Abstract
Background
The purpose of this study was to determine the association between posttraumatic stress disorder (PTSD), diagnosed prospectively during pregnancy, and the risk of delivering a low birthweight (<2500 grams) or preterm (<37 weeks gestational age) infant.
Methods
Pregnant women were recruited from obstetrics clinics and screened for major and minor depressive disorder, panic disorder, PTSD, and substance use. Current episodes of PTSD were diagnosed according to the MINI International Neuropsychiatric Interview, and pregnancy outcomes were abstracted from hospital records.
Results
Among the 1100 women included in analysis, 31 (3%) were in episode for PTSD during pregnancy. Substance use in pregnancy, panic disorder, major and minor depressive disorder, and prior preterm delivery were significantly associated with a diagnosis of PTSD. Preterm delivery was non-significantly higher in pregnant women with (16.1%) compared to those without (7.0%) PTSD (OR= 2.82, 95% C.I. 0.95, 8.38). Low birthweight (LBW) was present in 6.5% of women and was not significantly associated with a diagnosis of PTSD in pregnancy after adjusting for potential confounders. However, LBW was significantly associated with minor depressive disorder (OR= 1.82, 95% C.I.1.01, 3.29).
Limitations
There was a low prevalence of PTSD in this cohort, resulting in limited power.
Conclusions
These data suggest a possible association between PTSD and preterm delivery. Coupled with the association found between LBW and a depressive disorder, these results support the utility of screening for mental health disorders in pregnancy.
Keywords: posttraumatic stress disorder, low birthweight, preterm delivery
Introduction
Preterm delivery and low birth weight are major public health problems. In the United States, 75% of babies who die in infancy are born preterm (MacDorman et al. 2005). For those who are preterm and survive, there is an increased risk of developmental, cognitive, and behavioral impairments later in life (Bhutta et al. 2002; Cooke & Foulder-Hughes 2003). Stress has been linked with preterm delivery in most (Pagel et al. 1990; Copper et al. 1996; Nordentoft et al. 1996; Rini et al. 1999; Dominguez et al. 2005), but not all (Chalmers 1983; Perkin et al. 1993; Peacock et al. 1995; Lobel et al. 2000) studies. The heterogeneity in findings may be a result of trying to determine the impact of minor levels of stress (Whitehead et al. 2002), but the lack of consistency in operationalizing “stress” has also contributed to differences in prior results. In contrast to broadly-defined “stress”, posttraumatic stress disorder (PTSD) is well-defined and constitutes one of the most severe stress-related illnesses. It has an estimated point prevalence of 8% (Loveland Cook et al. 2004). Despite the frequency and severity of this stress-related illness in pregnant women, there has been inadequate research regarding whether women with PTSD are at higher risk of delivering preterm or delivering a low birth weight baby (Seng et al. 2001; Berkowitz et al. 2003; Engel et al. 2005)
The purpose of this study was to determine whether PTSD, diagnosed prospectively during pregnancy, was associated with preterm delivery (<37 weeks gestational age). Given prior work suggesting that stress increases the risk of preterm delivery, it was hypothesized that women with PTSD would have a higher estimated risk of preterm delivery. Secondarily, we explored possible associations between PTSD and low birthweight (<2500 grams) since some work also suggest associations between this outcome and stress (Copper et al. 1996; Dominguez et al. 2005).
Methods
This project was a part of a larger prospective cohort study of birth outcomes among pregnant women enrolled in the Healthy Start Initiative in Connecticut. A 1,362-cohort of pregnant women was recruited by convenience sampling from prenatal clinics located in inner-city New Haven, Connecticut. Recruitment occurred over a two-year period. Screening occurred once at any point in pregnancy. Inclusion criteria included current pregnancy, ability to speak either English or Spanish, and enrollment at one of the included prenatal care clinics. Written and verbal informed consent was obtained from all women at the time of screening. Behavioral health care referrals were offered to symptomatic women. Immediate triage to a higher level of care was given to women who endorsed suicidal ideation.
A diagnosis of current PTSD was made using the MINI Neuropsychiatric Interview 5.0, a validated questionnaire that uses DSM-IV criteria to diagnose PTSD (Sheehan et al. 1998). This questionnaire was administered by trained Master’s and Bachelor’s level research staff. For a diagnosis of PTSD the subject was required to endorse having experienced an “unusually traumatic or stressful event”, respond “yes” to re-experiencing the event over the last month and respond “yes” to at least 3 of the following: avoidance, amnesia, decreased interest in activities, detachment, numbing, foreshortened future, and at least 2 of the following: trouble sleeping, irritability, difficulty concentrating, nervousness, and feeling easily startled for at least “several days”. Additionally, the subject had to indicate psychosocial distress as a result of these symptoms.
The Primary Care Evaluation of Mental Disorders (PRIME-MD) Brief Patient Health Questionnaire (BHQ) was used to detect probable major depressive, minor depressive and panic disorder. The BHQ is based on the DSM-IV diagnostic criteria, has acceptable performance in comparison to clinical assessment by mental health professionals (Spitzer et al. 1994; Spitzer et al. 1999), and has been used validated for use in obstetric and gynecologic settings (Spitzer et al. 2000).
Substance use during pregnancy, including alcohol, tobacco, and drug use, as well as age, primary language spoken, medical and pregnancy history, complications of the current pregnancy, and race and ethnicity were self-reported at the time of screening.
After delivery, researchers blind to psychiatric diagnoses systematically reviewed medical records to abstract the following data: birth weight and gestational age at delivery, complications of pregnancy or delivery, newborn medical problems, medical history, documented use of substances, and medications taken during pregnancy and used during delivery. For the purposes of this study, LBW was defined as less than 2500 grams, and preterm delivery was defined as delivery at less than 37 completed weeks of pregnancy. Gestational age was calculated from first trimester ultrasound, or when this was unavailable, from the date of the last menstrual period.
Of the 1,511 women approached, 1,339 (88.6%) agreed to participate in the study. Of these 1,339 participants, outcomes were available for 1,100 (82.2%). Medical records, and hence birth outcomes, were not available for 239 subjects because the participants delivered outside of New Haven, records could not be located, or the funding ended prior to medical record review. This left 1100 subjects available for analysis. A comparison of subjects who did or did not have medical records available revealed that women who with available medical records had significantly lower rates of substance abuse and less PTSD compared to women for whom records were unavailable. Otherwise, demographic factors and rates of comorbid disorders did not significantly vary between groups.
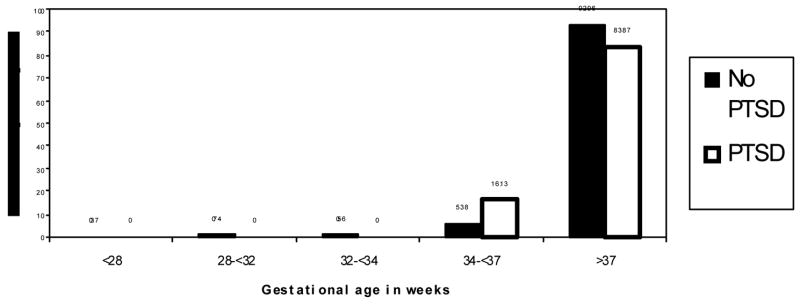
All analyses were performed using SAS 9.1. The Pearson Chi Square test and Student’s T-test were used to compare associations between PTSD and the potential confounders of race, language, tobacco, alcohol, and illicit drug use in pregnancy, maternal age, diagnosis of major and minor depression, the presence of panic disorder, and prior preterm delivery. Age, gestational age at delivery, and birth weight were left as continuous variables, while the remaining demographic variables, preterm delivery (less than 37 weeks), and low birthweight (less than 2500 grams) were dichotomized. T tests were used to compare the delivery weights and gestational ages at delivery between the PTSD and non-PTSD groups. Preterm delivery was recoded into the following smaller units 28 weeks, 28- less than 32 weeks, 32- less than 34 weeks, 34-less than 37 weeks, and greater than 37 weeks in order to plot the percent of women in each PTSD category delivering in each gestational age group. Logistic regression was used to estimate whether PTSD, as well as the potential confounders, contributed to models predicting preterm delivery or delivery of a low birth weight baby. Models were run separately for outcomes of LBW and preterm delivery. A backwards elimination method was then used to determine the most parsimonious models, keeping variables whose elimination changed the point estimate by 10% or more. A secondary analysis was performed that included women with subsyndromal PTSD, defined as having experienced a traumatic event with subjective impairment for at least 1 month and the following: at least 1 symptom of reexperiencing, and 2 symptoms of avoidance and 2 of hyperarousal or 3 of avoidance and 1 of hyperarousal(Stein et al. 1997). Finally, retrospective power calculations and the sample size needed to show statistical significance in a future study were completed using a chi-squared test for two proportions.
Results
Of the 1100 evaluable subjects, 31 (3%) met full diagnostic criteria for PTSD during pregnancy. As seen in Table 1 substance use, panic disorder, and major and minor depressive disorders occurred significantly more often among those with PTSD. However, the groups were demographically indistinguishable.
Table 1.
Description of Sample, by PTSD Status
| Characteristic | No PTSD (N=1079) | PTSD (N= 31) | p** |
|---|---|---|---|
| Age | 24.5 ± 5.8 | 24.3 ± 5.6 | 0.869 |
| Language | 0.868 | ||
| English | 667 (61.8) | 18 (58.1) | |
| Spanish | 409 (37.9) | 13 (41.9) | |
| Race/ethnicity | 0.991 | ||
| Non-Hispanic white | 140 (13.0) | 4 (12.9) | |
| Non-white | 939 (87.0) | 27 (87.1) | |
| Substance Use in Pregnancy | 0.008 | ||
| No | 799 (74.0) | 16 (51.6) | |
| Yes | 211 (19.6) | 13 (41.9) | |
| Panic Disorder | <0.001 | ||
| No | 1057 (98.0) | 22 (71.0) | |
| Yes | 22 (2.0) | 9 (29.0) | |
| Major Depressive Disorder | <0.001 | ||
| No | 1042 (96.6) | 24 (77.4) | |
| Yes | 37 (3.4) | 7 (22.6) | |
| Minor Depressive Disorder | <0.001 | ||
| No | 931 (86.3) | 20 (64.5) | |
| Yes | 148 (13.7) | 11 (35.5) |
Table values are mean ± sd for continuous variables and n (column %) for categorical variables. Numbers may not sum to 100% due to missing data and rounding
P-value is for t test (continuous variables) or chi square (categorical variables)
Table 2 illustrates the unadjusted associations between PTSD and LBW and preterm delivery. Preterm delivery occurred in 7.4% of the total population, and in 7.0% of those without and 16.1% of those with PTSD (p=0.055). Gestational age at delivery was an average of 0.5 weeks less in the PTSD group, which was not statistically significant. LBW occurred in 6.5% samples with and without PTSD. Birth weight was an average of 9.7 grams less in the PTSD population, which was not statistically significant.
Table 2.
Unadjusted Analysis: Pregnancy outcome, by PTSD status
| Outcome | No PTSD | PTSD | p value |
|---|---|---|---|
| Preterm Delivery (<37 weeks) | 0.055 | ||
| No | 1003 (93.0) | 26 (83.9) | |
| Yes | 76 (7.0) | 5 (16.1) | |
| Gestational Age at Delivery (weeks) | 39.1 ± 2.0 | 38.6 ± 1.8 | 0.266 |
| LBW (<2500g) | 0.994 | ||
| No | 1009 (93.5) | 29 (93.6) | |
| Yes | 70 (6.5) | 2 (6.5) | |
| Birth Weight (grams) | 3288.8 ± 539.0 | 3279.1 ± 519.5 | 0.921 |
Table values are mean ± sd for continuous variables and n (column%) for categorical variables Numbers may not sum to 100% due to missing data and rounding
P-value is for t test (continuous variables) or chi square (categorical variables)
The differences in gestational age at delivery between the PTSD and non-PTSD groups were most pronounced late in gestation. Figure 2 demonstrates the differences in gestational age by weeks according to PTSD status. The largest discrepancy between the PTSD and non-PTSD groups was in the 34–37 week interval: 16.1% (5/31) of those with and 5.4% (58/1100) of those without PTSD delivered between 34–37 weeks, differences which were not statistically significant.
Tables 3 and 4 show results of the adjusted models that estimate the association between PTSD and preterm delivery. Preterm delivery was nearly three-fold more likely in subjects with PTSD (OR=2.72, 95% C.I. 0.91, 8.14). The most parsimonious model (Table 4) included major and minor depression, substance use, and panic disorder.
Table 3.
Full model of logistic regression of PTSD on preterm delivery
| Variable | Odds Ratio | 95% confidence interval |
|---|---|---|
| PTSD | 2.72 | 0.91 to 8.14 |
| Older Age | 0.99 | 0.95 to 1.03 |
| Non-White Race | 0.89 | 0.41 to 1.92 |
| Spanish Language | 1.25 | 0.74 to 2.11 |
| Substance use in pregnancy | 0.93 | 0.50 to 1.74 |
| Major depression | 1.72 | 0.62 to 4.77 |
| Minor depression | 1.46 | 0.78 to 2.74 |
| Panic disorder | 0.57 | 0.12 to 2.76 |
Table 4.
Final model of logistic regression of PTSD on preterm delivery
| Variable | Odds Ratio | 95% confidence interval |
|---|---|---|
| PTSD | 2.82 | 0.95 to 8.38 |
| Substance use in pregnancy | 0.86 | 0.48 to 1.57 |
| Major depression | 1.63 | 0.59 to 4.49 |
| Minor depression | 1.43 | 0.76 to 2.66 |
| Panic disorder | 0.56 | 0.12 to 2.69 |
Low birthweight (LBW) was not significantly associated with a diagnosis of PTSD in pregnancy after adjusting for potential confounders of race, age, language spoken, depression, panic, and substance use in pregnancy. However, LBW was significantly associated with minor depressive disorder in both full and reduced models with a final OR= 1.82 (95% C.I. 1.01, 3.29).
The sample size calculation performed to determine the number of women needed in a hypothetical future study in order to demonstrate statistical significance using the rates of preterm delivery in the PTSD and non-PTSD groups found that at least 193 women would be needed in each exposure category. Acknowledging the limitations of retrospective power calculations, for the preterm delivery outcome, there was only 49% power to detect differences in this study. The secondary analysis including women with subsyndromal PTSD did not substantially alter the findings.
Discussion
In this longitudinal cohort study, women with PTSD were at greater risk of delivering preterm, although this comparison was different only at a trend level. The length in gestation showed the greatest variation in the interval between 34 and 37 weeks. This is consistent with suggestions in the literature that stress contributes to preterm deliveries that are closer to 37 weeks while other biomedical factors such as infection play a greater pathophysiological role in deliveries prior to 34 weeks (Wadhwa et al. 2001) (Hedegaard et al. 1993).
The relationship between minor depressive disorder and LBW is an important secondary finding in this study. The fact that the relationship between major depressive disorder and LBW was not significant may reflect limited power to detect significance in this relationship. It may also suggest an epi-phenomenon where an unmeasured mental health variable is associated with minor depressive disorder and PTSD, thus making it appear that the two are related. However, a relationship between depression and LBW has been noted in other studies (Reeb et al. 1987; Steer et al. 1992; Paarlberg et al. 1999).
While our cohort included only 31 women with PTSD, it is the largest study to prospectively evaluate birth outcomes in women who were systematically diagnosed with PTSD through the use of standard questionnaires. Investigators in an earlier study used ICD-9 codes to perform retrospective analysis from insurance forms to determine PTSD status and explore possible associations with a variety of birth outcomes (Seng et al. 2001). While PTSD was unrelated to preterm delivery, women with PTSD did have significantly increased odds of spontaneous abortion (OR=1.9, 95% C.I. 1.3, 2.9), preterm contractions (OR=1.4, 95% C.I. 1.1, 1.9), and ectopic pregnancy (OR=1.7, 95% C.I. 1.1, 2.8). It is worth noting that the use of insurance claims, rather than systematic assessment to define PTSD, may have missed cases of PTSD, resulting in misclassification bias. The low prevalence estimate of 0.4% found in this study suggests that women who carry a PTSD diagnosis were missed. Moreover, the methods used in that study precluded researchers from determining if the PTSD occurred before, during or after pregnancy, further weakening the investigators capacity to accurately estimate the association.
Two other reports, both derived from the same cohort, assessed whether PTSD symptoms conferred an increased risk of poor perinatal outcomes (Berkowitz et al. 2003; Engel et al. 2005). Women in this study resided in New York City at the time of the World Trade Center disaster of 2001. Researchers administered a PTSD symptoms checklist, to 187 pregnant women who lived or worked near the WTC, only 4 of whom had symptoms consistent with a diagnosis of PTSD (Berkowitz et al. 2003; Engel et al. 2005). As in the earlier study by Seng et al., the diagnosis of PTSD could have occurred before or after delivery.
Finally, in a small prospective pilot study of 25 women, 10 with PTSD, researchers found that number of PTSD symptoms was significantly negatively correlated (r=−0.725) with the Optimality Index-US, a combined measure of 52 dichotomous antenatal and postnatal events (Seng et al. 2005). Although the focus of this report was specifically preterm delivery, the study supports a higher general risk of birth complications among pregnant women with PTSD.
There is a theoretical pathophysiological mechanism for a connection between PTSD and preterm delivery. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous systems (Vermetten & Bremner 2002). Individuals with PTSD have elevations of central corticotrophin releasing hormone (CRH) consistent with a stress response (Bremner et al. 1997; Baker et al. 1999). Flashbacks and other symptoms of re-experiencing ensure that the stress system remains activated. Elevations in CRH can lead to higher levels of maternal adrenocorticotropin hormone (ACTH) and cortisol, which can elevate placental levels in a feed forward fashion (Mastorakos & Ilias 2003). Cortisol can cross into the fetal circulation and later in pregnancy, activate the fetal adrenal gland to increase production of estriol, a critical step in the sequence of events leading to delivery (Mastorakos & Ilias 2003).
PTSD also stimulates the sympathetic nervous system (Young & Breslau 2004; Maestripieri et al. 2005), resulting in tonically elevated levels of norepinephrine and epinephrine (Vermetten & Bremner 2002). Pregnant women with anxiety have been found to have increased uterine artery resistance (Teixeira et al. 1999), which is likely mediated by the sympathetic vasoconstriction (Teixeira et al. 1999) and is associated with fetal growth restriction and preeclampsia (Bower et al. 1993). Infection and inflammation may also link stress and early parturition. PTSD increases inflammatory cytokines (Maes et al. 1999), the effect of which may be to increase preterm delivery (Andrews et al. 1995; Osmers et al. 1995) through prostaglandin upregulation (Maymon et al. 2000). In addition to the direct pathophysiologic effects of PTSD, secondary effects including sleep disruptions and appetite suppression conspire to create a non-optimal maternal environment.
The limitations of this study include the inability to control for several variables of importance, including prior preterm delivery and weight gain in pregnancy, and the potential of residual confounding in the category of substance use in pregnancy. Additionally, the fact that the women who lacked birth outcome data had higher rates of PTSD and substance abuse than those with birth outcome data indicates that the sample may have been biased. However, this bias would only occur if attrition preferentially occurred in women who had both PTSD and preterm delivery. In this case, we would have underestimated the association between the two conditions.
This study indicates a need for more research into PTSD and pregnancy outcomes. Future studies should ideally investigate the effects of the timing of the traumatic event and PTSD on pregnancy outcomes, the possible contribution of trauma with and without PTSD on birth outcomes, and whether delivering a preterm or low birth weight baby in women with PTSD could be prevented by adequate treatment.
Conclusion
These data suggest that a possible association of PTSD and preterm delivery but the study was limited by the low rates of PTSD in this cohort and the inability to adequately control for several essential confounders. Taken together, these findings provide limited support for the hypothesized association between PTSD and preterm delivery. While these data do not support an association between PTSD and LBW, there is the suggestion that minor depressive disorder may be predictive of LBW.
Figure 1.
Plot of gestational age by PTSD status
Table 5.
Full model of logistic regression of PTSD on LBW
| Variable | Odds Ratio | 95% confidence interval |
|---|---|---|
| PTSD | 0.87 | 0.18 to 4.17 |
| Older Age | 0.96 | 0.91 to 1.1 |
| Non-White Race | 1.30 | 0.56 to 3.01 |
| Spanish Language | 0.75 | 0.42 to 1.34 |
| Substance use in pregnancy | 1.14 | 0.62 to 2.11 |
| Major depression | 1.25 | 0.36 to 4.30 |
| Minor depression | 1.91 | 1.02 to 3.56* |
| Panic disorder | 1.09 | 0.22 to 5.26 |
statistically significant at the p≤0.05 level
Table 6.
Final model of logistic regression of PTSD on LBW
| Variable | Odds Ratio | 95% confidence interval |
|---|---|---|
| PTSD | 0.83 | 0.19 to 3.66 |
| Major depression | 1.21 | 0.36 to 4.09 |
| Minor depression | 1.82 | 1.01 to 3.29* |
statistically significant at the p≤0.05 level
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andrews WW, Hauth JC, Goldenberg RL, Gomez R, Romero R, Cassell GH. Amniotic fluid interleukin-6: correlation with upper genital tract microbial colonization and gestational age in women delivered after spontaneous labor versus indicated delivery. Am J Obstet Gynecol. 1995;173(2):606–12. doi: 10.1016/0002-9378(95)90290-2. [DOI] [PubMed] [Google Scholar]
- Baker DG, West SA, Nicholson WE, Ekhator NN, Kasckow JW, Hill KK, Bruce AB, Orth DN, Geracioti TD., Jr Serial CSF corticotropin-releasing hormone levels and adrenocortical activity in combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1999;156(4):585–8. doi: 10.1176/ajp.156.4.585. [DOI] [PubMed] [Google Scholar]
- Berkowitz GS, Wolff MS, Janevic TM, Holzman IR, Yehuda R, Landrigan PJ. The World Trade Center disaster and intrauterine growth restriction. Jama. 2003;290(5):595–6. doi: 10.1001/jama.290.5.595-b. [DOI] [PubMed] [Google Scholar]
- Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. Jama. 2002;288(6):728–37. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- Bower S, Bewley S, Campbell S. Improved prediction of preeclampsia by two-stage screening of uterine arteries using the early diastolic notch and color Doppler imaging. Obstet Gynecol. 1993;82(1):78–83. [PubMed] [Google Scholar]
- Bremner JD, Licinio J, Darnell A, Krystal JH, Owens MJ, Southwick SM, Nemeroff CB, Charney DS. Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry. 1997;154(5):624–9. doi: 10.1176/ajp.154.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers B. Psychosocial factors and obstetric complications. Psychol Med. 1983;13(2):333–9. doi: 10.1017/s0033291700050959. [DOI] [PubMed] [Google Scholar]
- Cooke RW, Foulder-Hughes L. Growth impairment in the very preterm and cognitive and motor performance at 7 years. Arch Dis Child. 2003;88(6):482–7. doi: 10.1136/adc.88.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copper RL, Goldenberg RL, Das A, Elder N, Swain M, Norman G, Ramsey R, Cotroneo P, Collins BA, Johnson F, Jones P, Meier AM. The preterm prediction study: maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks’ gestation. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1996;175(5):1286–92. doi: 10.1016/s0002-9378(96)70042-x. [DOI] [PubMed] [Google Scholar]
- Dominguez TP, Schetter CD, Mancuso R, Rini CM, Hobel C. Stress in African American pregnancies: testing the roles of various stress concepts in prediction of birth outcomes. Ann Behav Med. 2005;29(1):12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- Engel SM, Berkowitz GS, Wolff MS, Yehuda R. Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Paediatr Perinat Epidemiol. 2005;19(5):334–41. doi: 10.1111/j.1365-3016.2005.00676.x. [DOI] [PubMed] [Google Scholar]
- Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. Psychological distress in pregnancy and preterm delivery. Bmj. 1993;307(6898):234–9. doi: 10.1136/bmj.307.6898.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobel M, DeVincent CJ, Kaminer A, Meyer BA. The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol. 2000;19(6):544–53. doi: 10.1037//0278-6133.19.6.544. [DOI] [PubMed] [Google Scholar]
- Loveland Cook CA, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet Gynecol. 2004;103(4):710–7. doi: 10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- MacDorman MF, Martin JA, Mathews TL, Hoyert DL, Ventura SJ. Explaining the 2001–02 Infant Mortality Increase: Data From the Linked Birth/Infant Death Data Set. National Vital Statistics Report 2005. 2005;53(12):1–23. [PubMed] [Google Scholar]
- Maes M, Lin AH, Delmeire L, Van Gastel A, Kenis G, De Jongh R, Bosmans E. Elevated serum interleukin-6 (IL-6) and IL-6 receptor concentrations in posttraumatic stress disorder following accidental man-made traumatic events. Biol Psychiatry. 1999;45(7):833–9. doi: 10.1016/s0006-3223(98)00131-0. [DOI] [PubMed] [Google Scholar]
- Maestripieri D, Lindell SG, Ayala A, Gold PW, Higley JD. Neurobiological characteristics of rhesus macaque abusive mothers and their relation to social and maternal behavior. Neurosci Biobehav Rev. 2005;29(1):51–7. doi: 10.1016/j.neubiorev.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Mastorakos G, Ilias I. Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartum. Ann N Y Acad Sci. 2003;997:136–49. doi: 10.1196/annals.1290.016. [DOI] [PubMed] [Google Scholar]
- Maymon E, Romero R, Pacora P, Gomez R, Athayde N, Edwin S, Yoon BH. Human neutrophil collagenase (matrix metalloproteinase 8) in parturition, premature rupture of the membranes, and intrauterine infection. Am J Obstet Gynecol. 2000;183(1):94–9. doi: 10.1067/mob.2000.105344. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Lou HC, Hansen D, Nim J, Pryds O, Rubin P, Hemmingsen R. Intrauterine growth retardation and premature delivery: the influence of maternal smoking and psychosocial factors. Am J Public Health. 1996;86(3):347–54. doi: 10.2105/ajph.86.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osmers RG, Blaser J, Kuhn W, Tschesche H. Interleukin-8 synthesis and the onset of labor. Obstet Gynecol. 1995;86(2):223–9. doi: 10.1016/0029-7844(95)93704-4. [DOI] [PubMed] [Google Scholar]
- Paarlberg KM, Vingerhoets AJ, Passchier J, Dekker GA, Heinen AG, van Geijn HP. Psychosocial predictors of low birthweight: a prospective study. Br J Obstet Gynaecol. 1999;106(8):834–41. doi: 10.1111/j.1471-0528.1999.tb08406.x. [DOI] [PubMed] [Google Scholar]
- Pagel MD, Smilkstein G, Regen H, Montano D. Psychosocial influences on new born outcomes: a controlled prospective study. Soc Sci Med. 1990;30(5):597–604. doi: 10.1016/0277-9536(90)90158-o. [DOI] [PubMed] [Google Scholar]
- Peacock JL, Bland JM, Anderson HR. Preterm delivery: effects of socioeconomic factors, psychological stress, smoking, alcohol, and caffeine. Bmj. 1995;311(7004):531–5. doi: 10.1136/bmj.311.7004.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkin MR, Bland JM, Peacock JL, Anderson HR. The effect of anxiety and depression during pregnancy on obstetric complications. Br J Obstet Gynaecol. 1993;100(7):629–34. doi: 10.1111/j.1471-0528.1993.tb14228.x. [DOI] [PubMed] [Google Scholar]
- Reeb KG, Graham AV, Zyzanski SJ, Kitson GC. Predicting low birthweight and complicated labor in urban black women: a biopsychosocial perspective. Soc Sci Med. 1987;25(12):1321–7. doi: 10.1016/0277-9536(87)90130-4. [DOI] [PubMed] [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999;18(4):333–45. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LK, Ben-Ami D, Liberzon I. Cortisol level and perinatal outcome in pregnant women with posttraumatic stress disorder: a pilot study. J Midwifery Womens Health. 2005;50(5):392–8. doi: 10.1016/j.jmwh.2005.04.024. [DOI] [PubMed] [Google Scholar]
- Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol. 2001;97(1):17–22. doi: 10.1016/s0029-7844(00)01097-8. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Jama. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183(3):759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. Jama. 1994;272(22):1749–56. [PubMed] [Google Scholar]
- Steer RA, Scholl TO, Hediger ML, Fischer RL. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093–9. doi: 10.1016/0895-4356(92)90149-h. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154(8):1114–9. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Teixeira JM, Fisk NM, Glover V. Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based study. Bmj. 1999;318(7177):153–7. doi: 10.1136/bmj.318.7177.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermetten E, Bremner JD. Circuits and systems in stress. I. Preclinical studies. Depress Anxiety. 2002;15(3):126–47. doi: 10.1002/da.10016. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Culhane JF, Rauh V, Barve SS, Hogan V, Sandman CA, Hobel CJ, Chicz-DeMet A, Dunkel-Schetter C, Garite TJ, Glynn L. Stress, infection and preterm birth: a biobehavioural perspective. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- Whitehead N, Hill HA, Brogan DJ, Blackmore-Prince C. Exploration of threshold analysis in the relation between stressful life events and preterm delivery. Am J Epidemiol. 2002;155(2):117–24. doi: 10.1093/aje/155.2.117. [DOI] [PubMed] [Google Scholar]
- Young EA, Breslau N. Cortisol and catecholamines in posttraumatic stress disorder: an epidemiologic community study. Arch Gen Psychiatry. 2004;61(4):394–401. doi: 10.1001/archpsyc.61.4.394. [DOI] [PubMed] [Google Scholar]