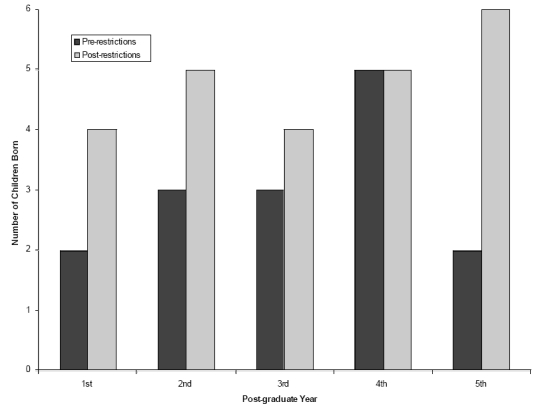
The distribution of the post-graduate-years status of the resident parents of the children born was fairly even between the pre- and post-restriction years. This argues against a more dramatic effect of the 80-hour work week on the earlier years of residency, with regard to birth rate.
Figure 3.
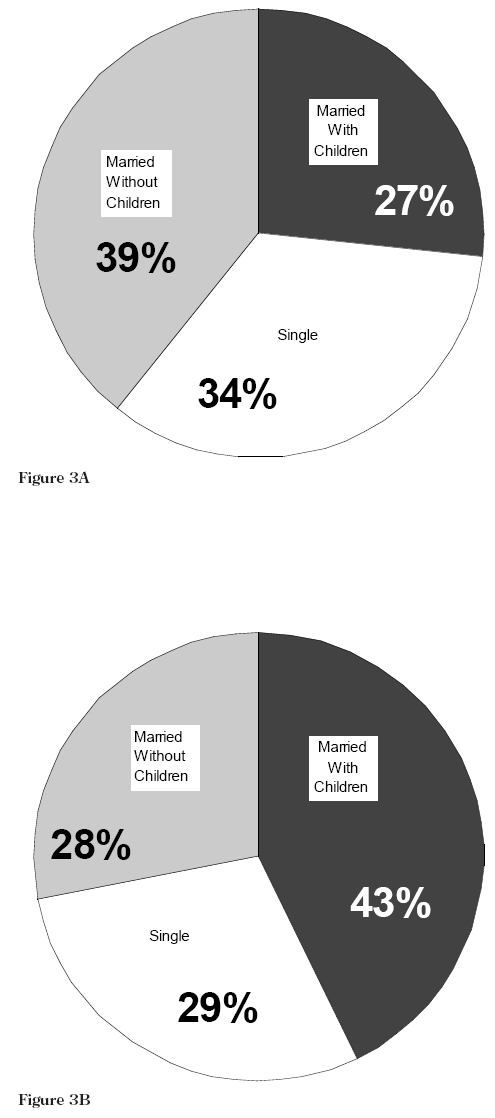
These pie charts demonstrate the relative prevalence (in duty months) of single residents (white wedges), married residents without children (gray wedges), and married residents with children (black wedges) both before (A) and after (B) the implementation of ACGME work-hours restrictions.
No resident underwent divorce during either time period studied. Two resident weddings occurred during the four pre-restriction years and five during the post-restriction years.
DISCUSSION
We report a 40 percent increase in births per married resident per year and a 60 percent increase in the relative prevalence of married residents with children associated with implementation of the ACGME mandate that the resident physician work week be restricted to no more than 80 hours of in-hospital duty. It is possible that this is simply due to sampling error. This study only involves four years prior to and following work hours restrictions. It only includes one residency program. Nonetheless, as a pilot study it is at least provocative that the difference may be real. A number of factors may have contributed to such an increase.
One explanation is that the 80-hour work week has changed the personal attributes of residents in the program. The central challenge to this interpretation is that most of the births in the four years following work hours restriction were to residents recruited prior to the work week limitations. Further, there has been no hard data to suggest that medical students are choosing specialties and programs differently since the implementation of the limited work week, although it has been widely suspected.4–6 The only hard evidence available is that voluntary attrition due to life-style concerns in general surgery programs seems not to have decreased.7 In our own recruitment process, some applicants have voiced that the limited work week prompted their consideration of a career in orthopaedic surgery, but no candidates vocal in this sentiment have joined our ranks.
Another interpretation is simply that residents have more time for personal pursuits, be they hunting, culinary arts, weight-lifting, or child-rearing. The difficulty with this interpretation standing alone is that 88 hours away from the hospital each week are still largely spent in educationally-related activities or sleep, and are sparse when considered against the time requirements for successful child-rearing. The previously well-quantified perception that residency is difficult for spouses and children of residents8 has not changed qualitatively. Certainly, spouses of residents in this residency program still regularly discuss their challenging schedule situation when together for group activities (Figure 4).
Figure 4.

This photo from an “Oortho Playgroup” outing to the fire station demonstrates the persistent absence of resident physicians in some of the most important departmental educational activities, even after implementation of the 80-hour work week.
Third, residents may have an improved sense of health and well-being with the work-hour restrictions, which may promote the decision to procreate. Studies have demonstrated improved mood and reduced psychological distress among surgical residents accompanying implementation of the 80-hour work week.9–11 One contrary study noted no change in resident burn-out, specifically, however.12 If such a change in mood and well-being were appreciable in our program, it might explain the large changes in birth rate. In the infertility literature, a study previously demonstrated that “cognitive weariness” associated strongly with male infertility, as did construction related careers to a lesser extent.13 While orthopaedics has been likened to carpentry previously, the 80-hour work week has only likely affected the weariness factor from this study. It is certainly possible that increased fertility from decreased weariness among residents is partly responsible for the increased birth rate. It is not known how many sought infertility counseling or treatment prior to or following the 80-hour restrictions mandate.
Finally, the increased rate of births may be due to an increased sense of control in resident life. Residents remain very busy with clinical and education responsibilities. Resident families continue to fend for themselves without the presence of the resident for most waking hours of the week. However, the 80-hour work week has prompted vast changes in the programs for call and clinical service coverage, most of which have dramatically increased the residents' sense of how predictable and manageable the schedule for the typical week can be. This sense of control, even if it is control over a still too-busy schedule, must promote the settled feelings that can engender thoughts of offspring.
While this pilot study has many limitations, it highlights the possibility that implementation of the 80-hour work has improved residents' ability to pursue non-career related life goals. Hopefully, this has been mated to an increase in resident quality of life and overall academic and professional performance.
Footnotes
Study performed in the Department of Orthopaedics and Rehabilitation, University of Iowa Hospitals and Clinics, Iowa City, Iowa, U.S.A.
References
- 1.Biller CK, Antonacci AC, Pelletier S, Homel P, Spann C, Cunningham MJ, Eavey RD. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006;135(2):275–81. doi: 10.1016/j.jss.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 2.de Virgilio C, Yaghoubian A, Lewis RJ, Stabile BE, Putnam BA. The 80-hour resident workweek does not adversely affect patient outcomes or resident education. Curr Surg. 2006;63(6):435–9. doi: 10.1016/j.cursur.2006.03.006. discussion 440. [DOI] [PubMed] [Google Scholar]
- 3.Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243(6):864–71. doi: 10.1097/01.sla.0000220042.48310.66. discussion 871-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schenarts PJ, Anderson Schenarts KD, Rotondo MF. Myths and realities of the 80-hour work week. Curr Surg. 2006;63(4):269–74. doi: 10.1016/j.cursur.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Smith RW. Resident recruiting and the 80-hour week. Fam Med. 2005;37(1):9. [PubMed] [Google Scholar]
- 6.Chandra RK. The resident 80-hour work week: how has it affected surgical specialties? Laryngo scope. 2004;114(8):1394–8. doi: 10.1097/00005537-200408000-00014. discussion 1319. [DOI] [PubMed] [Google Scholar]
- 7.Leibrandt TJ, Pezzi CM, Fassler SA, Reilly EF, Morris JB. Has the 80-hour work week had an impact on voluntary attrition in general surgery residency programs? J Am Coll Surg. 2006;202(2):340–4. doi: 10.1016/j.jamcollsurg.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 8.Strunk CL, et al. Resident work hours and working environment in otolaryngology. Analysis of daily activity and resident perception. Jama. 1991;266(10):1371–4. [PubMed] [Google Scholar]
- 9.Kiernan M, Civetta J, Bartus C, Walsh S. 24 hours on-call and acute fatigue no longer worsen resident mood under the 80-hour work week regulations. Curr Surg. 2006;63(3):237–41. doi: 10.1016/j.cursur.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Zare SM, et al. Psychological well-being of surgery residents before the 80-hour work week: a multiinstitutional study. J Am Coll Surg. 2004;198(4):633–40. doi: 10.1016/j.jamcollsurg.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Zare SM, Galanko JA, Behrns KE, Sieff EM, Boyle LM, Farley DR, Evans SR, Meyer AA, Farrell TM. Psychologic well-being of surgery residents after inception of the 80-hour workweek: a multi-institutional study. Surgery. 2005;138(2):150–7. doi: 10.1016/j.surg.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Gelfand DV, Podnos YD, Carmichael JC, Saltzman DJ, Wilson SE, Williams RA. Effect of the 80-hour workweek on resident burnout. Arch Surg. 2004;139(9):933–8. doi: 10.1001/archsurg.139.9.933. discussion 938-40. [DOI] [PubMed] [Google Scholar]
- 13.Sheiner EK, Carel R, Potashnik G, Sshoham-Vardi I. Potential association between male infertility and occupational psychological stress. J Occup Environ Med. 2002;44(12):1093–9. doi: 10.1097/00043764-200212000-00001. [DOI] [PubMed] [Google Scholar]


