Abstract
Among 203 strains of Staphylococcus aureus, the MICs of CG400549 were 0.06 to 1.0 μg/ml, with MIC50 and MIC90 values of 0.25 μg/ml each. All strains were susceptible to linezolid and quinupristin-dalfopristin (MICs, 0.25 to 2.0 μg/ml). The daptomycin MICs were 0.25 to 2.0 μg/ml for methicillin-susceptible and 0.25 to 4.0 μg/ml against methicillin-resistant strains (including vancomycin-intermediate strains). Single-passage selection testing showed low resistance frequencies with CG400549, but multistep analysis showed that CG400549 yielded resistant mutants after 14 to 17 days in all strains tested.
Although in the past most Staphylococcus aureus infections have been nosocomial, the past few years have witnessed a worrisome emergence of community-acquired strains, many of which produce Panton-Valentine leukocidin (PVL) and cause serious and life-threatening infections (4, 11, 12, 14, 16, 17). Most community and nosocomial strains are methicillin-resistant S. aureus (MRSA) and quinolone-resistant, nosocomially acquired MRSA strains are often multiresistant (18).
Since the first description of vancomycin-intermediate Staphylococcus aureus (VISA) strains in Japan, these organisms have been reported all over the world (21). The recent lowering by the Clinical Laboratory Standards Institute (CLSI) of the vancomycin susceptibility breakpoint from ≤4.0 μg/ml to ≤2.0 μg/ml (10) will surely lead to a much wider appreciation of the clinical importance of these strains. In 2002, the first report of vancomycin-resistant S. aureus (VRSA) producing vanA occurred (3): to date, seven VRSA strains have been reported (8, 22; M. Rybak, personal communication).
It seems clear that the widespread use of vancomycin or teicoplanin in the community and hospital settings produces the selective pressure for VISA and VRSA strains: in most cases, prior glycopeptide use has been found in individual patients. The further spread of virulent community-acquired S. aureus strains (9, 14) will only exacerbate this problem. There is therefore a need for new antistaphylococcal agents with unique mechanisms of action.
The last step in fatty acid synthesis is performed by enoyl-acyl carrier protein (ACP) reductase (FabI), which is responsible for the reduction of the double bond in the enoyl-ACP derivative (1, 5). In S. aureus and Escherichia coli, this enzyme has been shown to be the antibacterial target of triclosan and diazaborines, thereby showing the essentiality of FabI in these organisms (17, 20). FabI is absent in some organisms, and an alternative enoyl-ACP reductase, FabK, is present in some pathogens, such as Streptococcus pneumoniae. Both FabI and FabK have been found in Enterococcus faecalis and Pseudomonas aeruginosa (19).
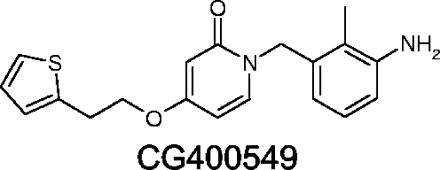
The current study investigates (i) the activity of CG400549, a new experimental FabI inhibitor (Fig. 1), in comparison with the activities of vancomycin, teicoplanin, linezolid, quinupristin-dalfopristin, daptomycin, amoxicillin-clavulanate, azithromycin, and levofloxacin against 203 S. aureus strains as determined by agar dilution MIC testing and (ii) the abilities of CG400549, vancomycin, linezolid, quinupristin-dalfopristin, and daptomycin to select for resistance in 10 strains by single- and multistep resistance selection techniques.
FIG. 1.
Structure of CG400549.
One hundred and three methicillin-susceptible Staphylococcus aureus (MSSA) and 100 MRSA strains were studied. Among MRSA strains, 54 were community-acquired and 47 of these produced PVL. The MRSA strains included five VISA strains (including a recently isolated VISA strain from a patient at Hershey Medical Center which developed the VISA phenotype while the patient was on vancomycin therapy) (15) and the first three VRSA strains described (from Michigan, Pennsylvania, and New York). The single- and multistep testing used 10 S. aureus strains of various phenotypes: two MSSA, four vancomycin-susceptible MRSA, two VISA, and two VRSA.
CG400549 susceptibility testing powder was obtained from Crystalgenomics, Inc., Seoul, Republic of Korea. Other antimicrobials were obtained from their respective manufacturers. Agar dilution testing was performed by the CLSI methodology, with added calcium for the daptomycin testing (10). The vancomycin MICs were read after a full 24-h incubation (10).
For the single-step resistance studies, two MSSA and eight MRSA (including two VRSA and two VISA) strains were tested as previously described (6). Because colonies obtained at these MICs often occurred on a background of confluent growth, retesting by the agar dilution MIC method was performed. To ensure the reproducibility and reliability of the results, resistance in the single-step studies was defined as a MIC more than four times greater than that against the parent.
In the multistep resistance selection tests, 10 S. aureus strains, including 8 MRSA (two VRSA and two VISA) and 2 MSSA strains, were examined. Serial passages were performed daily for each strain in subinhibitory concentrations of all antimicrobials. The methods were described previously (6). The identities of the mutants obtained and of their respective parents were confirmed at the end of the study by pulsed-field gel electrophoresis using a CHEF DR III apparatus (Bio-Rad, Hercules, CA) (2).
Among 203 methicillin-susceptible and -resistant strains of S. aureus, including strains with reduced susceptibility to vancomycin and teicoplanin, the MICs for CG400549 were all between 0.06 and 1.0 μg/ml, with MIC50 and MIC90 values of 0.25 μg/ml for each. All strains were susceptible to linezolid and quinupristin-dalfopristin (MICs between 0.25 and 2.0 μg/ml for both compounds). The daptomycin MICs ranged between 0.25 and 2.0 μg/ml for methicillin-susceptible and 0.25 and 4.0 μg/ml against methicillin-resistant strains. When vancomycin-nonsusceptible strains were excluded, the highest daptomycin MIC was 1.0 μg/ml. Methicillin-susceptible strains were amoxicillin-clavulanate susceptible, and resistance to levofloxacin and azithromycin was found (Table 1).
TABLE 1.
MICs of CG400549 compared with those of other agents against S. aureus
| Drug | MIC(s) (μg/ml) against:
|
|||||
|---|---|---|---|---|---|---|
| MSSA strains (n = 103)
|
MRSA strains (n = 100)
|
|||||
| Range | MIC50 | MIC90 | Range | MIC50 | MIC90 | |
| CG400459 | 0.06-1.0 | 0.25 | 0.25 | 00.06-1.0 | 0.25 | 0.25 |
| Vancomycin | 1.0-2.0 | 1.0 | 2.0 | 1.0->64.0 | 1.0 | 2.0 |
| Teicoplanin | 0.125-8.0 | 1.0 | 2.0 | 0.25->64.0 | 1.0 | 2.0 |
| Linezolid | 0.25-2.0 | 1.0 | 2.0 | 0.25-2.0 | 1.0 | 2.0 |
| Quinupristin-dalfopristin | 0.25-2.0 | 1.0 | 2.0 | 0.25-2.0 | 1.0 | 2.0 |
| Daptomycin | 0.25-2.0 | 1.0 | 1.0 | 0.25-4.0 | 0.5 | 0.5 |
| Amoxicillin-clavulanate | 0.125-4.0 | 1.0 | 2.0 | 0.5->64.0 | >64.0 | >64.0 |
| Levofloxacin | ≤0.06-32.0 | 0.25 | 4.0 | 0.125->32.0 | 1.0 | >32.0 |
| Azithromycin | 0.25->64.0 | 1.0 | >64.0 | 0.5->64.0 | >64.0 | >64.0 |
The results of single-step studies are presented in Table 2. The MICs (μg/ml) against the parental strains were as follows: for CG400549, 0.125 to 1; for vancomycin, 1 to >64; for linezolid, 0.5 to 2; for quinupristin-dalfopristin, 0.5 to 1; and for daptomycin, 0.5 to 8. The mutation frequencies with CG400549 ranged from 1.9 × 10−7 to <1.4 × 10−10 at 2× MIC to 1.5 × 10−8 to 8 × 10−10 at 8× MIC; the maximal CG400549 MIC for the recovered clones was 16 μg/ml. For vancomycin, the mutation frequencies at 2× and 8× MIC were 1.3 × 10−5 to <3.7 × 10−10 and 1.4 × 10−6 to <3.7 × 10−10, respectively. The linezolid mutation frequencies were 1.1 × 10−4 to <3.7 × 10−10 at 2× MIC and <1.3 × 10−10 to <3.7 × 10−10 at 8× MIC. The daptomycin mutation frequencies ranged from 1.2 × 10−6 to <2 × 10−10 at 2× MIC to <3.6 × 10−9 to <2.6 × 10−10 at 8× MIC. For quinupristin-dalfopristin, the mutation frequencies were in the range of 3.3 × 10−6 to 4.1 × 10−10 at 2× MIC and 1.1 × 10−10 to <3.3 × 10−10 at 8× MIC. Single-step mutants were verified by MIC (6).
TABLE 2.
Results of single-step resistance selection studies
| Strain; description | Drug | Mutation frequency at:
|
||
|---|---|---|---|---|
| 2× MIC | 4× MIC | 8× MIC | ||
| SA510; MRSA, VRSA | CG400549 | ∼6.8 × 10−9 | ∼3.4 × 10−9 | ∼6.8 × 10−9 |
| Vancomycin | NTa | NT | NT | |
| Linezolid | <3.3 × 10−10 | <3.3 × 10−10 | <3.3 × 10−10 | |
| Quinupristin-dalfopristin | ∼3.3 × 10−6 | ∼3.3 × 10−8 | <3.3 × 10−10 | |
| Daptomycin | ∼2.6 × 10−7 | <2.6 × 10−10 | <2.6 × 10−10 | |
| SA509; MRSA, VRSA | CG400549 | ∼3.0 × 10−7 | ∼1.5 × 10−8 | ∼1.5 × 10−8 |
| Vancomycin | NT | NT | NT | |
| Linezolid | <2.6 × 10−10 | <2.6 × 10−10 | <2.6 × 10−10 | |
| Quinupristin-dalfopristin | ∼3.9 × 10−9 | <2.6 × 10−10 | <2.6 × 10−10 | |
| Daptomycin | <1.7 × 10−10 | <1.7 × 10−10 | <1.7 × 10−10 | |
| SA555; MRSA, VISA | CG400549 | ∼2.0 × 10−9 | <1.0 × 10−10 | <1.0 × 10−10 |
| Vancomycin | <1.6 × 10−10 | <1.6 × 10−10 | <1.6 × 10−10 | |
| Linezolid | ∼4 × 10−6 | <2 × 10−10 | <2 × 10−10 | |
| Quinupristin-dalfopristin | <2 × 10−10 | <2 × 10−10 | <2 × 10−10 | |
| Daptomycin | <2 × 10−10 | <2 × 10−10 | <2 × 10−10 | |
| SA504; MRSA, VISA | CG400549 | <1.4 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 |
| Vancomycin | <3.7 × 10−10 | <3.7 × 10−10 | <3.7 × 10−10 | |
| Linezolid | <3.7 × 10−10 | <3.7 × 10−10 | <3.7 × 10−10 | |
| Quinupristin-dalfopristin | <1.6 × 10−10 | <1.6 × 10−10 | <1.6 × 10−10 | |
| Daptomycin | ∼4 × 10−6 | ∼2 × 10−8 | ∼3.6 × 10−9 | |
| SA481; MRSA | CG400549 | ∼3.0 × 10−9 | ∼3.0 × 10−9 | ∼8.0 × 10−10 |
| Vancomycin | <1.7 × 10−10 | <1.7 × 10−10 | <1.7 × 10−10 | |
| Linezolid | ∼1.7 × 10−6 | <1.7 × 10−10 | <1.7 × 10−10 | |
| Quinupristin-dalfopristin | <1.2 × 10−10 | <1.2 × 10−10 | <1.2 × 10−10 | |
| Daptomycin | <1.9 × 10−10 | ∼4.7 × 10−8 | ∼3.9 × 10−9 | |
| SA490; MRSA | CG400549 | ∼1.9 × 10−9 | ∼1.4 × 10−9 | <1.4 × 10−10 |
| Vancomycin | <1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| Linezolid | <1.4 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 | |
| Quinupristin-dalfopristin | ∼1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| Daptomycin | ∼7.6 × 10−8 | ∼2.6 × 10−8 | ∼6.4 × 10−9 | |
| SA525; MRSA | CG400549 | ∼5.3 × 10−8 | ∼7.3 × 10−9 | ∼2.3 × 10−9 |
| Vancomycin | <2.1 × 10−10 | ∼3.2 × 10−9 | <2.1 × 10−10 | |
| Linezolid | ∼1.1 × 10−4 | <2.1 × 10−10 | <2.1 × 10−10 | |
| Quinupristin-dalfopristin | ∼1.1 × 10−9 | <1.1 × 10−10 | <1.1 × 10−10 | |
| Daptomycin | ∼2.7 × 10−8 | <1.3 × 10−10 | <1.3 × 10−10 | |
| SA547; MRSA | CG400549 | ∼1.1 × 10−8 | ∼2.2 × 10−9 | ∼1.3 × 10−9 |
| Vancomycin | <1.7 × 10−10 | <1.7 × 10−10 | <1.7 × 10−10 | |
| Linezolid | ∼6.3 × 10−6 | <1.6 × 10−10 | <1.6 × 10−10 | |
| Quinupristin-dalfopristin | ∼4.1 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 | |
| Daptomycin | <1.9 × 10−10 | <1.9 × 10−10 | <1.9 × 10−10 | |
| SA540; MSSA | CG400549 | ∼1.9 × 10−7 | ∼2.5 × 10−9 | ∼1.3 × 10−9 |
| Vancomycin | <1.2 × 10−10 | <1.2 × 10−10 | <1.2 × 10−10 | |
| Linezolid | <1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| Quinupristin-dalfopristin | ∼1.2 × 10−10 | ∼2.4 × 10−10 | <1.2 × 10−10 | |
| Daptomycin | ∼1.2 × 10−6 | <1.2 × 10−10 | ∼4.9 × 10−9 | |
| SA543; MSSA | CG400549 | ∼2.2 × 10−7 | ∼1.2 × 10−8 | ∼5.2 × 10−9 |
| Vancomycin | ∼1.3 × 10−5 | ∼4.7 × 10−5 | ∼1.4 × 10−6 | |
| Linezolid | <1.4 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 | |
| Quinupristin-dalfopristin | <1.1 × 10−10 | <1.1 × 10−10 | <1.1 × 10−10 | |
| Daptomycin | <2 × 10−10 | <2 × 10−10 | <2 × 10−10 | |
NT, not tested.
The results of the multistep selection studies are presented in Table 3. The MIC (μg/ml) ranges for parent strains were as follows: for CG400549, 0.125 to 1; for vancomycin, 2 to >64; for linezolid, 1 to 4; for quinupristin-dalfopristin, 0.125 to 0.5; and for daptomycin, 1 to 16.
TABLE 3.
Results of multistep resistance selection studiesa
| Strain; description | Antibiotic | Initial MIC (μg/ml) | MIC (μg/ml) after resistance selection (no. of passages) | MIC after 10 antibiotic-free subcultures for:
|
||||
|---|---|---|---|---|---|---|---|---|
| CG400549 | Daptomycin | Linezolid | Quinupristin-dalfopristin | Vancomycin | ||||
| SA481; CAMRSA, PVL neg | CG400549 | 0.25 | 2 (14) | 2 | 1 | 4 | 0.25 | 2 |
| Daptomycin | 1 | 8 (14) | 0.25 | 8 | 4 | 0.25 | 4 | |
| Linezolid | 4 | 32 (37) | 0.125 | 1 | 32 | 0.5 | 2 | |
| Quinupristin-dalfopristin | 0.25 | 2 (16) | 0.25 | 1 | 4 | 2 | 2 | |
| Vancomycin | 2 | 8 (50) | NT | NT | NT | NT | NT | |
| SA490; CAMRSA, PVL pos | CG400549 | 0.25 | 8 (17) | 8 | 1 | 4 | 0.25 | 2 |
| Daptomycin | 1 | 8 (14) | 0.25 | 4 | 4 | 0.125 | 2 | |
| Linezolid | 4 | 32 (22) | 0.25 | 1 | 32 | 0.25 | 2 | |
| Quinupristin-dalfopristin | 0.25 | 4 (23) | 0.125 | 1 | 4 | 4 | 2 | |
| Vancomycin | 2 | 8 (50) | NT | NT | NT | NT | NT | |
| SA504; VISA | CG400549 | 0.25 | 2 (14) | 2 | 1b | 2 | 0.5 | 2b |
| Daptomycin | 4 | 16 (50) | NT | NT | NT | NT | NT | |
| Linezolid | 1 | 8 (22) | 0.25 | 1b | 8 | 0.5 | 8 | |
| Quinupristin-dalfopristin | 0.25 | 2 (16) | 0.5 | 2 | 2 | 2 | 2b | |
| Vancomycin | 8 | 8 (50) | NT | NT | NT | NT | NT | |
| SA509; VRSA, from Michigan | CG400549 | 1 | >64 (14) | >64 | 1 | 2 | 0.5 | 16b |
| Daptomycin | 1 | 8 (20) | 1 | 4 | 2 | 0.5 | 32b | |
| Linezolid | 2 | 16 (28) | 0.5 | 2 | 32 | 1 | >64 | |
| Quinupristin-dalfopristin | 0.5 | 4 (18) | 1 | 1 | 4 | 4 | 4b | |
| Vancomycin | >64 | NT | NT | NT | NT | NT | NT | |
| SA510; VRSA, from Hershey | CG400549 | 0.25 | 4 (14) | 4 | 1 | 2 | 0.25 | 16b |
| Daptomycin | 1 | 8 (18) | 0.125 | 4 | 4 | 0.25 | 2b | |
| Linezolid | 4 | 16 (50) | NT | NT | NT | NT | NT | |
| Quinupristin-dalfopristin | 0.25 | 4 (14) | 0.25 | 0.5 | 4 | 4 | 2b | |
| Vancomycin | 64 | NT | NT | NT | NT | NT | NT | |
| SA525; MRSA | CG400549 | 0.25 | 4 (14) | 4 | 1 | 4 | 0.25 | 1 |
| Daptomycin | 1 | 8 (20) | 0.125 | 2c | 4 | 0.25 | 2 | |
| Linezolid | 4 | 16 (50) | NT | NT | NT | NT | NT | |
| Quinupristin-dalfopristin | 0.25 | 2 (16) | 0.125 | 1 | 4 | 2 | 1 | |
| Vancomycin | 2 | 8 (50) | NT | NT | NT | NT | NT | |
| SA547; MRSA | CG400549 | 0.125 | 32 (14) | 8c | 1 | 4 | 0.25 | 2 |
| Daptomycin | 1 | 8 (21) | 0.125 | 4 | 4 | 0.25 | 4 | |
| Linezolid | 4 | 32 (48) | 0.125 | 2 | 32 | 0.5 | 2 | |
| Quinupristin-dalfopristin | 0.25 | 2 (21) | 0.125 | 1 | 4 | 2 | 2 | |
| Vancomycin | 2 | 8 (50) | NT | NT | NT | NT | NT | |
| SA555; VISA, from Hershey | CG400549 | 0.25 | 2 (14) | 2 | 8 | 2 | 0.06 | 8 |
| Daptomycin | 16 | 32 (50) | NT | NT | NT | NT | NT | |
| Linezolid | 2 | 4 (50) | NT | NT | NT | NT | NT | |
| Quinupristin-dalfopristin | 0.125 | 1 (20) | 0.25 | 2b | 4 | 0.5 | 2b | |
| Vancomycin | 8 | 8 (50) | NT | NT | NT | NT | NT | |
| SA540; MSSA | CG400549 | 0.125 | 16 (14) | 4c | 1 | 4 | 0.25 | 2 |
| Daptomycin | 1 | 8 (24) | 0.125 | 2c | 4 | 0.25 | 4 | |
| Linezolid | 4 | 32 (36) | 0.125 | 2 | 16 | 0.5 | 4 | |
| Quinupristin-dalfopristin | 0.25 | 2 (16) | 0.125 | 2 | 4 | 2 | 2 | |
| Vancomycin | 4 | 8 (50) | NT | NT | NT | NT | NT | |
| SA543; MSSA | CG400549 | 0.125 | 8 (14) | 8 | 1 | 4 | 0.25 | 1 |
| Daptomycin | 1 | 8 (17) | 0.125 | 4 | 4 | 0.25 | 2 | |
| Linezolid | 4 | 32 (15) | 0.125 | 2 | 32 | 0.25 | 2 | |
| Quinupristin-dalfopristin | 0.25 | 2 (18) | 0.125 | 2 | 4 | 2 | 4 | |
| Vancomycin | 2 | 8 (50) | NT | NT | NT | NT | NT | |
CAMRSA, community-acquired MRSA; NT, not tested. neg, negative; pos, positive.
MIC for mutant was ≥2 dilutions lower than MIC for parent.
MIC for mutant was 2 dilutions lower than its MIC after resistance selection was performed.
As can be seen, CG400549 selected for resistant mutants in all 10 strains after 14 to 17 days (parents, 0.125 to 1 μg/ml, and mutants, 2 to >64 μg/ml). By comparison, daptomycin selected mutants in 8 of the 10 strains after 14 to 24 days (parents, 1 μg/ml, and mutants, 8 μg/ml). Linezolid selected for resistant mutants in 7 of 10 strains after 15 to 48 days (parents, 1 to 4 μg/ml, and mutants, 8 to 32 μg/ml). Quinupristin-dalfopristin selected for resistant mutants in all 10 strains tested after 14 to 23 days (parents, 0.125 to 0.5 μg/ml, and mutants, 1 to 4 μg/ml). None of the eight vancomycin-susceptible and vancomycin-intermediate strains showed increased resistance to vancomycin even after 50 days of subculture. The two VRSA strains (MIC, ≥64 μg/ml) were not tested with vancomycin in single- or multistep studies. No cross-reactivity between drug groups was observed. Three mutants (one each with CG400549, linezolid, and quinupristin-dalfopristin) had daptomycin MICs that were two to three dilutions lower than those of the parent strains, and nine mutants (three with CG400549, two with daptomycin, and four with quinupristin-dalfopristin) had vancomycin MICs that were two to more than five dilutions lower than those of the parent strains (Table 3). Additionally, two CG400549 mutants and two daptomycin mutants had MICs that were two dilutions lower after 10 daily subcultures on antibiotic-free media than they had been before the subcultures (Table 3). All resistant clones were identical to their parent strains by pulsed-field analysis.
Previous studies have demonstrated elevated CG400549 MICs for FabI-overexpressing S. aureus strains; animal studies showed promising results, and the drug was safe at up to 1 g/kg of body weight of subcutaneous or oral use (C. Kim, J. Kwak, C. Lee, H. Park, S. Kang, J. Kim, Y. Song, S. Ro, T. Lee, and J. Cho, presented at the 45th Interscience Conference on Antimicrobial Agents and Chemotherapy, December 2005). The CG400549 MIC90 values were all 0.5 μg/ml against 1 VISA strain, 215 MRSA strains, and 41 coagulase-negative methicillin-resistant staphylococci (C. Kim, J. Kwak, Y. Kim, H. Yoon, H. Park, S. Ro, T. Lee, and J. Cho, presented at the 45th Interscience Conference on Antimicrobial Agents and Chemotherapy, December 2005). CG400549 was bactericidal at 8× MIC after 24 h, with a postantibiotic effect of 1 h against MRSA. The development of resistance to this drug in S. aureus was rare, with a frequency of 2.1 × 10−8 (C. Kim, Y. Kim, H. Yoon, J. Kim, S. Ro, T. Lee, and J. Cho, presented at the 45th Interscience Conference on Antimicrobial Agents and Chemotherapy, December 2005).
The results of single-step studies showed low frequencies of resistant mutants with CG400549, either comparable to or lower than those with other compounds tested, including against strains nonsusceptible to vancomycin. However, multistep resistance selection studies showed that in all 10 strains, CG400549 yielded resistant mutants with MICs of 2 to >64 μg/ml. The clinical significance of the low yield of resistant mutants by CG400549 in single-step testing compared with the high yield of resistant mutants by multistep testing remains to be elucidated.
Fourteen detected mutants selected by vancomycin or daptomycin showed unstable resistance phenotypes (Table 3). This phenomenon has been described in previous studies. Boyle-Vavra et al. described uniform decreases in the MICs of vancomycin and teicoplanin after 15 days of serial passage on nonselective medium; the presence of vancomycin in the medium prevented such reversion (7). Kaatz et al. reported that continuous exposure to daptomycin appears to be necessary to select stable mutants (13). Instability of vancomycin resistance has also been demonstrated in VRSA strains carrying the van(A) gene (22). The clinical significance of the single- and multistep findings obtained in our study for possible resistance selection in the potential future clinical use of CG400459 remains to be elucidated.
Experimental animal and pharmacokinetic/pharmacodynamic studies are necessary before the clinical usefulness of CG400549 in the treatment of staphylococcal infections can be investigated.
Acknowledgments
This study was supported by a grant from Crystalgenomics Inc., Seoul, Republic of Korea.
Footnotes
Published ahead of print on 17 September 2007.
REFERENCES
- 1.Baldock, C., J. B. Rafferty, S. E. Sedelnikova, P. J. Baker, A. R. Stuitje, A. R. Slabas, T. R. Hawkes, and D. W. Rice. 1996. A mechanism of drug action revealed by structural studies of enoyl reductase. Science 274:2107-2110. [DOI] [PubMed] [Google Scholar]
- 2.Bannerman, T. L., G. A. Hancock, F. C. Tenover, and J. M. Miller. 1995. Pulsed-field electrophoresis as a replacement for bacteriophage typing of Staphylococcus aureus. J. Clin. Microbiol. 33:551-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartley, J. 2002. First case of VRSA identified in Michigan. Infect. Control Hosp. Epidemiol. 23:480. [DOI] [PubMed] [Google Scholar]
- 4.Begier, E. M., K. Frenette, B. L. Barrett, P. Mshar, S. Petit, D. J. Boxrud, K. Watkins-Colwell, S. Wheeler, E. A. Cebelinski, A. Glennen, D. Nguyen, J. L. Hadler, and the Connecticut Bioterrorism Field Epidemiology Response Team. 2004. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin. Infect. Dis. 39:1446-1453. [DOI] [PubMed] [Google Scholar]
- 5.Bergler, H., S. Fuchsbichler, G. Högenauer, and F. Turnowsky. 1996. The enoyl-[acyl-carrier-protein] reductase (FabI) of Escherichia coli which catalyzes a key regulatory step in fatty acid biosynthesis, accepts NADH and NADPH as cofactors and is inhibited by palmitoyl-CoA. Eur. J. Biochem. 242:689-694. [DOI] [PubMed] [Google Scholar]
- 6.Bogdanovich, T., D. Esel, L. Kelly, B. Bozdogan, K. Credito, G. Lin, K. Smith, L. Ednie, D. Hoellman, and P. C. Appelbaum. 2005. Antistaphylococcal activity of DX-619, a new des-F(6)-quinolone, compared to those of other agents. Antimicrob. Agents Chemother. 49:3325-3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyle-Vavra, S., S. K. Berke, J. C. Lee, and R. S. Daum. 2000. Reversion of the glycopeptide resistance phenotype in Staphylococcus aureus clinical isolates. Antimicrob. Agents Chemother. 44:272-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 2004. Vancomycin-resistant Staphylococcus aureus—New York, 2004. Morb. Mortal. Wkly. Rep. 53:322-323. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. 1999. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997-1999. Morb. Mortal. Wkly. Rep. 48:707-710. [PubMed] [Google Scholar]
- 10.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 7th ed. Approved standard M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA.
- 11.Fergie, J. E., and K. Purcell. 2001. Community-acquired methicillin-resistant Staphylococcus aureus infections in south Texas children. Pediatr. Infect. Dis. J. 20:860-863. [DOI] [PubMed] [Google Scholar]
- 12.Heath, R. J., Y.-T. Yu, M. A. Shapiro, E. Olson, and C. O. Rock. 1998. Broad spectrum antimicrobial biocides target the FabI component of fatty acid synthesis. J. Biol. Chem. 273:30316-30320. [DOI] [PubMed] [Google Scholar]
- 13.Kaatz, G. W., T. S. Lundstrom, and S. M. Seo. 2006. Mechanisms of daptomycin resistance in Staphylococcus aureus. Int. J. Antimicrob. Agents 28:280-287. [DOI] [PubMed] [Google Scholar]
- 14.Kazakova, S. V., J. C. Hageman, M. Matava, A. Srinivasan, L. Phelan, B. Garfinkel, T. Boo, S. McAllister, J. Anderson, B. Jensen, D. Dodson, D. Lonsway, L. K. McDougal, M. Arduino, V. J. Fraser, G. Killgore, F. C. Tenover, S. Cody, and D. B. Jernigan. 2005. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N. Engl. J. Med. 352:468-475. [DOI] [PubMed] [Google Scholar]
- 15.Kosowska-Shick, K., M. Roos, H. Labischinski, C. Whitener, K. Julian, and P. C. Appelbaum. 2006. Abstr. 46th Intersci. Conf. Antimicrob. Agents Chemother., abstr. C1-685. [DOI] [PMC free article] [PubMed]
- 16.McDougal, L. K., C. D. Steward, G. E. Killgore, J. M. Chaitram, S. K. McAllister, and F. C. Tenover. 2003. Pulsed-field electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J. Clin. Microbiol. 41:5113-5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McMurry, L., M. Oethinger, and S. B. Levy. 1998. Triclosan targets lipid synthesis. Nature 394:531-532. [DOI] [PubMed] [Google Scholar]
- 18.Naimi, T. S., K. H. LeDell, K. Como-Sabetti, S. M. Borchardt, D. J. Boxrud, J. Etienne, S. K. Johnson, F. Vandenesch, S. Fridkin, C. O'Boyle, R. N. Danila, and R. Lynfield. 2003. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA 290:2976-2984. [DOI] [PubMed] [Google Scholar]
- 19.Payne, D. J., W. H. Miller, V. Berry, J. Brosky, W. J. Burgess, E. Chen, W. E. DeWolf, Jr., A. P. Fosberry, R. Greenwood, M. S. Head, D. A. Heerding, C. A. Janson, D. D. Jaworski, P. M. Keller, P. J. Manley, T. D. Moore, K. A. Newlander, S. Pearson, B. J. Polizzi, X. Qiu, S. F. Rittenhouse, C. Slater-Radosti, K. L. Salyers, M. A. Seefeld, M. G. Smyth, D. T. Takata, I. N. Uzinskas, K. Vaidya, N. G. Wallis, S. B. Winram, C. C. K. Yuan, and W. F. Huffman. 2002. Discovery of a novel and potent class of FabI-directed antibacterial agents. Antimicrob. Agents Chemother. 46:3118-3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slater-Radosti, C., G. Van Aller, R. Greenwood, R. O. Nicholas, P. Keller, W. E. DeWolf, F. Fan, D. J. Payne, and D. D. Jaworski. 2001. Biochemical and genetic characterisation of the action of triclosan on Staphylococcus aureus. J. Antimicrob. Chemother. 48:1-6. [DOI] [PubMed] [Google Scholar]
- 21.Tenover, F. C., M. V. Lancaster, B. C. Hill, C. D. Steward, S. A. Stocker, G. A. Hancock, C. M. O'Hara, N. C. Clark, and K. Hiramatsu. 1998. Characterization of staphylococci with reduced susceptibilities to vancomycin and other glycopeptides. J. Clin. Microbiol. 36:1020-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tenover, F. C., L. M. Weigel, P. C. Appelbaum, L. K. McDougal, J. Chaitram, S. McAllister, N. Clark, G. Killgore, C. M. O'Hara, L. Jevitt, J. B. Patel, and B. Bozdogan. 2004. Vancomycin-resistant Staphylococcus aureus isolate from a patient in Pennsylvania. Antimicrob. Agents Chemother. 48:275-280. [DOI] [PMC free article] [PubMed] [Google Scholar]