Abstract
Background
During the recovery period after acute ankle sprain, it is unclear whether conventional treatment should be supported by supervised exercise.
Aim
To evaluate the short- and long-term effectiveness of conventional treatment combined with supervised exercises compared with conventional treatment alone in patients with an acute ankle sprain.
Design
Randomised controlled clinical trial.
Setting
A total of 32 Dutch general practices and the hospital emergency department.
Method
Adults with an acute lateral ankle sprain consulting general practices or the hospital emergency department were allocated to either conventional treatment combined with supervised exercises or conventional treatment alone. Primary outcomes were subjective recovery (0–10 point scale) and the occurrence of a re-sprain. Measurements were carried out at intake, 4 weeks, 8 weeks, 3 months, and 1 year after injury. Data were analysed using intention-to-treat analyses.
Results
A total of 102 patients were enrolled and randomised to either conventional treatment alone or conventional treatment combined with supervised exercise. There was no significant difference between treatment groups concerning subjective recovery or occurrence of re-sprains after 3 months and 1-year of follow-up.
Conclusion
Conventional treatment combined with supervised exercises compared to conventional treatment alone during the first year after an acute lateral ankle sprain does not lead to differences in the occurrence of re-sprains or in subjective recovery.
Keywords: ankle, ankle injuries, conservative, physical therapy, randomised controlled trial, rehabilitation
INTRODUCTION
Ankle sprains are one of the most common musculoskeletal injuries. In the Netherlands an estimated 600 000 people sustain ankle injuries each year. Roughly half of these people visit GPs or, on their own initiative, emergency departments.1 In Dutch general practice there is an incidence of 12.8 ankle injuries per 1000 patients per year. Experimental studies of ligamentous healing indicate that gradually-increasing and functional load exercises stimulate healing and increase the strength of ligaments after injury.2–4 While injury to the ligaments may result in decreased mechanical stability of the ankle, neuromuscular deficits are also likely to occur as a result of injury to the nervous and musculo-tendinous tissue.5–7 This may also result in an unstable ankle, which can lead to re-injuries and a feeling of ‘giving way’. Balance training as part of rehabilitation may restrict the occurrence of functional instability and improve postural control after ankle sprains.8–10
Several reviews indicate that conventional treatment (early mobilisation, including mobilisation instructions and early weight bearing combined with or without the use of external support) is the preferred treatment strategy.11–16 External support used is tape, bandage, or a brace, but never a plaster cast. At present, this conventional treatment is known as usual care. Systematic reviews by Ogilvie-Harris and Gilbart,12 and Kerkhoffs et al15 report that there is no existing evidence for effectiveness of physiotherapy as a treatment strategy for acute ankle sprains. Even more precise is the conclusion of a systematic review by van Os et al17 which reports that there is limited evidence from randomised controlled trials that conventional treatment combined with supervised rehabilitation training may be superior to conventional treatment alone as a treatment for acute injuries of the lateral ligament complex of the ankle. It is unclear whether conventional treatment should be supplemented with supervised functional exercises to decrease the feeling of ‘giving way’ and, more importantly, to decrease re-sprains in the long-term. All three systematic reviews advise to conduct an randomised controled trial on this topic.12,15,17
How this fits in
Ankle injuries are a common problem in general practice. The incidence of ankle injuries in Dutch general practice is 12.8 per 1000 patients per year. Experimental studies of ligamentous healing indicate that gradually-increasing and functional load exercises stimulate healing and increase the strength of ligaments after injury. It is unclear whether conventional treatment should be supplemented with supervised functional exercises. This study shows that there is no strong indication that conventional treatment should be accompanied by supervised rehabilitation training.
The present prospective randomised study compared short- and long-term effects of conventional treatment alone with those of conventional treatment combined with supervised functional exercises in the treatment of an acute ankle sprain in adults.
METHOD
Patients
Patients who had an acute injury of the lateral collateral ligaments of the ankle and who presented to one of the 32 participating GPs or at the emergency department of the local hospital in the same district between March 2002 and December 2003 were asked for informed consent to participate in the trial. Patients with a lateral ankle sprain were eligible for the study if they were aged between 18 and 60 years and their first visit to the physician was within 1 week of injury. Patients were excluded if they had a history of an injury of the same ankle during the previous 2 years or if they had a fracture of the same ankle.
Study design
The GP or physician working in an accident and emergency department carried out a standardised clinical examination. Occurrence of swelling, haematoma, location of the sprain, and anterior drawer sign were reported. In addition, the physician estimated the severity of the injury. Categorising severity was based on clinical findings (stability, intensity, and location of swelling, pain, and haemorrhage), and graded according to three levels: grade I mild, grade II moderate, and grade III severe.18,19 If considered necessary based on the Ottawa ankle rules,20 radiological examination was performed to confirm the absence of bone injury.
After informed consent and after acquiring baseline information (questionnaire and clinical findings), each patient was randomised by a blinded and independent research assistant, making use of sealed envelopes which contained computer-generated randomisation cards, into either the conventional treatment group or the physical therapy group. Randomisation was stratified for setting (general practice versus emergency department) and severity of the injury (grade I and grade II versus grade III) with a block size of six.
Treatment
All participants in both groups received the same conventional treatment from their physician who was not aware of whether the patient undertook additional supervised exercises. Conventional treatment incorporated information about early ankle mobilisation, including advice for home exercises (for which patients received written instructions) and early weight bearing. Participants were encouraged to start these activities as early as possible, and to increase their activity level gradually. In general practice the ankle was protected by a tape or bandage if considered necessary by the physician, and in the emergency department the ankle was protected with a brace (Active Ankle Trainer, Louisville, US).
Patients in the physical therapy group participated in an individual and progressive training programme supervised by a physiotherapist, using a standardised protocol, which was based on guidance from the Royal Dutch Society of Physiotherapists21 (Supplementary Table 1). This programme existed of a maximum of nine half-hour sessions, within a period of 3 months, and included balance exercises, walking, running, and jumping.
Outcome assessment
The primary outcome measures were subjective recovery and occurrence of re-sprains at 3 months and 1 year of follow-up. Secondary outcome measures were patients appreciation of the received treatment, tested and reported instability and range of motion (ROM) of the ankle joint at 3 months' follow-up, and reported instability at 1 year of follow-up.
Questionnaires were administered at baseline at 4 weeks, 8 weeks, 3 months, and 1 year after injury. Information was asked about: subjective recovery on a 0–10 point scale (0 represents no recovery and 10 full recovery); re-sprain; the patient's appreciation of the received treatment (no, partial, or full appreciation); and reported instability. Treatment preference before randomisation (physical therapy, physician, or no preference at all) was measured at baseline only.
Three months after injury a blinded assessor performed a standardised clinical examination. The un-injured ankle was tested first during all tests and in all patients. All tests were performed barefooted. This examination included two functional stability tests (a modification of Romberg's test,8 and the one-leg hop test8, 22), and an active ROM test of the ankle.22
Tested instability was assessed by patients standing on one leg for a maximum of 1 minute with eyes open, and standing on one leg for a maximum of 30 seconds with eyes closed. Balance time (the time patients could stand on one leg) was noted and patients were asked if they experienced the same feeling of stability in both legs. If not, they were asked to indicate which leg felt less stable.8
A one-leg hop test (forward jumping and landing on the same foot five times with each leg) was performed to assess functional stability. Patients were asked if they experienced the same feeling of stability in both legs; if not, they were asked to indicate which leg they judged as less stable.
For the active ROM test a electronic digital inclinometer was used (Cybex EDI 320, New York, US). Sitting with the knees at 0 degrees and the ankle in maximal plantar flexion, participants performed maximal dorsal flexion in the ankle. Differences between sprained and not-sprained ankle scores were calculated.
Sample size
The study initially aimed at enrolling 158 patients during an inclusion period of 1 year, divided over two treatment groups of 79 persons each. This sample size was calculated to detect a 20% difference (a suspected decrease from 45% to 25%) between both groups in the occurrence of re-sprains after 3 months' follow-up, with a power of 80% (1–β) and a one-tailed level of significance (α) of 5%.
The 20% difference was based on a study by Wester et al23 which reported a difference of 29% in occurrence of re-sprains between a training group and no-training group after a mean follow-up of 230 days (standard deviation [SD] 62.9). Their population seemed comparable to the population in the current study. All patients with an acute lateral ankle sprain recruited from the local casualty department were given the usual conventional treatment and randomised to either a training group or a no-training group.
Statistical analysis
Data were analysed with researchers being unaware of participants' group assignment, using both an intention-to-treat analysis and a per-protocol analysis (that is, analysis based only on patients who complete the entire treatment protocol). For patients with incomplete datasets or who were lost to follow-up, the last available data were carried forward.
Patients' appreciation of the received treatment was dichotomised (full appreciation versus no or partial appreciation). Multivariable logistic regression was used to analyse relationships between dichotomous outcomes (re-sprain, appreciation of the received treatment, and dichotomised recovery) and treatment (conventional treatment alone or combined with supervised exercises). Multivariable logistic regression produced odds ratios (OR) as outcome dimensions; therefore, results are presented as ORs with 95% confidence intervals (CIs). Risk differences with CIs were also added, as these are easier to interpret. Multivariable linear regression was used to analyse relationships between continuous outcome measures (subjective recovery and ROM) and treatment.
Potential confounders were age, sex, body mass index, injury grade, treatment received as preferred, ankle load during work, and ankle load during leisure time at baseline. Variables that affected the univariate relationship (more than 10% change of the slope or β) were entered the multivariate model. Data are presented at a two-tailed level of significance (α) of 5%.
RESULTS
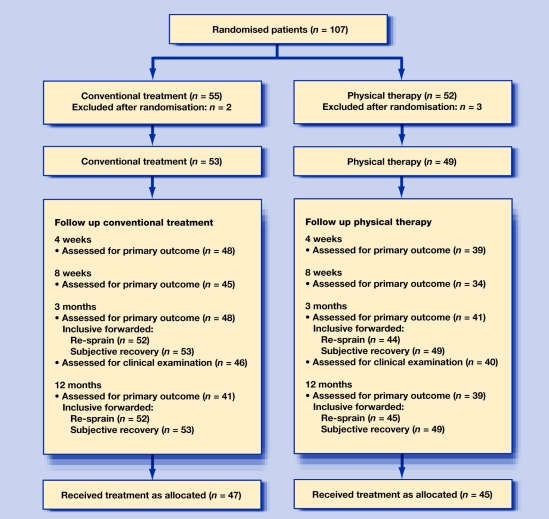
A total of 107 patients were randomised during the inclusion period. Five of these patients (three from the physical therapy group, two from the conventional treatment group) were randomised too early. Although they reported to have sent the baseline questionnaire at the time they were randomised, researchers never received it; therefore, these five patients could not be included in the analyses. During the trial another five patients (four from the physical therapy group, one from the conventional treatment group) were lost to follow-up, but their last available data were carried forward in the analyses (Figure 1).
Figure 1.
Flow of participants through the trial.
Patients in the physical therapy group received a mean of 6.1 (SD = 3) treatment sessions (median = 7). As some participants did not receive the treatment as initially allocated or crossed over and visited a physiotherapist during the trial, the treatment received was not 100% as initially allocated. Those who did not receive the physical therapy as allocated (n = 4) never attended the physical therapy practice. Of the patients assigned to the group with conventional treatment alone, 11% (n = 6) crossed over and visited a physiotherapist during follow up (all within the 3 months' follow-up period).
All patients in both groups received instructions on home exercises as part of the conventional treatment at the initial examination. In the group with additional supervised exercises, 74% (n = 28) of the patients reported to have done their home exercises regularly. Most patients in the group with conventional treatment alone (82%; n = 36) reported that in the first 3 weeks after injury they rarely or never did their home exercises.
Participants' baseline characteristics (Table 1) indicate that both groups are well balanced regarding their demographic and clinical variables.
Table 1.
Baseline characteristics of the study population.
| Characteristic | Conventional treatment (n = 53) | Physical therapy (n = 49) |
|---|---|---|
| Age, years: mean (SD) | 37.0 (11.9) | 37.0 (11.9) |
| Body mass index, kg/m2: mean (SD) | 25.4 (4.2) | 25.1 (3.8) |
| Interval between injury and baseline, days: mean (SD) | 4.6 (2.4) | 4.8 (2.3) |
| Sex, n (%) | ||
| Female | 22 (42) | 21 (43) |
| Male | 31 (59) | 28 (57) |
| Injury grade, n (%) | ||
| I, mild | 23 (43) | 20 (41) |
| II, moderate | 18 (34) | 23 (47) |
| III, severe | 1 (2) | 3 (6) |
| Unknown | 11 (21) | 3 (6) |
| Patient treatment preference, n (%) | ||
| No preference | 8 (15) | 15 (31) |
| Conventional treatment | 30 (57) | 23 (47) |
| Physical therapy | 9 (17) | 10 (20) |
| Unknown | 6 (11) | 1 (2) |
| Ankle affected, n (%) | ||
| Left | 26 (49) | 22 (45) |
| Right | 27 (51) | 27 (55) |
| Setting, n (%) | ||
| General practice | 33 (62) | 31 (63) |
| Emergency department | 20 (38) | 18 (37) |
| Ankle protection, n (%) | ||
| Tape or bandage | 31 (58) | 26 (53) |
| Brace | 8 (15) | 10 (20) |
| Ankle load during work, n (%) | ||
| No | 14 (26) | 11 (22) |
| Light | 20 (38) | 20 (41) |
| Heavy | 14 (26) | 17 (35) |
| Unknown | 5 (9) | 1 (2) |
| Ankle load during sports or hobby, n (%) | ||
| No | 13 (25) | 8 (16) |
| Light | 10 (19) | 16 (33) |
| Heavy | 25 (47) | 22 (45) |
| Unknown | 5 (9) | 3 (6) |
After 12 months' follow up there were five patients (one from the conventional treatment group and four patients of the physical therapy group) who only filled in their baseline questionnaire. Therefore, outcome measures could not be carried forward.
For the per-protocol analysis, six patients of the conventional treatment group and four patients of the physical therapy group who did not adhere to the treatment protocol were excluded.
Treatment effect after 3 months
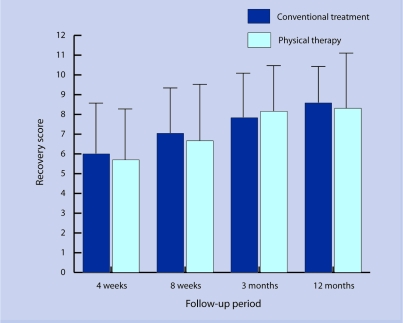
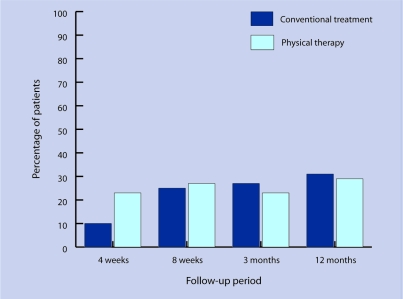
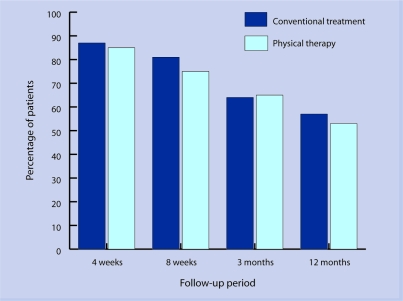
For all outcomes after 3 months no confounder was identified. Data for the primary and secondary outcomes at 3 months' follow-up are given in Table 2. No significant difference was found between treatment groups for subjective recovery (Figure 2), occurrence of re-sprains (Figure 3), tested instability, reported instability (Figure 4), or ROM.
Table 2.
Outcomes after 3 and 12 months' follow-up with univariate analysis.a
| Outcome, follow-up | Conventional treatment | Physical therapy | Univariate analysis | Risk difference |
|---|---|---|---|---|
| n (%) | n (%) | OR (95% CI) | AR% (95% CI) | |
| Re-sprain, 3 months | 14 (27) | 10 (23) | 0.80 (0.31 to 2.03) | −4.2 (−21.5 to 13.1%) |
| Re-sprain, 12 months | 16 (31) | 13 (29) | 0.91 (0.38 to 2.19) | 2.5 (−16.8 to 22.0%) |
| Reported instability, 3 months | 34 (64) | 32 (65) | 1.05 (0.47 to 2.37) | 1.2 (−17.4 to 19.7%) |
| Reported instability, 12 months | 30 (57) | 26 (53) | 0.87 (0.40 to 1.89) | 3.5 (−22.9 to 15.8%) |
| Tested instability, 3 months | 26 (57) | 18 (45) | 0.63 (0.27 to 1.48) | −11.5 (−32.6 to 9.5%) |
| Full treatment appreciation, 3 months | 32 (68) | 40 (91) | 4.69 (1.41 to15.5)b | 22.8 (7.0 to 38.7%) |
| Mean (SD) | Mean (SD) | Mean difference (95% CI) | Effect size (95% CI) | |
| Subjective recovery, 3 months | 7.8 (2.4) | 8.2 (2.4) | 0.33 (−0.60 to 1.27) | 0.14 (−0.25 to 0.54) |
| Subjective recovery, 12 months | 8.6 (1.9) | 8.3 (2.8) | −0.28 (−1.22 to 0.66) | −0.12 (−0.51 to 0.28) |
| ROM difference, 3 monthsc | 3.7 (8.0) | 1.9 (6.1) | −1.82 (−4.96 to 1.32) | −0.25 (−0.69 to 0.18) |
Primary outcomes in bold.
P≤0.05.
Injured ankle versus non-injured ankle. ROM = range of movement. AR = attributive risk.
Figure 2.
Subjective recovery: mean (standard deviation) recovery score (range 0–10) at 4 weeks, 8 weeks, 3 months, and 1-year of follow-up.
Figure 3.
Re-sprains: percentage of patients who reported a re-sprain within 4 weeks, 8 weeks, 3 months, and 1 year follow-up.
Figure 4.
Reported instability at 4 weeks, 8 weeks, 3 months, and 1-year of follow-up.
A significant difference was observed in the appreciation of the received treatment in favour of the supervised exercises: 68% patients from the conventional treatment group and 91 % patients from the physical therapy group fully appreciated the received treatment. OR for appreciation of the received treatment was 4.69 (95% CI = 1.41 to 15.5) in favour of the physical therapy group.
When subjective recovery is dichotomised (10 representing full recovery versus a score below 10) 19% patients from the conventional treatment group and 33% from the physical therapy group reported full recovery. OR of full recovery was 2.09 (95% CI = 0.84 to 5.18). When 9 was used as cut-off score instead of 10, 60% patients from the conventional treatment group and 59% from the physical therapy group reported full recovery, with an OR of 0.95 (95% CI =0.43 to 2.10).
Using per-protocol analysis, the mean subjective recovery score (possible range from 0 to 10) for the conventional treatment group was 8.1 (SD 2.2) and for the physical therapy group was 8.4 (SD 2.0); mean difference was −0.34 (95% CI = −1.21 to 0.54). OR for re-sprains was 0.99 (95% CI = 0.37 to 2.65). Similar to the intention-to-treat analysis, a significant difference was found in the appreciation of the received treatment with an OR of 3.48 (95% CI = 1.01 to 12.0). Tested and reported instability between both groups showed no significant difference; ORs were 0.66 (95% CI = 0.27 to 1.61) and 1.02 (95% CI = 0.44 to 2.37) respectively.
Treatment effect after 1 year
For all outcomes after 1 year no confounder was identified. Data for the primary and secondary outcomes at 12 months' follow up are given in Table 2. No significant difference was found between both groups in subjective recovery (Figure 2), occurrence of re-sprains (Figure 3), or reported instability (Figure 4).
Forty-two per cent of patients from the conventional treatment group and 53% from the physical therapy group reported full recovery when a score of 10 on a 11-point scale represents full recovery. OR of full recovery was 1.59 (95% CI = 0.73 to 3.49). If a score of 9 or 10 represents full recovery, 72% patients from the conventional treatment group and 74% patients from the physical therapy group reported full recovery, with an OR of 1.20 (95% CI = 0.51 to 2.84).
Similar to the intention-to-treat analysis, no significant difference was found using the per-protocol analysis. Mean difference for subjective recovery was 0.13 (95% CI = −0.79 to 1.04); OR for re-sprains was 1.10 (95% CI = 0.44 to 2.74); and OR for reported instability was 0.84 (95% CI = 0.37 to 1.91).
DISCUSSION
Summary of main findings
This study showed that usual care combined with supervised exercises compared with usual care alone at 3 months and 1-year of follow up after an acute lateral ankle sprain did not indicate clinically-meaningful differences in the occurrence of re-sprains or in subjective recovery in patients consulting a GP or the emergency department. However, due to the large CI of the risk difference for re-sprains after 3 months' follow up, there is a slight possibility that usual care combined with supervised exercises is the preferred treatment option for this population. In support of this approach, patients' appreciation of the received treatment was higher for those who consulted the physiotherapist for supervised exercises than those who received usual care.
Strength and limitations of the study
A few limitations of the present study should be noted. Due to financial and time restrictions, researchers had to finish the (already extended) inclusion period before 158 patients were included. Nevertheless, this trial is still one of the largest in the field of ankle sprains to study the effect of supervised rehabilitation training. Sample size calculation was based on a 20% decrease (45 to 25%) in occurrence of re-sprains, as found by Wester et al who had a comparable population to the current study.23 The occurrence of re-sprains in the conventional treatment group was lower than expected (27% after 3 months, 31% after 12 months). Compared with the control group only, an additional decrease of 4% after 3 months and only a decrease of 2% after 12 months in occurrence of re-sprains was seen in the group receiving supervised exercises. The magnitude of this difference indicates that adding supervised exercises to conventional treatment does not lead to clinically-relevant improvements. From the 95% CI of the difference (−21.5 to 13.1%) it may be concluded that a true population difference of 20% is not very likely with this intervention.
Comparison with existing literature
The main findings in the present study are concordant with several other studies.24–27 These studies found no difference in occurrence of re-sprains or subjective instability between groups. Nilsson24 examined elastic wrapping alone versus elastic wrapping combined with supervised exercises in patients who consulted the emergency department after 4.3 months and 3 years' follow up. Oostendorp25 compared plaster bandage alone with plaster bandage combined with a standardised exercise programme in patients who were injured during high-risk sport and referred to a physiotherapist after 3 months. Eiff et al26 conducted their trial at a military centre, and Konradsen et al27 treated 80 patients with grade III lateral ligament ruptures: both studies compared early mobilised and immobilised patients after 12 months' follow up.
Other studies reported more positive results. Holme et al28 and Reinhardt et al29 reported diminished re-sprains and less instability in the training group after 3 months' follow-up. However, the participants in these studies were, respectively, recreational athletes, and recruits and professional soldiers. Patients in the intervention group of Holme et al28 participated in a supervised-exercises group for 1 hour twice weekly, compared with the current study which conducted a maximum of nine half-hour sessions within in a period of 3 months. Oostendorp25 reported, in contrast to the results after 3 months' follow up, a significant difference in ‘fear of the ankle giving way’ after 6 months' follow up. The 24 participants included in Oostendorp's study exclusively had a grade I or II sprain, were aged between 15 and 30 years, and were injured during volleyball, basketball, handball, or soccer.
Wester et al23 and Holme et al28 reported fewer re-sprains after 12 months' follow up. Wester et al also reported less instability after 12 months in the 48 patients who completed the study. All were active in sport for at least 2 hours a week, patients with clinically demonstrable ankle instability were excluded, and the treatment only consisted of wobble-board training. The differences in outcome between the current study and these studies could be due to the smaller number of patients in those trials,8,23,28,29 specific patient groups,23,25,28,29 different settings,25,29 and different interventions.23,25,28
These latter studies demonstrate that specific patient groups (people involved in sport) may benefit from early ankle mobilisation combined with supervised exercises. In line with these studies is the study of Verhagen et al30 which found that a proprioceptive balance-board training programme does not have a primary preventive effect. Instead, the programme was thought to have a rehabilitative effect, as the training programme led to a lower incidence of ankle sprains for volleyball players with a history of ankle sprains.
To demonstrate benefits for a specific patient group in the current study, subgroup analyses are needed. For example, subgroups classified by injury grade or level of sport practice at baseline. Such subgroup analyses did not lead to any significant differences. These analyses were explorative and were based on very small numbers. Therefore, no meaningful conclusion can be made based on subgroup analysis in this study.
Furthermore, it is known that the Dutch conventional treatment as defined in the current study (early ankle mobilisation, including home exercises and early weight bearing) differs from the conventional treatment in other countries, which is much less involved. In the current study the difference in treatment between conventional treatment and intervention is less extreme compared with other studies. Therefore, this could explain why no difference was found between conventional treatment and intervention, while other studies have found a difference.
Implications for future research or clinical practice
This study was not large enough to perform meaningful subgroup analyses. However, a trial such as this in a specific subgroup would be of value. This study showed that after 1 year of follow up, some patients still had complaints relating to their initial injury. Factors causing persistent complaints are largely unknown. Therefore, a study to evaluate prognostic factors for poor recovery and occurrence of re-sprains is needed. The information derived from such a study could be used to determine a high-risk population for non recovery or re-sprain. Such a group may be a subgroup of interest for specific interventions.
Until further research is carried out, results from this and previous studies suggest that there is no strong indication that conventional treatment should be accompanied by supervised rehabilitation training.
Supplementary Material
Acknowledgments
We would like to thank the GPs, the emergency department of Oosterschelde hospital, and physiotherapists and patients in Goes, the Netherlands and surrounding areas.
Supplementary information
Additional information accompanies this article at http://www.rcgp.org.uk/bjgp-suppinfo
Funding body
Local fund, zorgonderzoek Erasmus MC, of the Erasmus University (EMCR-2000)
Ethics committee
The Medical Ethics Committee of the Erasmus Medical Centre in Rotterdam (196.926/2000/238)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Goudswaard ANTS, van den Bosch WJHM, van Weert HCPM, Geijer RMM. The Dutch College of General Practitioners (NHG) Practice Guideline ‘Ankle sprains’. http://nhg.artsennet.nl/upload/104/guidelines2/E04.htm2000. (accessed 8 Aug 2007)
- 2.Andriacchi T, Sabiston P, DeHaven K, et al. Ligament: injury and repair. In: Woo SL-Y, Buckwalter JA, editors. Injury and repair of the musculoskeletal soft tissues. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1987. pp. 103–128. [Google Scholar]
- 3.Cummings GS, Tillman LJ. Remodeling of dense connective tissue in normal adult tissues. In: Currier DP, Nelson RM, editors. Dynamics of human biologic tissues. Philadelphia, PA: FA Davis Company; 1992. pp. 45–73. [Google Scholar]
- 4.Tillman LJ, Cummings GS. Biologic mechanisms of connective tissue mutability. In: Currier DP, Nelson RM, editors. Dynamics of human biologic tissues. Philadelphia, PA: FA Davis Company; 1992. pp. 1–44. [Google Scholar]
- 5.Kleinrensink GJ, Stoeckart R, Meulstee J, et al. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med Sci Sports Exerc. 1994;26(7):877–883. [PubMed] [Google Scholar]
- 6.Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29(5):361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 7.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 8.Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 9.Goldie PA, Evans OM, Bach TM. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75(9):969–975. [PubMed] [Google Scholar]
- 10.Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 11.Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5(3):187–195. doi: 10.1097/00042752-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5(3):175–186. doi: 10.1097/00042752-199507000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lynch SA, Renstrom PA. Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999;27(1):61–71. doi: 10.2165/00007256-199927010-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kerkhoffs GM, Rowe BH, Assendelft WJ, et al. Immobilisation for acute ankle sprain. A systematic review. Arch Orthop Trauma Surg. 2001;121(8):462–471. doi: 10.1007/s004020100283. [DOI] [PubMed] [Google Scholar]
- 15.Kerkhoffs GM, Rowe BH, Assendelft WJ, et al. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD003762. CD003762. [DOI] [PubMed] [Google Scholar]
- 16.Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73(2):305–312. [PubMed] [Google Scholar]
- 17.Van Os AG, Bierma-Zeinstra SM, Verhagen AP, et al. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther. 2005;35(2):95–105. doi: 10.2519/jospt.2005.35.2.95. [DOI] [PubMed] [Google Scholar]
- 18.Birrer RB, Fani-Salek MH, Totten VY, et al. Managing ankle injuries in the emergency department. J Emerg Med. 1999;17(4):651–660. doi: 10.1016/s0736-4679(99)00060-8. [DOI] [PubMed] [Google Scholar]
- 19.Van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78(6):958–962. doi: 10.1302/0301-620x78b6.1283. [DOI] [PubMed] [Google Scholar]
- 20.Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269(9):1127–1132. doi: 10.1001/jama.269.9.1127. [DOI] [PubMed] [Google Scholar]
- 21.Wees PhJ, van der LA, Feijts YAEJ, et al. The Royal Dutch Society of Physiotherapists (KNGF) Practice Guideline ‘Ankle Injury’. http://www.fysionet.nl/dossier_files/uploadFiles/RLEnkelletsel_PRLencover151206.pdf (accessed 12 Sept 2007). (In Dutch)
- 22.Gerber JP, Williams GN, Scoville CR, et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 23.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 24.Nilsson S. Sprains of the lateral ankle ligaments. J Oslo City Hosp. 1983;33(2–3):13–36. [PubMed] [Google Scholar]
- 25.Oostendorp R. Functionele instabiliteit na het inversietrauma van enkel en voet: een effectonderzoek pleisterbandage versus pleisterbandage gecombineerd met fysiotherapie. [Functional instability after ankle sprains; a trial of taping versus taping and exercise] Geneeskd Sport. 1987;20:45–55. [Google Scholar]
- 26.Eiff MP, Smith AT, Smith GE. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22(1):83–88. doi: 10.1177/036354659402200115. [DOI] [PubMed] [Google Scholar]
- 27.Konradsen L, Holmer P, Sondergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot Ankle. 1991;12(2):69–73. doi: 10.1177/107110079101200202. [DOI] [PubMed] [Google Scholar]
- 28.Holme E, Magnusson SP, Becher K, et al. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9(2):104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 29.Reinhardt C, Tiedemann v. Propriorezeptives Training bei Distorsionen des OSG als Beitrag zur Sekundarprohylaxe und früheren Wiedereingliederung. [Proprioreceptive training in ankle sprains can contribute to secondary prophylaxis and earlier reintegration] Dtsch Z Sportmed. 1999;50:89–91. [Google Scholar]
- 30.Verhagen E, van der Beek A, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.