Abstract
Purpose
To determine the prevalence of anxiety and depressive disorders in youth with asthma compared to a control sample of youth and to determine the sociodemographic and clinical characteristics associated with having ≥1 anxiety/depressive disorders among youth with asthma.
Methods
A telephone interview was offered to all youth aged 11 to 17 with asthma (N=781) and a random sample of similar aged controls (N=598) enrolled in a Health Maintenance Organization (HMO). The C-DISC-4.0 was used to diagnose anxiety and depressive disorders and reliable and valid questionnaires were used to assess severity of anxiety and depressive symptoms. Automated diagnostic, pharmacy and health utilization data were used to measure asthma treatment intensity, asthma severity and non-asthmatic medical comorbidity. One parent was interviewed to assess sociodemographic variables, child/adolescent psychiatric symptoms and to confirm the asthma diagnosis.
Results
16.3% of youth with asthma compared to 8.6% of youth without asthma met DSM-IV criteria for ≥1 anxiety and depressive disorders (OR = 1.92, 95% CI 1.13–3.28). Independent factors associated with a significantly higher likelihood of meeting criteria for ≥1 anxiety or depressive disorders included female gender [OR = 1.96 (95% CI 1.27, 3.03)], living in a single parent household, [OR = 1.96 (95% CI 1.26, 3.07)], more parent-reported externalizing behaviors [OR = 1.03 (95% CI 1.01, 1.05)], more recent diagnosis of asthma [OR = 0.94 (95% CI 0.89, 0.98)], and more impairment on the asthma physical health scale [OR = 0.95 (95% CI 0.94, 0.96)].
Conclusions
Youth with asthma have an almost two-fold higher prevalence of comorbid DSM-IV anxiety and depressive disorders compared to control youth. Clinical factors associated with meeting criteria for ≥1 anxiety and depressive included more recent asthma diagnosis, more impairment on the asthma physical health scale and increased externalizing behaviors.
Keywords: anxiety, depression, asthma, youth
Cross-sectional studies have repeatedly found an increased prevalence of panic disorder among youth with asthma.[1–5] A large family history study also recently reported that first degree relatives of patients with panic disorder had a significantly higher prevalence of asthma and chronic obstructive lung disease compared to a control group without panic disorder.[6] Recent research suggests that youth with asthma also have a high rate of other depressive and anxiety disorders.[4, 7–9] A recent longitudinal study also found that anxiety and depressive disorders were associated with a higher risk of subsequent development of asthma.[10]
While these epidemiologic studies are suggestive of an association between anxiety and depressive disorders and asthma, conclusions are limited by the fact that only one study had information on physician diagnosis of asthma, as well as other medical comorbidities, there was no or limited data on asthma severity, asthma treatments (some of which can cause increased anxiety), and health risk behaviors such as smoking [11]. In addition, few of the studies included potential validators of structured psychiatric interviews such as parental reports of symptoms of anxiety or depression or child-rated anxiety and depression rating scales.
It is important for clinicians to accurately recognize anxiety and depressive disorders in youth with asthma because these comorbid disorders are associated with increased asthma symptom burden[12], additive functional impairment[13], increased requests for asthma medication[14], increased emergency room visits[15] and increased hospitalizations[16].
The current study’s goals were: 1) to determine the prevalence of DSM-IV anxiety and depressive disorders using structured diagnostic interviews in a large sample of youth with asthma compared to a random sample of controls without asthma who were both enrolled in an HMO; and 2) to examine the demographic and clinical predictors of anxiety and depressive diagnoses in youth with asthma.
Methods
Setting
Group Health Cooperative (GHC) is a nonprofit health maintenance organization in Washington State with 25 GHC-owned primary care clinics as well as 75 contracted clinics. GHC has computerized cost and accounting systems that have organized cost and utilization summaries for every GHC enrollee since 1989. The study protocol was reviewed and approved by the institutional review board of GHC.
Participants and Recruitment
Potential participants between 11 and 17 years of age who were enrolled in GHC ≥6 months were identified from administrative data. The control sample of youth was required to have no evidence of asthma medication use or ICD-9 diagnoses of asthma in the last 12 months. A unique random number was given to each potential control, and in each 4 to 6 week recruitment wave, the youth with the lowest 100 numbers were released to the survey team.
Youth with asthma were required to meet at least one of the following criteria in the prior year in order to exclude those with very mild asthma (i.e. exercise induced):
hospitalization with an asthma diagnosis and ≥1 asthma prescription;
≥1 emergency room or urgent care visit with an asthma diagnosis and ≥1 asthma prescription;
≥2 office visits with an asthma diagnosis and ≥1 asthma prescription;
only 1 asthma visit, but ≥2 asthma prescriptions filled on different days;
≥4 prescriptions for asthma medication;
≥1 visit with an asthma diagnosis in the past year and another in the past 18 months and ≥1 asthma prescription during that year.
Following receipt of a letter inviting participation in the study and providing consent, participants completed a telephone interview that included a 15- to 20-minute parent interview and 45- to 75-minute child/adolescent interview. Both the parent and the youth aged 13 to 17 provided written informed consent. Only parental consent was required for youth <13.
Data Collection
The parent interview included demographic questions and the Child Behavior Checklist (CBCL), a 120-item checklist of symptoms of internalizing (anxiety and depressive symptoms) and externalizing (behavioral problems) disorders, found to have high reliability and validity across numerous research studies.[17] As a proxy for socioeconomic status, census block data based on address and zip code was used to estimate median household income. For youth with asthma, the parent interview included confirmation that the child had been diagnosed with asthma and use of asthma medication.
All youth completed a telephone version of the Diagnostic Interview Schedule for Children NIMH DISC-4.0, a reliable and valid structured interview designed for lay interviewers, which includes algorithms to diagnose DSM-IV disorders in children and adolescents.[18] Telephone versions of structured psychiatric interviews in both adults[19] and youth[20] have been found to have a high correlation with in-person interviews. In order to decrease patient burden, only selected DISC-4.0 depression modules (major depression, dysthymia) and anxiety modules (panic disorder, separation anxiety, social phobia, generalized anxiety disorder and agoraphobia) were used.
All interviewers received 12 hours of classroom and hands-on training and additional, project-specific training on the C-DISC-4.0. Interview quality was continuously assessed through silent monitors installed on all telephones. Written feedback on errors, and corrective instruction were provided.
The youth interview also included the following measures. The Childhood Anxiety Sensitivity Index (ASI)[21] is a 16-item self report measure which assesses fear of anxiety symptoms and catastrophic cognitions regarding bodily sensations. Questions such as “It scares me when I am nauseous” and “It scares me when my heart beats rapidly” are scored on a 1 to 5 Likert Scale.. High scores on the ASI in patients with asthma have been shown to correlate with anxiety comorbidity.[22] The Mood and Feelings Questionnaire[23] short form is a 13-item questionnaire that codes symptoms on a 3 point scale (“true”, “sometimes true”, “not true”). This scale has been found to have high reliability and validity and the short form is made up of items that best discriminated depressed and non-depressed children in field trials using structured psychiatric interviews. Youth with asthma were also given the Child Health Survey-Asthma (CHS-A)[24], which is a functional status measure with high reliability and validity[24]. The instrument contains 3 subscales, 2 of which will be reported in this paper (physical health, activity limitations). Smoking status was measured by one question that has been shown to have high reliability and validity in a large U.S. study, “Have you smoked at least 100 cigarettes in your lifetime, that is about 5 packs of cigarettes”.[25]
The Pediatric Chronic Disease Scale (PCDS), an algorithm that classifies children into chronic disease categories by using claims data from prescription fills, was used to measure non-asthma and non-mental health-related medical comorbidity (such as sinusitis, diabetes, urinary tract infection).[26] The PCDS is a significant predictor of subsequent one-year health utilization and health care costs.
The Health Plan Employer Data and Information Set (HEDIS) definition of youth who are at high risk of adverse asthmatic events was used as one method to determine asthma severity.[27] In this definition, meeting criteria for any of the following four health care utilization variables over a 12-month period identifies the individuals at high medical risk: 1) ≥4 dispensings of asthma medication; 2) ≥1 emergency visit for asthma; 3) ≥1 hospitalization for asthma; 4) ≥4 ambulatory visits for asthma.[27] Because approximately 66% of our sample met the criteria for ≥4 dispensings of the asthma medication, suggesting lack of specificity as a measure of severity, we also developed a measure with a modified medication criteria (criteria 2, 3 and 4 above and ≥1 oral steroid prescriptions for asthma over a 12-month period).
Statistical Analysis
Since different methods of sampling were used in the two groups, we examined differences in deidentified data between survey respondents and nonrespondents using automated data in the two groups separately. We estimated response propensity scores (probability of being a respondent) for youth with asthma as a function of the following variables: age, gender, RUCA code (defining rural versus urban areas using zip code), being on Medicaid, Pediatric Chronic Disease Score, number of primary care visits, number of asthma-related emergency room visits and hospitalizations, oral steroid prescription, number of specialty mental health visits, any prescription for antidepressant or antianxiety medication, and an ICD-9 diagnosis of depression or anxiety. We used these same variables except for the inclusion of one variable, GHC primary care physician versus network physician, and exclusion of the asthma utilization and oral steroid prescription variables to estimate response propensity in controls. All health utilization variables refer to the past year.
We predicted response/nonresponse status for each sample as a function of the above predictor variables using logistic regression. Then, for each survey respondent, we estimated a response probability (the response propensity score). We divided this response probability into one to estimate a response probability adjusted analyses weight for each respondent. In subsequent weighted analyses, individuals with a low probability of responding are given a higher weight in the analysis to represent the larger number of nonrespondents with similar characteristics. All analyses use weighted data.
Demographic and clinical variables were compared between the asthma and control group using t tests for continuous variables and X2 with corrections for continuity for categorical outcomes. Rates of anxiety and depressive diagnoses were then calculated and compared between asthma and control groups using logistic regression analyses to calculate unadjusted odds ratios and their 95% confidence intervals. Adjusted odds ratios controlling for sociodemographic and clinical differences between the samples were also calculated and used to compare differences between the two groups in the percentage with ≥1 anxiety and depressive diagnosis and the percentage with each specific diagnosis.
Self-report and parental symptom measures were compared for groups with and without ≥1 anxiety and depressive disorders both in those with and without asthma using unadjusted t-tests. Adjusted analyses were then performed using analyses of covariance controlling for significant sociodemographic and clinical differences between the diagnostic groups.
The youth with asthma were divided into those with no psychiatric diagnoses and those with ≥1 anxiety and depression diagnosis, and were compared on the study demographic and clinical variables using chi square analyses with corrections for continuity for the categorical variables and t tests for the continuous variables. In order to identify variables that were independently and significantly associated with having ≥1 depressive and anxiety disorder, logistic regression modeling was employed. Variables that were univariately associated with the diagnostic grouping (p < .05) were first entered into the full regression model. Demographic, clinical and asthma-related variables were examined and eliminated individually from the full model. The final model included only statistically significant variables.
Results
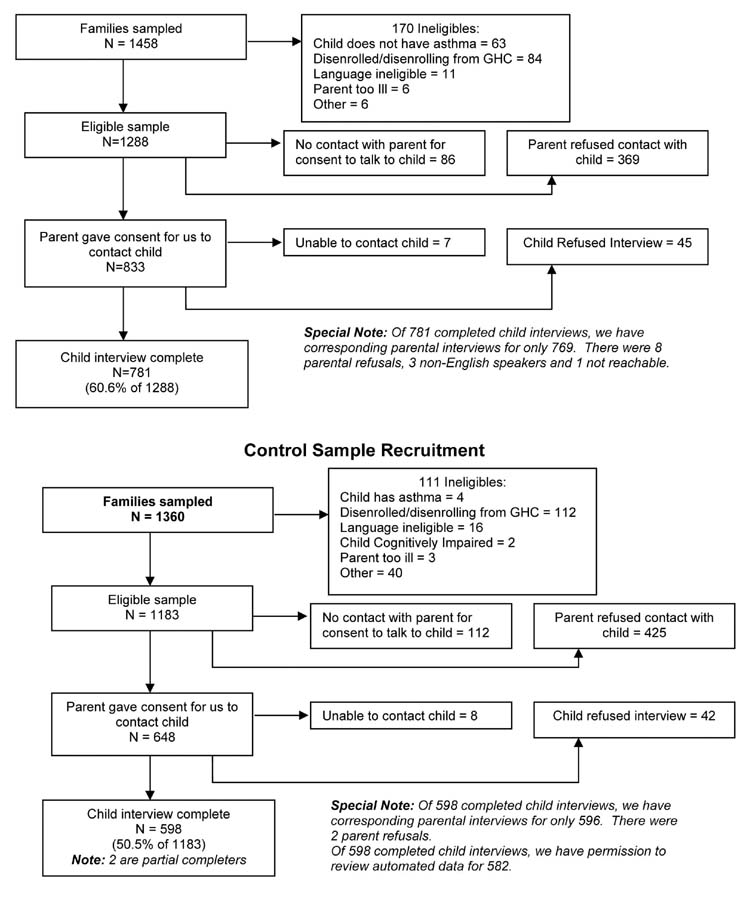
Of the 1458 youth with asthma and parents in the initial sample, 1288 proved eligible (Figure 1). A total of 833 eligible parents gave consent and permission for us to contact their child/adolescent with asthma. Of these, we completed 781 child/adolescent interviews for a final recruitment rate of 60.6%. Of the 1360 control youth without asthma, 1183 proved eligible (Figure 1). A total of 648 eligible parents gave consent and permission to contact their child/adolescent without asthma. Of these, we completed 598 youth interviews for a recruitment rate of 50.5% in control youth.
Figure 1.
Recruitment of Youth with Asthma and Controls Youth with Asthma Recruitment
As shown in Table 1, youth with asthma compared to controls were significantly more likely to be African-American, were more likely to have both parents unemployed, to come from a single parent family, to be on Medicaid, to have higher medical comorbidity scores and higher parent-rated scores on the CBCL internalizing and externalizing scales, as well as rating themselves as having higher levels of severity on the ASI and Mood and Feelings questionnaires.
Table 1.
Demographic and Clinical Variables Stratified for Youth with and without Asthma (N = 1351 Youth + 1339 Parents)
| Total Sample | No Asthma N (%) N = 582 | Asthma N (%) N = 769 | Test Statistics t(1349) or X2(1) |
|---|---|---|---|
| Demographics N (%) | |||
| Age (Mean ± SD) | 14.1 ± 1.9 | 14.0 ± 1.9 | 1.13 |
| N (%) Female | 294 (50.5) | 358 (46.6) | 1.93 |
| Education Level of Most Educated Parent
N (%) High School Graduate or Less N (%) Some College N (%) College Graduate or More |
48 (8.2) 207 (35.6) 327 (56.2) |
61 (8.1) 326 (43.1) 370 (48.9) |
8.04* |
| Parent Ethnicity
Caucasian N (%) African-American N (%) Asian & Pacific Islander N (%) Native American N (%) Other N (%) |
474 (81.6) 28 (4.8) 38 (6.5) 25 (4.3) 16 (2.8) |
606 (80.4) 47 (6.2) 26 (3.4) 51 (6.8) 24 (3.2) |
11.46* df = 4 |
| N (%) Any Parent Employed PT or FT | 559 (96.0) | 710 (93.7) | 3.26* |
| Parental Marital Status
N (%) Married N (%) Single N (%) Divorced, Separated, Widowed |
465 (79.9) 35 (6.0) 82 (14.1) |
551 (72.8) 55 (7.3) 151 (19.9) |
9.45** df = 2 |
| N (%) Eastern WA | 192 (33.0) | 261 (33.9) | 0.10 |
| N (%) Medicaid | 47 (8.1) | 105 (13.7) | 9.77** |
| Median Household Income in 1999 ($)† | 52135 ± 18303 | 50460 ± 17015 | t(1322) = 1.72 |
| Clinical | |||
| Medical Comorbidity Score (PedCDS without asthma) | 323.6 ± 436.5 | 614.3 ± 959.7 | 7.44*** |
| N (%) Smoking at least 100 Cigs in Life | 23 (4.0) | 38 (4.9) | 0.54 |
| CBCL Internalizing | 6.8 ± 6.4 | 10.4 ± 8.3 | 9.00*** |
| CBCL Externalizing | 6.7 ± 7.2 | 9.2 ± 8.2 | 5.94*** |
| Anxiety Sensitivity Index (ASI) | 10.3 ± 8.6 | 11.7 ± 9.0 | 2.78** |
| Mood and Feelings Questionnaire | 3.0 ± 4.3 | 3.7 ± 4.6 | 2.72** |
N = 742 for asthma and 582 for non-asthma samples
p < 0.05;
p < 0.01;
p < 0.001
As shown in Table 2, a significantly higher percentage of youth with asthma compared to control youth (16.3% vs. 8.6%) met DSM-IV criteria in the prior 12 months for ≥1 DSM-IV anxiety and/or depressive disorder. In the adjusted models, there was a significantly higher rate of agoraphobia in youth with asthma compare to control youth. There was also non-significant trends for the prevalence of all anxiety and depressive disorders (except dysthymia) to be increased in youth with asthma compared to controls (odds ratios between 1.69 and 2.28).
Table 2.
C-DISC-4.0 Results: Overall Rates of DSM-IV Anxiety and Depressive Disorders
| Diagnosis - Past Year | All (N = 1351) | No Asthma (N = 582) | Asthma (N = 769) | Unadjusted OR 95% CI | Adjusted† OR 95% CI |
|---|---|---|---|---|---|
| Major Depression | 78 (5.8%) | 23 (4.0%) | 55 (7.2%) | 1.89* (1.15 – 3.11) | 1.65 (.99 – 2.76) p = .056 |
| Dysthymia | 1 (0.1%) | 0 (0.0%) | 1 (0.1%) | -- | -- |
| Panic Disorder | 26 (1.9%) | 7 (1.2%) | 19 (2.5%) | 2.09 (.87 – 5.00) | 1.93 (.78 – 4.77) |
| Generalized Anxiety Disorder | 24 (1.8%) | 7 (1.2%) | 17 (2.2%) | 1.86 (.77 – 4.51) | 1.80 (.71 – 4.56) |
| Social Phobia | 33 (2.4%) | 8 (1.4%) | 25 (3.3%) | 2.41* (1.08 – 5.39) | 2.28 (.99 – 5.26) p = .053 |
| Separation Anxiety | 37 (2.7%) | 11 (1.9%) | 26 (3.4%) | 1.82 (.89 – 3.71) | 1.69 (.82 – 3.48) |
| Agoraphobia | 77 (5.7%) | 20 (3.4%) | 57 (7.5%) | 2.27** (1.34 – 3.82) | 1.92** (1.13 – 3.28) |
| Any 1 Anxiety or Depressive Diagnosis | 175 (13.0%) | 50 (8.6%) | 125 (16.3%) | 2.07** (1.46 – 2.93) | 1.83*** (1.28 – 2.62) |
Adjusted for ethnicity, education, marital status, Medicaid and Pediatric CDS
p < 0.05;
p < 0.01;
p < 0.001
Data from the self-report anxiety (Anxiety Sensitivity Index) and depression (Mood and Feelings) questionnaires (Table 3) also show that youth with and without asthma who met criteria for ≥1 DSM-IV anxiety and depressive disorders on structured interviews rated themselves as having significantly more anxiety and depressive symptoms than children/adolescents who did not meet DSM-IV criteria for ≥1 of these illnesses. Parents also rated youth with and without asthma who met DSM-IV criteria for ≥1 anxiety and depressive disorders as having significantly higher scores on the internalizing subscale of the Child Behavior Checklist. When these analyses were repeated adjusting for gender, parental education, employment, and marital status, Medicaid insurance and the PCDS, the significant differences between the youth with and without anxiety/depression diagnoses within the asthma and control groups were retained.
Table 3.
Parental and Self Report Ratings of Anxiety and Depressive Symptoms
| Total Sample | No Depressive/Anxiety Disorders | Any Anxiety or Depressive Disorder | Test Statistics t† |
|---|---|---|---|
| Youth with Asthma (N = 768) | N = 643 | N = 125 | |
| CBCL Internalizing | 9.3 ± 7.3 | 16.0 ± 10.4 | 6.80*** |
| Anxiety Sensitivity Index (ASI) | 9.8 ± 7.0 | 21.5 ± 11.5 | 11.02*** |
| Mood and Feelings Questionnaire | 2.8 ± 3.6 | 8.6 ± 5.9 | 10.73*** |
| Control Youth (N = 582) | N = 532 | N = 50 | |
| CBCL Internalizing | 6.6 ± 6.2 | 9.2 ± 7.2 | 2.45* |
| Anxiety Sensitivity Index (ASI) | 9.5 ± 7.7 | 18.6 ± 12.5 | 5.06*** |
| Mood and Feelings Questionnaire | 2.5 ± 3.4 | 8.9 ± 7.4 | 6.11*** |
df = 387 for control youth and 764 for youths with asthma
p < 0.05;
p < 0.01;
p < 0.001
Table 4 shows the univariate comparisons of children/adolescents with asthma with no anxiety or depressive disorder versus those with ≥1 disorders. Those with ≥1 anxiety or depressive disorders were significantly more likely to be female, to have parents with less education, who were less likely to be married, were more likely to live in a neighborhood with lower median household income, and to be on Medicaid. Those with ≥1 anxiety or depressive disorders also had significantly higher medical comorbidity, a more recent diagnosis of asthma, were more likely to be smoking, had higher scores on externalizing behavior on the parental version of the CBCL, had more asthma symptom days, more impairment on the asthma-related physical health and activity limitations subscales, and were more likely to have been prescribed a long acting beta-agonist compared to youth without psychiatric disorders. No differences were seen between the two subgroups on either asthma severity measure or any of the individual health utilization variables included in these measures.
Table 4.
Demographic, Clinical and Asthma Severity Variables in Youth with Asthma Stratified by Those Meeting and Not Meeting Criteria for ≥1 Anxiety and Depressive Disorders (N = 768)
| Total Sample | No Depressive/Anxiety Disorders | Any DSM-IV Anxiety or Depressive Disorder | Test Statistics t(765) or X2(1) |
|---|---|---|---|
| Demographics N (%) | 643 (83%) | 125 (17%) | |
| Age (Mean ± SD) | 13.9 ± 1.9 | 14.2 ± 2.0 | 1.17 |
| N (%) Female | 276 (43.0) | 80 (64.0) | 17.73*** |
| Education Level of Most Educated Parent:
N (%) High School Graduate or Less N (%) Some College N (%) College Graduate or More |
43 (6.8) 269 (42.4) 323 (50.9) |
18 (15.4) 57 (46.9) 47 (37.7) |
11.73** df = 2 |
| Parent Ethnicity (N = 765)
Caucasian N (%) African-American N (%) Asian & Pacific Islander N (%) Native American N (%) Other N (%) |
514 (81.4) 33 (5.2) 23 (3.6) 42 (6.6) 20 (3.2) |
91 (74.6) 15 (12.3) 3 (2.5) 9 (7.4) 4 (3.2) |
9.16 df = 5 |
| N (%) Any Parent Employed PT or FT (N = 756) | 598 (94.3) | 110 (90.2) | 2.32 |
| Parental Marital Status (N = 756)
N (%) Married N (%) Single N (%) Divorced, Separated, Widowed |
481 (75.9) 40 (6.9) 113 (17.8) |
70 (57.4) 15 (12.3) 37 (30.3) |
17.90*** df = 2 |
| N (%) Eastern WA | 218 (34.0) | 42 (33.6) | 0.00 |
| N (%) Medicaid | 79 (12.3) | 25 (20.2) | 4.82* |
| Median Household Income in 1999 ($) | 51091 ± 16806 | 47212 ±17841 | 2.19* |
| Clinical | |||
| Years Since Asthma Diagnosis | 7.4 ± 4.3 | 6.4 ± 4.3 | 2.27* |
| Medical Comorbidity Score (PedCDS without asthma) | 580.5 ± 962.5 | 794.8 ± 934.5 | 2.28* |
| N (%) Smoking At Least 100 Cigs in Life | 23 (3.6) | 14 (11.3) | 11.83*** |
| CBCL Externalizing | 8.6 ± 7.9 | 12.5 ± 9.4 | 4.30*** |
| Asthma Severity | |||
| N (%) Severe on the Asthma Severity Measure: Any one of the following:
● ER or inpatient asthma visit ● ≥1 oral steroid prescription ● ≥4 outpatient visits |
190 (29.5) |
43 (34.4) |
0.95 |
| N (%) Severe on the HEDIS Asthma Severity Measure: Any one of the following:
● ER or inpatient asthma visit ● ≥4 outpatient visits ● ≥4 asthma prescriptions of any kind |
447 (69.6) |
86 (68.8) |
0.01 |
| Symptom Days in Last 2 Weeks | 3.5 ± 3.9 | 5.4 ± 4.2 | 4.53*** |
| Physical Health (CHS-A) Subscale | 75.9 ± 14.4 | 62.4 ± 16.4 | 9.32*** |
| Activity Limitations Scale (CHS-A) Subscale | 85.6 ± 16.2 | 74.2 ± 18.1 | 6.52*** |
| N (%) Controller Medication Prescribed (leukotrine inhibitor, inhaler-steroid, long-acting beta-agonist)
% Any One Medication N (%) inhaled steroid N (%) Leukotriene modifier N (%) long-acting beta-agonist N (%)Two or Three Medications |
475 (73.9) 441 (68.6) 97 (15.1) 114 (17.8) 154 (24.0) |
90 (72.6) 85 (68.5) 16 (12.8) 12 (9.7) 20 (16.0) |
0.04 0.00 0.16 4.37* 3.36 |
p < 0.05;
p < 0.01;
p < 0.001
The final logistic regression model found that being female [OR = 1.96; 95% CI = 1.27, 3.03; β = 0.68, Walds (df = 1) = 9.31], living with a currently unmarried parent [OR = 1.96; 95% CI = 1.26, 3.07; β = 0.68, Walds (df = 1) = 8.80], a more recent diagnosis of asthma [OR = 0.94; 95% CI = 0.89, 0.98; β = −0.07, Walds (df = 1) = 6.81], higher externalizing scores on the CBCL [OR = 1.03; 95% CI = 1.01, 1.05; β = 0.03, Walds (df = 1) = 4.47] and a lower physical health score on the asthma-specific functional impairment scale [OR = 0.95; 95% CI = 0.94, 0.96; β = −0.05, Walds (df = 1) = 48.96] were associated with a higher likelihood of meeting criteria for ≥1 anxiety and depressive diagnosis in youth with asthma.
Discussion
Youth with asthma compared to controls were found to be almost twice as likely to meet DSM-IV criteria for ≥1 anxiety and depressive disorders. Unlike some prior reports, which have emphasized a higher rate of panic disorder in youth with asthma[1–5], our data suggest that there is an increase in all anxiety and depressive disorders in youth with asthma compared to controls (although only the difference in rates of agoraphobia reached statistical significance). These results extend the findings of previous research by including physician diagnoses of asthma and other medical comorbidities, asthma treatments and asthma severity and smoking. Because symptoms of anxiety (i.e. shortness of breath, rapid heart rate) and depressive disorders (i.e. insomnia, fatigue) may overlap with symptoms of asthma, our study also included validators of psychiatric diagnoses such as parental reports of anxiety and depressive symptoms and child-rated anxiety and depression questionnaires. Our data showed that youth who were identified as meeting DSM-IV criteria for ≥1 anxiety and depressive disorders on the C-DISC also scored significantly higher on these parent- and child-rated constructs compared to controls.
Four recent studies have also reported increased rates of multiple anxiety and depressive disorders in youth and adults with asthma compared to controls.[4, 8, 9, 28] A recent epidemiologic study in youth 9 to 17 years of age reported that youth with a history of asthma were more likely to have any anxiety disorder, simple phobia, separation anxiety and overanxious disorder compared to controls.[4] Data from two large, longitudinal studies of youth also found an association between asthma and an increased likelihood of developing depressive and anxiety disorders.[8, 9] Finally, one adult study of over 1,000 community adult respondents found that lifetime severe asthma was associated with an increased likelihood of panic disorder, social phobia, generalized anxiety disorder, any anxiety disorder and bipolar disorder.[28]
The 7.5% prevalence of agoraphobia in the prior 12-months was particularly high compared to the 3.4% rate found in control youth as well as the 0.5% to 4.0% rates found in community-based epidemiologic studies.[29–31] The C-DISC questions on agoraphobia specifically ask about feelings of fear about: traveling in cars, buses or trains, being on bridges or in tunnels, being in crowded places and going out of the house by oneself. Some of these agoraphobic fears could be conditioned by frightening experiences with asthma such as a severe episode that occurred when alone or episodes in public transportation or crowded areas exacerbated by smoking, perfumes or other pollutants. Parental overprotection of youth with asthma because of previous frightening or life-threatening episodes may also affect youth self-confidence and development of autonomy. Alternatively both asthma and anxiety disorders such as agoraphobia may result from a shared genetic (i.e. instability of the autonomic nervous system) or environmental diathesis (i.e. chronic exposure to second hand cigarette smoke) or an abusive early environment.[11]
Given that many youth with asthma and comorbid anxiety and depressive disorders are not accurately diagnosed by primary care physicians[32], the factors associated with higher risk of these psychiatric disorders are important to emphasize. The factors that were significantly associated with meeting DSM-IV criteria for ≥1 anxiety or depressive disorders in youth with asthma included female gender, living in a single parent household, higher externalizing behavioral scores, more recent asthma diagnosis, and greater functional impairment. In univariate analyses, several markers of lower socioeconomic status including less parental education, single parent family, lower median neighborhood household income, and Medicaid were also significantly associated with meeting criteria for ≥1 anxiety or depressive disorder. In previous studies variables such as less parent education and income, living in poorer neighborhoods, and single parent households have been shown to be associated with higher prevalence rates of both asthma[33, 34] and of DSM-IV anxiety and depressive disorders[29–31]. Youth who are raised in single parent households have also been shown to have a higher risk of externalizing disorders.[35] Thus, primary care physicians should be especially vigilant to screen for anxiety and depressive disorders among youth with asthma who have reduced resources in the home as well as behavioral problems.
Neither asthma severity measure was associated with anxiety or depressive disorders. On the other hand, greater physical functional limitations due to asthma were associated with meeting criteria for ≥1 anxiety and depressive disorders. Although these are cross-sectional data limiting causal interpretation, prior studies have shown that anxiety and depressive disorders in patients with chronic illness (such as asthma and diabetes) are associated with a higher number of physical symptoms[12, 36], and greater functional impairment[13, 37] even after controlling for severity of medical disease.
It is worrisome that children/adolescents with asthma and ≥1 anxiety/depressive disorder were over three times as likely to be smokers. We have previously shown that over 97% of youth with asthma who were smokers were in the 15- to 17-year age range when rates of anxiety and depressive disorders are also highest[38] Smoking is a major risk factor in asthma medication failure[39], and could contribute to the higher asthma symptom burden[12] and asthma related physical impairment[13] seen in youth with ≥1 anxiety/depressive disorders. Enhanced screening for anxiety and depressive disorders in youth with asthma who smoke and provision of effective treatment for these mental health disorders may help decrease rates of this high-risk health behavior.
More recent diagnosis of asthma was also associated with a higher likelihood of having ≥1 anxiety and depressive disorders. The initial development of asthma can be associated with significant stress for parents and the child/adolescent, which may decrease over time as families and children learn to manage and adapt to this illness. Patients with chronic medical illness often describe more impairment in functioning and quality of life initially compared to later stages.[40] This early stressful period may explain the association of a more recent diagnosis of asthma with psychiatric illness.
Limitations of this study include: the lack of objective physiologic tests for asthma diagnosis and asthma severity; subjects were from one large HMO in one geographic region of the United States and the 61% response rate in youth with asthma and the 51% response rate in controls limits generalizability; and overlapping symptoms of anxiety and asthma such as shortness of breath may make differentiation of anxiety and asthma symptomatology difficult.
CONCLUSIONS
Physicians should be aware of the increased rate of DSM-IV anxiety and depressive disorders in youth with asthma and that factors that raise the risk of meeting criteria for these mental health disorders include female gender, living in a single parent household, more recent asthma diagnosis, higher parent rated behavior problems, and greater asthma physical impairment. Given the high rate of comorbid anxiety and depressive disorders in youth with asthma and the adverse effect on asthma symptom burden,[12] functional impairment[13] and medical costs,[16] health care systems should consider developing programs that provide: 1) enhanced parent and youth education about the increased risk for anxiety and depressive disorders in youth with asthma; 2) routing screening for comorbid anxiety and depressive disorders; and 3) development of evidence-based anxiety and depression treatment programs for these youth.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health to Dr. Katon (MH-067587 and MH-069741)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kashani JH, Konig P, Shepperd JA, Wilfley D, Morris DA. Psychopathology and self-concept in asthmatic children. J Pediatric Psychol. 1988;13:509–20. doi: 10.1093/jpepsy/13.4.509. [DOI] [PubMed] [Google Scholar]
- 2.Vila G, Nollet-Clemencon C, de Blic J, Mouren-Simeoni MC, Scheinmann P. Prevalence of DSM IV anxiety and affective disorders in a pediatric population of asthmatic children and adolescents. Journal of Affective Disorders. 2000;58:223–31. doi: 10.1016/s0165-0327(99)00110-x. [DOI] [PubMed] [Google Scholar]
- 3.Vila G, Nollet-Clemencon C, Vera M, et al. Prevalence of DSM-IV disorders in children and adolescents with asthma versus diabetes. Can J Psychiatry. 1999;44:562–9. doi: 10.1177/070674379904400604. [DOI] [PubMed] [Google Scholar]
- 4.Ortega AN, Huertas SE, Canino G, Ramirez R, Rubio-Stipec M. Childhood asthma, chronic illness, and psychiatric disorders. Journal of Nervous and Mental Disease. 2002;190:275–81. doi: 10.1097/00005053-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Goodwin RD, Pine DS, Hoven CW. Asthma and panic attacks among youth in the community. Journal of Asthma. 2003;40:139–45. doi: 10.1081/jas-120017984. [DOI] [PubMed] [Google Scholar]
- 6.van Beek N, Schruers KR, Griez EJ. Prevalence of respiratory disorders in first-degree relatives of panic disorder patients. Journal of Affective Disorders. 2005;87:337–40. doi: 10.1016/j.jad.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Craske MG, Poulton R, Tsao JC, Plotkin D. Paths to panic disorder/agoraphobia: an exploratory analysis from age 3 to 21 in an unselected birth cohort. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:556–63. doi: 10.1097/00004583-200105000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Goodwin RD, Fergusson DM, Horwood LJ. Asthma and depressive and anxiety disorders among young persons in the community. Psychological Medicine. 2004;34:1465–74. doi: 10.1017/s0033291704002739. [DOI] [PubMed] [Google Scholar]
- 9.Feldman JM, Ortega AN, McQuaid EL, Canino G. Comorbidity between asthma attacks and internalizing disorders among Puerto Rican children at one-year follow-up. Psychosomatics. 2006;47:333–9. doi: 10.1176/appi.psy.47.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hasler G, Gergen PJ, Kleinbaum DG, et al. Asthma and panic in young adults: a 20-year prospective community study. American Journal of Respiratory and Critical Care Medicine. 2005;171:1224–30. doi: 10.1164/rccm.200412-1669OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosomatic Medicine. 2004;66:349–55. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- 12.Richardson LP, Lozano P, Russo J, et al. Asthma symptom burden: relationship to asthma severity and anxiety and depression symptoms. Pediatrics. 2006;118:1042–51. doi: 10.1542/peds.2006-0249. [DOI] [PubMed] [Google Scholar]
- 13.McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. Gen Hosp Psychiatry. 2007;29:214–22. doi: 10.1016/j.genhosppsych.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dahlem NW, Kinsman RA, Horton DJ. Panic-fear in asthma: requests for as-needed medications in relation to pulmonary function measurements. Journal of Allergy and Clinical Immunology. 1977;60:295–300. doi: 10.1016/0091-6749(77)90108-7. [DOI] [PubMed] [Google Scholar]
- 15.Nouwen A, Freeston MH, Labbe R, Boulet LP. Psychological factors associated with emergency room visits among asthmatic patients. Behavior Modif. 1999;23:217–33. doi: 10.1177/0145445599232002. [DOI] [PubMed] [Google Scholar]
- 16.Dirks JF, Kinsman RA, Horton DJ, Fross KH, Jones NF. Panic-fear in asthma: rehospitalization following intensive long-term treatment. Psychosomatic Medicine. 1978;40:5–13. doi: 10.1097/00006842-197802000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Achenbach T. Manual for Childhood Behavior Checklist (4–18) and 1991 Profile. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- 18.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Wells KB, Burnam MA, Leake B, Robins LN. Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH Diagnostic Interview Schedule. Journal of Psychiatric Research. 1988;22:207–20. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- 20.Wasserman GA, McReynolds LS, Lucas CP, Fisher P, Santos L. The voice DISC-IV with incarcerated male youths: prevalence of disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:314–21. doi: 10.1097/00004583-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Silverman W, Flergig W, Rabian B, Peterson R. Childhood Anxiety Sensitivity Index. Journal of Clinical Child Psychology. 1995;20:162–8. [Google Scholar]
- 22.Carr RE, Lehrer PM, Rausch LL, Hochron SM. Anxiety sensitivity and panic attacks in an asthmatic population. Behaviour Research and Therapy. 1994;32:411–8. doi: 10.1016/0005-7967(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 23.Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:726–37. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the Children’s Health Survey for Asthma. Pediatrics. 1999;104:e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 25.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychology. 1996;15:355–61. doi: 10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- 26.Fishman PA, Shay DK. Development and estimation of a pediatric chronic disease score using automated pharmacy data. Medical Care. 1999;37:874–83. doi: 10.1097/00005650-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 27.National Committee for Quality Assurance. HEDIS 3.0. 1997
- 28.Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Archives of General Psychiatry. 2003;60:1125–30. doi: 10.1001/archpsyc.60.11.1125. [DOI] [PubMed] [Google Scholar]
- 29.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129–36. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 30.Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:865–77. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 31.McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:50–9. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44:1064–72. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 33.Smith LA, Hatcher-Ross JL, Wertheimer R, Kahn RS. Rethinking race/ethnicity, income, and childhood asthma: racial/ethnic disparities concentrated among the very poor. Public Health Reports. 2005;120:109–16. doi: 10.1177/003335490512000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Litonjua AA, Carey VJ, Weiss ST, Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatric Pulmonology. 1999;28:394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 35.Spencer N. Does material disadvantage explain the increased risk of adverse health, educational, and behavioural outcomes among children in lone parent households in Britain? A cross sectional study. Journal of Epidemiology and Community Health. 2005;59:152–7. doi: 10.1136/jech.2004.020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry. 2003;54:216–26. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 37.Von Korff M, Katon W, Lin EH, et al. Potentially modifiable factors associated with disability among people with diabetes. Psychosomatic Medicine. 2005;67:233–40. doi: 10.1097/01.psy.0000155662.82621.50. [DOI] [PubMed] [Google Scholar]
- 38.Bush T, Richardson L, Katon W, et al. Anxiety and depressive disorders are associated with smoking in adolescents with asthma. J Adolesc Health. 2007;40:425–32. doi: 10.1016/j.jadohealth.2006.11.145. [DOI] [PubMed] [Google Scholar]
- 39.Livingston E, Thomson NC, Chalmers GW. Impact of smoking on asthma therapy: a critical review of clinical evidence. Drugs. 2005;65:1521–36. doi: 10.2165/00003495-200565110-00005. [DOI] [PubMed] [Google Scholar]
- 40.Damschroder LJ, Zikmund-Fisher BJ, Ubel PA. The impact of considering adaptation in health state valuation. Social Science and Medicine. 2005;61:267–77. doi: 10.1016/j.socscimed.2004.11.060. [DOI] [PubMed] [Google Scholar]