Abstract
Lung ultrasound can be routinely performed at the bedside by intensive care unit physicians and may provide accurate information on lung status with diagnostic and therapeutic relevance. This article reviews the performance of bedside lung ultrasound for diagnosing pleural effusion, pneumothorax, alveolar-interstitial syndrome, lung consolidation, pulmonary abscess and lung recruitment/derecruitment in critically ill patients with acute lung injury.
Introduction
Management of critically ill patients requires imaging techniques, which are essential for optimizing diagnostic and therapeutic procedures. The diagnosis and drainage of localized pneumothorax and empyema, the assessment of lung recruitment following positive end-expiratory pressure and/or recruitment maneuver, the assessment of lung over-inflation, and the evaluation of aeration loss and its distribution all require direct visualization of the lungs. To date, chest imaging has relied on bedside chest radiography and lung computed tomography (CT).
General and cardiac ultrasound can be easily performed at the bedside by physicians working in the intensive care unit (ICU) and may provide accurate information with diagnostic and therapeutic relevance. It has become an attractive diagnostic tool in a growing number of situations, including evaluation of cardiovascular status, acute abdominal disease such as peritoneal collections, hepatobiliary tract obstruction, acalculous acute cholecystitis, diagnosis of deep venous thrombosis and ventilator-associated sinusitis [1]. Furthermore, ultrasound is relatively inexpensive and does not utilize ionizing radiation.
Recently, chest ultrasound has become an attractive new tool for assessing lung status in ventilated critically ill patients, as suggested by the increasing number of articles written about it by physicians practicing in chest, intensive care or emergency medicine. As a matter of fact, chest ultrasound can be used easily at the bedside to assess initial lung morphology in severely hypoxemic patients [2] and can be easily repeated, allowing the effects of therapy to be monitored.
Conventional lung imaging in critically ill patients
Bedside chest radiography
In the ICU, bedside chest radiography is routinely performed on a daily basis and is considered as a reference for assessing lung status in critically ill patients with acute lung injury. Limited diagnostic performance and efficacy of bedside portable chest radiography have been reported in several previous studies [3-5]. Several reasons account for the limited reliability of bedside chest radiography. First, during the acquisition procedure, the patient and the thorax often move, decreasing the spatial resolution of the radiological image. Second, the film cassette is placed posterior to the thorax. Third, the X-ray beam originates anterior, at a shorter distance than recommended and quite often not tangentially to the diaphragmatic cupola, thereby hampering the correct interpretation of the silhouette sign. These technical difficulties lead to incorrect assessment of pleural effusion, lung consolidation and alveolar-interstitial syndrome.
Lung computed tomography
Lung CT is now considered as the gold standard not only for the diagnosis of pneumothorax, pleural effusion, lung consolidation, atelectasis and alveolar-interstitial syndrome but also for guiding therapeutic procedures in critically ill patients, such as trans-thoracic drainage of localized pneumo-thorax, empyema or lung abscess. Lung image formation during CT relies on a physical principle similar to that used for image formation during chest radiography: the X-rays hitting the film or the CT detector depend on tissue absorption, which is linearly correlated to physical tissue density. In the first generation of CT scanners, the tube emitting X-rays and the X-ray detector were positioned on the opposite sides of a ring that rotated around the patient. Typically, a 1 cm-thick CT section was taken during each rotation, lasting 1 second, and the table supporting the patient had to be moved to acquire the next slice, the ring remaining in a fixed position. These conventional scanners were slow and had a poor ability to reconstruct images in different planes.
In the nineties, spiral CT scanners equipped with a slip ring were introduced, giving the possibility of scanning a volume of tissue rather than an individual slice. Acquisition time was markedly reduced and high quality reconstruction in coronal, sagittal and oblique planes became possible using a work station. Current multi-slice CT scanners, the third generation of CT scanners, are equipped with multiple X-ray detectors and the tube rotates in less than one second around the thorax while the table supporting the patient moves continuously. The multiple detectors and the decrease in rotation time allow faster coverage of a given volume of lung tissue, contributing to increased spatial resolution (voxel smaller than 1 mm3). Using specifically designed computer software offering sophisticated reconstruction and postprocessing capabilities, several hundred consecutive axial sections of the whole lung can be reconstructed from the volumetric data and visualized on the screen of a personal computer. If the computer is connected to an appropriate workstation, it is then possible to 'move into the lung' and to measure CT attenuations in any part of the pulmonary parenchyma, providing direct access to regional lung aeration. In addition, images can be reconstructed in coronal, sagittal and oblique planes, offering the possibility of a three-dimensional view of the organ. For hospitals having a computer server to store and retrieve pictures from, films are no longer necessary and physicians can derive much more accurate information on patients' lung status.
With the old generation of conventional CT scanners, obtaining contiguous 1.5 mm-thick CT sections from the apex to the diaphragm would have exposed patients to unsafe radiation levels. With the new generation of multi-slice CT scanners, the ionizing radiation is slightly greater than from a single slice spiral scanner. However, because more slices and images can be easily obtained with multi-slice CT scanners, there is a potential for increased radiation exposure [6] that has to be balanced against the total radiation dose resulting from chest radiography performed daily at the bedside.
To perform a lung CT scan, however, requires transportation to the department of radiology, a risky procedure necessitating the presence of trained physicians and sophisticated cardio-respiratory monitoring [7]. In addition, helical multi-detector row CT exposes the patient to a substantial radiation dose, which limits the repeatability of the procedure [6]. For these different reasons, lung CT remains a radiological test, access to which is limited in many ICUs, and bedside lung ultrasound appears as an attractive alternative method for deriving information on lung status.
Bedside lung ultrasound in critically ill patients
Technical equipment
Ultrasound machines should be lightweight, compact, easy to transport and robust, allowing multiple bedside examinations. They should be equipped with a high-performance screen and a paper recorder allowing transmission of medical information and subsequent comparisons. Generally, basic models presented by manufacturers combine all these features, and have the additional advantage of being reasonably priced. Such ultrasound machines are available in many emergency wards, ICUs, units of medical transportation and even in space [8-11].
Another technical characteristic should be required for the use of lung ultrasound in the ICU: the probes and the ultrasound machine should comply with repeated decontamination procedures since they serve multiple patients, and can be the vector for resistant pathogens that could be disseminated in the ICU [12-24]. The efficiency of the decontamination procedure is facilitated by a compact ultrasound machine equipped with a waterproof keyboard. This latter characteristic is present on a few ultrasound machines only, restricting choice.
Ultrasound machines are classified as non-critical items that contact only intact skin and require low level disinfection with chlorine-based products, phenolic, quaternary ammonium compounds or 70% to 90% alcohol disinfectant [25]. In critically ill patients, the skin and the digestive tract are considered as reservoirs from which nosocomial infections can issue. By transmitting nosocomial cutaneous flora from patient to patient, the probe may contribute to the dissemination of multi-resistant strains in the ICU and increase the incidence of nosocomial infections. If lung ultrasound is to be used routinely, our recommendation is to set up a rigid procedure of disinfection that must be strictly followed. As an example, the written decontamination procedure used in the Surgical ICU of La Pitié-Salpêtrière hospital in Paris is summarized in Table 1.
Table 1.
Cleaning and disinfecting procedure of ultrasound machine and probe in the Surgical ICU of La Pitié-Salpêtrière hospital
| Reduction of environmental contamination |
| Avoid as much as possible contact between ultrasound machine and patient's environment |
| Use single-patient package of coupling gela |
| Limit the probe contact to patient's skin |
| During examination, restrict contacts with the ultrasound machine to the probe and the keyboard |
| At the end of the examination, leave the probe on the bedb |
| Disinfection procedure at the end of the examination |
| Cleaning of examiner's hands |
| Cleaningc of the ultrasound machine, including the probe holder |
| Cleaning of the keyboard |
| Removing of gel with paper toweld |
| Cleaning of the probeb |
| Spontaneous air drying |
aAvoid using a gel bottle because the tip may be contaminated by contact with the probe or the patient's skin. Such contact may result in the contamination of the gel contained in the bottle. bThe contaminated probe should not be placed in the probe holder before decontamination. cWe use a detergent-disinfectant based on a quaternary ammonium compound with a processing time of at least 60 seconds. It cleans by removing organic material and suspending grease or oil and disinfects. After 11 years of experience, we have not found evidence of this causing material damage, including significant alterations of acoustic properties of the probe. dRemaining ultrasound gel on the lung ultrasound probe has shown bacterial growth when left overnight [20].
Ideally, an emission frequency of 5 to 7 MHz is desirable for optimizing ultrasound visualisation of the lung. The probe should be small with a convex tip so it can be easily placed on intercostal spaces, which offer an acoustic window on the lung parenchyma. Generally, a convex array probe (3 to 5 MHz), as available on multi-purpose ultrasound machines, combines these advantages and allows a good visualization of lung.
Lung ultrasound examination
The patient can be satisfactorily examined in the supine position. The lateral decubitus position offers, however, a better view on dorsal regions of lower lobes. A complete evaluation of both lungs requires a systematic protocol of examination. First, the operator should locate the diaphragm and the lungs. Lung consolidation or pleural effusion are found predominantly in dependant and dorsal lung regions and can be easily distinguished from liver or spleen once the diaphragm has been located. Using anterior and posterior-axillary lines as anatomical landmarks, each chest wall can be divided into six lung regions that should be systematically analyzed: upper and lower parts of the anterior, lateral and posterior chest wall. In a given region of interest, all adjacent intercostal spaces offer acoustic windows that allow the assessment of the lung surface by moving the probe transversally. Dorsal lung segments of upper lobes, located behind the scapula, are the only regions that cannot be explored by lung ultrasound. To provide an exhaustive assessment of lung aeration and pleural effusion, the ultrasound examination should cover both lungs, just as for auscultation. To be comprehensive, a chest ultrasound examination should take around 15 minutes, although with enough knowledge and skills, users can perform lung examination more quickly.
Normal ultrasound pattern and basic abnormalities
Normally, ultrasounds are not transmitted through anatomical structures filled with gas and the lung parenchyma is not visible beyond the pleura. The injured lung is characterized by a marked increase in tissue extending to lung periphery that produces ultrasound artifacts resulting from the abnormal gas/tissue interface. A number of recently published studies have demonstrated the ability of bedside lung ultrasound to accurately assess lung aeration in patients with acute lung injury.
When the loss of aeration is massive and results in lung consolidation, or when a pleural effusion is present, ultrasounds are transmitted to deep intra-thoracic structures. As a consequence, intramediastinal organs like the aortic arch can be visualized in the presence of consolidation of upper lobes [26]. Several studies have clearly established the value of lung ultrasound for detecting and quantifying pleural effusion and lung consolidation. For physicians beginning their lung ultrasound training on critically ill patients on mechanical ventilation, the detection of pleural effusion and lung consolidation in dependant lung regions is the easiest part and the basic skill is generally acquired over a very short period of time [27].
Normal pattern
For each considered intercostal space, the probe should be positioned perpendicular to the ribs. Using a longitudinal view, the ribs, characterized by a posterior shadowing, should be identified. A hyperechoic and sliding line, moving forward and back with ventilation, is seen 0.5 cm below the rib line, and is called the 'pleural line'. In time-motion mode, a 'seashore sign' is present, characterized by motionless parietal tissue over the pleural line and a homogeneous granular pattern below it [28]. The pleural line results from the movement of the visceral pleura against the parietal pleura during the respiratory cycle. Beyond this pleural line, motionless and regularly spaced horizontal lines are seen: they are meaningless and correspond to 'artifacts of repetition'. Thus, a normal ultrasound pattern is defined by 'lung sliding' associated with artifactual horizontal A-lines (Figure 1, Additional file 1). In one-third of patients with normal lungs, however, isolated vertical B-lines can be detected in dependant lung regions and are devoid of any pathological significance. B-lines move with the pleural line and efface A-lines.
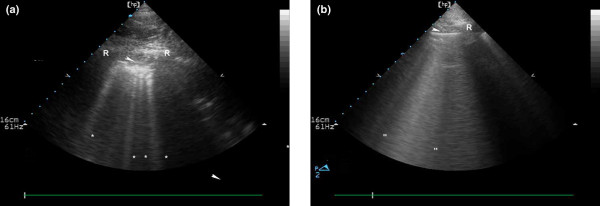
Figure 1.

Ultrasound pattern of normal lung. The pleural line (white arrow) is a roughly horizontal hyperechoic line 0.5 cm below the upper and lower ribs identified by acoustic shadow (R). A single vertical artifact arising from the pleural line and spreading up to the edge of the screen (comet-tails, indicated by asterisk) can be seen in dependant regions in normally aerated lungs.
Alveolar-interstitial syndrome
In the presence of injured lung characterized by an increased amount of lung tissue extending to lung periphery [29], vertical artifacts arising from the pleura and extending to the edge of the screen [30] are detected and called vertical 'B-lines' or 'comet tails'. They appear as shining vertical lines arising from the pleural line and reach the edge of the screen. The number of these vertical B-lines depends on the degree of lung aeration loss, and their intensity increases with inspiratory movements [2,31]. As mentioned above, less than one or two vertical artifacts can be detected in dependant lung regions in normally aerated lungs [31].
It has been demonstrated that multiple B-lines 7 mm apart are caused by thickened interlobular septa characterizing interstitial edema (Figure 2a, Additional file 2). In contrast, B-lines 3 mm or less apart are caused by ground-glass areas characterizing alveolar edema (Figure 2b, Additional file 3).
Figure 2.
Ultrasound aspects of alveolar-interstitial syndrome. (a) B-lines 7 mm apart or spaced comet-tail artifacts. The pleural line (white arrow) and the ribs (R) with their acoustic shadow. Spaced comet-tail artifacts (indicated by asterisks) or B-lines arising from the pleural line and spreading up to the edge of the screen are present. These artifacts correspond to thickened interlobular septa on chest CT scan. (b) B-lines 3 mm or less apart. The pleural line (white arrow) and the rib (R) with their acoustic shadow. Contiguous comet-tails arising from the pleural line and spreading up to the edge of screen are present. These artefacts correspond to ground-glass areas on chest CT scan.
Lung consolidation
Massive lung edema, lobar bronchopneumonia, pulmonary contusion and lobar atelectasis all induce a massive loss of lung aeration that enables ultrasounds to be transmitted towards the depth of the thorax. Lung consolidation appears as a hypoechoic tissue structure that is poorly defined and wedge-shaped [32]. Within the consolidation, hyperechoic punctiform images can be seen, corresponding to air bronchograms (air-filled bronchi) [33]. Penetration of gas into the bronchial tree of the consolidation during inspiration produces an inspiratory reinforcement of these hyperechoic punctiform images. The ultrasound size of the consolidation is not influenced by respiratory movements (Figure 3a,b, Additional file 4). Several studies have demonstrated that lung ultrasound has a high performance in diagnosing alveolar consolidation and is helpful for guiding percutaneous lung biopsy [2,34-37].
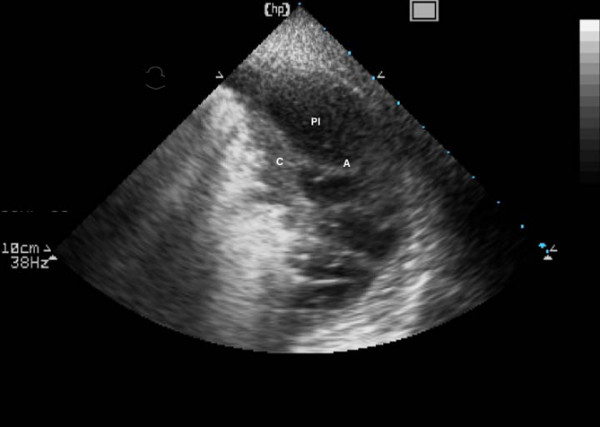
Figure 3.
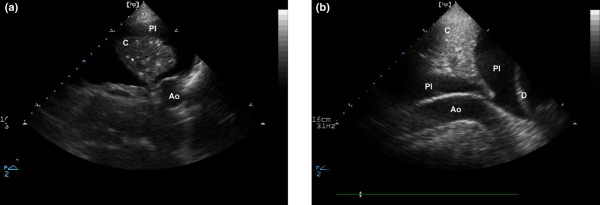
Ultrasound aspect of a lung consolidation and a pleural effusion. (a) Transversal view of consolidated left lower lobe; lung consolidation is seen as a tissular structure (C). In this consolidation, hyperechoic punctiform images (indicated by asterisk) can be seen; these correspond to air bronchograms (air-filled bronchi). Pleural effusion is anechoic (Pl). (b) Cephalocaudal view of consolidated left lower lobe: lung consolidation with air bronchograms. Ao, descending aorta; D, diaphragm; Pl, pleural effusion.
Peripheral lung abscesses with pleural contact or included inside a lung consolidation are also detectable by lung ultrasound [32,35,38,39]. They appear as rounded hypo-echoic lesions with outer margins (Figure 4, Additional file 5). If a cavity is present, additional non-dependant hyperechoic signals are generated by the interface gas/tissue. By analogy with percutaneous drainage of abdominal collections, ultrasound-guided percutaneous drainage of lung abscesses has proved to be a safe and effective alternative to CT-guided drainage [32,35,38,39].
Figure 4.
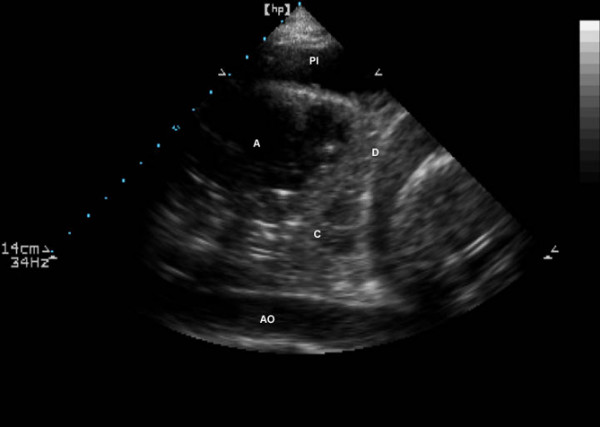
Cephalocaudal view of consolidated left lower lobe with a peripheral abscess. The abscess (A) appears as rounded hypoechoic lesions inside a lung consolidation (C). Ao, descending aorta; D, diaphragm; Pl, pleural effusion.
Ultrasound assessment of alveolar recruitment and lung re-aeration
Lung ultrasound has been recently shown to provide the possibility of assessing quantitatively the lung re-aeration resulting from antimicrobial therapy in 24 critically ill patients with ventilator-associated pneumonia [40]. At the bedside, the whole lung was examined as described above, and each region of interest was attributed a score according to four stages of lung aeration before and after antimicrobial therapy: normal, interstitial syndrome (B lines 7 mm apart), alveolar-interstitial syndrome (B lines less than 3 mm apart) and alveolar consolidation. A tight correlation was found between pulmonary re-aeration measured by lung CT and the change in the 'ultrasound score'. Further studies are required to confirm whether lung ultrasound, using similar principles, provides the possibility of measuring alveolar recruitment resulting from positive end expiratory pressure (PEEP) or recruitment maneuver.
Pleural effusion
Pleural effusion should be sought on a longitudinal view, in dependant lung regions delineated by the chest wall and the diaphragm. It appears as a hypoechoic and homogeneous structure with no gas inside and is present during expiration and inspiration [41]. In other words, it appears as a dependant dark zone free of echo (Figure 3a,b, Additional file 4). Since pleural effusion acts as an acoustic window, lung can be seen as a bright pleural line if it remains aerated. If the pleural effusion is abundant enough to be compressive, the lung is seen consolidated and floating in the pleural effusion (Figure 5, Additional file 6). Assessment of pleural effusion requires attention to spleen or liver and diaphragm, especially when pleural puncture is considered. Pleural effusion can be easily distinguished from spleen or liver by using color Doppler that shows intrasplenic and intrahepatic blood vessels; or by visualization of a sinusoidal inspiratory movement of the visceral pleura from depth to periphery [42]. The skills required to detect pleural effusion are easy to acquire, as suggested by several publications [43-45].
Figure 5.
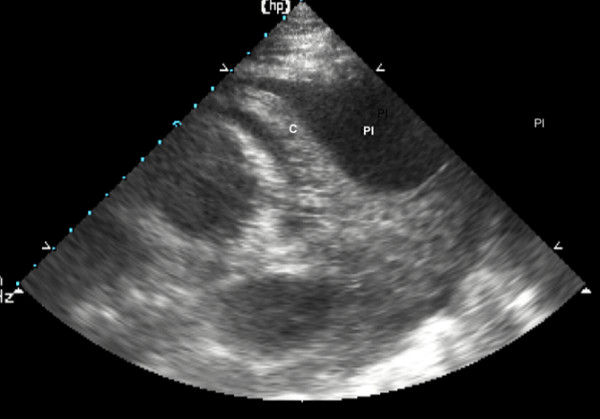
Consolidated lung 'floating' in a massive pleural effusion. The pleural effusion (Pl) is abundant enough to be compressive and the lung (C) is seen consolidated and floating in the pleural effusion.
The lung ultrasound approach has been proposed for quantifying pleural effusion volume [45-48]. In the supine position, an interpleural distance at the lung base, defined as the distance between the lung and the posterior chest wall, ≥50 mm is highly predictive of a pleural effusion ≥500 ml [45,48]. Measurement of the interpleural distance can be performed at either end-expiration or end-inspiration [46], with no difference between them, and seems less reliable when measured on the left side [46]. All studies agree that ultrasound measurement of the interpleural space at the lung base is not accurate enough to quantify small (≤500 ml) and very large (≥1,000 ml) pleural effusions [45-47]. Recently, another ultrasound approach has been proposed for quantifying pleural effusion: by multiplying the height of the pleural effusion by its transversal area, measured half-way between upper and lower limits. An excellent correlation was found between the volume of pleural effusion assessed by CT of the whole lung and the ultrasound determination [49].
Although the nature of pleural effusion (transudate or exsu-date) cannot be accurately assessed on ultrasound examination only, some ultrasound patterns are evocative. Transudates are always anechoic but exsudates appear often to be echoic and loculated [50].
Last but not least, lung ultrasound is increasingly used for guiding thoracocentesis at the bedside [42,51]. It provides the possibility of detecting pleural adherences that may hamper efficient thoracic drainage and transform thoraco-centesis into a risky procedure (Figure 6, Additional file 7). It enables the safe thoracic drainage of small and/or loculated pleural effusions. It may reduce the risk of intrafissural or intraparenchymal placement of thoracic tubes [52].
Figure 6.
Consolidated lung and adjacent pleural effusion with pleural adherences. The pleural effusion (Pl) is abundant and the lung is seen consolidated and floating (C) in the pleural effusion with pleural adherences (A).
Pneumothorax
Pneumothorax is defined by the interposition of gas between visceral and parietal pleural layers. As a consequence, lung sliding is abolished, ultrasounds cannot be transmitted through the injured lung parenchyma and comet tails (vertical B-lines) are no longer visible. Only longitudinal reverberations of motionless pleural line (horizontal A-lines) can be seen [53]. In some circumstances, such as the presence of a thoracic tube, pleural adherences, bullous emphysema and advanced chronic obstructive pulmonary disease, lung sliding can be abolished in the absence of pneumothorax. The diagnosis remains uncertain in patients with normal lung aeration whereas in patients with lung injury, the presence of vertical B-lines rules out the diagnosis.
The ultrasound diagnosis of pneumothorax is the most difficult part of training: long experience is required to acquire appropriate skills that rely on the ability to recognize lung sliding and its abolition [42]. When possible, the use of higher emission frequencies (5 to 10 MHz) facilitates the recognition of lung sliding abolition. The diagnosis is even more difficult in the presence of partial pneumothorax. The patient should lie strictly supine to allow location of pleural gas effusion in non-dependant lung regions. To confirm the diagnosis of partial pneumothorax, examination should be extended lo lateral regions of the chest wall to localize the point where the normal lung pattern (lung sliding and/or the presence of vertical B-lines) replaces the pneumothorax pattern (absent lung sliding and horizontal A-lines). This point is called the 'lung point' [54] (Additional file 8). Utilization of the time motion mode can facilitate detection of the lung point (Figure 7).
Figure 7.
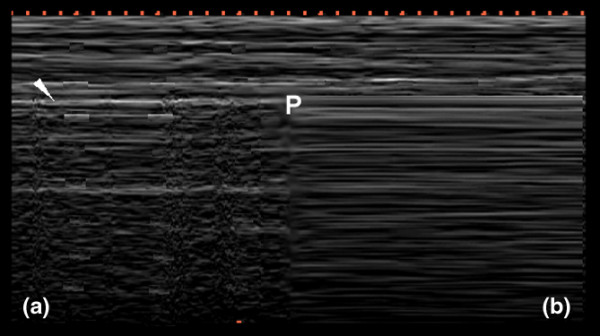
Time-motion mode lung ultrasound. (a) Normal lung and (b) pneumothorax patterns using time-motion mode lung ultrasound. In time motion mode, one must first locate the pleural line (white arrow) and, above it, the motionless parietal structures. Below the pleural line, lung sliding appears as a homogenous granular pattern (a). In the case of pneumothorax and absent lung sliding, horizontal lines only are visualised (b). In a patient examined in the supine position with partial pneumothorax, normal lung sliding and absence of lung sliding may coexist in lateral regions of the chest wall. In this boundary region, called the 'lung point' (P), lung sliding appears (granular pattern) and disappears (strictly horizontal lines) with inspiration when using the time-motion mode.
The ultrasound pattern characterizing pneumothorax was described in the early 1990s [55-57]. Several studies have demonstrated that bedside lung ultrasound is more efficient than bedside chest radiography for diagnosing pneumothorax in emergency conditions if rapidly performed by the clinician in charge [28,58-60]. Recently, interest in lung ultrasound for diagnosing pneumothorax in emergency and trauma patients has been reported [61]. Using a portable ultrasound device and a 3.5 to 7 MHz probe, three emergency physicians, having received formal 28 hour training for emergency bedside ultrasound, systematically performed lung ultrasound in 135 trauma patients admitted either to the resuscitation or the Emergency ICU of the Second Affiliated Hospital of Hangzhou (China). At admission, all patients had frontal chest radiography and 131 a thoracic computed scan of the whole lung, which served as gold standard for the diagnosis of pneumothorax. The sensitivity and specificity of lung ultrasound for diagnosing pneumothorax were 86% and 97%, respectively, whereas conventional chest radiography had sensitivity and specificity of 28% and 100%, respectively. Lung ultrasound over-diagnosed pneumothorax in two patients with pleural adherences. Bedside chest radiography missed all partial pneumothoraces whereas lung ultrasound detected the majority of them by identifying the lung point. In addition, lung ultrasound allowed the detection of pneumothorax within 2 to 4 minutes compared to 20 to 30 minutes for the chest radiography.
Limitations of lung ultrasound
When adopting lung ultrasound as a routine monitoring tool in the ICU, physicians should be aware of its limitations. Lung ultrasound examination and correct interpretation of the resulting images require formal training aimed at acquiring the necessary knowledge and skills. If several lung ultrasound examinations are performed on a daily basis, the learning curve for acquiring skills for diagnosing pleural effusion, lung consolidation and alveolar-interstitial syndrome is short, less than six weeks. The intra- and inter-observer variability is small, less than 5% [2]. The learning time for acquiring skills required for diagnosing pneumothorax is probably longer due to its low incidence in the critical care environment. In fact, the acquisition of the skills for diagnosing pneumothorax is the most difficult part of lung ultrasound training.
Lung ultrasound has intrinsic limitations that are not operator dependent but patient dependent. Obese patients are frequently difficult to examine using lung ultrasound because of the thickness of their rib cage. The presence of subcutaneous emphysema or large thoracic dressings alters or precludes the propagation of ultrasound beams to the lung periphery. Last but not least, it has to be pointed out that lung ultrasound cannot detect lung over-inflation resulting from an increase in intrathoracic pressures.
Conclusion
Accuracy of lung ultrasound for diagnosing pneumothorax, lung consolidation, alveolar-interstitial syndrome and pleural effusion in critically ill patients is clearly established. The routine use of lung ultrasound appears as an attractive alternative to bedside chest radiography: it is non-invasive, easily repeatable at the bedside and provides an accurate evaluation of the respiratory status of patients with acute lung injury. In ICUs where it is used as a routine monitoring tool, the indications of bedside chest radiography can be restricted to the assessment of the intrathoracic position of catheters and endotracheal tubes and to patients where lung ultrasound is not feasible. As a consequence, radiation exposure to physicians, nurses and patients is drastically reduced as well as costs. Lung ultrasound performed by physicians in charge of ICUs appears to be one of the most promising techniques for respiratory monitoring and should rapidly expand in the near future.
Abbreviations
CT = computed tomography; ICU = intensive care unit.
Competing interests
The authors declare that they have no competing interests.
Supplementary Material
An avi movie showing ultrasound pattern of normal lung: pleural line is a roughly horizontal hyperechoic line 0.5 cm below the upper and lower ribs identified by acoustic shadow. motionless and regularly spaced horizontal lines are seen below. They are meaningless and correspond to "artifacts of repetition".
An avi movie showing B lines 7 mm apart or spaced comet-tail artefacts. These spaced comet-tail artefacts arise from the pleural line and spread up to the edge of screen. These artefacts correspond to thickened interlobular septa at chest computed tomography scan.
An avi movie showing B lines 3 mm or less apart: contiguous comet-tails arising from the pleural line and spreading up to the edge of screen are present. These artefacts correspond to ground-glass areas on chest computed tomography scan.
An avi movie showing a cephalocaudal view of consolidated left lower lobe in and pleural effusion. Lung consolidation with air bronchograms, diaphragm and descending aorta are seen.
An avi movie showing a cephalocaudal view of consolidated left lower lobe with a peripheral abscess. The abscess appears as rounded hypoechoic lesions inside a lung consolidation.
An avi movie showing a massive pleural effusion enough to be compressive. the lung is seen consolidated and floating in this pleural effusion.
An avi movie showing a consolitated lung and adjacent pleural effusion with pleural adherences: the pleural effusion is abundant and the lung is seen consolidated and floating in the pleural effusion with pleural adherences.
An avi movie showing pneumothorax and "lung point". In a patient examined in the supine position with partial pneumothorax, normal lung sliding (left part of the screen) and pneumothoax (absence of lung sliding at right part of the screen) coexist. This boundary region is called the "lung point". It should be noted that lung sliding appears (coming from the left part of the screen) and disappears (absent lung sliding, horizontal lines only are visualised) with inspiration.
References
- Lichtenstein D, Biderman P, Meziere G, Gepner A. The "sinusogram", a real-time ultrasound sign of maxillary sinusitis. Intensive Care Med. 1998;24:1057–1061. doi: 10.1007/s001340050716. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100:9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- Greenbaum DM, Marschall KE. The value of routine daily chest x-rays in intubated patients in the medical intensive care unit. Crit Care Med. 1982;10:29–30. doi: 10.1097/00003246-198201000-00007. [DOI] [PubMed] [Google Scholar]
- Bekemeyer WB, Crapo RO, Calhoon S, Cannon CY, Clayton PD. Efficacy of chest radiography in a respiratory intensive care unit. A prospective study. Chest. 1985;88:691–696. doi: 10.1378/chest.88.5.691. [DOI] [PubMed] [Google Scholar]
- Rouby JJ, Puybasset L, Cluzel P, Richecoeur J, Lu Q, Grenier P. Regional distribution of gas and tissue in acute respiratory distress syndrome. II. Physiological correlations and definition of an ARDS Severity Score. CT Scan ARDS Study Group. Intensive Care Med. 2000;26:1046–1056. doi: 10.1007/s001340051317. [DOI] [PubMed] [Google Scholar]
- Mayo JR, Aldrich J, Muller NL. Radiation exposure at chest CT: a statement of the Fleischner Society. Radiology. 2003;228:15–21. doi: 10.1148/radiol.2281020874. [DOI] [PubMed] [Google Scholar]
- Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med. 2004;30:1579–1585. doi: 10.1007/s00134-004-2177-9. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick AW, Breeck K, Wong J, Hamilton DR, McBeth PB, Sawadsky B, Betzner MJ. The potential of handheld trauma sonography in the air medical transport of the trauma victim. Air Med J. 2005;24:34–39. doi: 10.1016/j.amj.2004.10.012. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Courret JP. Feasibility of ultrasound in the helicopter. Intensive Care Med. 1998;24:1119. doi: 10.1007/s001340050730. [DOI] [PubMed] [Google Scholar]
- Sargsyan AE, Hamilton DR, Jones JA, Melton S, Whitson PA, Kirkpatrick AW, Martin D, Dulchavsky SA. FAST at MACH 20: clinical ultrasound aboard the International Space Station. J Trauma. 2005;58:35–39. doi: 10.1097/01.ta.0000145083.47032.78. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick AW, Nicolaou S, Campbell MR, Sargsyan AE, Dulchavsky SA, Melton S, Beck G, Dawson DL, Billica RD, Johnston SL, Hamilton DR. Percutaneous aspiration of fluid for management of peritonitis in space. Aviat Space Environ Med. 2002;73:925–930. [PubMed] [Google Scholar]
- Muradali D, Gold WL, Phillips A, Wilson R. Can ultrasound probes and coupling gel be a source of nosocomial infection in patients undergoing sonography? An in vivo and in vitro study. Am J Roentgenol. 1995;164:1521–1524. doi: 10.2214/ajr.164.6.7754907. [DOI] [PubMed] [Google Scholar]
- Patterson SL, Monga M, Silva JB, Bishop KD, Blanco JD. Microbiologic assessment of the transabdominal ultrasound transducer head. South Med J. 1996;89:503–504. doi: 10.1097/00007611-199605000-00011. [DOI] [PubMed] [Google Scholar]
- Tesch C, Froschle G. Sonography machines as a source of infection. Am J Roentgenol. 1997;168:567–568. doi: 10.2214/ajr.168.2.9016251. [DOI] [PubMed] [Google Scholar]
- Abdullah BJ, Mohd Yusof MY, Khoo BH. Physical methods of reducing the transmission of nosocomial infections via ultrasound and probe. Clin Radiol. 1998;53:212–214. doi: 10.1016/S0009-9260(98)80103-7. [DOI] [PubMed] [Google Scholar]
- Gaillot O, Maruejouls C, Abachin E, Lecuru F, Arlet G, Simonet M, Berche P. Nosocomial outbreak of Klebsiella pneumoniae producing SHV-5 extended-spectrum beta-lactamase, originating from a contaminated ultrasonography coupling gel. J Clin Microbiol. 1998;36:1357–1360. doi: 10.1128/jcm.36.5.1357-1360.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohara T, Itoh Y, Itoh K. Ultrasound instruments as possible vectors of staphylococcal infection. J Hosp Infect. 1998;40:73–77. doi: 10.1016/S0195-6701(98)90028-7. [DOI] [PubMed] [Google Scholar]
- Fowler C, McCracken D. US probes: risk of cross infection and ways to reduce it – comparison of cleaning methods. Radiology. 1999;213:299–300. doi: 10.1148/radiology.213.1.r99au41299. [DOI] [PubMed] [Google Scholar]
- Ohara T, Itoh Y, Itoh K. Contaminated ultrasound probes: a possible source of nosocomial infections. J Hosp Infect. 1999;43:73. doi: 10.1053/jhin.1999.0618. [DOI] [PubMed] [Google Scholar]
- Karadenz YM, Kilic D, Kara Altan S, Altinok D, Guney S. Evaluation of the role of ultrasound machines as a source of nosocomial and cross-infection. Invest Radiol. 2001;36:554–558. doi: 10.1097/00004424-200109000-00009. [DOI] [PubMed] [Google Scholar]
- Kibria SM, Kerr KG, Dave J, Gough MJ, Homer-Vanniasinkam S, Mavor AI. Bacterial colonisation of Doppler probes on vascular surgical wards. Eur J Vasc Endovasc Surg. 2002;23:241–243. doi: 10.1053/ejvs.2001.1552. [DOI] [PubMed] [Google Scholar]
- Bello TO, Taiwo SS, Oparinde DP, Hassan WO, Amure JO. Risk of nosocomial bacteria transmission: evaluation of cleaning methods of probes used for routine ultrasonography. West Afr J Med. 2005;24:167–170. doi: 10.4314/wajm.v24i2.28190. [DOI] [PubMed] [Google Scholar]
- Schabrun S, Chipchase L, Rickard H. Are therapeutic ultrasound units a potential vector for nosocomial infection? Physiother Res Int. 2006;11:61–71. doi: 10.1002/pri.329. [DOI] [PubMed] [Google Scholar]
- Schabrun S, Chipchase L. Healthcare equipment as a source of nosocomial infection: a systematic review. J Hosp Infect. 2006;63:239–245. doi: 10.1016/j.jhin.2005.10.013. [DOI] [PubMed] [Google Scholar]
- Rutala WA, Weber DJ. Disinfection and sterilization in health care facilities: what clinicians need to know. Clin Infect Dis. 2004;39:702–709. doi: 10.1086/423182. [DOI] [PubMed] [Google Scholar]
- Barbry T, Bouhemad B, Leleu K, de Castro V, Remerand F, Rouby JJ. Transthoracic ultrasound approach of thoracic aorta in critically ill patients with lung consolidation. J Crit Care. 2006;21:203–208. doi: 10.1016/j.jcrc.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Doelken P, Strange C. Chest ultrasound for "Dummies". Chest. 2003;123:332–333. doi: 10.1378/chest.123.2.332. [DOI] [PubMed] [Google Scholar]
- Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP, Gepner A, Goldstein I, Tenoudji-Cohen M. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231–1238. doi: 10.1097/01.CCM.0000164542.86954.B4. [DOI] [PubMed] [Google Scholar]
- Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby J-J, the CT Scan ARDS Study Group Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences on lung morphology. Intensive Care Med. 2000;26:857–869. doi: 10.1007/s001340051274. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Meziere G. A lung ultrasound sign allowing bedside distinction between pulmonary edema and COPD: the comet-tail artifact. Intensive Care Med. 1998;24:1331–1334. doi: 10.1007/s001340050771. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med. 1997;156:1640–1646. doi: 10.1164/ajrccm.156.5.96-07096. [DOI] [PubMed] [Google Scholar]
- Yang PC, Chang DB, Yu CJ, Lee YC, Kuo SH, Luh KT. Ultrasound guided percutaneous cutting biopsy for the diagnosis of pulmonary consolidations of unknown aetiology. Thorax. 1992;47:457–460. doi: 10.1136/thx.47.6.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg B, Diakoumakis EE, Kass EG, Seife B, Zvi ZB. The air bronchogram: sonographic demonstration. Am J Roentgenol. 1986;147:593–595. doi: 10.2214/ajr.147.3.593. [DOI] [PubMed] [Google Scholar]
- Yang PC, Luh KT, Chang DB, Yu CJ, Kuo SH, Wu HD. Ultra-sonographic evaluation of pulmonary consolidation. Am Rev Respir Dis. 1992;146:757–762. doi: 10.1164/ajrccm/146.3.757. [DOI] [PubMed] [Google Scholar]
- Yang PC, Luh KT, Lee YC, Chang DB, Yu CJ, Wu HD, Lee LN, Kuo SH. Lung abscesses: US examination and US-guided transthoracic aspiration. Radiology. 1991;180:171–175. doi: 10.1148/radiology.180.1.2052687. [DOI] [PubMed] [Google Scholar]
- Yu CJ, Yang PC, Chang DB, Luh KT. Diagnostic and therapeutic use of chest sonography: value in critically ill patients. Am J Roentgenol. 1992;159:695–701. doi: 10.2214/ajr.159.4.1529829. [DOI] [PubMed] [Google Scholar]
- Lichtenstein DA, Lascols N, Meziere G, Gepner A. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med. 2004;30:276–281. doi: 10.1007/s00134-003-2075-6. [DOI] [PubMed] [Google Scholar]
- Klein JS, Schultz S, Heffner JE. Interventional radiology of the chest: image-guided percutaneous drainage of pleural effusions, lung abscess, and pneumothorax [see comments] Am J Roentgenol. 1995;164:581–588. doi: 10.2214/ajr.164.3.7863875. [DOI] [PubMed] [Google Scholar]
- Gehmacher O, Mathis G, Kopf A, Scheier M. Ultrasound imaging of pneumonia. Ultrasound Med Biol. 1995;21:1119–1122. doi: 10.1016/0301-5629(95)02003-9. [DOI] [PubMed] [Google Scholar]
- Bouhemad B, Liu Z, Zhang M, Lu Q, Rouby JJ. Lung ultrasound detection of lung re-aeration in patients treated for ventilator-associated pneumonia [abstract] Intensive Care Med. 2006;32:S221. doi: 10.1007/s00134-006-0323-2. [DOI] [Google Scholar]
- Doust BD, Baum JK, Maklad NF, Doust VL. Ultrasonic evaluation of pleural opacities. Radiology. 1975;114:135–140. doi: 10.1148/114.1.135. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Hulot JS, Rabiller A, Tostivint I, Meziere G. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999;25:955–958. doi: 10.1007/s001340050988. [DOI] [PubMed] [Google Scholar]
- Joyner CR, Jr, Herman RJ, Reid JM. Reflected ultrasound in the detection and localization of pleural effusion. JAMA. 1967;200:399–402. doi: 10.1001/jama.200.5.399. [DOI] [PubMed] [Google Scholar]
- Gryminski J, Krakowka P, Lypacewicz G. The diagnosis of pleural effusion by ultrasonic and radiologic techniques. Chest. 1976;70:33–37. doi: 10.1378/chest.70.1.33. [DOI] [PubMed] [Google Scholar]
- Eibenberger KL, Dock WI, Ammann ME, Dorffner R, Hormann MF, Grabenwoger F. Quantification of pleural effusions:sonography versus radiography. Radiology. 1994;191:681–684. doi: 10.1148/radiology.191.3.8184046. [DOI] [PubMed] [Google Scholar]
- Roch A, Bojan M, Michelet P, Romain F, Bregeon F, Papazian L, Auffray JP. Usefulness of ultrasonography in predicting pleural effusions > 500 mL in patients receiving mechanical ventilation. Chest. 2005;127:224–232. doi: 10.1378/chest.127.1.224. [DOI] [PubMed] [Google Scholar]
- Vignon P, Chastagner C, Berkane V, Chardac E, Francois B, Normand S, Bonnivard M, Clavel M, Pichon N, Preux PM, et al. Quantitative assessment of pleural effusion in critically ill patients by means of ultrasonography. Crit Care Med. 2005;33:1757–1763. doi: 10.1097/01.CCM.0000171532.02639.08. [DOI] [PubMed] [Google Scholar]
- Balik M, Plasil P, Waldauf P, Pazout J, Fric M, Otahal M, Pachl J. Ultrasound estimation of volume of pleural fluid in mechanically ventilated patients. Intensive Care Med. 2006;32:318–321. doi: 10.1007/s00134-005-0024-2. [DOI] [PubMed] [Google Scholar]
- Remerand F, Dellamonica J, Mao Z, Rouby JJ. Direct bedside quantification of pleural effusion in ICU: a new sonographic method [abstract] Intensive Care Med. 2006;32:S220. [Google Scholar]
- Yang PC, Luh KT, Chang DB, Wu HD, Yu CJ, Kuo SH. Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. Am J Roentgenol. 1992;159:29–33. doi: 10.2214/ajr.159.1.1609716. [DOI] [PubMed] [Google Scholar]
- Mayo PH, Goltz HR, Tafreshi M, Doelken P. Safety of ultrasound-guided thoracentesis in patients receiving mechanical ventilation. Chest. 2004;125:1059–1062. doi: 10.1378/chest.125.3.1059. [DOI] [PubMed] [Google Scholar]
- Remerand F, Dellamonica J, Mao Z, Rouby JJ. Percutaneous chest tube insertions: is the" safe triangle" safe for the lung? Intensive Care Med. 2006;32:S43. [Google Scholar]
- Lichtenstein D, Meziere G, Biderman P, Gepner A. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25:383–388. doi: 10.1007/s001340050862. [DOI] [PubMed] [Google Scholar]
- Lichtenstein D, Meziere G, Biderman P, Gepner A. The "lung point": an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26:1434–1440. doi: 10.1007/s001340000627. [DOI] [PubMed] [Google Scholar]
- Wernecke K, Galanski M, Peters PE, Hansen J. Pneumothorax: evaluation by ultrasound – preliminary results. J Thorac Imaging. 1987;2:76–78. doi: 10.1097/00005382-198704000-00015. [DOI] [PubMed] [Google Scholar]
- Targhetta R, Bourgeois JM, Chavagneux R, Balmes P. Diagnosis of pneumothorax by ultrasound immediately after ultrasonically guided aspiration biopsy. Chest. 1992;101:855–856. doi: 10.1378/chest.101.3.855. [DOI] [PubMed] [Google Scholar]
- Targhetta R, Bourgeois JM, Chavagneux R, Coste E, Amy D, Balmes P, Pourcelot L. Ultrasonic signs of pneumothorax: preliminary work. J Clin Ultrasound. 1993;21:245–250. doi: 10.1002/jcu.1870210406. [DOI] [PubMed] [Google Scholar]
- Dulchavsky SA, Schwarz KL, Kirkpatrick AW, Billica RD, Williams DR, Diebel LN, Campbell MR, Sargysan AE, Hamilton DR. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma. 2001;50:201–205. doi: 10.1097/00005373-200102000-00003. [DOI] [PubMed] [Google Scholar]
- Liu DM, Forkheim K, Rowan K, Mawson JB, Kirkpatrick A, Nicolaou S. Utilization of ultrasound for the detection of pneumothorax in the neonatal special-care nursery. Pediatr Radiol. 2003;33:880–883. doi: 10.1007/s00247-003-0964-z. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, Hameed SM, Brown R, Simons R, Dulchavsky SA, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST) J Trauma. 2004;57:288–295. doi: 10.1097/01.ta.0000133565.88871.e4. [DOI] [PubMed] [Google Scholar]
- Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, Jiang GY. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10:R112. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An avi movie showing ultrasound pattern of normal lung: pleural line is a roughly horizontal hyperechoic line 0.5 cm below the upper and lower ribs identified by acoustic shadow. motionless and regularly spaced horizontal lines are seen below. They are meaningless and correspond to "artifacts of repetition".
An avi movie showing B lines 7 mm apart or spaced comet-tail artefacts. These spaced comet-tail artefacts arise from the pleural line and spread up to the edge of screen. These artefacts correspond to thickened interlobular septa at chest computed tomography scan.
An avi movie showing B lines 3 mm or less apart: contiguous comet-tails arising from the pleural line and spreading up to the edge of screen are present. These artefacts correspond to ground-glass areas on chest computed tomography scan.
An avi movie showing a cephalocaudal view of consolidated left lower lobe in and pleural effusion. Lung consolidation with air bronchograms, diaphragm and descending aorta are seen.
An avi movie showing a cephalocaudal view of consolidated left lower lobe with a peripheral abscess. The abscess appears as rounded hypoechoic lesions inside a lung consolidation.
An avi movie showing a massive pleural effusion enough to be compressive. the lung is seen consolidated and floating in this pleural effusion.
An avi movie showing a consolitated lung and adjacent pleural effusion with pleural adherences: the pleural effusion is abundant and the lung is seen consolidated and floating in the pleural effusion with pleural adherences.
An avi movie showing pneumothorax and "lung point". In a patient examined in the supine position with partial pneumothorax, normal lung sliding (left part of the screen) and pneumothoax (absence of lung sliding at right part of the screen) coexist. This boundary region is called the "lung point". It should be noted that lung sliding appears (coming from the left part of the screen) and disappears (absent lung sliding, horizontal lines only are visualised) with inspiration.


