Abstract
A 46 year old male developed spontaneous acute carpal tunnel syndrome of the right wrist without any antecedent trauma. Surgical exploration revealed hemorrhage secondary to diffuse giant cell tumor of tendon sheath as the underlying cause.
INTRODUCTION
Acute carpal tunnel syndrome is a rare entity, most commonly resulting from trauma to the upper extremity. Spontaneous acute onset of symptoms has been reported in patients with hemophilia, a history of anticoagulation therapy, or other bleeding diathesis. Acute carpal tunnel syndrome due to diffuse giant cell tumor of tendon sheath (GCTTS) arising from the flexor tendons has not been reported previously in the literature, though there is one previous account of acute carpal tunnel syndrome secondary to hemorrhage from pigmented villonodular synovitis (PVNS) involving the intercarpal joints.1
CASE REPORT
A 46 year old right hand dominant male presented to the emergency room with a one hour history of severe right hand and wrist pain. The patient had been eating lunch with his wife when he experienced the sudden onset of severe pain in his wrist. He denied any trauma to the wrist or hand. Over the next hour, he also developed paresthesias in a median nerve distribution in his hand. His pain was not relieved by ice, elevation, or 15 mg of morphine administered in the emergency room.
Of note, the patient had experienced similar symptoms, though less severe, six months prior to his presentation to the emergency room for this episode. At that time, he had moderate wrist pain with mild paresthesias, again without any associated trauma. He was evaluated by his primary care physician, who recommended ice, elevation, and anti-inflammatory medication. The patient's symptoms resolved over the next few days, though he noted that extensive ecchymosis developed several days after the onset of symptoms.
He had a history of known right scaphoid nonunion dating back to junior high school (Figure 1). He had no history of bleeding disorder or anticoagulation therapy, and was not taking any medications at the time of presentation.
Figure 1.


(A) AP and (B) scaphoid views of the wrist show chronic scaphoid nonunion.
On physical exam, he had firm swelling in the area of the wrist and proximal palm. There was no ecchymosis or skin lesion. He had 5 mm two point discrimination in his ring and small fingers, with greater than 10 mm two point discrimination in his thumb, index, and long fingers. He was able to flex and extend all digits, including his thumb. He had a normal radial pulse.
An MRI was obtained to evaluate for a space occupying lesion in the wrist. The MRI revealed heterogeneous fluid surrounding the flexor tendons with associated fluid-fluid levels consistent with hemorrhage (Figure 2). At this point, the patient's symptoms had not improved despite strict elevation, and open carpal tunnel release and flexor tenosynovectomy was performed.
Figure 2.
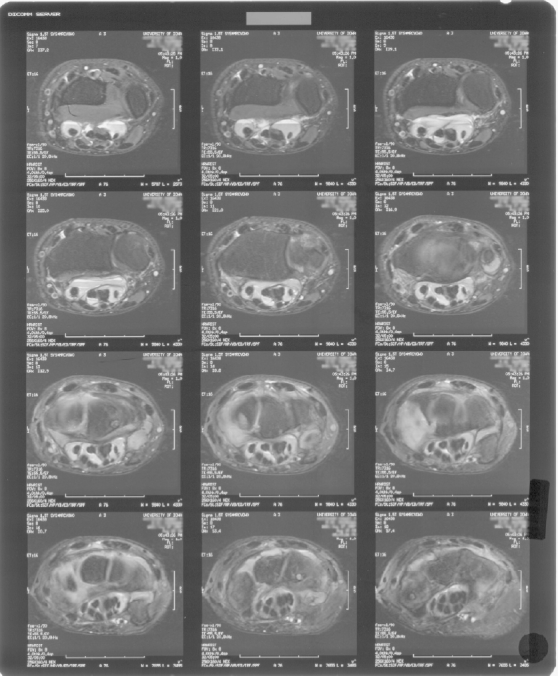
Axial T2-weighted MRI just proximal to the carpal tunnel reveals fluid-fluid levels consistent with hemorrhage. Axial T2-weighted MRI of the carpal tunnel at the level of the tunnel itself reveals a heterogeneous mass surrounding the flexor tendons.
An approximately 10 cm volar longitudinal incision was made along the FCR tendon sheath that extended past the distal palmar crease. Dissection was taken down to the transverse carpal ligament, which was released under direct vision. An infiltrative soft tissue hemorrhagic mass was identified and excised. The mass had encompassed all of the flexor tendons as well as the median nerve. The mass was fusiform in shape, approximately 12cm long and 3 cm wide, and appeared to arise from the flexor tendon sheaths themselves and not the carpal bones. The mass was carefully dissected free from the underlying tissues and a flexor tenosynovectomy was performed. The wound was closed over a drain which was removed on the first postoperative day.
Pathologic examination of the specimen revealed fibroadipose tissue with a synovial lining containing abundant hemosiderin deposition. The specimen's appearance was consistent with diffuse giant cell tumor of tendon sheath, as it contained numerous synovial clefts and relatively few giant cells (Figure 3).
Figure 3.
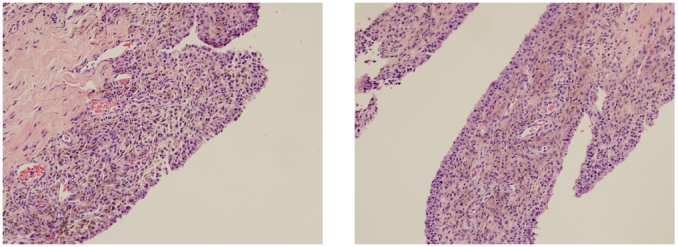
(A) and (B) Low-power photomicrographs show multiple synovial lined clefts and hemosiderin deposits in the subsynovial layer consistent with diffuse GCTTS. Giant cells are more scarce in diffuse GCTTS than localized GCTTS (Hematoxylin-eosin stain).
The patient had immediate pain relief following surgery and required only acetaminophen for analgesia during the postoperative period. Two weeks following surgery, his wound was well healed and he had 5 mm two point discrimination in all digits, except his long finger, which had 6 mm two point discrimination. Approximately six months after his surgery, the patient reported intermittent bouts of swelling and pain in his wrist, usually following activity. Each episode resolved with rest and over the counter anti-inflammatory medication, but these symptoms interfered with his daily activities.
A repeat MRI was performed which showed a small amount of heterogeneous material at the base of the carpal tunnel. A repeat flexor tenosynovectomy was performed through the previous incision. Some hemorrhagic tissue adherent to the flexor tendons was excised. Microscopic examination of this tissue revealed chronic synovitis with mild chronic inflammation. Two months following the repeat surgery, the patient reported resolution of his previous aching and swelling symptoms, though he continued to have slightly diminished sensation in his long finger.
DISCUSSION
Spontaneous onset of carpal tunnel syndrome without antecedent trauma is very unusual. Bauman et al previously reported five cases of acute carpal tunnel syndrome, all of which were associated with previous distal radius fracture or surgery.2 Spontaneous carpal tunnel syndrome has been reported in patients with hemophilia3 and von Willebrand's disease,4 patients on anticoagulation therapy,5,6 and as a result of a thrombosed persistent median artery.7 Chidgey published the only previously reported case of acute carpal tunnel syndrome as a result of pigmented villonodular synovitis. He described an 89 year old female who developed symptoms following aspiration of her wrist.1
PVNS and giant cell tumor of tendon sheath are the result of the same pathologic process and have similar histologic appearance. The term PVNS is reserved for intraarticular lesions, and is most commonly found in the knee and hip.11 Giant cell tumor of tendon sheath applies to extraarticular lesions, and can be localized (nodular) or diffuse. Localized giant cell tumor of tendon sheath is the second most common neoplasm identified in the hand, and 85% of cases occur in the digits.14,15 Localized GCTTS often presents as well circumscribed, firm, slow growing nodules in the hand. Diffuse GCTTS, also sometimes referred to as extraarticular PVNS, is much less common than the nodular form, and most commonly occurs around the knee.14 Complete surgical excision is the treatment of choice for both localized and diffuse GCTTS, though recurrence is common and occurs in 9-44% of cases.13 Though these lesions may be locally aggressive, they do not metastasize.15
Though localized GCTTS may be suspected from a characteristic clinical history and physical exam, diagnosis of diffuse GCTTS often requires more advanced imaging and biopsy. MRI can be helpful both for identification and surgical planning. MRI often shows hypertrophied synovium, sometimes with fatty infiltration due to the presence of lipid laden macrophages. Foci of low signal intensity on both T1 and T2 weighted images suggest the presence of hemosiderin.12 In our case, hemorrhage resulted in fluid-fluid levels within the tissue as well.
Regardless of etiology, early recognition and decompression is the key to successful treatment of acute carpal tunnel syndrome. Review of the literature reveals that patients who underwent surgery 12 or more hours after presentation were more likely to have residual neurologic deficits. Bauman described five cases of acute carpal tunnel syndrome in five patients following trauma or surgery. Surgical decompression was undertaken 36 to 96 hours following trauma in four patients when conservative measures failed to relieve symptoms. Only one patient recovered full median nerve function. Ford treated four patients with acute carpal tunnel syndrome following trauma. One patient underwent surgical release four hours after presentation and had full recovery.8 Of the remaining four patients who underwent decompression four to 96 hours after presentation, only one patient recovered normal median nerve function. The remaining patients suffered dysesthesias and diminished sensation.
Even patients with an atraumatic origin of their symptoms benefit from early decompression. Rahimtoola operated within 12 hours of admission in two cases of hemophiliacs with acute carpal tunnel syndrome and both patients experienced complete resolution of their neurologic deficit.3 Likewise, Chidgey performed carpal tunnel release within 24 hours of admission in the patient with PVNS of the wrist, and the patient had full recovery.1
References
- 1.Chidgey LK, Szabo RM, Wiese DA. Acute carpal tunnel syndrome caused by pigmented villonodular synovitis of the wrist. CORR. 1988;228:254–257. [PubMed] [Google Scholar]
- 2.Bauman TD, Gelberman RH, Mubarak SJ, Garfin SR. The acute carpal tunnel syndrome. CORR. 1981;156:151–156. [PubMed] [Google Scholar]
- 3.Rahimtoola ZO, van Baal SG. Two cases of acute carpal tunnel syndrome in classic hemophilia. Scand J Plast Reconstr Surg. 2002;36:186–188. doi: 10.1080/028443102753718104. [DOI] [PubMed] [Google Scholar]
- 4.Parthenis DG, Karagkevrekis CB, Waldram MA. Von Willebrand's disease presenting as acute carpal tunnel syndrome. J Hand Surg Br. 1998;23:114. doi: 10.1016/s0266-7681(98)80239-8. [DOI] [PubMed] [Google Scholar]
- 5.Black PR, Flowers MJ, Saleh M. Acute carpal tunnel syndrome as a complication of oral anticoagulation therapy. J Hand Surg Br. 1997;22:50–51. doi: 10.1016/s0266-7681(97)80015-0. [DOI] [PubMed] [Google Scholar]
- 6.Bonatz E, Seabol KE. Acute carpal tunnel syndrome in a patient taking Coumadin: case report. J Trauma. 1993;35:143–144. doi: 10.1097/00005373-199307000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Khashaba A. Carpal tunnel syndrome from thrombosed persistent median artery. J of Emergency Medicine. 2002;22:55–57. doi: 10.1016/s0736-4679(01)00436-x. [DOI] [PubMed] [Google Scholar]
- 8.Ford DJ, Ali MS. Acute carpal tunnel syndrome: complications of delayed decompression. JBJS Br. 1986;68B:758–759. doi: 10.1302/0301-620X.68B5.3782239. [DOI] [PubMed] [Google Scholar]
- 9.Patel MR, Zinberg EM. Pigmented villonodular synovitis of the wrist invading bone- report of a case. J Hand Surgery. 1984;9A:854–858. doi: 10.1016/s0363-5023(84)80066-0. [DOI] [PubMed] [Google Scholar]
- 10.Jamieson TW, Curran JJ, Desmet AA, Cotelingam JD, Kimmich H. Bilateral pigmented villonodular synovitis of the wrists. Orthop Rev. 1990;19:432–436. [PubMed] [Google Scholar]
- 11.Schwartz HS, Unni KK, Pritchard DJ. Pigmented villonodular synovitis: a retrospective review of affected large joints. Clin Orthop. 1989;247:243–255. [PubMed] [Google Scholar]
- 12.Hughes TH, Sartoris DJ, Schweitzer ME, Resnick DL. Pigmented villonodular synovitis: MRI characteristics. Skeletal Radiol. 1995;23:7–12. doi: 10.1007/BF02425937. [DOI] [PubMed] [Google Scholar]
- 13.Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheath. J Hand Surgery. 1999;24A:1298–1302. doi: 10.1053/jhsu.1999.1298. [DOI] [PubMed] [Google Scholar]
- 14.Kempson RL, Fletcher CDM, Evans HL, Hendrickson MR, Sibley RK. Atlas of Tumor Pathology; Tumors of the Soft Tissues. Washington DC: Armed Forces Institute of Pathology; 2001. pp. 388–393. [Google Scholar]
- 15.Fletcher CDM, Unni KK, Mertens F. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon, France: IARCPress; 2002. pp. 110–115. [Google Scholar]


