Abstract
Background
Gestational weight gain is important to assess for epidemiological and public health purposes: it is correlated with infant growth and may be related to maternal outcomes such as reproductive health and chronic disease risk. Methods commonly used to assess weight gain incorporate assumptions that are usually not borne out, such as a linear weight gain, or do not account for differential length of gestation.
Methods
We introduce a novel method to assess gestational weight gain, the area under the weight gain curve. This is easily interpretable as the additional pound-days carried due to pregnancy and avoids many flaws in alternative assessments. We compare the performance of the simple difference, weekly gain, Institute of Medicine categories and the area under the weight gain curve in predicting birthweight and maternal weight retention at 6, 12, 24 and 36 months post-partum. The analytic sample comprises 2016 participants in Project Viva, an observational prospective cohort study of pregnant women in Massachusetts.
Results
For birthweight outcomes, none of the weight gain measures is a meaningfully superior predictor. For 6-month postpartum weight retention the simple difference is superior, while for 12-, 24- and 36-month weight retention the area under the weight gain curve is superior.
Conclusions
These findings are plausible biologically: the same amount of weight gained early vs later in the pregnancy may reflect increased maternal fat stores. The timing of weight gain is reflected best in the area under the weight gain curve. Different methods of measuring gestational weight gain may be appropriate depending on the context.
Keywords: Pregnancy, weight gain, pregnancy weight retention, weight gain metrics, weight gain measures
Introduction
Prospective studies identify gestational weight gain as a predictor of both infant birthweight1–6 and pre-term delivery7–14 Greater gestational weight gain is associated with increased risk of postpartum weight retention2, 15–18 and increased risk of caesarean section,19, 20 even after adjustment for infant birth-weight.21, 22 Various methods for assessing gestational weight gain have been used, including total weight gain during pregnancy, total weekly rate of weight gain and weekly rate of gain over specific trimesters or months.
None of these methods has been universally adopted, possibly leading to conflicting results or recommendations due to different definitions. Each of the methods currently in use has limitations. For example, total weight gain necessarily correlates with length of gestation. Rate of gain adjusts for gestation length, but only under the false assumption that weight increases linearly. Both of these methods ignore the pattern of the weight gain over pregnancy. This may lead to incorrect conclusions regarding the relationship of gestational weight gain to infant and maternal outcomes if weight gain in different periods of a pregnancy affects outcomes in different ways. There has been no systematic comparison of the different techniques.
We have developed a novel method of measuring gestational weight gain, obtained by calculating the area under the gestational weight gain curve (AUC). This method, described in detail subsequently, provides a single measure that reflects both the amount of weight gain and the timing of gain. The purpose of this study is to compare the AUC with commonly used gestational weight gain measurements as regards their association with fetal and maternal outcomes.
Methods
Subjects and setting
Study participants were women enrolled in Project Viva, a prospective observational study of gestational exposures, pregnancy outcomes and offspring health.23 Women were recruited at their initial pre-natal visit at eight obstetrical offices of a multi-specialty group practice in eastern Massachusetts. Eligibility criteria included fluency in English, gestational age less than 22 weeks at the initial prenatal clinical appointment, and singleton pregnancy. We enrolled 2341 eligible participants, of whom 9% withdrew (n = 195) or were lost to follow-up (n = 18). Of the 2128 remaining women, mothers who delivered prior to 34 weeks gestation (n = 45) were excluded because the relationship between weight gain and outcomes is expected to be qualitatively different in this group and few such deliveries occurred. Of the remaining mothers, 54 had insufficient pre-delivery weight data, leaving 2029 women. Further exclusion of women missing race (n = 14) or birth outcome data (n = 1) left 2014. This article includes data available as of December, 2006.
After obtaining informed consent, we collected demographic and health history information by interview and self-administered questionnaire. All procedures were in accordance with the ethical standards for human experimentation established by the Declaration of Helsinki.24 Institutional Review Boards of participating institutions approved the study.
Birth data
We obtained infant birthweight from the hospital medical record. We calculated the length of gestation by subtracting the date of the last menstrual period (LMP) from the date of delivery. If gestational age according to a 16–20-week ultrasound differed from that according to the LMP by >10 days, we used the ultrasound result to determine gestation length. We determined birthweight for gestational age Z-values using as a reference a combined 1999–2000 US Natality data set.25
Maternal weight and height
Women self-reported their height and pre-pregnancy weight. Self-reported weight generally correlates well with measured weight, although there is a tendency for overweight women to underreport their weight.26, 27 Data from 170 women in Project Viva with both self-reported and clinical measurement of pre-pregnancy weight showed a correlation of 0.98. We obtained missing heights from the clinical record (n = 55). For 71 women who were missing a reported pre-pregnancy weight, we imputed pre-pregnancy weight, using as predictors maternal age and height, and weight and weeks of gestation at the first pre-natal visit. We also calculated pre-pregnancy body mass index (BMI, kg/m2).
We obtained serial pregnancy weights from the clinical obstetric record. We excluded from analysis women who did not have a weight recorded within the 4 weeks preceding delivery. The number of weights measured during pregnancy per participant ranged from 4 to 36; 91% had between 10 and 20 weights available.
Postpartum weights were not available on all women, mainly because women dropped out of the study. Postpartum weights were available for 1179, 1196, 1313 and 1215 women at 6, 12, 24 and 36 months postpartum, respectively. In our analyses of weight retention, we exclude women with intercurrent pregnancies as these would substantially alter the relationship between the weight gain in a prior pregnancy and later weight. There were postpartum weights available for 1179, 1054, 864 and 662 women with no intercurrent pregnancies at 6, 12, 24 and 36 months after the index delivery. Women self-reported their weights at 6, 12 and 24 months postpartum. Research assistants measured weight at 36 months postpartum. We compared self-reported weights with research assistant measured weights in 1133 women with both available at 36 months and found a correlation of 0.99. In this sample, self-report and measured weights are very similar.
We assessed gestational weight gain using four techniques, three based on methods often used in the literature and one novel method: (i) Difference. We calculated the difference between the self-reported pre-pregnancy weight and the final pre-delivery weight.5, 6, 15, 19, 28, 29 (ii) Linear weekly gain. We estimated the weekly weight gain for each woman using the pre-pregnancy weight as the weight at week 0 and estimating a linear regression across all weights through the final pre-pregnancy weight.1, 7, 14 (iii) Institute of Medicine (IOM) category. We determined whether a woman was below, within, or above the weight gain range recommended by the IOM for her pre-pregnancy BMI.30 We combined the low and appropriate weight gain categories because few women had low weight gain.
Finally, we introduce (iv) the area under the gestational weight gain curve (AUC). This measures the area between the woman’s weight trend plotted over time and her pre-pregnancy weight. The AUC is an estimate of the additional pound-days, relative to remaining at pre-pregnancy weight, that are carried during pregnancy. We estimated the AUC by summing the areas of the trapezoids formed between successive weight measures and perpendicular lines drawn to the level of the pre-pregnancy weight, over the time from LMP to the last weight measured before delivery. This calculation is illustrated in Figure 1. An example of a trapezoid is defined by the points A, B, C and D; the AUC is the sum of the areas of all such trapezoids. Some women have weights during pregnancy that are smaller than their pre-pregnancy weights. Rather than considering these values as causing negative pound-days, we replaced them with the pre-pregnancy weight.
Figure 1.
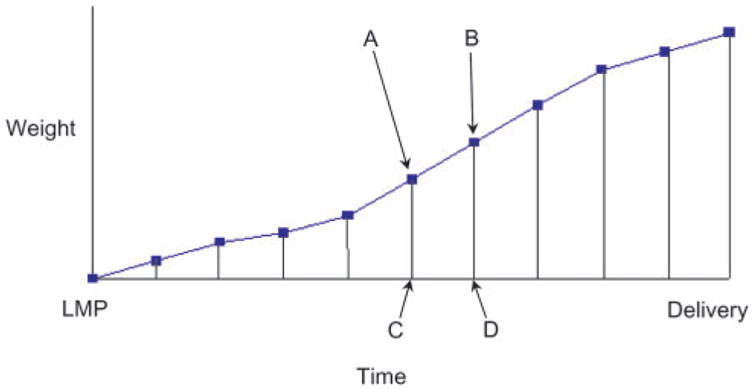
Schematic diagram of gestational weight gain. The x-axis represents time, beginning with the date of the last menstrual period (LMP), the y-axis represents weight, beginning with weight at LMP. The squares represent weights measured during pregnancy, with vertical lines intersecting the date of the measurement. Trapezoids are formed between successive measured weights, e.g. A, B and the corresponding values on the x-axis, e.g. C, D. The area under the curve is calculated by summing all such trapezoids
One feature of the AUC bears particular emphasis: A pound gained on the first day of pregnancy and retained throughout contributes over 200 pound-days to the AUC, while a pound gained on the last day of pregnancy contributes only one pound-day. Thus a total gain of 30 lbs, accrued primarily in the early months of pregnancy, will result in a greater AUC than the same total weight gain accrued later in pregnancy. In contrast to the other three metrics, the AUC incorporates in a single statistic not only the final weight but also the trajectory travelled to reach it.
Others have suggested using only the weight gained after the first trimester, since first trimester weight gain is typically smaller than that in the second and third trimesters, so we also measured the weight gained after the first trimester by three of the above methods (excluding the IOM recommendation).4, 11, 15, 31 We substituted the weight at 98 days gestation for the pre-pregnancy weight in each of the methods. For the linear method, we used only weight measures on or after the 98th day in calculating the weekly gain; for the difference and AUC, we performed a linear interpolation between the two surrounding weight measures to estimate the weight on the 98th day if no day 98 measure was available, and used that weight in place of the pre-pregnancy weight in the earlier described calculations.
We evaluated each gestational weight gain assessment method as a potential predictor of two infant birth outcomes and four postpartum maternal outcomes. The birth outcomes were the birthweight and birthweight-for-gestational-age z-value. The maternal outcomes were the differences between the mother’s weight at 6, 12, 24 and 36 months postpartum and her pre-pregnancy weight. We refer to these values as ‘weight retention’.
Statistical analysis
To compare the utility of the various methods of assessing weight gain, we used the overall F-statistic from linear models predicting each of the outcomes above. The models contained either (i) the weight measure and gestational age at birth, or (ii) additionally: maternal age, pre-pregnancy BMI, height, race/ethnicity, education and smoking behaviour during pregnancy, and infant sex. Each model within a comparison group contains the same number of predictors, so the relative values of the F-statistic reflect the predictive values of the models, as other tools do.32 The numerical values of such model-comparison tools have no intrinsic interpretation. While larger F-statistics indicate improvements to the model, we consider that only a 5% or greater difference between the largest and second-largest value indicates a meaningful advantage for the largest.
Results
Table 1 displays descriptive statistics. Average pre-pregnancy BMI was 24.8 kg/m2; women retained on average 7.9, 1.4, 1.1 and 3.1 pounds at 6, 12, 24 and 36 months postpartum. More than half (52%) of the women gained more than the IOM recommendation for gestational weight gain. Babies weighed 3500 g on average, and the positive mean z-value (0.17) shows that they were slightly heavier than the US median for their gestational ages, on average.
Table 1.
Characteristics of 2016 women enrolled in Project Viva, an ongoing cohort study of pregnant women and their children in Massachusetts
| N (% of 2016) | Mean (SD) | |
|---|---|---|
| Age (years) | 31.9 (5.2) | |
| Weight (lbs, pre-pregancy) | 148.8 (34.6) | |
| Height (m) | 1.65 (0.07) | |
| BMI (kg/m2) | 24.8 (5.46) | |
| Weight retention 6 months postpartum (lbs, N = 1180) | 7.9 (11.2) | |
| Women with no intercurrent pregnancies | ||
| Weight retention 12 months postpartum (lbs, N = 1055) | 1.4 (11.3) | |
| Weight retention 24 months postpartum (lbs, N = 865) | 1.1 (11.3) | |
| Weight retention 36 months postpartum (lbs, N = 663) | 3.07 (14.3) | |
| Gestational age (days) | 277.4 (10.1) | |
| Birthweight (g) | 3500 (525) | |
| Birthweight for gestational age z-value | 0.17 (0.98) | |
| Weight gain per IOM recommendationa | ||
| Low or appropriate | 977 (48) | |
| High | 1039 (52) | |
| Education | ||
| High school diploma or less | 245 (12) | |
| Some college | 465 (23) | |
| College degree | 708 (35) | |
| Post-graduate | 598 (30) | |
| Race/ethnicity | ||
| Asian | 112 (6) | |
| Black | 329 (16) | |
| Hispanic | 148 (7) | |
| White | 1353 (67) | |
| Other | 74 (4) | |
| First pregnancy | ||
| Yes | 612 (30) | |
| No | 1404 (70) | |
IOM recommendation incorporates pre-pregnancy BMI.30
Table 2 shows the differences among the women with no weight available at 6, 12, 24 and 36 postpartum, women with weight available at these times but with an intercurrent pregnancy (who were thus excluded from the analyses of postpartum weight retention) and women included in analyses of postpartum weight. The table shows that the mothers included in the analysis were slightly older, lighter and thinner and that their infants were slightly heavier as well as heavier for their gestational age. The mothers who are included in the analysis were also much better educated, more likely to be white, and somewhat less likely to be primiparous in the index pregnancy.
Table 2.
Mean or percentage for variables measured on women and children among women missing outcome data, used in the analyses of weight retention, or with intercurrent pregnancies by 1, 2 or 3 years postpartum
| 6-month missing | 6-month used | 1-year missing | 1-year Intercurrent | 1-year used | 2-year missing | 2-year Intercurrent | 2-year used | 3-year missing | 3-year inter-current | 3-year used | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 835 | 1179 | 818 | 142 | 1054 | 701 | 449 | 864 | 799 | 553 | 662 |
| Age (years) | 31.1 | 32.4 | 31.0 | 30.3 | 32.7 | 30.7 | 31.0 | 33.2 | 31.0 | 31.0 | 33.6 |
| Weight (lbs, pre-pregancy) | 150.6 | 147.5 | 152.5 | 144.6 | 146.5 | 151.0 | 142.8 | 150.1 | 151.7 | 142.2 | 150.8 |
| BMI (kg/m2) | 25.16 | 24.6 | 25.5 | 24.0 | 24.4 | 25.3 | 23.8 | 25.0 | 25.4 | 23.7 | 25.1 |
| Birthweight (g) | 3481.7 | 3513.7 | 3469.4 | 3415.7 | 3535.9 | 3457.2 | 3503.9 | 3533.7 | 3478.0 | 3502.8 | 3525.4 |
| Birthweight for gestational age z-value | 0.144 | 0.198 | 0.11 | 0.04 | 0.242 | 0.08 | 0.19 | 0.24 | 0.13 | 0.16 | 0.24 |
| Education (%) | |||||||||||
| High school diploma or less | 19 | 7 | 19 | 11 | 7 | 21 | 7 | 8 | 18 | 7 | 9 |
| Some college | 26 | 21 | 28 | 23 | 19 | 28 | 16 | 23 | 28 | 15 | 24 |
| College degree | 33 | 37 | 32 | 33 | 38 | 29 | 40 | 37 | 32 | 39 | 35 |
| Post-graduate | 23 | 35 | 21 | 32 | 36 | 21 | 37 | 33 | 21 | 38 | 32 |
| Race/ethnicity (%) | |||||||||||
| Asian | 6 | 5 | 7 | 5 | 5 | 7 | 5 | 5 | 6 | 6 | 5 |
| Black | 21 | 13 | 24 | 14 | 11 | 24 | 8 | 14 | 22 | 9 | 16 |
| Hispanic | 9 | 6 | 10 | 9 | 5 | 11 | 6 | 5 | 10 | 5 | 7 |
| White | 60 | 72 | 55 | 66 | 76 | 55 | 77 | 72 | 60 | 76 | 69 |
| Other | 4 | 3 | 4 | 6 | 3 | 4 | 4 | 3 | 2 | 5 | 4 |
| First pregnancy | |||||||||||
| Yes | 28 | 32 | 28 | 39 | 31 | 30 | 45 | 23 | 30 | 48 | 16 |
| No | 72 | 68 | 72 | 61 | 69 | 70 | 55 | 77 | 70 | 52 | 84 |
Table 3 contains descriptive statistics for the three continuous measures of weight gain in the two different periods. Over their entire pregnancies, women carried an average extra 3997 pound-days, gaining an average 34.5 pounds at a rate of 0.96 pounds per week. After the 98th day of gestation, women carried an extra 2337 pound-days relative to their weight at day 98 of pregnancy, gaining an average 27.3 pounds at a rate of 1.13 pounds per week. Note the skewed distribution, with outlying women who carried many extra pound-days. Women carried only about half their extra pound-days after the 98th day, while about three-quarters of their weight were gained in this period.
Table 3.
Descriptive statistics of gestational weight gain measures
| Measures on full pregnancy | Mean | SD | Median | 25% | 75% |
|---|---|---|---|---|---|
| AUC (pound-days)a | 3996.7 | 1876.6 | 3915.3 | 2935.8 | 5098.8 |
| Difference (lbs)b | 34.5 | 12.5 | 34.0 | 27.0 | 42.0 |
| Linear (lbs/week)c | 0.96 | 0.33 | 0.96 | 0.77 | 1.16 |
| Measures excluding first 97 days | |||||
| AUC (pound-days)a | 2337.2 | 1022.7 | 2367.9 | 1775.7 | 2929.5 |
| Difference (lbs)b | 27.3 | 10.2 | 27.1 | 21.2 | 33.1 |
| Linear (lbs/week)c | 1.13 | 0.42 | 1.12 | 0.87 | 1.37 |
From 2016 women enrolled in Project Viva, an ongoing cohort study of pregnant women and their children in Massachusetts.
AUC: area under the gestational weight gain curve.
Difference between baseline and immediate pre-delivery weight.
Regression-estimated linear weight gain.
Table 4 shows the weight gain measures for the women who dropped out, were retained but had intercurrent pregnancies, or were included in the analyses of weight retention at 6, 12, 24 and 36 months postpartum. The table shows that the included women carried somewhat fewer excess pound-days in general, generally gained slightly fewer pounds and gained about the same number of pounds per week.
Table 4.
Mean weight gain measures among women missing outcome data, used in the analyses of weight retention, or with intercurrent pregnancies by 1, 2 or 3 years postpartum
| 6-month missing | 6-month used | 1-year missing | 1-year intercurrent | 1-year used | 2-year missing | 2-year intercurrent | 2-year used | 3-year missing | 3-year intercurrent | 3-year used | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 835 | 1179 | 818 | 142 | 1054 | 701 | 449 | 864 | 799 | 553 | 662 |
| AUC (pound-days)a | 4075.2 | 3939.9 | 4115.4 | 3830.8 | 3925.7 | 4109.9 | 4073.1 | 3863.6 | 4037.2 | 4111.1 | 3850.2 |
| Difference (lbs)b | 34.8 | 34.3 | 34.9 | 35.1 | 34.1 | 35.06 | 35.8 | 33.4 | 34.4 | 36.1 | 33.2 |
| Linear (lbs/week)c | 0.963 | 0.960 | 0.96 | 0.99 | 0.96 | 0.97 | 1.01 | 0.93 | 0.95 | 1.01 | 0.93 |
| Measures excluding first 97 days | |||||||||||
| AUC (pound-days)a | 2334.4 | 2340.8 | 2318.3 | 2411.4 | 2343.6 | 2299.0 | 2499.2 | 2286.2 | 2306.4 | 2483.9 | 2254.5 |
| Difference (lbs)b | 27.2 | 27.4 | 27.1 | 28.9 | 27.3 | 27.2 | 28.9 | 26.2 | 26.9 | 29.0 | 26.3 |
| Linear (lbs/week)c | 1.119 | 1.132 | 1.113 | 1.2 | 1.13 | 1.13 | 1.19 | 1.09 | 1.11 | 1.20 | 1.08 |
AUC: area under the gestational weight gain curve.
Difference between baseline and immediate pre-delivery weight.
Regression-estimated linear weight gain.
Table 5 shows the best measures of weight gain for predicting the six outcomes. For birthweight, no measure shows greater predictive value. For predicting maternal weight retention at 6 months, the simple number of pounds gained was superior to any other method of weight gain assessment. For longer-term weight retention at 12, 24 or 36 months postpartum, the AUC was usually superior. Note the absence of post 98th-day weight gain measures; these methods were markedly inferior to the full-pregnancy methods in every case.
Table 5.
Most-predictive measures of gestational weight gain for various outcomes
| Birthweight-for- gestational-age z-value | Birthweight | Weight retention 6 months | |
|---|---|---|---|
| Models | |||
| GWG +Ga | Difference | Difference | Differencec |
| GWG +CG | Linearb | Linear | Difference |
| Weight | Weight | Weight | |
| retention | retention 2 | retention 3 | |
| 1 year | years | years | |
| Models | |||
| GWG +Ga | AUC | AUC | AUC |
| GWG +CG | AUC | AUC | AUC |
Institute of Medicine status30 is excluded from this set of comparisons, as it implicitly includes BMI as a covariate.
Linear: regression-estimated Linear weekly rate of gain.
Difference: difference between baseline and immediate pre-delivery weight.
AUC, area under the gestational weight gain curve GWG, gestational weight gain measured by one of the four methods: ‘Difference’, ‘Linear’, ‘IOM’, or ‘AUC’; G, Gestational length; C, additional covariates: infant sex and mother’s age, pre-pregnancy BMI, height, race/ ethnicity, education and smoking behaviour during pregnancy.
Models included gestational weight gain measured any of four ways during both the full pregnancy and only after the 98th day. Measure with the largest F-statistic is shown; measure appears in bold type if the F-statistic for the model was greater by 5% or more than the next largest F-statistic, in plain type otherwise. Table results include only models for the full pregnancy because the models using data after 98th day were universally inferior.
In Table 6 we provide the full data used to generate Table 5. The table provides a sense of summarizing necessary to combine all of the results into Table 5, and demonstrates the degree of superiority achieved by the AUC for later time points.
Table 6.
Values of F-statistics for each measure, proportional to the F-statistic obtained when using the area under the curve method (1.00)
| Birthweight-for- gestational-age z-value (N = 2016) | Birthweight (N = 2016) | Six-months weight retention (N = 1180) | One-year weight retention (N = 1055) | Two-years weight retention (N = 865) | Three-years weight retention (N = 663) | |
|---|---|---|---|---|---|---|
| GWG +G | ||||||
| AUC (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| AUC 98 | 1.04 | 1.01 | 0.28 | 0.33 | 0.09 | 0.10 |
| Linear | 1.15 | 1.04 | 0.79 | 0.75 | 0.45 | 0.45 |
| Linear 98 | 0.98 | 1.00 | 0.43 | 0.40 | 0.17 | 0.12 |
| Difference | 1.16 | 1.04 | 1.07 | 0.93 | 0.71 | 0.68 |
| Difference 98 | 1.11 | 1.02 | 0.46 | 0.41 | 0.17 | 0.15 |
| GWG +CG | ||||||
| AUC (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| AUC 98 | 1.02 | 1.01 | 0.37 | 0.59 | 0.45 | 0.53 |
| Linear | 1.08 | 1.05 | 0.85 | 0.85 | 0.65 | 0.69 |
| Linear 98 | 1.02 | 1.01 | 0.51 | 0.63 | 0.49 | 0.54 |
| Difference | 1.08 | 1.04 | 1.09 | 0.97 | 0.82 | 0.82 |
| Difference 98 | 1.05 | 1.03 | 0.52 | 0.64 | 0.49 | 0.56 |
| IOM | 0.99 | 1.00 | 0.64 | 0.58 | 0.53 | 0.78 |
GWG, gestational weight gain measured by one of the four methods: ‘Difference’, ‘Linear’, ‘IOM’, or ‘AUC’; G, Gestational age; C, additional covariates: infant sex and mother’s age, pre-pregnancy BMI, height, race/ethnicity, education and smoking behavior during pregnancy.
Methods labelled ‘98’ used data only from the 98th day forward; others used data from the entire pregnancy.
We did not include the IOM status among the weight measures in models that included only weight gain and gestational age as predictors, i.e. in the first rows of Tables 5 and 6. The IOM recommendation varies based on BMI, meaning essentially that the BMI is included as a covariate in any model including the IOM recommendation status. In comparison (data not shown) between IOM status and other measures in models including only gestational age, the IOM method was superior. However, in comparison (data not shown) between the IOM method and other measures, including only gestational age and BMI as covariates, the other measures were superior.
Discussion
In this article, we have compared several measures of gestational weight gain, including those most frequently used in the literature and a novel measure, AUC. For birth-weight and gestational-age-adjusted birthweight, none of the included measures of gestational weight gain meets our criteria for superior prediction. In contrast, for weight retention at 6 months postpartum, total gain is a better predictor than how fast or in what pattern the weight was gained. For weight retention at 1, 2 or 3 years, the AUC, which incorporates both the pattern and amount of weight gain, is more predictive.
There is a plausible biological reason why the pattern of weight gain may be important for longer-term post-pregnancy weight retention. It has been argued that weight gain in the last trimester primarily reflects fetal growth and weight gain early in pregnancy primarily reflects accumulation of maternal fat stores.30 If this is the case, it would make sense that a higher AUC, possibly reflecting earlier gain and thus greater gain of maternal stores, may predict a more difficult time losing this weight after pregnancy.
Total weight gain is the most commonly employed measurement of gestational weight gain.5, 6, 15, 19, 33, 34 A variation on this method is net weight gain, in which the weight of the infant and placenta is subtracted from total weight gain.11, 19, 35, 36 A second variation on total weight gain is total proportional weight gain, defined as the total or net weight gain divided by the mother’s pre-pregnancy BMI.37, 38 Because none of these approaches adjust for gestational age, the weight gain-birthweight relationship is confounded by length of gestation: longer pregnancies allow both mother and fetus more time to gain weight. This limitation also applies to the AUC and is discussed in that light subsequently.
To adjust for gestation length, several studies have used rate of weight gain. Different studies have used the entire pregnancy,39, 40 individual trimesters8, 12, 41 or specific weeks.2, 10, 11, 13, 42, 43 The present analysis used linear regression to estimate the rate of weight gain.1, 7, 14 The principal limitation to using overall rate of gain, arrived at by any method, is the false assumption of linearity of gain. In contrast, while calculating different rates of weight gain for pre-defined sections of pregnancy can provide a more accurate (curvilinear) picture of the weight gain pattern, these different rates generate other problems. For example, it is difficult to interpret 9 monthly or even three trimester-specific rates simultaneously.
Two groups have fit the weight gain pattern to a quadratic curve.14, 40 However, data provided by Carmichael and colleagues14 and representative examples from our own cohort (data not shown) demonstrate that in many individuals gestational weight gain slows in the final weeks before delivery, in contrast to the steep upward slope typically predicted by quadratic models of gestational weight gain. In addition, interpretation of the resulting linear and quadratic slopes is at least as difficult as interpreting many linear slopes. This method has not been widely adopted by subsequent publications and thus was not used as a comparison measure in this analysis.
We included measures based on only the second and third trimesters, as suggested by others.4, 11, 15, 31 This approach reduced the predictive value of all methods for all outcomes. We conclude that weight gain during the first trimester is important in predicting both birthweight and weight retention using any of these methods. A reviewer suggested that in light of the current results, one might assess first-trimester weight gain as a predictor of future weight retention; this is an interesting idea, and studies of weight retention may benefit from examining that possibility.
The AUC, as presented, is correlated with the length of gestation. We considered an alternative method of calculating the AUC, namely truncating the measure at 259 days (37 weeks) and calculating the area under the weight gain curve between LMP and 259 days. This value is calculable for all term pregnancies. We also calculated the difference and weekly gain between LMP and 259 days. The results were similar to those described fully above, namely that the summary results presented in Table 5 were unchanged. Thus future researchers who are troubled by the correlation between gestation length and weight measures may calculate term-independent measures of pregnancy weight gain and still be guided by the results presented in full above.
Some limitations of our analysis bear further comment. Our models for weight retention exclude breastfeeding practice. We excluded breastfeeding because it may be situated in the causal pathway between weight gain and weight retention. Women with higher gestational weight gain tend to have lower breastfeeding initiation rates and earlier termination44, 45 while breastfeeding may accelerate postpartum weight loss. Another potential problem with our analysis is that pre-pregnancy and 6-, 12- and 24-month postpartum weights were self-reported, weights during pregnancy were recorded clinically and 36-month postpartum weights were measured according to a research standard. In general, we would expect that the errors in measurement due to the clinical and self-reported weights would affect each weight gain measure equally. Study participants were generally older, wealthier and better-educated individuals than the pregnant population at large. The women and infants included in the analyses were also older, better educated and more likely to be white than the women on whom follow-up weight data could not be obtained. As such, these results may not be generalizable to the low-income or higher-risk cohorts studied in past analyses.8–13, 37 Women included in the analyses also gained somewhat less weight during pregnancy than women on whom follow-up weight data could not be obtained, according to any of the weight gain metrics discussed. However, this discrepancy was too small to be likely to affect the conclusions here.
The AUC method encompasses two important characteristics of gestational weight gain—total gain and timing of gain—in one variable. Thus the AUC will distinguish a woman who gains weight at a constant rate from a woman who gains the same amount of weight, but predominantly at the beginning or end of her pregnancy. This distinction is lost with difference-based weight gain measurements. In addition, the AUC incorporates all of the observed weight data with limited parametric assumptions. The importance of the pattern of weight gain is illustrated in our results regarding postpartum weight retention. These results suggest that a pattern of weight gain characterized by gain earlier in pregnancy is predictive of longer-term weight retention, a finding that agrees with previous studies using different methods to assess early weight gain.42
The area under the gestational weight gain curve is a relatively simple assessment of gestational weight gain that does not rely on assumptions about the shape of the weight gain curve. The AUC is reported as pound-days, a readily interpretable metric, and incorporates information about both the amount and the timing of gain. If longer-term maternal outcomes are to be studied, the AUC appears to be the best assessment of gestational weight gain. Future studies are needed to investigate whether it is a superior measure for other pregnancy or post partum outcomes of interest as well. We anticipate that the AUC will serve as a useful method for the assessment of gestational weight gain by epidemiologists.
KEY MESSAGES.
Gestational weight gain is correlated with infant growth and may be related to important health outcomes.
Methods currently used to measure gestational weight gain at best needlessly simplify a complex process and at worst incorporate false assumptions; this can lead to mistaken conclusions about the association between weight gain and potential correlates.
We propose a new measure of gestational weight gain, the area under the pregnancy weight gain curve, and show that it is a superior predictor of long-term weight retention than traditional measures such as the total weight gained and the weight gain per week.
The new measure may be a useful tool for assessing risk of weight retention at 1 year postpartum and beyond.
Acknowledgments
This work was supported in part by NIH grants HD34568, HL64925 and HL68041. The authors appreciate the assistance of Sheryl Rifas-Shiman, MPH, in preparing data sets used in the article.
Footnotes
Conflict of interest: None declared.
References
- 1.Abrams B, Selvin S. Maternal weight gain patterns and birth weight. Obstet Gynecol. 1995;86:163–69. doi: 10.1016/0029-7844(95)00118-b. [DOI] [PubMed] [Google Scholar]
- 2.Scholl TO, Hediger ML, Schall JI, Ances IG, Smith WK. Gestational weight gain, pregnancy outcome, and postpartum weight retention. Obstet Gynecol. 1995;86:423–27. doi: 10.1016/0029-7844(95)00190-3. [DOI] [PubMed] [Google Scholar]
- 3.Scholl TO, Hediger ML, Ances IG, Belsky DH, Salmon RW. Weight gain during pregnancy in adolescence: predictive ability of early weight gain. Obstet Gynecol. 1990;75:948–53. [PubMed] [Google Scholar]
- 4.Hickey CA, Cliver SP, McNeal SF, Hoffman HJ, Goldenberg RL. Prenatal weight gain patterns and birth weight among nonobese black and white women. Obstet Gynecol. 1996;88:490–96. doi: 10.1016/0029-7844(96)00262-1. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell MC, Lerner E. Weight gain and pregnancy outcome in underweight and normal weight women. J Am Diet Assoc. 1989;89:634–38. [PubMed] [Google Scholar]
- 6.Ogunyemi D, Hullett S, Leeper J, Risk A. Prepregnancy body mass index, weight gain during pregnancy, and perinatal outcome in a rural black population. J Matern-Fetal M. 1998;7:190–93. doi: 10.1002/(SICI)1520-6661(199807/08)7:4<190::AID-MFM5>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 7.Schieve LA, Cogswell ME, Scanlon KS, et al. Prepregnancy body mass index and pregnancy weight gain: associations with preterm delivery. Obstet Gynecol. 2000;96:194–200. doi: 10.1016/s0029-7844(00)00883-8. [DOI] [PubMed] [Google Scholar]
- 8.Siega-Riz AM, Adair LS, Hobel CJ. Institute of medicine maternal weight gain recommendations and pregnancy outcome in a predominantly Hispanic population. Obstet Gynecol. 1994;84:565–73. [PubMed] [Google Scholar]
- 9.Wen SW, Goldenberg RL, Cutter GR, Hoffman HJ, Cliver SP. Intrauterine growth retardation and preterm delivery: prenatal risk factors in an indigent population. Am J Obstet Gynecol. 1990;162:213–18. doi: 10.1016/0002-9378(90)90853-y. [DOI] [PubMed] [Google Scholar]
- 10.Siega-Riz AM, Adair LS, Hobel CJ. Maternal underweight status and inadequate ate of weight gain during the third trimester of pregnancy increases the risk of preterm delivery. J Nutr. 1996;126:146–53. doi: 10.1093/jn/126.1.146. [DOI] [PubMed] [Google Scholar]
- 11.Spinillo A, Capuzzo E, Piazzi G, Ferrari A, Morales V, Di Mario M. Risk for spontaneous preterm delivery by combined body mass index and gestational weight gain patterns. Acta Obstet Gyn Scan. 1998;77:32–36. [PubMed] [Google Scholar]
- 12.Hickey CA, Cliver SP, McNeal SF, Hoffman HJ, Goldenberg RL. Prenatal weight gain patterns and spontaneous preterm birth among nonobese black and white women. Obstet Gynecol. 1995;85:909–14. doi: 10.1016/0029-7844(95)00067-2. [DOI] [PubMed] [Google Scholar]
- 13.Hediger ML, Scholl TO, Belsky DH, Ances IG, Salmon RW. Patterns of weight gain in adolescent pregnancy: effects on birth weight and preterm delivery. Obstet Gynecol. 1989;74:6–12. [PubMed] [Google Scholar]
- 14.Carmichael S, Abrams B, Selvin S. The association of pattern of maternal weight gain with length of gestation and risk of spontaneous preterm delivery. Paediatr Perinat Ep. 1997;11:392–406. doi: 10.1046/j.1365-3016.1997.d01-28.x. [DOI] [PubMed] [Google Scholar]
- 15.Keppel KG, Taffel SM. Pregnancy-related weight gain and retention: implications of the 1990 Institute of Medicine guidelines. Am J Public Health. 1993;83:1100–3. doi: 10.2105/ajph.83.8.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.To WWK, Cheung W. The relationship between weight gain in pregnancy, birth-weight and postpartum weight retention. Aust Nz J Obstet Gyn. 1998;38:176–79. doi: 10.1111/j.1479-828x.1998.tb02996.x. [DOI] [PubMed] [Google Scholar]
- 17.Luke B, Hediger M, Scholl T. Point of diminishing returns: when does gestational weight gain cease benefiting birth weight and begin adding to maternal obesity. J Matern Fetal Med. 1996;5:168–73. doi: 10.1002/(SICI)1520-6661(199607/08)5:4<168::AID-MFM2>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 18.Olson CM, Strawderman MS, Hinton PS, Pearson TA. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1y postpartum. Int J Obesity. 2003;27:117–27. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 19.Johnson JW, Longmate JA, Frentzen B. Excessive maternal weight and pregnancy outcome. Am J Obstet Gynecol. 1992;167:353–72. doi: 10.1016/s0002-9378(11)91414-8. [DOI] [PubMed] [Google Scholar]
- 20.Young TK, Woodmansee B. Factors that are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol. 2002;187:312–20. doi: 10.1067/mob.2002.126200. [DOI] [PubMed] [Google Scholar]
- 21.Witter FR, Caulfield LE, Stoltzfus RJ. Influence of maternal anthroprometric status and birth weight on the risk of cesarean delivery. Obstet Gynecol. 1995;85:947–51. doi: 10.1016/0029-7844(95)00082-3. [DOI] [PubMed] [Google Scholar]
- 22.Parker J, Abrams B. Prenatal weight gain advice: an examination of the recent prenatal weight gain recommendations of the Institute of Medicine. Obstet Gynecol. 1992;79:664–69. [PubMed] [Google Scholar]
- 23.Gillman MW, Rich-Edwards JW, Rifas-Shiman SL, Lieberman ES, Kleinman KP, Lipshultz SE. Maternal age and other predictors of newborn blood pressure. J Pediatr. 2004;144:240–45. doi: 10.1016/j.jpeds.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 24.World Medical Association. World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. J Amer Med Assoc. 1997;277:925–26. [PubMed] [Google Scholar]
- 25.Oken E, Kleinman KP, Rich-Edwards JW, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stewart AL. The reliability and validity of self-reported weight and height. J Chron Dis. 1982;35:295–309. doi: 10.1016/0021-9681(82)90085-6. [DOI] [PubMed] [Google Scholar]
- 27.Palta M, Prineas RJ, Berman R, Hannan P. Comparison of self-reported and measured height and weight. Am J Epidemiol. 1982;115:223–30. doi: 10.1093/oxfordjournals.aje.a113294. [DOI] [PubMed] [Google Scholar]
- 28.Berenson AB, Wiemann CM, Rowe TF, Rickert VI. Inadequate weight gain among pregnant adolescents: risk factors and relationship to infant birth weight. Am J Obstet Gynecol. 1997;176:1220–24. doi: 10.1016/s0002-9378(97)70338-7. [DOI] [PubMed] [Google Scholar]
- 29.Bianco AT, Smilen SW, Davis Y, Lopez S, Lapinski R, Lockwood CJ. Pregnancy outcome and weight gain recommendations for the morbidly obese woman. Obstet Gynecol. 1998;91:97–102. doi: 10.1016/s0029-7844(97)00578-4. [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine. Nutrition During Pregnancy . Part I, Weight Gain. Washington, DC: National Academy Press; 1990. [Google Scholar]
- 31.Strauss RS, Dietz WH. Low maternal weight gain in the second or third trimester increases the risk for intrauterine growth retardation. J Nutr. 1999;129:988–93. doi: 10.1093/jn/129.5.988. [DOI] [PubMed] [Google Scholar]
- 32.Akaike H. A new look at statistical model identification. IEEE T Automat Contr. 1974;19:716–23. [Google Scholar]
- 33.Kramer MS, McLean FH, Eason EL, Usher RH. Maternal nutrition and spontaneous preterm birth. Am J Epidemiol. 1992;136:574–83. doi: 10.1093/oxfordjournals.aje.a116535. [DOI] [PubMed] [Google Scholar]
- 34.Schieve LA, Cogswell ME, Scanlon KS. Maternal weight gain and preterm delivery: differential effect by body mass index. Epidemiology. 1999;10:141–47. doi: 10.1097/00001648-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Shepard MJ, Saftlas AF, Leo-Summers L, Bracken MB. Maternal anthropometric factors and risk of primary cesarean delivery. Am J Public Health. 1998;88:1534–38. doi: 10.2105/ajph.88.10.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shepard MJ, Hellenbrand KG, Bracken MB. Proportional weight gain and complications of pregnancy, labor, and delivery in healthy women of normal prepregnant stature. Am J Obstet Gynecol. 1986;155:947–54. doi: 10.1016/0002-9378(86)90323-6. [DOI] [PubMed] [Google Scholar]
- 37.Abrams B, Newman V, Key T, Parker J. Maternal weight gain and preterm delivery. Obstet Gynecol. 1989;74:577–83. [PubMed] [Google Scholar]
- 38.Caulfield LE, Stoltzfus RJ, Witter FR. Implications of the institute of medicine weight gain recommendations for preventing adverse pregnancy outcomes in black and white women. Am J Public Health. 1998;88:1168–74. doi: 10.2105/ajph.88.8.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dawes MG, Grudzinskas JG. Patterns of maternal weight gain in pregnancy. Brit J Obstet Gynaec. 1991;98:195–201. doi: 10.1111/j.1471-0528.1991.tb13368.x. [DOI] [PubMed] [Google Scholar]
- 40.Villamor E, Gofin R, Adler B. Maternal anthropometry and pregnancy outcome among Jerusalem women. Ann Hum Biol. 1998;25:331–43. doi: 10.1080/03014469800005682. [DOI] [PubMed] [Google Scholar]
- 41.Brown JE, Murtaugh MA, Jacobs DR, Jr, Margellos HC. Variation in newborn size according to pregnancy weight change by trimester. Am J Clin Nutr. 2002;76:205–9. doi: 10.1093/ajcn/76.1.205. [DOI] [PubMed] [Google Scholar]
- 42.Muscati S, Gray-Donald K, Koshi K. Timing of weight gain during pregnancy: promoting fetal growth and minimizing maternal weight retention. Int J Obesity. 1996;20:526–32. [PubMed] [Google Scholar]
- 43.Neufeld LM, Haas JD, Grajeda R, Martorell R. Changes in maternal weight from the first to second trimester of pregnancy are associated with fetal growth and infant length at birth. Am J Clin Nutr. 2004;79:646–52. doi: 10.1093/ajcn/79.4.646. [DOI] [PubMed] [Google Scholar]
- 44.Hilson JA, Rasmussen KM, Kjolhede CL. Excessive weight gain during pregnancy is associated with earlier termination of breast-feeding among white women. J Nutr. 2006;136:140–46. doi: 10.1093/jn/136.1.140. [DOI] [PubMed] [Google Scholar]
- 45.Li R, Jewell S, Grummer-Strawn L. Maternal obesity and breast-feeding practices. Am J Clin Nutr. 2003;77:931–36. doi: 10.1093/ajcn/77.4.931. [DOI] [PubMed] [Google Scholar]


