The phenomenon of antimicrobial agent dependence has been infrequently described, with vancomycin-dependent Enterococcus faecalis first reported in 1994 (3) and then occasionally thereafter (7, 9). Although heteroresistance of the Acinetobacter baumannii-Acinetobacter calcoaceticus complex (ABC) to colistin has been described, the dependence of the ABC on antimicrobial agents has not been reported (5). We describe the isolation of a colistin-dependent subpopulation of the ABC from a clinical isolate.
A 77-year-old diabetic male was admitted with calcaneal osteomyelitis and bacteremia due to multidrug-resistant ABC. He was treated with colistin (colistimethate sodium, 125 mg) intravenously every 12 h for 9 days. A calcaneus bone specimen was submitted for culture during a below-the-knee amputation on the fifth day of colistin therapy. The ABC was isolated and identified using the Vitek system (bioMerieux, Inc., Durham, NC) and was stored frozen in the clinical laboratory. This patient isolate and 18 other ABC clinical isolates were subsequently subcultured twice on sheep blood agar, and colistin susceptibility was confirmed by broth microdilution (BMD) MIC testing using in-lab-prepared frozen panels. The panels contained colistin, polymyxin B, and 10 other drugs (Table 1). BMD was performed according to the Clinical and Laboratory Standards Institute method with cation-adjusted Mueller-Hinton broth, a standard inoculum density of 5 × 105 CFU/ml, and incubation at 35°C for 20 to 24 h (1). Quality control organisms Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were tested simultaneously, and results were within acceptable limits (2).
TABLE 1.
BMD MIC results for the index patient ABC isolate before and after subculturing it on Mueller-Hinton agar containing 8 μg/ml colistin
| Antimicrobial agent | MIC of index patient isolate (μg/ml)
|
|
|---|---|---|
| Before colistin subculture | After colistin subculture | |
| Colistin | 1 | >16 |
| Polymyxin B | 1 | 4 |
| Tigecycline | 2 | 0.12 |
| Doxycycline | 8 | 1 |
| Minocycline | 1 | NGa |
| Ceftazidime | >64 | NG |
| Sulbactam | >64 | NG |
| Ampicillin-sulbactam | >128/64 | NG |
| Ticarcillin-clavulanate | >256/2 | NG |
| Imipenem | >16 | NG |
| Gentamicin | >8 | NG |
| Amikacin | 8 | NG |
| Azithromycin | >8 | NG |
NG, no growth.
For population analysis studies, colistin sulfate (Sigma, St. Louis, MO) was added to molten Mueller-Hinton agar (Difco, BD, Sparks, MD) to produce plates containing 8 μg/ml colistin. A suspension of each patient isolate was prepared in 0.9% saline to a 5 McFarland standard, and 100-μl aliquots were used to inoculate each of two colistin plates. The plates were incubated at 35°C for 20 to 24 h. Colonies recovered from the colistin plates were subcultured twice onto sheep blood agar plates prior to repeat BMD testing. Colonies of the index patient isolate were subsequently recovered from wells containing 16 μg/ml of colistin, subcultured again, and then streaked in duplicate onto Mueller-Hinton agar plates. A colistin (10-μg) disk (BD Microbiology Systems, Cockeysville, MD) was placed on each plate prior to incubation for 20 to 24 h.
Initial BMD testing of the index patient isolate (prior to being plated on colistin-containing agar) demonstrated susceptibility to colistin and polymyxin B and resistance to several other antimicrobial agents (Table 1). Subsequent BMD testing of the subpopulation selected by exposure to 8 μg/ml colistin revealed a growth pattern consistent with colistin and polymyxin B dependence, with very scant or no growth in BMD wells that did not contain colistin or polymyxin B but increasingly luxuriant growth as the colistin concentration increased from 0.12 to 16 μg/ml. In contrast to growth in colistin, growth in polymyxin B wells became more florid as the concentration increased to 2 μg/ml but was inhibited at higher concentrations. Scant growth also occurred in wells containing low concentrations of tigecycline (<0.12 μg/ml) and doxycycline (<1 μg/ml) only but not in wells containing other drugs.
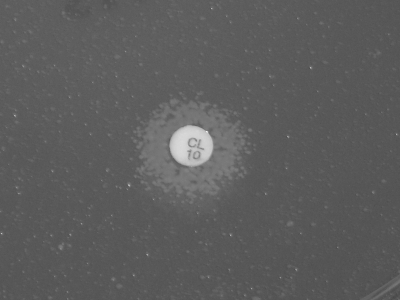
While all 19 isolates demonstrated an ABC subpopulation able to grow on the plates containing 8 μg/ml colistin, only the index patient isolate developed a colistin-dependent growth pattern. When plated on Mueller-Hinton agar with a colistin disk, the isolate grew heavily immediately around the disk (16-mm diameter zone of growth), with scant growth over the remainder of the plate (Fig. 1).
FIG. 1.
Kirby-Bauer plate demonstrating colistin-dependent growth pattern. The diameter of the zone of growth is 16 mm.
Polymyxins disrupt the bacterial cell membrane by interfering with phospholipids, damaging the osmotic barrier. Resistance to colistin may occur via alteration of the lipid A binding site or by efflux pumps (8). One possible mechanism for colistin dependence may be a mutation of lipid A which results in a defective cell membrane and osmotic trauma in the absence of colistin.
Antimicrobial-agent-dependent growth is an unusual phenomenon that has not been previously reported for Acinetobacter. The development of heteroresistance or the dependence of the ABC on colistin is of concern due to few other therapeutic options (4). Recent reports of ABC heteroresistance to colistin and a negative postantibiotic effect of colistin on ABC are contributing to a realization that colistin may not be the drug of choice for highly resistant gram-negative infections in the future (5, 6). Future research should be directed toward elucidating the mechanism of colistin dependence.
Acknowledgments
We thank M. Leticia McElmeel and Letitia C. Fulcher for excellent technical assistance.
The views expressed herein are those of the authors and do not reflect the official policy or position of the Department of the Army, the Department of Defense, or the U.S. Government.
Footnotes
Published ahead of print on 17 September 2007.
REFERENCES
- 1.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA.
- 2.Clinical and Laboratory Standards Institute. 2006. Performance standards for antimicrobial susceptibility testing; 16th informational supplement. CLSI document M100-S16. Clinical and Laboratory Standards Institute, Wayne, PA.
- 3.Fraimow, H. S., D. L. Jungkind, D. W. Lander, D. R. Delso, and J. L. Dean. 1994. Urinary tract infection with an Enterococcus faecalis isolate that requires vancomycin for growth. Ann. Intern. Med. 121:22-26. [DOI] [PubMed] [Google Scholar]
- 4.Hawley, J. S., C. K. Murray, M. E. Griffith, M. L. McElmeel, L. C. Fulcher, D. R. Hospenthal, and J. H. Jorgensen. 2007. Susceptibility of Acinetobacter strains isolated from deployed U.S. military personnel. Antimicrob. Agents Chemother. 51:376-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li, J., C. R. Rayner, R. L. Nation, R. J. Owen, D. Spelman, K. E. Tan, and L. Liolios. 2006. Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 50:2946-2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owen, R. J., J. Li, R. L. Nation, and D. Spelman. 2007. In vitro pharmacodynamics of colistin against Acinetobacter baumannii clinical isolates. J. Antimicrob. Chemother. 59:473-477. [DOI] [PubMed] [Google Scholar]
- 7.Tambyah, P. A., J. A. Marx, and D. G. Maki. 2004. Nosocomial infection with vancomycin-dependent Enterococci. Emerg. Infect. Dis. 10:1277-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tzeng, Y.-L., K. D. Ambrose, S. Zughaier, X. Zhou, Y. K. Miller, W. M. Shafer, and D. S. Stephens. 2005. Cationic antimicrobial peptide resistance in Neisseria meningitidis. J. Bacteriol. 187:5387-5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Bambeke, F., M. Chauvel, P. E. Reynolds, H. S. Fraimow, and P. Courvalin. 1999. Vancomycin-dependent Enterococcus faecalis clinical isolates and revertant mutants. Antimicrob. Agents Chemother. 43:41-47. [DOI] [PMC free article] [PubMed] [Google Scholar]