Abstract
Azithromycin is a major drug used in the treatment and prophylaxis of chlamydial infections. Spontaneous azithromycin-resistant mutants of Chlamydia psittaci 6BC were isolated in vitro in the plaque assay at a frequency of about 10−8. Isogenic clonal variants with A2058C, A2059G, or A2059C mutations in the unique 23S rRNA gene (Escherichia coli numbering system) displayed MICs for multiple macrolides (i.e., azithromycin, erythromycin, josamycin, and spiramycin) at least 100 times higher than those of the parent strain and were also more resistant to the lincosamide clindamycin. Chlamydia trachomatis L2 variants with a Gln-to-Lys substitution in ribosomal protein L4 at position 66 (E. coli numbering system), conferring an eightfold decrease in azithromycin and erythromycin sensitivities and a fourfold decrease in josamycin and spiramycin sensitivities, were isolated following serial passage in subinhibitory concentrations of azithromycin. Each mutation was stably maintained in the absence of selection but severely affected chlamydial infectivity, as determined by monitoring the development of each isolate over 46 h in the absence of selection, in pure culture or in 1:1 competition with the isogenic parent. Data in this study support the hypothesis that the mechanisms which confer high-level macrolide resistance in chlamydiae carry a prohibitive physiological cost and may thus limit the emergence of highly resistant clones of these important pathogens in vivo.
The Chlamydiaceae are etiological agents of many important human and animal diseases. Formerly called Chlamydia, with only two recognized species 25 years ago (Chlamydia trachomatis and Chlamydia psittaci), the family now contains nine species divided into two genera, Chlamydia and Chlamydophila (9). As many believe the genus division unnecessary, we refer to both genera as Chlamydia for simplicity. These gram-negative bacteria are obligate intracellular organisms that are transmitted as metabolically inactive particles called elementary bodies (EBs). Once inside a host cell, the EB reorganizes morphologically into a reticulate body (RB), within a membrane-bound vacuole known as an inclusion, to grow and replicate by binary fission. Later in the developmental cycle—18 to 48 h postinfection, depending on the species—RBs redifferentiate back to EBs and exit the cell to repeat the cycle (1).
The obligate intracellular nature of these pathogens and their unique biphasic lifestyle pose challenges for the treatment of associated infections (53). Indeed, an efficient antichlamydial drug not only must achieve adequate intracellular penetration and concentration but also must be able to inhibit the metabolically active form of the organism (RBs) in its ability to undergo DNA or protein synthesis, cell division, or differentiation into infectious particles (EBs). Currently, the recommended first-line therapeutic regimens for chlamydial infections are the tetracyclines and the macrolide azithromycin (AZM), which inhibit bacterial translation by binding to the 30S and 50S ribosomal subunits, respectively (53). In addition to its chemotherapeutic use, AZM is used for chemoprophylaxis of blinding trachoma, a chronic infection caused by ocular serovars of C. trachomatis, common in developing countries (15).
Although chlamydial infections are characterized by a high recurrence rate despite appropriate drug therapy (23), the majority of clinical failures has been attributed to reinfection or relapse following deviation of the organism to persistent, nonreplicating chlamydial forms that are phenotypically antibiotic resistant but can revert to typical RBs at the end of the treatment (22). On the other hand, clinical failures linked to true genotypic resistance due to chromosomal mutations have rarely been reported, suggesting that mutations which confer antibiotic resistance in chlamydiae are not selected for in vivo (23, 61).
Resistance to ribosome-targeting antibiotics due to mutations in rRNA genes has been observed mainly in pathogens possessing a low copy number of rRNA operons, because the selective advantage of a mutation in one rRNA copy is usually masked by the abundance of wild-type drug-sensitive rRNAs transcribed from the other unmutated gene copy (or copies) (49). Interestingly, the Chlamydiaceae harbor either one or two rRNA operons depending on the species, implying that resistance to the current antichlamydial drugs could emerge from ribosomal mutations. Previously, we showed that spontaneous resistant mutants of C. psittaci 6BC with distinct mutations in the unique 16S rRNA gene could be isolated in the plaque assay in the presence of the aminoglycoside spectinomycin (at a frequency of 5 × 10−5) but not in the presence of tetracycline, another 16S-targeting antibiotic (frequency, <3 × 10−9) (6, 7). Because the physiological burden of resistance mutations is an important factor that affects the appearance, stability, and maintenance of the phenotype (3, 27), we suggested that chromosomal point mutations conferring resistance to tetracycline incurred a high fitness cost for the bacteria that was reflected in the rarity of genotypic antibiotic resistance among chlamydial clinical isolates. Indeed, stable tetracycline resistance in chlamydiae has been reported only for Chlamydia suis, and this resistance probably arose from horizontal gene transfer rather than spontaneous genetic mutations affecting the bacterial ribosome (13).
In this study, we examined the contribution of spontaneous chromosomal mutation to emergence of AZM resistance in chlamydiae in vitro. AZM-resistant chlamydial isolates were isolated either in the plaque assay using a clonal population of C. psittaci 6BC (one rRNA operon) or following serial passages in AZM for C. trachomatis L2, which harbors two rRNA operons. We found that mutations in the unique C. psittaci 23S rRNA gene at position 2058 or 2059 (Escherichia coli numbering system) and in C. trachomatis ribosomal protein L4 lowered bacterial sensitivities to multiple antibiotics. However, these mutations were associated with a high physiological burden, as evidenced by a reduced production of infectious particles in tissue culture in the absence of antibiotic. The implications of these results for the use of macrolides in treatment of chlamydial infections are discussed.
MATERIALS AND METHODS
Propagation of C. psittaci, C. trachomatis, and L2 cells.
C. psittaci serovar 6BC and C. trachomatis serovar L2/LGV/434/Bu were grown in mouse fibroblast L2 cells as described in reference 7. Infectious particles from a single plaque purified in the plaque assay from our laboratory stock of C. psittaci 6BC were expanded for five developmental cycles to obtain the recent clonal and therefore genetically homogeneous population BCRB. On the other hand, the laboratory stocks of C. psittaci 6BC and C. trachomatis L2 have been propagated for many years without any kind of clonal purification and are expected to be polymorphic (17).
Titration and antimicrobial susceptibility testing of C. trachomatis and C. psittaci.
The susceptibilities of the chlamydial strains to AZM, erythromycin (ERM), josamycin (JOS), spiramycin (SPI), clindamycin (CLI), virginiamycin M1 (VIR), and chloramphenicol (CLM) were determined in a plaque assay. The MIC was defined as the drug concentration that inhibited the development of 105 chlamydial PFU in a confluent L2 monolayer in a 60-mm dish (7). All antibiotics were purchased from Sigma Chemical Co.
Isolation of chlamydial mutants.
To isolate spontaneous AZM-resistant variants, 60-mm dishes were infected with 107 to 108 PFU, corresponding to multiplicities of infection (MOI) of 1 and 10, respectively, and AZM was added 2 h postinoculation (p.i.) at concentrations ranging from 200 ng/ml to 1 μg/ml. The frequency of spontaneous mutation to drug resistance was determined by dividing the number of PFU on selective medium by the number of PFU added to the monolayer (as measured by titration of PFU in the absence of antibiotic) (7).
AZM-resistant populations of C. trachomatis L2 were isolated following enrichment by serial passage in subinhibitory concentrations of AZM. Starting with 2 × 109 wild-type C. trachomatis L2 infectious particles, we ended up with a population that grew in the presence of 200 ng/ml of AZM after 30 passages.
To monitor the stability of the resistance phenotype, we compared the number of PFU obtained in the absence or presence of antibiotic following the growth of each variant for a minimum of 14 days in the plaque assay in the absence of AZM.
PCR and DNA sequencing of the macrolide resistance targets.
PCR amplification and DNA sequencing were used to determine whether resistance to AZM was due to a mutation in the 23S rRNA gene or in rplD and rplV (encoding L4 protein and ribosomal L22 protein, respectively). PCR primers are listed in Table 1. Total genomic DNA was prepared from infected cells with DNeasy tissue kits (Qiagen). Alternatively, single plaques were collected in 10 μl sterile H2O and diluted with 230 μl SPG (250 mM sucrose, 10 mM sodium phosphate, 5 mM l-glutamic acid). PCR amplification was then performed on 10 μl of the plaque lysate which had been denatured for 10 min at 96°C beforehand, in a 50-μl reaction mixture using Platinum Taq high-fidelity DNA polymerase (Invitrogen) supplemented with 0.8 μg/ml bovine serum albumin. After 30 cycles, the PCR product was ligated in pGEM-T (Promega) and sequenced with primers annealing to the vector (i.e., PUC-R and PUC-F) or to the insert (Table 1).
TABLE 1.
Primers used for PCR amplification and sequencing
| Primer target and designation | Position(s)a | Sequence (5′ → 3′) |
|---|---|---|
| C. psittaci 6BC 23S rRNAb | ||
| 6BC8 | 3415 | AGCTGTTGATGGTGACCGTAC |
| 23S-R | 4814; C | ACGTATACTAATAGACGCTTAAGAGAG |
| 23SR | 4812; C | GTATACTAATAGACGCTTAAGAGAG |
| C. psittaci 6BC rplDc | ||
| L4-F2 | 108696 | CAGAAGAGGTCCTAATGG |
| L4-R2 | 109447; C | TTCTCGGTTACATAATGCCG |
| C. psittaci 6BC rplVc | ||
| L22-F2 | 110879 | GGGTAAGTCTAAAGGAGAC |
| L22-R2 | 111268; C | TTGGACATCCTTTCTGACCC |
| DNA insert in pCRSCRIPT Cam or pGEM-T cloning vectorsd | ||
| PUC-F | 847; C | AGCGGATAACAATTTCACACAGGAAAC |
| PUC-R | 579 | GGTTTTCCCAGTCACGACGTTGT |
| C. trachomatis L2 23S rRNAe | ||
| 23S-F1 | 855946, 877992 | TGGTGGATGCCTTGGCATTGAC |
| AZM-F | 857854, 879900 | TGAACCTAAGCCCTGGTGAATG |
| rrn1-R3 (allele 1)f | 859716; C | TACGTTTGCGGTCCTGCTCTG |
| rrn2-R (allele 2)f | 881617; C | CCCTATTCACCCATCGAGAATC |
| C. trachomatis L2 rplDe | ||
| L4-F | 595704; C | AAGCGTTCTTGCGGAGTAG |
| L4-R | 594936 | GCCTTCTCGGTCACATAATGTC |
| C. trachomatis L2 rplVe | ||
| L22-F | 593564; C | GACACAAGTTGGGAGAGTTC |
| L22-R | 593130 | GACCCATACCTTACTCCTACTG |
Position in GenBank entry for the first base of the primer. C, complementary strand.
Designed according to the sequence of the C. psittaci 6BC 23S rRNA (GenBank accession number U68447).
Designed based on the respective homologous gene present in the total genome sequences of the closely related C. caviae guinea pig inclusion conjunctivitis strain (reference for primer position), C. felis Fe/C-56, and C. abortus strain S26/3 (GenBank accession numbers AE015925, AP006861, and CR848038, respectively).
Designed using GenBank accession number U46018 for the pCRSCRIPT Cam sequence and GenBank accession number X65308 for the pGEM-T sequence. Primer positions in the pCRSCRIPT Cam vector are indicated.
Designed based on the C. trachomatis D/UW-3/CX complete genome sequence (GenBank accession number AE001273).
Allele-specific primers are downstream of the 23S rRNA.
C. psittaci 6BC rplD and rplV were amplified with Ultra Pfu high-fidelity DNA polymerase (Stratagene) for 15 cycles using primers based on the available genome sequences of the Chlamydia caviae guinea pig inclusion conjunctivitis strain, C. felis Fe/C-56, and C. abortus strain S26/3 (Table 1), cloned in pCRSCRIPT Cam SK(+) (Stratagene) and sequenced on both strands using PUC-F and PUC-R primers.
DNA sequences for each antibiotic resistant isolate were aligned using Clone Manager 8 (Scientific & Educational Software, Durham, NC) and compared to the respective DNA sequence obtained for the wild-type parental strain.
Physiological cost associated with the mutations. (i) Pairwise competition experiment.
C. psittaci 6BC wild-type BCRB and one isogenic representative of each AZM-resistant variant were coinfected at a ratio of ∼ 1:1 to a MOI of 1 in confluent mouse fibroblast monolayers in 60-mm dishes and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed. The cells were washed twice with Dulbecco's modified Eagle medium (DMEM; GIBCO) and incubated in DMEM supplemented with 10% fetal bovine serum, 1× MEM nonessential amino acids (Sigma-Aldrich), and 2 μg of cycloheximide per ml. EBs were harvested in triplicate after sonication of the infected cells at 19, 24, 29, 34, and 46 h p.i. and stored at −80°C in 400 μl SPG. Approximately 8 × 106 infectious particles from the mixed infection obtained at 46 h p.i. were passed a second time into fresh monolayers in 60-mm dishes, allowed to grow for another 46 h, and harvested as before. Titers of serial dilutions of each harvest were determined in duplicate in the plaque assay in both drug-free DMEM (total PFU) and drug-containing DMEM (AZM-resistant PFU). Plaques were counted after 10 days of incubation. The plating efficiency of each resistant mutant was unaffected by the presence of AZM. The twofold PFU increase rate was estimated by using Prism 3.0 software from a plot of ln(PFU) = f(time), where the slope is ln2/twofold PFU increase rate (hours). The competition index was defined as the ratio of the output mutant/wild-type ratio to the input mutant/wild-type ratio (6). Additionally, the sizes of a minimum of 60 plaques formed by each C. psittaci 6BC strain in the absence of selection at 10 days p.i. were determined and averaged.
(ii) Pure culture.
C. trachomatis L2 infectivity was determined while the strains were growing in pure culture in the absence of selection. Confluent mouse fibroblast monolayers in 60-mm dishes were infected with each strain to an MOI of 0.1 and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed and the cells were incubated in DMEM supplemented with 10% fetal bovine serum, 1× MEM nonessential amino acids, and 2 μg of cycloheximide per ml. EBs were harvested in triplicate after sonication of the infected cells at 46 h p.i. and stored at −80°C in 400 μl SPG. Titers of serial dilutions of each harvest were determined in duplicate in the plaque assay in the absence of selection. Plaques were counted after 14 days of incubation. Sizes of 173 C. trachomatis L2 wild-type plaques and 287 and 270 plaques for L2AZM#23 and L2AZM#31, respectively, were determined and averaged. The EB generation rate at 46 h p.i. was defined as the number of total PFU obtained at 46 h p.i. divided by the number of PFU used to infect initially.
Nucleotide sequence accession numbers.
C. psittaci 6BC rplV and rplD sequences determined in the present study have been deposited in GenBank under accession numbers EU035809 and EU035810, respectively.
RESULTS
Genetic characterization of spontaneous AZM-resistant isolates of C. psittaci 6BC.
The introduction of single-dose AZM therapy is an important step forward in the treatment of chlamydial infections. AZM, an azalide-macrolide antibiotic, is stable in acidic environments, with additional pharmacokinetic features such as a low plasma concentration, a long half-life of 35 to 40 h, and an elevated penetration in tissues as well as in immune cells. For example, a single 500-mg dose of AZM given to healthy volunteers results in accumulation of the drug to a level of 2 μg/ml in secretions (epithelial lining fluid) (24).
In our laboratory, sensitivity of Chlamydia spp. to antibiotics is measured in the plaque assay, and the MIC is defined as the concentration of drug that inhibits the development of 105 PFU. The number of input bacteria corresponds to an MOI of 0.01 in a confluent monolayer of L2 mouse fibroblasts in 60-mm dishes (7). The AZM MIC is 100 ng/ml for C. psittaci 6BC. When monolayers were infected with a minimum of 8 × 107 PFU in the presence of AZM ranging from 200 to 1,000 ng/ml, resistant plaques appeared at a frequency of 1.35 × 10−8 ± 0.15 × 10−8 for the laboratory stock of C. psittaci 6BC (population genetically heterogeneous) and 0.75 × 10−8 ± 0.5 × 10−8 for the clonal population BCRB. Fifteen independent AZM-resistant plaques were isolated from both the heterogeneous and the clonal populations of C. psittaci 6BC, expanded in the presence of AZM, and further analyzed.
Biochemical studies have shown that AZM reversibly binds to the large ribosomal subunit in the vicinity of the peptidyl transferase center and causes cell growth arrest due to inhibition of protein synthesis (11, 44, 52, 59). More precisely, AZM interacts with bacterial 23S rRNA by connecting hairpin 35 in domain II of the rRNA and the peptidyl transferase loop in domain V. The sequence of the AZM binding site in the 23S rRNA gene was determined by sequencing approximately 900 nucleotides of the 1,400-bp PCR fragment amplified from the parent strain C. psittaci 6BC and 30 independent AZM-resistant mutants (Table 2). Each mutant showed a single mutation at A2058 or A2059 (E. coli numbering system), both of which are known to confer the highest levels of macrolide resistance in other organisms (60). One AZM-resistant representative of each mutant class, i.e., BCRBAZ1, BCRBAZ2, and BCRBAZ5, was chosen from the C. psittaci 6BC clonal population and expanded for two developmental cycles to perform further phenotypic and physiological characterizations on bacterial populations which were as isogenic as possible (Table 2). Because mutations in ribosomal proteins L4 (rplD) and L22 (rplV) have also been reported to confer macrolide resistance in some organisms (12), we amplified, cloned, and sequenced both genes in the isogenic mutant strains. We did not find any changes in the DNA sequences of these two genes. This result indicates that spontaneous AZM resistance arose in C. psittaci 6BC from single mutations in the unique 23S rRNA gene, resulting in either an A2058C, A2059C, or A2059G mutation.
TABLE 2.
Ribosomal mutations observed in spontaneous AZM-resistant isolates of C. psittaci 6BC
| No. of independent mutants of C. psittaci 6BC isolated from:
|
Representative C. psittaci straina | Nucleotide change in the 23S rRNA geneb | |
|---|---|---|---|
| Laboratory stock | BCRB | ||
| 4 | 7 | BCRBAZ2 | A2058C |
| 4 | 7 | BCRBAZ5 | A2059C |
| 7 | 1 | BCRBAZ1 | A2059G |
Isogenic to the parental isolate BCRB.
E. coli numbering. No change in the L4 or L22 protein was observed.
Resistance phenotypes associated with the 23S rRNA alleles in C. psittaci 6BC.
Genetic and biochemical data have shown that macrolides, lincosamides, and streptogramins B bind to the peptidyl transferase center of 50S ribosomal subunits at sites that are close to each other or overlapping (44, 52, 59, 60). Consequently, mutations conferring resistance to a drug belonging to one of these groups of antibiotics may confer cross-resistance to chemically diverse compounds (60). Macrolides are classified according to the size of the lactone ring they harbor (24), and we found that C. psittaci 6BC was sensitive to the 14-member-ring ERM, the 15-member-ring azalide AZM, and the 16-member-ring JOS and SPI, with MICs of 200 ng/ml, 100 ng/ml, 50 ng/ml, and 1 μg/ml, respectively, in the plaque assay (Table 3). In addition, we observed growth inhibition of C. psittaci 6BC by CLI, a lincosamide antibiotic, and by VIR, a streptogramin A antibiotic, with MICs of 400 ng/ml and 2 μg/ml, respectively, in the plaque assay (Table 3).
TABLE 3.
Resistance phenotypes associated with the 23S rRNA alleles in C. psittaci 6BC
| C. psittaci 6BC strain | 23S rRNA mutationa | MIC (μg/ml) of:
|
||||||
|---|---|---|---|---|---|---|---|---|
| AZM | ERY | JOS | SPI | CLI | VIR | CLM | ||
| BCRB | None | 0.1 | 0.2 | 0.05 | 1 | 0.4 | 2 | 0.4 |
| BCRBAZ2 | A2058C | >20 | >20 | ≥10 | ≥200 | 40 | 2 | 0.4 |
| BCRBAZ5 | A2059C | >20 | >20 | >10 | >200 | 5 | 2 | 0.4 |
| BCRBAZ1 | A2059G | >20 | >20 | >10 | >200 | 40 | 4 | 0.4 |
E. coli numbering.
Since the three AZM-resistant C. psittaci isolates are isogenic, apart from their rRNA mutations, the resistance phenotypes are related directly to the effects of the mutations on drug binding. Although CLM has also been shown to interact with the ribosomal peptidyl transferase cavity (52, 60), BCRBAZ1, BCRBAZ2, and BCRBAZ5 were as sensitive to this drug as the wild-type C. psittaci 6BC parent strain BCRB, indicating that none of the mutations in the 23S rRNA at position 2058 or 2059 affected the binding of CLM to the bacterial ribosome (Table 3). On the other hand, A2058C conferred high-level resistance to AZM and ERM and resulted in significant resistance to the 16-membered-ring macrolides JOS and SPI, as well as to the lincosamide CLI, but had no effect on the interactions of VIR with the ribosome (Table 3). This observation has been reported for other organisms (5, 43, 46). As expected, the A2059C and A2059G mutations were associated with high-level resistance to the four macrolides tested but marginally altered the susceptibility of the ribosomes to VIR (Table 3). Interestingly BCRBAZ5, bearing the A2059C mutation in the 23S rRNA, was not as resistant to CLI as the two other variants, harboring an A2058C or an A2059G transition (i.e., 5 versus 40 μg/ml) (Table 3). A similar observation was recently reported for mycobacteria (45).
The stability of the acquired resistance was then tested by growth in the absence of selective pressure (i.e., no AZM). Plaques formed by each C. psittaci 6BC variant grown for 14 days in the absence of selection displayed the same number of infectious particles when titers were determined in the presence or absence of 200 ng/ml of AZM, indicating that the resistance phenotype of these three chlamydial mutants was stable (data not shown).
Ribosomal mutations observed in AZM-tolerant isolates of C. trachomatis L2.
Although C. trachomatis L2 has the same sensitivity to AZM as C. psittaci 6BC (MIC of 100 ng/ml in the plaque assay), we were unable to obtain spontaneous AZM-resistant isolates of C. trachomatis L2 (frequency, <1.3 × 10−8 on 200 and 400 ng/ml AZM and <4.0 × 10−9 on 800 ng/ml and 1.5 μg/ml AZM). Because C. trachomatis L2 harbors two copies of the 23S rRNA gene, we hypothesized that a single mutation in only one ribosomal operon might not confer a level of AZM resistance high enough to be selected in one step in the plaque assay. Therefore, we reasoned that serial passage in subinhibitory concentrations of antibiotic would allow the enrichment of putative bacteria with low-level AZM resistance. Starting with 2 × 109 wild-type C. trachomatis L2 infectious particles, we isolated an AZM-tolerant population of C. trachomatis L2 growing in the presence of twice the MIC after 30 passages with AZM.
Ten individual plaques formed after expansion of the last harvest in the presence or absence of AZM for 2 weeks revealed no mutations in either of the two 23S rRNA genes of the mutants. We also sequenced the rplD and rplV genes, coding for ribosomal proteins L4 and L22, respectively. These genes represent two other known mutational targets for macrolide resistance (12). In all 10 isolates, one single mutation, C196 to A, was found in rplD, creating to a Gln-to-Lys alteration at position 66 in the C. trachomatis L2 ribosomal protein L4. This mutation arose in the population as early as the 23rd passage (in L2AZM#23).
Drug sensitivity phenotypes associated with the Q66K alteration in C. trachomatis L2 ribosomal protein L4.
Gln66 in C. trachomatis L2 ribosomal protein L4 corresponds to Gln62 in the homologous E. coli protein and lies within the highly conserved region of L4 that is responsible for binding to 23S rRNA (28, 64). The alteration in ribosomal protein L4 conferred an eightfold decrease in sensitivity for AZM, a fourfold decrease in ERM, JOS, SPI, and CLI sensitivity, and a twofold decrease for VIR sensitivity but did not affect the binding of CLM to ribosomes (Table 4). However, the MICs for the macrolides, with the exception of SPI, and the lincosamide were still lower than 1 μg/ml, suggesting that these antibiotics should still show clinical efficacy against these chlamydial mutants in vivo (24, 53).
TABLE 4.
Drug sensitivity phenotypes associated with the Q66K alteration in C. trachomatis L2 ribosomal protein L4
| C. trachomatis L2 strain | MIC (μg/ml) of:
|
||||||
|---|---|---|---|---|---|---|---|
| AZM | ERY | JOS | SPI | CLI | VIR | CLM | |
| Wild type | 0.1 | 0.2 | 0.05 | 0.8 | 0.125 | 4 | 0.4 |
| L2AZM#23a | 0.8 | 0.8 | 0.2 | 4 | 0.5 | 8 | 0.4 |
| L2AZM#31b | 0.8 | 0.8 | 0.2 | 4 | 0.5 | 8 | 0.4 |
Twenty-three passages in various concentrations of AZM (up to 50 ng/ml).
Twenty-eight passages with up to 100 ng/ml AZM followed by three expansions without AZM.
Physiological costs due to mutations in the 23S rRNA gene associated with AZM resistance in C. psittaci 6BC.
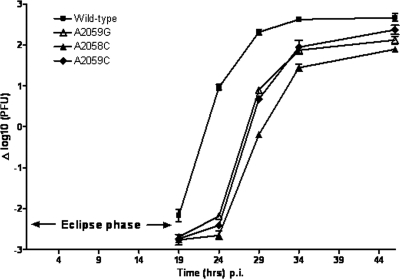
To be able to survive in a natural environment, a bacterium carrying a mutated allele must compete with the wild-type ancestor population. The outcome of the competition process depends on its relative fitness, defined as the efficiency of multiplication and transmission of the mutant cell compared with that of the wild-type ancestor strain (3). The developmental cycle of Chlamydia spp. alternates between replication and growth as RBs and conversion to EBs for transmission (1). In this study, bacterial fitness was assessed by monitoring bacterial infectivity during coinfection of wild-type C. psittaci 6BC with each AZM-resistant isogenic variant in L2 cell monolayers in the absence of drug. Figure 1 shows that the eclipse phase, i.e., the period in which infectious progeny EBs have differentiated into noninfectious RBs, lasted longer for the three mutants than for the parental strain, resulting in a severe delay in the RB-to-EB transition. Yet the doubling rate of EB formation during the exponential phase of the cycle was severely affected only for BCRBAZ2, being 1.5 times lower than the rates for the two other mutants and the wild-type strain (44 min versus 29 min) (Table 5) (6). None of the AZM-resistant mutants were able to recover their initial delay in production of infectious particles. Consequently, they were all clearly outcompeted in the absence of selection by the parent strain at the end of the developmental cycle, as reflected by the competition index (CI) (6). With CIs ranging from 0.03 to 0.19 at the end of the first round of competition and 0.006 to 0.09 after the second round (Table 5), it is clear that the AZM resistance mutations A2058C, A2059C, and A2059G in the 23S rRNA gene were associated with a high physiological cost in C. psittaci 6BC. The plaques formed by the AZM-resistant C. psittaci variants in the absence of selection were 40 to 70% smaller than the parent strain (Table 5). This phenotype also reflects the fitness cost associated with the mutation to resistance.
FIG. 1.
Growth competition between wild-type C. psittaci 6BC and the three isogenic 23S rRNA mutants during one developmental cycle. Infectivity curves for the C. psittaci 6BC wild-type strain BCRB and the three isogenic mutants with mutations in the 23S rRNA gene, BCRBAZ1 (A2059G), BCRBAZ2 (A2058C), and BCRBAZ5 (A2059C), were generated by harvesting at 19, 24, 29, 34, and 46 h p.i. Data are means ± standard deviations of duplicate determinations performed in two separate experiments.
TABLE 5.
Physiological costs of mutations in the 23S rRNA gene associated with AZM resistance in C. psittaci 6BC
| C. psittaci 6BC strain | 23S rRNA mutationa | Plaque sizeb (mm) | Eclipse (h)c | 2-fold PFU increase rate (h)c,e | CIf at passage:
|
|
|---|---|---|---|---|---|---|
| 1 (46 h p.i.) | 2 (92 h p.i.)g | |||||
| BCRB | None | 0.89 ± 0.31 | 19 | 0.48 | NA | NA |
| BCRBAZ2 | A2058C | 0.23 ± 0.19 | 24 | 0.73 | 0.03 ± 0.01 | 0.006 ± 0.001 |
| BCRBAZ5 | A2059C | 0.54 ± 0.30 | 19-24d | 0.49 | 0.18 ± 0.03 | 0.07 ± 0.01 |
| BCRBAZ1 | A2059G | 0.27 ± 0.10 | 19-24d | 0.49 | 0.19 ± 0.03 | 0.09 ± 0.01 |
E. coli numbering system.
The size of a minimum of 50 individual plaques was determined for each strain in the absence of antibiotic at 10 days p.i. and averaged.
Data from Fig. 1.
Eclipse phase lasted more than 19 h but less than 24 h.
Estimated as described in Materials and Methods.
Ratio of the output mutant/wild-type ratio at the indicated time to the input mutant/wild-type ratio. NA, not applicable.
Determined after a second passage for another 46 h as described in Materials and Methods.
Physiological costs due to the Q66K mutation in ribosomal protein L4 in C. trachomatis L2.
The relative decrease in AZM sensitivity incurred by the alteration in C. trachomatis ribosomal protein L4 was not high enough to differentiate between the sensitive wild-type strain and the C. trachomatis L2 populations harboring the rplD C196A allele when small inocula were used in the plaque assay (data not shown). Consequently, the bacterial fitness was estimated in pure culture as described in Materials and Methods. We observed a strong biological cost associated with the Q66-to-K change in C. trachomatis ribosomal protein L4, illustrated by the formation of smaller plaques and a decrease in the yield of infections particles at 46 h p.i. (Table 6). Interestingly, additional passages of L2AZM#23 in the presence and absence of AZM allowed the selection of a population that generated as much infectious particles per developmental cycle as the parent strain (Table 6). Nevertheless, L2AZM#31 still formed plaques that were half the size of those formed by the parent strain, suggesting that this mutant population would still be outcompeted by the parent strain in the absence of antibiotic selection pressure.
TABLE 6.
Physiological cost associated with the Q66K alteration in C. trachomatis L2 ribosomal protein L4
| Strain | Mutation | Plaque size (mm)c | EB generation rate (fold increase)d |
|---|---|---|---|
| CtL2 | Wild-type | 0.87 ± 0.24 | 258 ± 47 |
| L2AZM#23a | rplD C196A (K66Q) | 0.21 ± 0.12 | 126 ± 26 |
| L2AZM#31b | rplD C196A (K66Q) | 0.47 ± 0.18 | 241 ± 59 |
Twenty-three passages on various concentrations of AZM (up to 50 ng/ml).
Twenty-eight passages with up to 100 ng/ml AZM followed by three expansions without AZM.
The size of a minimum of 150 individual plaques was determined for each strain in the absence of antibiotic at 14 days p.i. and averaged.
The number of PFU produced at 46 h p.i divided by the number used at the time of infection.
DISCUSSION
When cost is not an issue, the macrolide AZM is a major drug used in the treatment as well as in the prophylaxis of chlamydial infections because of the convenient single-dose administration, the high bacterial sensitivity, and the apparent lack of treatment failure due to stable resistance of these obligate intracellular bacteria (23, 53, 61). Additional macrolides, including the 14-member-ring ERM, roxithromycin, and clarithromycin and the 16-member-ring JOS and SPI, also show clinical efficacy against chlamydiae (14, 30, 36, 53). These antibiotics inhibit protein synthesis by reversibly binding to the 50S ribosomal subunit at a site formed by the association of domains II and V of the bacterial 23S rRNA and including the ribosomal proteins L4 and L22, which line the protein exit tunnel (44, 52). Interestingly, lincosamides, such as CLI, and streptogramins, particularly type B components such as pristinamycin IA, inhibit peptide elongation similarly to macrolides, with which they share physically overlapping binding sites on the ribosome (59). Clinical efficacy of CLI has been reported for C. trachomatis (2), whereas antichlamydial activity of pristinamycin or virginiamycin has been shown in vitro (26) and in an animal model (35). In this study, we used the plaque assay to confirm the sensitivity of wild-type C. psittaci 6BC and C. trachomatis L2 to these drugs (Tables 3 and 4) and obtained MICs consistent with those previously reported (25, 55).
Although treatment failures (defined as Chlamydia persistence 1 month after treatment) following macrolide therapy have been reported, most reports do not address the role of genetic resistance in the recurrence of chlamydial infections (23, 61). For example, Golden et al. (18) reported a treatment failure rate of 8% among women who reported no new sexual exposures, but that study did not include phenotypic or genotypic susceptibility analysis of the bacteria. Similarly, no genetic analysis was initiated in a patient who failed to clear C. trachomatis infection with JOS (51). In veterinary practice, too, Owen et al. reported that infections with C. felis (C. psittaci feline pneumonitis agent) appeared to be insensitive to AZM in four of five cats studied but did not analyze the possible contribution of mutations to treatment failure (37).
In the present study, high-level AZM resistance arose in C. psittaci 6BC at a frequency of around 1 × 10−8. This frequency is similar to that reported for Mycobacterium avium, which, like C. psittaci, harbors a single rRNA operon (21, 31). We previously noted a similarity in the development of aminoglycoside resistance by both species (7). Here, we found that spontaneous macrolide resistance arose in C. psittaci 6BC from single mutations in the unique 23S rRNA gene resulting in an A2058C, A2059C, or A2059G substitution. This is the first report showing stable, high-level resistance to multiple clinically relevant antibiotics in a chlamydial strain following single point mutations in the 23S rRNA gene. Interestingly, although the A2058G substitution in 23S rRNA is the most common macrolide resistance mutation encountered in bacterial pathogens (12, 60), it was found in none of the 30 independent mutants of C. psittaci 6BC analyzed in this study. This suggests that the A2058G change is deleterious for C. psittaci 6BC. Pfister et al. (42) recently proposed that the fitness cost associated with this particular mutation is dependent on the nature of the adjacent 2057-2611 base pair, as bacteria with A2057-U2611, such as mycobacteria, are more tolerant to the resistance mutation than species with G2057-C2611, such as E. coli, Helicobacter pylori, and Streptococcus pneumoniae. However, C. psittaci 6BC and other Chlamydiaceae display the A2057-U2611 pair as in the mycobacteria. Therefore, one would expect that the biological cost of an A2058G mutation would be tolerated in C. psittaci as it is in mycobacteria. We isolated no such mutants. It is possible that, compared to mycobacteria, C. psittaci 6BC lacks additional genetic factors such as an intragenic or extragenic compensatory mutation to balance the cost of the A2058G mutation (8, 29). Moreover, no A-to-U transition was observed at position 2058 or 2059 in the AZM-resistant C. psittaci mutants, and we did not detect any mutation at positions 2057, 2452, and 2611, although those have been shown to confer low-level macrolide resistance in some other bacteria (60). Because bacteria growing at high density exhibit a low level of antibiotic resistance, we used high concentrations of antibiotic to select for resistant mutants (7). This strategy precluded isolating low-level-resistance isolates of Chlamydia by plaque assay. Furthermore, isolation of chlamydial variants by this technique depends on both growth and cell-to-cell transmission of the organism. In the absence of a genetic system for chlamydiae, we cannot determine at this time if any of these mutations would be associated with a level of AZM resistance too low to allow selection in the plaque assay or if the mutations would be deleterious for the organism.
In contrast to C. psittaci 6BC, we were unable to obtain highly AZM-resistant isolates of C. trachomatis L2 in the plaque assay. We showed previously that the frequencies of resistance to rifampin are on the same order for both chlamydial species (7), suggesting that mutations in the 23S rRNA gene should form at equivalent rates. However, because C. trachomatis harbors two 23S rRNA gene copies, selection of spontaneous AZM-resistant isolates in the plaque assay requires the mutation to be dominant over the wild-type (unmutated) copy. Although a resistant phenotype is apparently codominant in mycobacteria (49), Staphylococcus aureus (47), H. pylori (57), Mycoplasma hominis (38), and Ureaplasma parvum (40), homogenization of the mutation to all ribosomal copies by gene conversion has been linked to high-level macrolide resistance (32, 56) as well as better stability or homogeneity of the resistance phenotype (4, 57, 62). At the present time, we lack the genetic tools to examine the contribution of single mutations in one 23S rRNA gene copy to the level of macrolide resistance in C. trachomatis L2. Interestingly, a double mutation, A2058C T2611C, was recently characterized in clinical isolates of C. trachomatis after AZM treatment failure, suggesting that multiple mutations in the 23S rRNA gene are necessary for expression of high-level resistance (30). However, the percentages of heterozygous and homozygous populations are not clear in that report, as both wild-type and mutated copies of the 23S rRNA were detected in the clinical isolates.
In the present study, we isolated a population of C. trachomatis L2 with an eightfold decrease in AZM susceptibility due to a mutation in rplD coding for ribosomal protein L4. Gln66 (Gln62 in E. coli) lies in a phylogenetically conserved disordered loop that displays many basic residues proposed to be the central element in binding of the protein to the 23S rRNA (28, 64). Replacement of the uncharged Gln with the positively charged Lys is likely to affect the binding of the chlamydial ribosomal protein L4 to the cognate 23S rRNA molecules. Indeed, mutations at residues in this conserved L4 disordered loop were found to affect the overall folding of 23S rRNA in domains II, III, and V, perturbing both the translational activity of ribosomes and the action of antibiotics known to interact with nucleotide residues in the peptidyl transferase center (28, 33, 58). Although rplD mutations linked to low-level macrolide resistance have been selected in vitro in clinically relevant organisms (10, 39, 54), such mutations are frequently found to be paired with additional mutations in 23S rRNA or in rplV (ribosomal protein L22) in clinical isolates (41, 48). Wolter et al. elegantly showed that persistence of macrolide-resistant clinical isolates of Streptococcus pneumoniae resulting from alterations in ribosomal protein L4 is linked to acquisition of secondary mutations that compensate for the defect in bacterial growth as well as increasing the level of macrolide resistance (63). In the present work, we found that the physiological cost associated with the Q66K mutation in C. trachomatis L4 protein could be alleviated without reversion of the drug sensitivity characteristics of the strain (Table 4 and 6). Further experiments are planned to test whether the new “adapted” genetic background would now be more favorable for acquisition of high-level AZM-resistant mutations.
The rate of increase in frequency of resistance to an antibiotic is directly proportional to the efficacy of the drug and the extent of its use and is inversely proportional to the cost that resistance imposes on bacterial fitness, i.e., its rate of infectious transmission and its ability to compete with other strains (3). We analyzed the biological costs associated with point mutations in the 23S rRNA gene conferring macrolide resistance to C. psittaci 6BC by comparing growth of the susceptible parent to that of three isogenic macrolide-resistant variants in the absence of selection. Each mutant was delayed in the formation of infectious particles, as seen by the extended eclipse phase of the development cycle. Additionally, each mutant was severely outcompeted by the wild-type strain at the end of the cycle (CI less than 0.2). These results indicate that mutations in the 23S RNA gene associated with AZM resistance also impose a high physiological cost on C. psittaci. It is worth adding that chlamydial growth conditions in this study were optimized for cell culture, i.e., cycloheximide was added to the medium to create a more favorable environment for bacterial growth by inhibiting host protein synthesis, thus making more nutrients available to the bacteria (20). One might expect even stronger developmental differences between each mutant and the parent strain when they have to compete for survival in the natural host. Therefore, we predict that these mutations would not be maintained in vivo unless compensatory mutations are selected to adapt to the costs of chromosomal antibiotic resistance (8, 27, 29).
It is clear that many interacting factors influence the probability of macrolide resistance development in chlamydial infections. Antibiotic-resistant mutants selected in vivo tend to be ones with low or no fitness cost in vitro (16, 34, 50). Unfortunately, the lack of a small animal model for C. trachomatis L2 precludes testing the consequence of the change in ribosomal protein L4 on the pathogenicity of the strain. In addition, our laboratory strain of C. psittaci 6BC has been passaged in tissue culture for several years, and its current level of virulence in parrots has not been studied. Nevertheless, our results give rise to some general considerations regarding the likelihood of development and persistence of AZM-resistant chlamydial strains. In this study, mutants were readily obtained in vitro for C. psittaci 6BC following mutations in the unique 23S rRNA gene, while only rplD mutants of C. trachomatis L2 with increased tolerance to AZM were isolated. Each mutant strain was attenuated for growth in the absence of selection, suggesting that emergence of AZM resistance in chlamydiae in vivo depends on acquisition of compensatory mutations. Frequent intermittent antimicrobial treatments as a consequence of recurrent infections or repeated mass prophylaxis therapy currently in place to control trachoma in countries where it is endemic (15), as well as for experimental prevention of coronary artery diseases (19), might select for isolates adapted to the high cost of chromosomal resistance. Allowing the C. trachomatis rplD mutant to evolve during serial passages permitted selection of a more fit bacterial population in vitro without changing the antibiotic sensitivity characteristics of the strain. However, we still lack information on whether chlamydiae are evolving in vivo in response to antibiotic selection pressure. It will be important to examine the consequences of drug resistance mutations on the pathogenicity and survival of chlamydiae such as C. muridarum or C. caviae, which can be tested in their natural small mammal hosts (i.e., mice and guinea pigs, respectively). Additionally, follow-up of potential treatment failures with both phenotypic and genotypic susceptibility assays of C. trachomatis isolates will be important in order to understand whether and how antibiotic resistance occurs in the clinical setting. In the meantime, caution should be used in relying upon AZM for treatment of human and veterinary psittacosis.
Acknowledgments
This work was supported by grant AI44033 from the National Institute of Allergy and Infectious Diseases.
We thank Nancy E. Adams for technical assistance, Anne-Laure Prunier for her comments and critical reading of the manuscript, and Michael N. Flora and the USUHS Biomedical Instrumentation Center for DNA sequencing and oligonucleotide synthesis services.
The opinions or assertions contained herein are those of the authors and are not to be construed as official or reflecting the views of the Department of Defense or the Uniformed Services University of the Health Sciences.
Footnotes
Published ahead of print on 1 October 2007.
REFERENCES
- 1.Abdelrahman, Y. M., and R. J. Belland. 2005. The chlamydial developmental cycle. FEMS Microbiol. Rev. 29:949-959. [DOI] [PubMed] [Google Scholar]
- 2.Alger, L. S., and J. C. Lovchik. 1991. Comparative efficacy of clindamycin versus erythromycin in eradication of antenatal Chlamydia trachomatis. Am. J. Obstet. Gynecol. 165:375-381. [DOI] [PubMed] [Google Scholar]
- 3.Andersson, D. I., and B. R. Levin. 1999. The biological cost of antibiotic resistance. Curr. Opin. Microbiol. 2:489-493. [DOI] [PubMed] [Google Scholar]
- 4.Bartkus, J. M., B. A. Juni, K. Ehresmann, C. A. Miller, G. N. Sanden, P. K. Cassiday, M. Saubolle, B. Lee, J. Long, A. R. Harrison, Jr., and J. M. Besser. 2003. Identification of a mutation associated with erythromycin resistance in Bordetella pertussis: implications for surveillance of antimicrobial resistance. J. Clin. Microbiol. 41:1167-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berisio, R., N. Corti, P. Pfister, A. Yonath, and E. C. Bottger. 2006. 23S rRNA 2058A→G alteration mediates ketolide resistance in combination with deletion in L22. Antimicrob. Agents Chemother. 50:3816-3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binet, R., and A. T. Maurelli. 2005. Fitness cost due to mutations in the 16S rRNA associated with spectinomycin resistance in Chlamydia psittaci 6BC. Antimicrob. Agents Chemother. 49:4455-4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Binet, R., and A. T. Maurelli. 2005. Frequency of spontaneous mutations that confer antibiotic resistance in Chlamydia spp. Antimicrob. Agents Chemother. 49:2865-2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottger, E. C., B. Springer, M. Pletschette, and P. Sander. 1998. Fitness of antibiotic-resistant microorganisms and compensatory mutations. Nat. Med. 4:1343-1344. [DOI] [PubMed] [Google Scholar]
- 9.Bush, R. M., and K. D. Everett. 2001. Molecular evolution of the Chlamydiaceae. Int. J. Syst. Evol. Microbiol. 51:203-220. [DOI] [PubMed] [Google Scholar]
- 10.Clark, C., B. Bozdogan, M. Peric, B. Dewasse, M. R. Jacobs, and P. C. Appelbaum. 2002. In vitro selection of resistance in Haemophilus influenzae by amoxicillin-clavulanate, cefpodoxime, cefprozil, azithromycin, and clarithromycin. Antimicrob. Agents Chemother. 46:2956-2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dinos, G. P., M. Michelinaki, and D. L. Kalpaxis. 2001. Insights into the mechanism of azithromycin interaction with an Escherichia coli functional ribosomal complex. Mol. Pharmacol. 59:1441-1445. [DOI] [PubMed] [Google Scholar]
- 12.Doucet-Populaire, F., K. Buriankova, J. Weiser, and J. L. Pernodet. 2002. Natural and acquired macrolide resistance in mycobacteria. Curr. Drug Targets Infect. Disord. 2:355-370. [DOI] [PubMed] [Google Scholar]
- 13.Dugan, J., D. D. Rockey, L. Jones, and A. A. Andersen. 2004. Tetracycline resistance in Chlamydia suis mediated by genomic islands inserted into the chlamydial inv-like gene. Antimicrob. Agents Chemother. 48:3989-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dylewski, J., B. Clecner, J. Dubois, C. St-Pierre, G. Murray, C. Bouchard, and R. Phillips. 1993. Comparison of spiramycin and doxycycline for treatment of Chlamydia trachomatis genital infections. Antimicrob. Agents Chemother. 37:1373-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emerson, P. M., M. Burton, A. W. Solomon, R. Bailey, and D. Mabey. 2006. The SAFE strategy for trachoma control: using operational research for policy, planning and implementation. Bull. W. H. O. 84:613-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gagneux, S., C. D. Long, P. M. Small, T. Van, G. K. Schoolnik, and B. J. Bohannan. 2006. The competitive cost of antibiotic resistance in Mycobacterium tuberculosis. Science 312:1944-1946. [DOI] [PubMed] [Google Scholar]
- 17.Gieffers, J., R. J. Belland, W. Whitmire, S. Ouellette, D. Crane, M. Maass, G. I. Byrne, and H. D. Caldwell. 2002. Isolation of Chlamydia pneumoniae clonal variants by a focus-forming assay. Infect. Immun. 70:5827-5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golden, M. R., W. L. Whittington, H. H. Handsfield, J. P. Hughes, W. E. Stamm, M. Hogben, A. Clark, C. Malinski, J. R. Helmers, K. K. Thomas, and K. K. Holmes. 2005. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N. Engl. J. Med. 352:676-685. [DOI] [PubMed] [Google Scholar]
- 19.Grayston, J. T., R. A. Kronmal, L. A. Jackson, A. F. Parisi, J. B. Muhlestein, J. D. Cohen, W. J. Rogers, J. R. Crouse, S. L. Borrowdale, E. Schron, and C. Knirsch. 2005. Azithromycin for the secondary prevention of coronary events. N. Engl. J. Med. 352:1637-1645. [DOI] [PubMed] [Google Scholar]
- 20.Hatch, T. P. 1975. Competition between Chlamydia psittaci and L cells for host isoleucine pools: a limiting factor in chlamydial multiplication. Infect. Immun. 12:211-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heifets, L., N. Mor, and J. Vanderkolk. 1993. Mycobacterium avium strains resistant to clarithromycin and azithromycin. Antimicrob. Agents Chemother. 37:2364-2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hogan, R. J., S. A. Mathews, S. Mukhopadhyay, J. T. Summersgill, and P. Timms. 2004. Chlamydial persistence: beyond the biphasic paradigm. Infect. Immun. 72:1843-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horner, P. 2006. The case for further treatment studies of uncomplicated genital Chlamydia trachomatis infection. Sex. Transm. Infect. 82:340-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain, R., and L. H. Danziger. 2004. The macrolide antibiotics: a pharmacokinetic and pharmacodynamic overview. Curr. Pharm. Design 10:3045-3053. [DOI] [PubMed] [Google Scholar]
- 25.Johnson, F. W., M. J. Clarkson, and W. N. Spencer. 1983. Susceptibility of Chlamydia psittaci (ovis) to antimicrobial agents. J. Antimicrob. Chemother. 11:413-418. [DOI] [PubMed] [Google Scholar]
- 26.Lefevre, J. C., and R. Bauriaud. 1989. Comparative in vitro activities of pristinamycin and other antimicrobial agents against genital pathogens. Antimicrob. Agents Chemother. 33:2152-2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lenski, R. E. 1998. Bacterial evolution and the cost of antibiotic resistance. Int. Microbiol. 1:265-270. [PubMed] [Google Scholar]
- 28.Leontiadou, F., M. A. Xaplanteri, G. Papadopoulos, C. Gerassimou, D. L. Kalpaxis, and T. Choli-Papadopoulou. 2003. On the structural and functional importance of the highly conserved Glu56 of Thermus thermophilus L4 ribosomal protein. J. Mol. Biol. 332:73-84. [DOI] [PubMed] [Google Scholar]
- 29.Maisnier-Patin, S., and D. I. Andersson. 2004. Adaptation to the deleterious effects of antimicrobial drug resistance mutations by compensatory evolution. Res. Microbiol. 155:360-369. [DOI] [PubMed] [Google Scholar]
- 30.Misyurina, O. Y., E. V. Chipitsyna, Y. P. Finashutina, V. N. Lazarev, T. A. Akopian, A. M. Savicheva, and V. M. Govorun. 2004. Mutations in a 23S rRNA gene of Chlamydia trachomatis associated with resistance to macrolides. Antimicrob. Agents Chemother. 48:1347-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nash, K. A., and C. B. Inderlied. 1995. Genetic basis of macrolide resistance in Mycobacterium avium isolated from patients with disseminated disease. Antimicrob. Agents Chemother. 39:2625-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ng, L. K., I. Martin, G. Liu, and L. Bryden. 2002. Mutation in 23S rRNA associated with macrolide resistance in Neisseria gonorrhoeae. Antimicrob. Agents Chemother. 46:3020-3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Connor, M., S. T. Gregory, and A. E. Dahlberg. 2004. Multiple defects in translation associated with altered ribosomal protein L4. Nucleic Acids Res. 32:5750-5756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Neill, A. J., T. Huovinen, C. W. Fishwick, and I. Chopra. 2006. Molecular genetic and structural modeling studies of Staphylococcus aureus RNA polymerase and the fitness of rifampin resistance genotypes in relation to clinical prevalence. Antimicrob. Agents Chemother. 50:298-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Orfila, J., and F. Haider. 1984. Action of pristinamycin on Chlamydia. Pathol. Biol. (Paris) 32:443-445. [PubMed] [Google Scholar]
- 36.Orfila, J., F. Haider, and D. Thomas. 1988. Activity of spiramycin against chlamydia, in vitro and in vivo. J. Antimicrob. Chemother. 22(Suppl. B): 73-76. [DOI] [PubMed] [Google Scholar]
- 37.Owen, W. M., C. P. Sturgess, D. A. Harbour, K. Egan, and T. J. Gruffydd-Jones. 2003. Efficacy of azithromycin for the treatment of feline chlamydophilosis. J. Feline. Med. Surg. 5:305-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pereyre, S., P. Gonzalez, B. de Barbeyrac, A. Darnige, H. Renaudin, A. Charron, S. Raherison, C. Bebear, and C. M. Bebear. 2002. Mutations in 23S rRNA account for intrinsic resistance to macrolides in Mycoplasma hominis and Mycoplasma fermentans and for acquired resistance to macrolides in M. hominis. Antimicrob. Agents Chemother. 46:3142-3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pereyre, S., C. Guyot, H. Renaudin, A. Charron, C. Bebear, and C. M. Bebear. 2004. In vitro selection and characterization of resistance to macrolides and related antibiotics in Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 48:460-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pereyre, S., M. Metifiot, C. Cazanave, H. Renaudin, A. Charron, C. Bebear, and C. M. Bebear. 2007. Characterisation of in vitro-selected mutants of Ureaplasma parvum resistant to macrolides and related antibiotics. Int. J. Antimicrob. Agents. 29:207-211. [DOI] [PubMed] [Google Scholar]
- 41.Peric, M., B. Bozdogan, M. R. Jacobs, and P. C. Appelbaum. 2003. Effects of an efflux mechanism and ribosomal mutations on macrolide susceptibility of Haemophilus influenzae clinical isolates. Antimicrob. Agents Chemother. 47:1017-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pfister, P., N. Corti, S. Hobbie, C. Bruell, R. Zarivach, A. Yonath, and E. C. Bottger. 2005. 23S rRNA base pair 2057-2611 determines ketolide susceptibility and fitness cost of the macrolide resistance mutation 2058A→G. Proc. Natl. Acad. Sci. USA 102:5180-5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pfister, P., S. Jenni, J. Poehlsgaard, A. Thomas, S. Douthwaite, N. Ban, and E. C. Bottger. 2004. The structural basis of macrolide-ribosome binding assessed using mutagenesis of 23S rRNA positions 2058 and 2059. J. Mol. Biol. 342:1569-1581. [DOI] [PubMed] [Google Scholar]
- 44.Poehlsgaard, J., and S. Douthwaite. 2005. The bacterial ribosome as a target for antibiotics. Nat. Rev. Microbiol. 3:870-881. [DOI] [PubMed] [Google Scholar]
- 45.Poehlsgaard, J., P. Pfister, E. C. Bottger, and S. Douthwaite. 2005. Molecular mechanisms by which rRNA mutations confer resistance to clindamycin. Antimicrob. Agents Chemother. 49:1553-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Porse, B. T., and R. A. Garrett. 1999. Sites of interaction of streptogramin A and B antibiotics in the peptidyl transferase loop of 23 S rRNA and the synergism of their inhibitory mechanisms. J. Mol. Biol. 286:375-387. [DOI] [PubMed] [Google Scholar]
- 47.Prunier, A. L., B. Malbruny, D. Tande, B. Picard, and R. Leclercq. 2002. Clinical isolates of Staphylococcus aureus with ribosomal mutations conferring resistance to macrolides. Antimicrob. Agents Chemother. 46:3054-3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reinert, R. R., A. Wild, P. Appelbaum, R. Lutticken, M. Y. Cil, and A. Al-Lahham. 2003. Ribosomal mutations conferring resistance to macrolides in Streptococcus pneumoniae clinical strains isolated in Germany. Antimicrob. Agents Chemother. 47:2319-2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sander, P., T. Prammananan, A. Meier, K. Frischkorn, and E. C. Bottger. 1997. The role of ribosomal RNAs in macrolide resistance. Mol. Microbiol. 26:469-480. [DOI] [PubMed] [Google Scholar]
- 50.Sander, P., B. Springer, T. Prammananan, A. Sturmfels, M. Kappler, M. Pletschette, and E. C. Bottger. 2002. Fitness cost of chromosomal drug resistance-conferring mutations. Antimicrob. Agents Chemother. 46:1204-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Savicheva, A. M., E. S. Shipitsyna, N. Vorobyova, E. Sokolovsky, A. Guschin, P. Ryzhikh, and G. Shipulin. 2006. Monitoring of Chlamydia trachomatis eradication during and after treatment of genital chlamydial infection, p. 81-84. In Chlamydial infections. Proceedings of the Eleventh International Symposium on Human Chlamydial Infections.
- 52.Schlunzen, F., R. Zarivach, J. Harms, A. Bashan, A. Tocilj, R. Albrecht, A. Yonath, and F. Franceschi. 2001. Structural basis for the interaction of antibiotics with the peptidyl transferase centre in eubacteria. Nature 413:814-821. [DOI] [PubMed] [Google Scholar]
- 53.Senn, L., M. R. Hammerschlag, and G. Greub. 2005. Therapeutic approaches to Chlamydia infections. Expert Opin. Pharmacother. 6:2281-2290. [DOI] [PubMed] [Google Scholar]
- 54.Sidhu, A. B., Q. Sun, L. J. Nkrumah, M. W. Dunne, J. C. Sacchettini, and D. A. Fidock. 2007. In vitro efficacy, resistance selection, and structural modeling studies implicate the malarial parasite apicoplast as the target of azithromycin. J. Biol. Chem. 282:2494-2504. [DOI] [PubMed] [Google Scholar]
- 55.Suchland, R. J., W. M. Geisler, and W. E. Stamm. 2003. Methodologies and cell lines used for antimicrobial susceptibility testing of Chlamydia spp. Antimicrob. Agents Chemother. 47:636-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tait-Kamradt, A., T. Davies, P. C. Appelbaum, F. Depardieu, P. Courvalin, J. Petitpas, L. Wondrack, A. Walker, M. R. Jacobs, and J. Sutcliffe. 2000. Two new mechanisms of macrolide resistance in clinical strains of Streptococcus pneumoniae from Eastern Europe and North America. Antimicrob. Agents Chemother. 44:3395-3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taylor, D. E., Z. Ge, D. Purych, T. Lo, and K. Hiratsuka. 1997. Cloning and sequence analysis of two copies of a 23S rRNA gene from Helicobacter pylori and association of clarithromycin resistance with 23S rRNA mutations. Antimicrob. Agents Chemother. 41:2621-2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tsagkalia, A., F. Leontiadou, M. A. Xaplanteri, G. Papadopoulos, D. L. Kalpaxis, and T. Choli-Papadopoulou. 2005. Ribosomes containing mutants of L4 ribosomal protein from Thermus thermophilus display multiple defects in ribosomal functions and sensitivity against erythromycin. RNA 11:1633-1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tu, D., G. Blaha, P. B. Moore, and T. A. Steitz. 2005. Structures of MLSBK antibiotics bound to mutated large ribosomal subunits provide a structural explanation for resistance. Cell 121:257-270. [DOI] [PubMed] [Google Scholar]
- 60.Vester, B., and S. Douthwaite. 2001. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob. Agents Chemother. 45:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang, S. A., J. R. Papp, W. E. Stamm, R. W. Peeling, D. H. Martin, and K. K. Holmes. 2005. Evaluation of antimicrobial resistance and treatment failures for Chlamydia trachomatis: a meeting report. J. Infect. Dis. 191:917-923. [DOI] [PubMed] [Google Scholar]
- 62.Wolter, N., A. M. Smith, D. J. Farrell, and K. P. Klugman. 2006. Heterogeneous macrolide resistance and gene conversion in the pneumococcus. Antimicrob. Agents Chemother. 50:359-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wolter, N., A. M. Smith, D. J. Farrell, W. Schaffner, M. Moore, C. G. Whitney, J. H. Jorgensen, and K. P. Klugman. 2005. Novel mechanism of resistance to oxazolidinones, macrolides, and chloramphenicol in ribosomal protein L4 of the pneumococcus. Antimicrob. Agents Chemother. 49:3554-3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Worbs, M., R. Huber, and M. C. Wahl. 2000. Crystal structure of ribosomal protein L4 shows RNA-binding sites for ribosome incorporation and feedback control of the S10 operon. EMBO J. 19:807-818. [DOI] [PMC free article] [PubMed] [Google Scholar]