Abstract
This study examines the relationship among neighborhood stressors, stress-buffering mechanisms, and likelihood of alcohol, drug, and mental health (ADM) disorders in adults from 60 US communities (n=12,716). Research shows that larger support structures may interact with individual support factors to affect mental health, but few studies have explored buffering effects of these neighborhood characteristics. We test a conceptual model that explores effects of neighborhood stressors and stress-buffering mechanisms on ADM disorders. Using Health Care for Communities with census and other data, we found a lower likelihood of disorders in neighborhoods with a greater presence of stress-buffering mechanisms. Higher neighborhood average household occupancy and churches per capita were associated with a lower likelihood of disorders. Cross-level interactions revealed that violence-exposed individuals in high crime neighborhoods are vulnerable to depressive/anxiety disorders. Likewise, individuals with low social support in neighborhoods with high social isolation (i.e., low average household occupancy) had a higher likelihood of disorders. If replicated by future studies using longitudinal data, our results have implications for policies and programs targeting neighborhoods to reduce ADM disorders.
Keywords: neighborhood effects, stress, social support, mental health, substance abuse, USA
Introduction
Although a growing body of evidence indicates that neighborhood characteristics are associated with prevalence of alcohol, drug, and mental health (ADM) conditions, research identifying mechanisms through which contextual effects operate is necessary to plan and develop health care systems that integrate aspects of place with service. “Neighborhood effects” research has focused on demonstrating how neighborhood disadvantage contributes to risk for ADM problems (Wheaton & Clarke 2003; Boardman, et al. 2001; Ross 2000; Aneshensel & Sucoff 1996; Weich, et al. 2003; Reijneveld & Schene 1998; Park & Nelson 1998). However, neighborhoods can also provide resources to support routine activity and facilitate social support, lowering risk for ADM conditions (Robert 1999; Heaney & Israel 2002).
Some research has shown that larger support structures may interact with individual supports to affect mental health (Lin, Ye, & Ensel 1999); few have explored effects of neighborhood characteristics and their stress-buffering effects for ADM disorders. In this paper, we test a conceptual model that explores effects of neighborhood stressors and stress-buffering mechanisms on ADM disorders. We use neighborhood-level data from US Census and other sources to develop neighborhood measures that parallel stress-buffering functions of individual social support and stress. We have two research questions. First, net of neighborhood economic context, what role do neighborhood stressors and stress-buffering mechanisms play in prevalence of ADM disorders? Second, does the impact of individual-level stress and social support on likelihood of ADM disorders differ depending on neighborhood stressors and stress-buffering mechanisms?
Neighborhood Context, Stress, and ADM conditions
Durkheim's studies of suicide (Durkheim 1951) began a long tradition of exploring the association between social environment and individual well-being. Faris & Dunham (1939) were the first to link “social disorganization” with schizophrenia and substance abuse at the neighborhood level, arguing that disorganized neighborhoods increased social isolation, as positive relationships were more difficult to develop and maintain. Within the life stress paradigm, the effects of social support and isolation on mental health have been recognized (Heaney & Israel 2002; Kawachi & Berkman 2001), and supportive resources have received much attention as stress mediators (Aneshensel 1992; Wenzel, et al. 2002). These studies emphasize that individuals are embedded within social structures that determine exposure to stress, stress mediators at their disposal, and perceptions of stress. This research focuses on functional social support as an individual characteristic, with family and friends as primary sources of social support.
Individual-level structural and functional dimensions of social support are fairly well developed and their effects on well-being, particularly the stress-buffering mechanism, have been explored. However, “supports” in the form of stress-buffering mechanisms at the neighborhood level remain under-explored. Although some have explored the protective effects of neighborhood “social capital” (Kawachi & Berkman 2000; Sampson, et al. 2002; van der Linden, et al. 2003), few quantitative national studies in the US have explored how presence of organizational resources and potential for social interaction provided by neighborhood context affects mental health.
Conceptual Framework
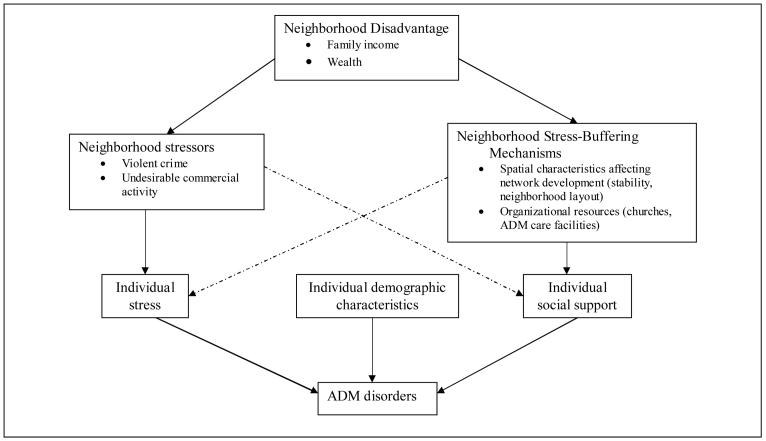
Figure 1 illustrates pathways through which neighborhood economic context may impact mental health, demonstrating hypothesized relationships among neighborhood economic context, stressors, and stress-buffering mechanisms. It acknowledges that individual demographics, stress, and social support affect likelihood of ADM disorders. Below we discuss relevant literature supporting our conceptual model. To summarize, neighborhood disadvantage operates through its effects on neighborhood stressors and stress-buffering mechanisms. These neighborhood factors may have actual consequences for likelihood of ADM disorders, but also shape perceptions of residents regarding sources of stress and social supports in their neighborhoods. The model illustrates the potential for cross-level interactions: neighborhood stressors may exacerbate effects of individual-level stressors, and neighborhood stress-buffering mechanisms may enhance the effect of individual social support on mental health status.
Figure 1.
Conceptual Model
Neighborhood Disadvantage
Literature on the relationship between neighborhood disadvantage and health points to at least two pathways through which economic context impacts mental health. Social disorganization theory posits that disadvantaged urban neighborhoods lack social and economic resources, predisposing them to high levels of physical and social disorder and low levels of informal social control (Sampson, et al. 1997). Low levels of trust and high levels of social isolation serve as barriers to collaborative efforts to reduce crime and other signs of neighborhood disorder (Ross, et al. 2001). First, the lack of trust discourages local network development that Lin et al. (1999) demonstrated is necessary for development of intimate ties that enhance social support. Second, residents perceive disadvantaged neighborhoods as dangerous, threatening, and stressful (Ross, et al. 2000). Stress from perceptions of the social environment is associated with higher levels of depression, anxiety, substance abuse, and psychological distress (Latkin & Curry 2003; Boardman, et al. 2001; Ross 2000; Aneshensel & Sucoff 1996).
Neighborhood Stressors
A number of studies have identified neighborhood crime, perceptions of crime, and violence as chronic stressors associated with higher prevalence of depression (Robinson & Keithley 2000; Powdthavee 2005; Chaix et al. 2006; Aneshensel & Sucoff 1996; Ross & Mirowsky 2001; Latkin & Curry 2003) and increased substance use and abuse (Boardman et al. 2001; Duncan, et al. 2002). Signs of neighborhood disorder such as public drinking/drug use, the presence of commercial operations such as bars, adult video stores, etc., and crime contribute to the perception of disadvantaged neighborhoods as threatening and dangerous.
Area crime rates can impact mental health by increasing the risk of victimization and by influencing residents' perceptions of their neighborhoods as dangerous. Although fear of crime varies due to factors unassociated with area crime rates (Pain 2001), individuals concerned about crime in their neighborhood may curtail their outdoor activities and isolate themselves, increasing risk of ADM disorders. Crime victims and those who witness crime have higher risk of experiencing PTSD, alcohol abuse, and other mental health disorders (Robinson & Keithley 2000). In addition, the effect of neighborhood crime rate on ADM disorders may differ depending on victimization status (Powdthavee 2005); in higher crime areas, the difference between victimized and non-victimized has been found to be smaller.
Several studies have demonstrated that alcohol availability is associated with alcohol-related community problems (drunk-driving, drunk-driving fatalities, and crime,) (Gruenewald, et al. 2002; Stockwell and Gruenewald 2001), and restricting local alcohol availability can reduced these problems (Treno & Lee 2002; Holder 2002; Dent, et al. 2005). Besides contributing to the perception of neighborhoods as stressful, alcohol availability is associated with neighborhood stress by increasing residents' actual risk of harmful consequences due to alcohol consumption (Gruenewald & Treno 2000).
Neighborhood Stress-Buffering Mechanisms
Underlying our conceptualization of neighborhood stress-buffering mechanisms is Lin et al.'s (1999) premise of “nested support systems” consisting of layers of structure upon which the stress-buffering function of social support depends. The outer layer of “community” determines potential for development of social networks, which in turn determines availability of social support, providing a protective function against psychological distress. We focus on two features of social environment that are associated with development of local social networks: neighborhood stability and spatial design. Social disorganization theory posits that residential stability fosters the development of trusting relationships and strong ties with neighbors (Sampson, et al. 2002). In addition, land use studies show that neighborhood design and housing distribution affect social interaction and development of “social capital” (Leyden 2003), and some have shown that design of multi-family dwellings can affect interaction patterns and feelings of social isolation (Evans, et al. 2003).
The wider neighborhood social environment can also provide support in the form of organizational resources to facilitate routine and non-routine activities (Robert 1999; Heaney & Israel 2002). As literature on stress-buffering effects of social support has demonstrated that personal resources can mediate effects of stress (Aneshensel 1992), neighborhood organizational resources available to residents in times of need may also serve a protective function against stress. In particular, churches and faith-based organizations are important community resources that provide spiritual counseling and social services (Chaves & Tsitsos 2001; Koenig, et al. 2001). Latkin & Curry (2003) found lower levels of depression among frequent church-goers, suggesting that churches are an important organizational resource for mental health needs. Availability of ADM services in the neighborhood may also affect prevalence, as utilization of services is associated with health sector behavioral care “social capital” (Hendryx & Ahern 2001).
Thus, neighborhood spatial features may impact individual mental health by facilitating social network development and influencing perceptions of greater social support among neighbors. In addition, neighborhood organizational resources may impact ADM disorder prevalence by providing sources of care for distressed individuals.
Hypotheses
We hypothesize that greater presence of neighborhood stressors will be associated with higher likelihood of disorder. Although neighborhood economic context can be a source of stress, and thus may be associated with a higher likelihood of disorder, we explore whether specific sources of stress, including violent crime and alcohol availability, mediate the effect of neighborhood economic context. In contrast, neighborhood stress-buffering mechanisms should be associated with lower likelihood of disorders.
We also test three sets of interaction effects. First, we hypothesize that individual violence exposure exacerbates stressful effects of neighborhood violent crime and alcohol availability. Second, we hypothesize that neighborhood stress-buffering mechanisms enhance the effects of individual-level social support. Finally, we hypothesize that individual social support and neighborhood stress-buffering mechanisms buffer effects of individual exposure to violence and neighborhood stressors.
Methods
Data
We used cross-sectional data from Healthcare for Communities (HCC) wave 2 telephone survey, supplemented with cases from wave 1. HCC was designed to track effects of the changing health care system on risk for ADM disorders. Both HCC waves were drawn from participants in the Community Tracking Study (CTS), a sequence of telephone surveys that focused on health care and health insurance coverage (Kemper, et al. 1996). The first HCC wave (1997-1998) sampled 14,985 individuals from the 30,375 respondents to the first CTS wave (1996-97); 9,585 completed interviews were obtained (64% response rate) (Sturm, et al. 1999). All HCC wave 1 participants were included in the wave 2 sampling frame, and 10,500 additional individuals were drawn from 39,504 respondents to CTS wave 2 (1998-99). 12,158 respondents completed HCC wave 2 (fielded during 2000-2001) for a response rate of 60.5%. In order to increase the sample size in addition to the wave 2 sample we included wave 1 data for 2926 HCC participants who were in the sampling frame for wave 2 but did not complete the survey. After eliminating HCC participants who lived outside of the 60 study communities and those with missing data, 12,716 cases remained. 1176 cases were excluded due to missing data, primarily resulting from a large number of missing values for violent crime arrests (943 missing).
Our data on neighborhood stressors and structural supports were derived from the 2000 US Census, FBI Uniform Crime Reports, and InfoUSA. “Neighborhood” characteristics were measured at the level of Census tract, zip code, or county. Wherever possible we use data for the smallest geographic entity to more accurately represent neighborhood characteristics (Hillemeier, et al. 2003).
Dependent Variables
Focusing on one outcome might result in the conclusion that some individuals are not affected by stress, when in fact they react differently. For this reason, we use a broad indicator of any ADM disorders (0=no disorder, 1=one or more disorders) in the prior 12 months, constructed from ADM screening items as well as measures of perceived need for care. Probable major depression, dysthymia, generalized anxiety disorder, and lifetime mania were based on DSM-III criteria and assessed using the Composite International Diagnostic Interview short form (CIDI-SF) (Kessler, et al. 1998). The CIDI screener for probable panic disorder was modified to reduce false-positives by requiring limitation in social or role functioning using 2 items from the 12-Item Short-Form Health Survey and 3 items from the Sickness Impact Profile (Ware, et al. 1996). Probable illicit drug use was assessed using items from the CIDI 2.1 (WHO 1997). Lifetime psychosis was assessed by asking if respondents had ever stayed overnight in hospital for psychotic symptoms. Probable schizophrenia was assessed by asking respondents if they ever had a diagnosis of schizophrenia or schizoaffective disorder. Probable alcohol abuse was assessed with the Alcohol Use Disorders Identification Test (AUDIT) (WHO 2001). Perceived need for care was based on two survey items asking respondents if in the past 12 months they felt they needed help for an emotional/mental health problem (“such as feeling sad, blue, anxious or nervous?”) or an alcohol/drug problem. The survey items used to derive the outcome variables can be found at http://www.hsrcenter.ucla.edu/research/hcc.shtml.
Using a broad indicator of any ADM disorders assumes that the pathway is the same regardless of type of disorder. To explore whether neighborhood characteristics have different effects on different ADM disorders, we estimated separate models for indicators of probable depressive or anxiety disorder and probable alcohol abuse or illicit drug use within 12 months.
Neighborhood economic context
We include median family income and percent of owner occupied units, measured continuously at the Census tract level (US Census Bureau 2000). These measures parallel individual measures of SES included in the model, representing economic stability (income) and wealth (home ownership).
Neighborhood stressors
Based on research demonstrating the importance of crime and violence to perceptions of neighborhood stress, we include an indicator for violent crime arrest rate measured at the county level, scored as 1 for counties with violent crime arrests of 300 or more per 100,000 capita (approximately the 75th percentile of our sample distribution), 0 otherwise (Uniform Crime Reporting Program 2000). Because jurisdictions that do not provide any data may appear to have an arrest rate of 0, we eliminate from the analyses all counties (and individuals in those counties) with a coverage indicator of 0 and that did not report any arrests for the year. Alcohol availability was derived from ZIP Code Business Patterns data from US Census Bureau and US Dept. of Commerce (2001) as the number of stores and bars selling alcohol (not including restaurants) per 100,000 population.
Neighborhood Stress-Buffering Mechanisms
We include two measures of organizational resources that may perform a stress-buffering function by providing supportive resources for routine and non-routine activities. Per capita ADM care facilities was derived from ZIP Code Business Patterns data as the sum of inpatient and outpatient mental health and substance abuse facilities per 100,000 population, including physicians who specialize in mental health, other mental health practitioners, psychiatric and substance abuse hospitals, other specialty mental health hospitals, and residential mental health and substance abuse facilities. We also include number of churches per 1,000 capita, measured at the county level (InfoUSA 2003).
Average household occupancy from US Census was derived by dividing number of persons per square mile by number of occupied housing units per square mile (US Census 2000). This variable provides a measure of how people are distributed among housing units in a neighborhood (i.e., whether on average a neighborhood is composed primarily of people who live alone), capturing the potential for neighborhood social interaction and availability of social support. To capture neighborhood stability, the median number of years a householder has lived in the unit was derived from Census tract level data.
Table 1 contains a correlation matrix of neighborhood characteristics.
Table 1.
Correlation matrix of neighborhood-level characteristics.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Median family income | .577*** | −134*** | −.095*** | −.400*** | .126*** | .133*** | .179*** | |
| 2. Percent of units owner-occupied | −.251*** | −236*** | .013 | −.200*** | .194*** | .509*** | ||
| 3. Availability of alcohol | .152*** | −.165*** | .340*** | −.105*** | −.133*** | |||
| 4. Violent crimes per 100,000 pop. | −.014 | .099*** | −.011 | −.041*** | ||||
| 5. Churches per 1,000 pop. | −.179*** | −.144*** | .056*** | |||||
| 6. Number of ADM care facilities | −.154*** | −.123*** | ||||||
| 7. Household occupancy | .080*** | |||||||
| 8. Number of years lived in residence |
Individual Characteristics
As measures of stressors and stress-buffering factors, we use personal exposure to violence and social support. Violence exposure was indicated by an affirmative response to the question: “During the past 12 months, did any of the following things happen to you . . . You saw or witnessed someone being beaten, abused, or killed.” Social support was calculated as the average of 6 items used in the Medical Outcomes Study, each measured on a 6-point scale with 6=all of the time and 1=none of the time (Sherbourne & Stewart 1991). The items measured how often forms of support are available: 1) someone to help with daily chores if you were sick; 2) someone to love and make you feel wanted; 3) someone to confide in or talk to about yourself or your problems; 4) someone to have a good time with; 5) someone to give you information to help you understand a situation; and 6) someone to give you money if you needed it.
Other individual-level covariates include race/ethnicity (white, black, Hispanic, other), education (less than high school, high school graduate, college graduate), gender, married or living as married, and age in years. Log of family savings (stocks, bonds, and other capital assets) and family income were measured continuously. Family savings represents resources available for individuals to draw upon in times of crisis, while total family income represents continuous income stream used to sustain lifestyle. In addition, we tested interactions between social support and gender, age, and financial resources to examine whether social support mediates effects of these characteristics, as has been found in previous research (Kawachi & Berkman 2001). Only interactions with gender and age were statistically significant, and are included in models in which a significant effect was found.
Table 2 contains descriptive statistics for all individual characteristics used in the analysis.
Table 2.
Characteristics (unweighted) of Adults in the HCC Cross-sectional Sample (n=12716)
| Individual-level Characteristics | Percentage or Mean (s.d.) |
|---|---|
| Female | 60.9% |
| Education | |
| Less than high school diploma | 12.6% |
| Graduated high school | 60.0% |
| College graduate or more | 27.4% |
| Race/Ethnicity | |
| White | 77.4% |
| Black | 11.9% |
| Hispanic | 7.0% |
| Other | 3.7% |
| Married or living as married | 63.2% |
| Age | 47.5 yrs (sd=16.5 yrs) |
| Family savings | $86,605 (sd=$425,381) |
| Total family income in the past 12 months | $53,490 (sd=$56,913) |
| Witnessed a beating, abuse or murder in past 12 months | 3.3% |
| Social support | 4.74 (sd=1.2) |
| Any ADM disorders in prior 12 months | 30.6% |
| Probable anxiety or Depressive disorder in prior 12 months | 17.5% |
| Alcohol abuse or illicit drug use in prior 12 months | 7.6% |
Analysis
Using the software package MLwiN (Bryk & Raudenbush 1992; Rasbash, et al. 2003), separate hierarchical models with random intercepts were estimated for three outcomes, with counties as Level-4 units (n=493), Census tracts as Level-3 units (n=6698), households as Level-2 units (n=10457), and individuals as Level-1 units (n=12716). First, we estimated a baseline model that included neighborhood economic context variables and individual-level predictors to determine if neighborhood SES has any significant effect above and beyond individual characteristics. We then entered neighborhood stressors and stress-buffering mechanisms in separate blocks to explore effects of each block independently. To estimate the relative effects of each block of variables, the final model included all individual and neighborhood characteristics. In all models, continuous variables were centered at their grand means in order to provide a point of comparison for interpretation. Sensitivity analyses of models estimated for men and women separately found no substantively important differences.
The HCC sample used a complex sampling design with a multistage sample of sites, households, and individuals. We used unweighted multilevel models that incorporated design variables and predictors of survey nonresponse as fixed effects to mitigate the impact of an informative sampling design (Pfeffermann & LaVange 1989). In addition, we used extended hot deck multiple imputation that modifies the predictive mean matching method to impute missing items (Little 1988). Data for family savings, family income, social support, probable depressive/anxiety disorder in prior 12 months were imputed. The results across 5 imputed data sets were combined by averaging, and standard errors were adjusted to reflect within- and between-imputation variability (Rubin 1987).
To explore buffering effects of social support, in the presence of significant main effects we tested the interaction of neighborhood stressor and stress-buffering variables with individual social support and violence exposure. Only interactions between average neighborhood household occupancy and individual social support and between neighborhood violent crime and individual violence exposure were significant, and were included in the models presented. To facilitate interpretation of significant cross-level interaction effects, we calculated standardized predictions using the observed value of all predictors except for the individual-level variable of interest. Separate predictions were calculated for each individual, for each value of the variable of interest. Predictions were then averaged across individuals for a given value on the variable of interest.
Results
Any Alcohol, Drug, or Mental Health (ADM) Disorders
Model 1 (Table 3) shows that with all individual-level variables in the model, neighborhood economic context was not significantly associated with likelihood of any ADM disorder. Non-whites, married, and individuals with more family savings had lower likelihoods of ADM disorders, while having less than high school education increased likelihood. Likelihood of ADM disorders decreased with age and higher social support. The significant interaction terms for social support by age and social support by gender suggest that the effect of social support was stronger for older people and females. Individuals who witnessed violence had more than twice the odds of having any ADM disorder.
Table 3.
Odds Ratios for Individual and Community Factors on ADM Outcomes
| Any ADM disorder |
Anxiety/ Depression |
Substance Abuse |
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 4 | Model 4 | |
| Individual characteristics | ||||||
|
Education (ref. grp.: completed college) |
||||||
| Graduated high school | 1.062 | 1.069 | 1.065 | 1.069 | 1.370* | 1.282** |
| Less than high school diploma | 1.262** | 1.311** | 1.286** | 1.324** | 1.718* | 1.446** |
| Race/Ethnicity (ref. grp.: White) | ||||||
| Black | 0.758* | 0.800** | 0.802** | 0.836* | 0.840* | 0.819 |
| Hispanic | 0.755* | 0.740** | 0.802* | 0.784** | 0.752** | 1.052 |
| Other | 0.689** | 0.687** | 0.689** | 0.693** | 0.807 | 0.422* |
| Female | 0.930 | 0.942 | 0.934 | 0.940 | 1.283* | 0.316* |
| Married or living as married | 0.856** | 0.861** | 0.874** | 0.874** | 1.058 | 0.674* |
| Age | 0.979* | 0.978* | 0.978* | 0.978* | 0.986* | 0.964* |
| Family income, log transformed | 1.001 | 1.005 | 1.000 | 1.004 | 0.998 | 1.046 |
| Family savings, log transformed | 0.971* | 0.972* | 0.971* | 0.972* | 0.960* | 0.981 |
| Social Support | 0.753* | 0.755* | 0.751* | 0.754* | 0.702* | 0.887* |
| Social support*Age | 1.002* | 1.002 | 1.002* | 1.002 | ||
| Social support*Female | 0.903** | 0.896** | 0.902** | 0.896** | ||
| Witnessed a beating, etc. past 12 mon. |
2.193* | 2.002* | 2.177* | 2.245* | 1.640* | 2.490* |
| Neighborhood Economic Context | F(2,536) =0.65 | F(2,491) =1.13 | F(2,518) =0.41 | F(2,490) =0.27 | F(2,490) =3.13* | F(2,490) =3.24* |
| Neighborhood median family income |
1.000 | 1.000 | 1.000 | 1.000 | 1.000* | 1.000* |
| Percent owner occupied units | 0.999 | 0.998 | 1.001 | 1.000 | 1.003 | 0.995 |
| Neighborhood stressors | F(3,491) =2.77* | F(2,490) =2.65† | F(3,490) =2.41 | F(2,490) =0.17 | ||
| 300+ violent crime arrests/100k pop. |
0.854* | 0.883* | 0.879 | 0.950 | ||
| Witnessed beating*violent arrests | 1.620 | 1.879* | ||||
| Number of bars, liquor stores, etc. | 1.000 | 1.000 | 1.000 | 1.000 | ||
|
Neighborhood Stress-Buffering Mechanisms |
F(5,518) =5.48* | F(5,490) =5.32* | F(4,490) =0.51 | F(5,490) =3.00* | ||
| Number of churches per 1k population |
0.929* | 0.926* | 0.979 | 0.911 | ||
| Number of IP/OP ADM facilities | 0.999 | 0.999 | 1.000 | 0.998 | ||
| Average housing occupancy | 0.867** | 0.877** | 0.952 | 0.860 | ||
| Social support housing occupancy | 1.136* | 1.148* | 1.202** | |||
| Median years occupied residence | 0.992 | 0.994 | 0.989 | 1.006 | ||
| Household Level Error Variance | 0.088 | 0.127 | 0.087 | 0.131 | 0.000* | 0.000* |
| Tract Level Error Variance | 0.126* | 0.087 | 0.129* | 0.087 | 0.138* | 0.233* |
| County Fips Level Error Variance | 0.015 | 0.012 | 0.009 | 0.008 | 0.009 | 0.002 |
Note: All continuously measured variables were centered at their grand mean for analysis
P<0.10; p<0.05
p<0.01
p<0.001 (two-tailed tests)
An indicator for violent crime arrests, an interaction for individual exposure to violence with the arrest indicator, and availability of alcohol were added in Model 2 to assess the effects of neighborhood stressors. The effect for violent crime arrests was negative and significant, but the interaction term was not, suggesting that living in a high violent crime area did not compound the effect of individual violence exposure. Alcohol availability was not significant. A group significance test of the combined effect of neighborhood stressors was significant.
Model 3 considered effects of neighborhood stress-buffering mechanisms and the interaction between average household occupancy and individual social support on any ADM disorders. Higher average neighborhood household occupancy was associated with lower likelihood of disorders, partially supporting our hypothesis that neighborhood stress-buffering mechanisms are associated with lower likelihood of disorder. Furthermore, the interaction of social support and average household occupancy was significant, indicating that the effect of average household occupancy differs depending on social support. In addition, more churches per capita was significantly associated with lower likelihood of disorder. A significance test of the combined effect of neighborhood structural support variables was significant.
Model 4 contains all individual-level variables, neighborhood stressors and stress-buffering mechanisms, and significant interaction terms. The main findings demonstrated above hold when all predictors and significant interactions are included, and the magnitude of the effects does not change dramatically. A group significance test of neighborhood stress-buffering mechanisms remained significant, but the combined effect of stressors was not. Interactions between social support and neighborhood stressors were not significant, nor were interactions of violence exposure and neighborhood stress-buffering mechanisms. We found no evidence to support our hypothesis that individual and neighborhood stress-buffering mechanisms protect against effects of stress from violence exposure, neighborhood violent crime, or alcohol availability.
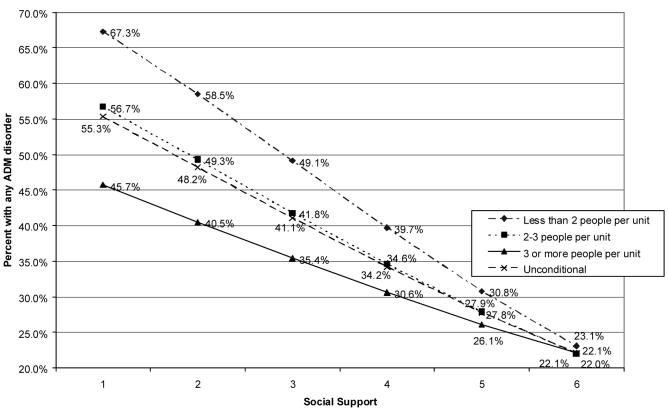
Based on Model 4 parameters, standardized predictions in Figure 2 indicate that regardless of neighborhood household occupancy rates, a higher level of social support is associated with a lower probability of ADM disorders. However, among those with lower levels of social support, lower household occupancy levels are associated with higher probability of ADM disorders, compared with residents of higher household occupancy neighborhoods.
Figure 2.
Standardized prediction for probability of any ADM disorder as a function of social support, by average household occupancy
Probable Anxiety or Depressive Disorders
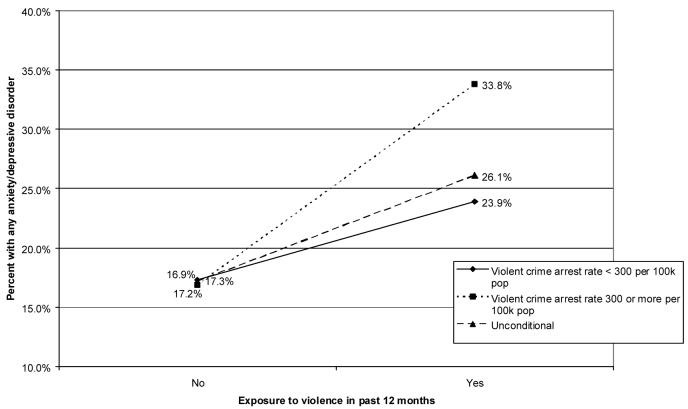
Similar patterns were found in models for depressive/anxiety disorders (Table 3) but in the full model, females were more likely to have probable depressive/anxiety disorders. We also found a significant effect for neighborhood median family income, indicating that individuals in higher income neighborhoods were less likely to experience these disorders. A group test of neighborhood disadvantage variables was significant. Model 2 (not shown) examining effects of neighborhood stressors revealed a significant negative effect for neighborhood violent crime and a positive effect for the interaction of neighborhood crime and violence exposure. However, in the full model (Model 4, Table 3), only the interaction remained significant. The group test of neighborhood stressors was not significant. None of the neighborhood stress-buffering mechanisms were significant in Model 3 (not shown) or Model 4 (Table 3), and a group test of neighborhood stress-buffering mechanisms was not significant. Standardized predictions for the interaction of violent crime with violence exposure (Figure 3) illustrate that individuals who live in high crime areas and have violence exposure are more likely to experience depressive/anxiety disorders, compared with their counterparts living in lower crime areas; for those with no violence exposure, neighborhood crime is not associated with higher rates of disorder.
Figure 3.
Standardized predictions for any Anxiety/Depressive disorder, controlling for exposure to violence, by violent crime arrest rate level
It appears that neighborhood stressors operate similarly in predicting probable depressive/anxiety disorders and any ADM disorders. This is not true for neighborhood stress-buffering mechanisms. The findings for females and neighborhood economic context demonstrate that the effect of these characteristics on the likelihood of depressive/anxiety disorders is different, from their effect on any ADM disorders.
Probable alcohol or substance abuse disorder
Model 4 (full model) for probable alcohol/substance abuse disorders appear in Table 3. Blacks and Hispanics were as likely as whites to have probable alcohol/substance abuse, and females were less likely than males to have such disorders. As with depressive/anxiety disorders, we found small yet significant effects for neighborhood median family income. However, the group significance test for neighborhood economic context was not significant. None of the neighborhood stressors were significant in Model 2 (not shown) or Model 4 and group tests of their effects were not significant. For neighborhood stress-buffering mechanisms, only the interaction between neighborhood average household occupancy and social support was significant. The group significance test of their combined effect was significant. The effect of neighborhood household occupancy was similar to the model for any ADM disorders, suggesting that social support is more important for reducing substance abuse in neighborhoods with very low household occupancy levels. For example, in such neighborhoods, the standardized predictions (Figure 4) indicate that substance abuse varies from 20.8% with social support=1 to 7.0% in the highest social support group.
Figure 4.
Standardized predictions for alcohol/substance abuse disorders as a function of social support, by average household occupancy
The results for alcohol/substance abuse demonstrate that individual and neighborhood characteristics affect likelihood of substance abuse disorders differently, as compared with any ADM disorders or probable depressive/anxiety disorders. In addition, the results provide support for our hypothesis that neighborhood stress-buffering mechanisms are associated with lower likelihood of substance abuse disorders, but this effect is moderated by individual-level social support.
Conclusions
Building on previous research that points to physical and structural characteristics of disadvantaged neighborhoods as sources of stress (Boardman et al. 2001; Robert 1999), we found evidence that one neighborhood stressor (high violent crime) is associated with worse mental health outcomes, above and beyond effects of neighborhood economic context. In contrast to studies suggesting that signs of public drinking and alcohol-related problems are sources of stress, alcohol availability was not associated with our outcomes. We believe that neighborhood crime operates to influence perceptions of neighborhoods as dangerous, threatening, or stressful and by increasing residents' risk of being a victim of crime. In turn, these increased risks and negative perceptions are associated with ADM disorders.
Studies of stress suggest that social support and personal resources have positive effects on health and mental health (Kawachi & Berkman 2001). Our results expand on this finding to demonstrate that neighborhood stress-buffering mechanisms, particularly neighborhood housing distribution characteristics and organizational resources such as churches, are associated with a lower likelihood of any ADM disorders. Moreover, these effects remain significant when neighborhood economic context and stressors are included, and may reduce effects of neighborhood stressors, as indicated by the non-significant group test of neighborhood stressors in Model 4. We believe that these factors operate by affecting network development among neighbors, perceptions of social support in the neighborhood, and by providing resources to alleviate psychological distress.
We also explored whether neighborhood characteristics interact with individual-level characteristics to compound or buffer their effects. Our results demonstrate that high neighborhood violent crime amplifies the negative effect of violence exposure. Our results expand on the literature (Kawachi & Berkman 2001) by demonstrating that neighborhood stress-buffering mechanisms may also interact with individual-level functional social support to protect against social isolation. However, we did not find that neighborhood stress-buffering mechanisms protect against effects of individual trauma (i.e., violence exposure). Based on these findings and results of previous research, we believe that higher household occupancy rates may contribute to better ADM outcomes by creating more opportunities for social interaction, particularly for those who lack social support, and encouraging the development of social ties among neighbors. However, our results suggest that neighborhood stability (median years lived in unit) may not be as important for social interaction and development of networks as has been suggested by social disorganization theory.
Even after controlling for neighborhood stressors, a significant effect remained for some neighborhood economic context variables on two outcomes. The result for depressive/anxiety disorders confirms results of previous studies that demonstrated no or a negative effect on likelihood. Likewise, although counter to what social disorganization theory suggests, the positive association between neighborhood income and likelihood of alcohol/substance abuse disorders has also been found by Ennett, et al. (1997). Compared with lower income areas, individuals in higher income neighborhoods may have more discretionary income with which to purchase “luxury” items such as alcohol and other illicit substances. Alternatively, although the model did include design variables that should account for non-response, these results could reflect either response or reporting bias (for example, people living in low income neighborhoods may be less likely to report substance abuse problems, or low income people with substance abuse problems may be more difficult to contact by telephone).
Finally, we caution readers to consider the following methodological issues. First, the response rate for HCC is relatively low. Although our models include design variables to account for oversampling and higher likelihood of attrition, and we adjust for individual-level characteristics that may be related to attrition, our results should not be considered conclusive. These analyses should be replicated using other nationally representative samples of adults before firm conclusions are drawn about the relationship between neighborhood characteristics and ADM disorders.
The second, and potentially most serious issue, is the possibility of selection effects. Others have cautioned that people with ADM disorders may choose or be forced as a result of circumstances to live in disadvantaged neighborhoods that not only lack stress-buffering mechanisms, but also have more environmental stressors. Less plausible but still a consideration is the possibility that migration of people with ADM disorders to certain neighborhoods actually causes neighborhood deterioration. Adjusting for individual socioeconomic characteristics, as our analyses do, should at least partially offset the effect of selection processes. In sensitivity analysis (not reported; contact first author for full results), we used the longitudinal component of HCC to investigate the possibility of selection effects.1 We explored whether people with ADM disorders were more likely to move, and whether movers with ADM disorders were more likely to move to worse neighborhoods. Our exploration found no evidence in support of selection effects due to ADM disorders. Other potential mechanisms, such as individual socioeconomic characteristics, should be explored in future research.
Another issue common to neighborhood effects research is how contextual effects may vary as a result of geographic conceptualization (Sampson, et al. 2002; Pickett & Pearl 2001; Robert 1999). Neighborhood effects research is limited to the extent that the geographic “neighborhood” is defined by the entity that collects data on neighborhood characteristics. Thus, the neighborhood as operationalized may not correspond closely with the geographic area considered “the neighborhood” by its residents, making it more difficult to find neighborhood effects. One study that explored the differences due to size of geographic areas found almost no difference in the size of health differences by area characteristics when using larger versus smaller area definitions (Reijneveld, et al. 2000). Nevertheless, because where boundaries are drawn is just as important as size of the geographic area considered “neighborhood”, we used data for the smallest geographic unit available, i.e., the Census tract, whenever possible. However, data on crime, churches per capita, and some of our neighborhood variables were not available at the Census tract level. We thus used data that was measured at the zip code and the county levels. Both ZIP codes and counties cover diverse areas, especially urban ones, that vary widely within each unit in terms of their size and the geographic level variables used here, since their boundaries are not drawn to create sociodemographically homogenous areas as are census tracts. This may have resulted in weaker effects than would have otherwise been found if boundaries were drawn to reflect “neighborhoods”. Future research on neighborhood effects should consider employing spatial techniques, such as hierarchical geostatistical modeling (Chaix et al. 2006) that rely less on artificially imposed neighborhood boundaries and take into account characteristics of proximate neighborhoods.
A few other limitations should also be considered. First, crime rates may be biased towards underreporting because reporting jurisdictions don't provide complete reports and individuals don't report crimes. We addressed the first of these by eliminating jurisdictions that did not report crimes; however our results are vulnerable to underreporting by individuals. As a consequence, the relationship between crime rate and ADM disorders may be weaker than what would be expected with complete reporting. In addition, since we do not have a measure of congregation size or church attendance, number of churches per capita can only be considered a proxy variable for stress-buffering supports from religious institutions, and a stronger relationship may have been discovered if we had a more direct measure of contact with communities of faith. The number of ADM facilities in neighborhoods may be a poor approximation of access to care, given that health care coverage is not universal in the US. Finally, individuals with ADM disorders may be more likely to have negative perceptions of their neighborhoods, may be more sensitive to variations in neighborhood characteristics, and/or more vulnerable to neighborhood stressors. For example, some research has found that individuals with SMI are more likely to be victimized (Teplin et al. 2005), which may account for the association between neighborhood characteristics and mental health. We used crime rates rather than fear of crime, which minimizes the risk of reverse causation.
Until our results are replicated with longitudinal data for neighborhood characteristics, they should be considered suggestive, rather than conclusive, evidence of a causal relationship. If replicated by future studies using longitudinal data, our results have implications for policies and programs targeting neighborhoods. First, our findings suggest that interventions targeting violence-exposed persons in high crime neighborhoods may reduce depressive/anxiety disorders. In fact, one program in Los Angeles, CA to address the consequences of violence exposure among school-aged children is showing promising preliminary results (Stein et al. 2003; Kataoka et al. 2003). In addition, our findings suggest that neighborhoods and housing can be designed to increase opportunities for social interaction and network development among neighbors, and this may be particularly important for people who lack social support. Some researchers examining the link between housing and health have suggested that housing guidelines and codes that encourage more social interaction should be developed and implemented (Kreiger & Higgins 2002; Ahrentzen 2003).
Acknowledgments
The authors would like to acknowledge and thank the following people for their contributions to the conceptualization of the analysis variables, technical assistance, and helpful comments: Ruth Klap, Roland Sturm, and Diana Liao. This research was supported by grants from the Robert Wood Johnson Foundation (038273), the National Institute of Mental Health (P30MH068639:01), and the National Institute of Environmental Health Sciences (P50ES012383)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Unfortunately, the longitudinal component of HCC (n=6659) could not be used for the analysis of neighborhood effects due to the lack of neighborhood data. The data waves of HCC were collected in 1997-98 and 2000-2001. Since most of our neighborhood variables were constructed from Census data, and Census data are only collected every 10 years, we would have to use Census data from 2000 to construct neighborhood data for both waves. Thus, the neighborhood measures would not reflect changes in neighborhood characteristics.
Contributor Information
Dr. Susan E. Stockdale, UCLA Los Angeles, CA UNITED STATES, sstockdale@mednet.ucla.edu
Kenneth B. Wells, UCLA Semel Institute Health Service Research Center and the RAND Corp., kwells@ucla.edu
Lingqi Tang, UCLA Semel Institute Health Services Research Center, lqtang@ucla.edu
Thomas R. Belin, UCLA Biostatistics Department, tbelin@ucla.edu
Lily Zhang, UCLA Semel Institute Health Services Research Center, lizhang@ucla.edu
Cathy D. Sherbourne, RAND Corp., cathyd@rand.org
References
- Ahrentzen S. Double indemnity or double delight? The health consequences of shared housing and ‘doubling up’. Journal of Social Issues. 2003;59:547–568. [Google Scholar]
- Aneshensel CS. Social stress: theory and research. Annual Review of Sociology. 1992;18:15–38. [Google Scholar]
- Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. Journal of Health and Social Behavior. 1996;37:293–310. [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health & Social Behavior. 2001;42(2):151–165. [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models. Sage Publications; Newbury Park, CA: 1992. [Google Scholar]
- Chaix B, Leyland AH, Sabel CE, Chauvin P, Rastam L, Kristersson H, Merlo J. Spatial clustering of mental disorders and associated characteristics of the neighbourhood context in Malmo, Sweden, in 2001. Journal of Epidemiology and Community Health. 2006;60:427–435. doi: 10.1136/jech.2005.040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaves M, Tsitsos W. Congregations and social services: what they do, how they do it, and with whom? Nonprofit & Voluntary Sector Quarterly. 2001;30(4):660–683. [Google Scholar]
- Dent CW, Grube JW, Biglan A. Community level alcohol availability and enforcement of possession laws as predictors of youth drinking. Preventive Medicine. 2005;40(3):355–362. doi: 10.1016/j.ypmed.2004.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prevention Science. 2002;3(2):125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- Durkheim E. Suicide. The Free Press; New York, NY: 1951. [Google Scholar]
- Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. Journal of Health and Social Behavior. 1997;38(1):55–71. [PubMed] [Google Scholar]
- Evans GW, Wells NM, Moch A. Housing and mental health: A review of the evidence and a methodological and conceptual critique. Journal of Social Issues. 2003;59(3):475–500. [Google Scholar]
- Faris RE, Dunham HW. Mental Disorders in Urban Areas: An Ecological Study of Schizophrenia and Other Psychoses. University of Chicago Press; Chicago: 1939. [Google Scholar]
- Gruenewald PJ, Remer L, Lipton R. Evaluating the alcohol environment: community geography and alcohol problems. National Institute on Alcohol Abuse and Alcoholism; Bethesda, Maryland: 2002. [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Treno AJ. Local and global alcohol supply: economic and geographic models of community systems. Addiction. 2000;95(4):S537–S549. doi: 10.1080/09652140020013764. [DOI] [PubMed] [Google Scholar]
- Heaney CA, Israel BA. Social Networks and Social Support. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory research and practice. Jossey-Bass; San Francisco, CA: 2002. pp. 185–209. [Google Scholar]
- Hendryx MS, Ahern MM. Access to mental health services and health sector social capital. Administration and Policy in Mental Health. 2001;28(3):205–218. doi: 10.1023/a:1007860002137. [DOI] [PubMed] [Google Scholar]
- Hillemeier MM, Lynch J, Harper S, Casper M. Measuring contextual characteristics for community health. Health Services Research. 2003;38(6):1645–1718. doi: 10.1111/j.1475-6773.2003.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder HD. Prevention of alcohol and drug ‘abuse’ problems at the community level: what research tells us. Substance Use & Misuse. 2002;37(810):901–921. doi: 10.1081/ja-120004158. [DOI] [PubMed] [Google Scholar]
- InfoUSA Database of the number of churches by county in the US. 2003 October 1; obtained from InfoUSA at www.infousa.com.
- Kataoka SH, Stein BD, Jaycox LH, Wong M, Escudero P, Tu W, Zaragoza C, Fink A. A school-based mental health program for traumatized Latino immigrant children. Journal of the Academy of Child and Adolescent Psychiatry. 2003;42:311–318. doi: 10.1097/00004583-200303000-00011. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social cohesion, social capital, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. pp. 174–190. [Google Scholar]
- Kemper P, Blumenthal D, Corrigan JM, Cunningham PJ, Felt SM, Grossman JM, Kohn LT, Metcalf CE, Peter RF, Strouse RC, Ginsburg PB. The design of the Community Tracking Study: A longitudinal study of health system change and its effects on people. Inquiry. 1996;33(2):195–206. [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7(4):171–85. [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. Oxford University Press; New York, NY: 2001. [Google Scholar]
- Krieger J, Higgins DL. Housing and health: time again for public health action. American Journal of Public Health. 2002;92(5):758–68. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. Journal of Health & Social Behavior. 2003;44:34–44. [PubMed] [Google Scholar]
- Leyden KM. Social capital and the built environment: The importance of walkable neighborhoods. American Journal of Public Health. 2003;93(9):1546–1551. doi: 10.2105/ajph.93.9.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin N, Ye X, Ensel WM. Social support and depressed mood: A structural analysis. Journal of Health & Social Behavior. 1999;40:344–359. [PubMed] [Google Scholar]
- Little RJ. Missing data adjustments in large surveys. Journal of Business and Economic Statistics. 1988;6:287–301. [Google Scholar]
- Pain R. Gender, race, age and fear in the city. Urban Studies. 2001;38(56):899–913. [Google Scholar]
- Park J, Nelson CH. The investigation of stress in resource-dependent communities: the effect of rapid socioeconomic changes on mental health service use. International Journal of Circumpolar Health. 1998;57(Suppl 1):432–38. [PubMed] [Google Scholar]
- Pfeffermann D, LaVange L. Regression models for stratified multi-stage cluster samples. In: Skinner CJ, Holt D, Smith TMF, editors. Analysis of Complex Surveys. John Wiley & Sons; New York, NY: 1989. [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology and Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powdthavee N. Unhappiness and crime: evidence from South Africa. Economica. 2005;72:531–547. [Google Scholar]
- Rasbash J, Steele F, Browne W. A User's Guide to MLwiN. Centre for Multilevel Modeling; London, England: 2003. [Google Scholar]
- Reijneveld S, Schene AH. Higher prevalence of mental disorders in socioeconomically deprived urban areas in the Netherlands: community or personal disadvantage? Journal of Epidemiology and Community Health. 1998;52:2–7. doi: 10.1136/jech.52.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reijneveld SA, Verheij RA, de Bakker DH. The impact of area deprivation on differences in health: does the choice of geographical classification matter? Journal of Epidemiology and Community Health. 2000;54:306–313. doi: 10.1136/jech.54.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- Robinson F, Keithley J. The impacts of crime on health and health services: a literature review. Health, Risk, & Society. 2000;2(3):253–266. [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior. 2000;41(2):177–87. [PubMed] [Google Scholar]
- Ross CE, Mirowsky J, Pribesh S. Powerlessness and the amplification of threat: neighborhood disadvantage, disorder, and mistrust. American Sociological Review. 2001;66:568–91. [Google Scholar]
- Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior. 2001;42:258–276. [PubMed] [Google Scholar]
- Ross CE, Reynolds JR, Geis KJ. The contingent meaning of neighborhood stability for residents' psychological well-being. American Sociological Review. 2000;65:581–97. [Google Scholar]
- Rubin DB. Multiple Imputation for Non-Response in Surveys. J Wiley & Sons; New York: 1987. [Google Scholar]
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Annual Review of Sociology. Vol. 28. Assessing ‘neighborhood effects’: Social processes and new directions in research: 2002. pp. 443–78. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;227:918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliot M, Fink A. A mental health intervention for schoolchildren exposed to violence: A randomized controlled trial. JAMA. 2003;290:603–612. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Stockwell T, Gruenewald PJ. Controls on the physical availability of alcohol. In: Heather N, Peters TJ, Stockwell T, editors. International Handbook of Alcohol Dependence and Problems. John Wiley and Sons; New York: 2001. pp. 699–720. [Google Scholar]
- Sturm R, Gresenz C, Sherbourne C, Minnium K, Klap R, Bhattacharya J, Farley D, Young AS, Burnham MA, Wells KB. The design of Healthcare for Communities: A study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry. 1999;36:221–233. [PubMed] [Google Scholar]
- Teplin LA, McClellan GM, Abram KM, Weiner DA. Crime victimization in adults with severe mental illness – comparison with the national crime victimization survey. Archives of General Psychiatry. 2005;62(8):911–921. doi: 10.1001/archpsyc.62.8.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treno AJ, Lee JP. Approaching alcohol problems through local environmental interventions. Alcohol Research and Health. 2002;26(1):35–41. [PMC free article] [PubMed] [Google Scholar]
- Unified Crime Reporting Program County Detailed Arrest and Offense Data. 2000 Obtained from www.icpsr.umich.edu, August 20, 2003.
- US Census Bureau. US Dept. of Commerce ZIP Code Business Patterns data (CD-ROM) 2001
- U.S. Census 2000 Summary File 3 – Sample Data. Tables P55, P87, H1, H7, H30, H39; Summary File 1 (SF1) – Sample Data. Table P8. Last accessed on April 28, 2005 at http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=DEC&_lang=en.
- van der Linden J, Drukker M, Gunther N, Feron F, van Os J. Children's mental health service use, neighborhood socioeconomic deprivation, and social capital. Social Psychiatry and Psychiatric Epidemiology. 2003;38:507–14. doi: 10.1007/s00127-003-0665-9. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinksi M, Keller SF. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weich S, Twigg L, Holt G, Lewis G, Jones K. Contextual risk factors for the common mental disorders in Britain: a multilevel investigation of the effects of place. Journal of Epidemiology and Community Health. 2003;57:616–621. doi: 10.1136/jech.57.8.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel L, Glanz K, Lerman C. Stress, coping and health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory research and practice. Jossey-Bass; San Francisco, CA: 2002. pp. 210–239. [Google Scholar]
- Wheaton B, Clarke P. Space meets time: integrating temporal and contextual influences on mental health in early adulthood. American Sociological Review. 2003;68:680–706. [Google Scholar]
- World Health Organization (WHO) Composite International Diagnostic Interview, Core Version 2.1 Computer Manual. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- World Health Organization (WHO) Guidelines for Use in Primary Health Care. Second edition World Health Organization; Geneva, Switzerland: 2001. The Alcohol Use Disorders Identification Test (AUDIT) [Google Scholar]