Abstract
A comparative study on the prevalence and pathology of bovine tuberculosis (TB) was conducted on 5,424 cattle (2,578 zebus, 1,921 crosses, and 925 Holsteins), which were kept on pasture in the central highlands of Ethiopia, using a comparative intradermal tuberculin test, postmortem examination, and bacteriology. The overall prevalence of bovine TB was 13.5%; prevalence was higher in Holsteins than either zebus (22.2% versus 11.6%, χ2 = 61.8; P < 0.001) or crosses (22.2% versus 11.9%, χ2 = 50.7; P < 0.001). Moreover, the severity of pathology in Holsteins (mean ± standard error of the mean [SEM], 6.84 ± 0.79) was significantly higher (P = 0.018) than the severity of pathology in zebus (5.21 ± 0.30). In addition, the risk of TB in Holsteins was more than twice (odds ratio [OR] = 2.32; 95% confidence interval [CI] = 1.89, 2.85) that in zebus. Animals between 5 and 9 years of age were at higher (OR = 2.37; 95% CI = 1.80, 3.12) risk of bovine TB than those 2 years of age or below. A significant difference (χ2 = 351; P < 0.001) in the occurrence of TB lesions in lymph nodes was recorded; the mesenteric lymph node (mean pathology score ± SEM, 1.95 ± 0.08) was most severely affected, followed by the retropharyngeal (0.80 ± 0.05) and caudal mediastinal (0.8 ± 0.06) lymph nodes. Fifty-six percent (n = 145) of the animals with gross TB lesions were culture positive; the lowest culture positivity was recorded in the skin lesions (27.3%) and the lesions of the mesenteric lymph node (31.5%). Both the skin test response and the postmortem findings suggested a higher susceptibility to bovine TB in Holsteins than zebus under identical field husbandry conditions (on pasture). In the light of increased numbers of Holstein cattle introduced into this area to raise milk production to satisfy the needs of Addis Ababa's growing population, these findings highlight the need for a control program in these herds.
Bovine tuberculosis (TB) is caused by intracellular infection with the acid-fast bacterium Mycobacterium bovis. In cattle, exposure to this organism can result in a chronic disease that jeopardizes animal welfare and productivity and in some countries leads to significant economic losses (36). Moreover, human TB of animal origin caused by M. bovis is becoming increasingly important in developing countries. In sub-Saharan Africa, humans and animals share the same microenvironment and water holes, especially during droughts and the dry season, thereby potentially promoting the transmission of M. bovis from animals to humans. In industrialized countries, bovine TB is controlled by testing and slaughter of animals and pasteurization of milk, and therefore the risk of human infection is minimized. In Africa, however, bovine TB represents potential health hazards for both animals and humans. Nonetheless, in most African countries, M. bovis infection remains an uninvestigated problem (13). In general, the epidemiology and public health significance of bovine TB in Africa remain largely unknown. Many of the factors which account for this are politico-economic, including the high cost of testing, social unrest and ethnic war, displacement of large numbers of human and animal populations, and a lack of veterinary expertise and communication networks, as well as insufficient collaboration between neighboring countries (6). Moreover, scarce human and financial resources are absorbed by action against the incidence of other acute and fatal diseases, such as contagious bovine pleuropneumonia, foot and mouth disease, African and classical swine fever, and parasitic diseases (6).
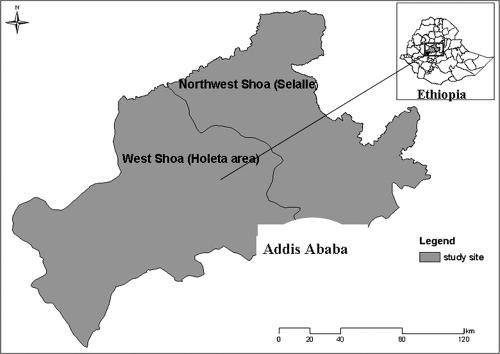
In Ethiopia, although the endemic nature of bovine TB has been known since 1967, little information about its epidemiology and its public health significance is available. It is estimated that 82% of the milk is supplied unpasteurized by intra- and peri-urban producers to consumers, while only 18% is supplied by dairy enterprises in pasteurized form. The central highlands, mainly Selalle and Holeta (Fig. 1), are the major dairying areas, and as a result they are the main sources of milk for Addis Ababa, Ethiopia's capital and main urban population center, where 8% of its inhabitants live. Furthermore, farmers in Selalle and Holeta are conscious of the milk market and produce milk for commercial sale, unlike the majority of Ethiopian farmers, who produce milk for home use. In Selalle and Holeta, farmers keep high-yield crossbred (zebu × Holstein) and Holstein dairy cattle mainly for milk production alongside native zebu breeds. It is of paramount importance to assess the difference in susceptibility to bovine TB among the native zebus and the exotic Holsteins or their crosses with zebus kept under identical husbandry conditions. Thus, this study was designed to compare the prevalence and severity of bovine TB among zebus, Holsteins, and zebu-Holstein crosses kept on pasture by traditional farmers in central Ethiopia.
FIG. 1.
Map of the study area. Selalle and Holeta are known for their dairy production. Farmers in these areas keep three major breeds of cattle (Holstein, zebu, and Holstein × zebu) under similar conditions. Unlike the majority of Ethiopian farmers, who use milk for home consumption, farmers in Holeta and Selalle sell milk, and the two areas are the major sources of milk for Addis Ababa.
MATERIALS AND METHODS
Study area and animals.
The study was conducted in two areas (Fig. 1), namely, West Shewa (Holeta area) and North West Shewa (commonly called Selalle), which are located in the central highlands of Ethiopia. The climate of the two areas is predominantly temperate and thus conducive to dairy production. Smallholder farmers rear dairy cattle for production of milk that is sold to consumers. These areas were selected because relatively high concentrations of Holsteins and/or crosses are found alongside native zebus (mainly of the Arsi breed). In addition, the two study areas are among the few areas of Ethiopia where the two types of cattle and their cross-breeds are kept under similar conditions by traditional farmers, making a comparative study possible. The study districts and villages were further selected on the basis of the concentration of Holsteins and their interaction with zebus. The total number of Holsteins and crosses in the study areas is estimated to be 40,000, of which about 30,000 are managed under a traditional farming system (grazing in the field) by local farmers, while the other 10,000 are managed under intensive or semi-intensive farming conditions by members of the private sector (investors). All of the farmers who keep either Holsteins or crosses also keep zebus, as keeping the former breed is a new development in the area. The average herd size (at household level) in traditional cattle farming was 10, half being Holsteins and/or crosses and the other half being zebus. The ratio of Holsteins to zebus in the study herds was 1:3, while that of Holsteins to crosses was 1:2. The total number of herds containing mixed breeds under traditional management in the study area was estimated to be 6,000; the majority of the farmers keep zebus alone. Study animals were selected from herds with at least one Holstein or cross that was kept with zebus. Thus, 100% of the sampled herds keep zebus as well as either Holsteins, crosses, or both. For the present study, a total of 573 herds (10% of the target herds) were randomly selected and tested. Once herds were selected, all cattle within the herds over 6 months of age were tested. The numbers of cattle included in this study also constituted about 10% (2,846 = 925 Holsteins and 1,921 crosses) of the crosses/Holsteins and 9% (2, 578) of the zebus in the target population. The age structures of all the three breeds were similar, as all three breeds were kept for the same purposes, i.e., females were predominantly for milk production while males were for plowing. Moreover, the body conditions of the three breeds were similar, as they were managed under identical husbandry systems.
Comparative intradermal tuberculin test.
Purified protein derivatives (PPDs), which are crude proteins extracted from mycobacteria, were used for this study. Avian PPD (PPD-A) is extracted from Mycobacterium avium, while bovine PPD (PPD-B) is extracted from M. bovis. The two antigens were used to increase the specificity of the skin test. For each of the 5,424 cattle, two sites on the right side of the mid-neck, 12 cm apart, were shaved, and the skin thicknesses were measured with calipers. One site was injected with an aliquot of 0.1 ml containing 2,500 IU/ml PPD-B (Veterinary Laboratories Agency, Addlestone, Surrey, United Kingdom). Similarly, 0.1 ml of 2,500 IU/ml PPD-A (Veterinary Laboratories Agency) was injected into the second site. After 72 h, the skin thickness at the injection sites was measured, and the difference between the reaction sizes at the two injection sites was determined. An animal was classified as tuberculin positive if the increase in the skin thickness at the injection site for PPD-B was at least 4 mm greater than the increase in skin thickness at the injection site for PPD-A. In addition, to assess skin test responses to PPD-A and PPD-B individually, skin indurations greater than 4 mm after each PPD injection were considered positive.
Body condition scoring.
The body condition of each of the study animal was scored using the guidelines established by Nicholson and Butterworth (32). Accordingly, on the basis of observation of anatomical parts such as vertebral column, ribs, spines, tip of tail, etc., the study animals were classified as lean (score, 1 to 3), medium (4 to 6), or fat (7 to 9).
Postmortem examination and pathology scoring.
A total of 153 animals (80 Holsteins and 73 zebus) with positive skin test reactions were slaughtered for postmortem examination and pathology scoring. All 73 zebus and 50 of the 80 Holsteins were obtained from grazing herds that were kept under identical traditional cattle management systems, while 30 of the Holsteins were obtained from an intensive herd; these 30 were not used for comparison of severity of pathology between the two breeds to avoid the bias that could be caused by the intensive husbandry. These 123 cattle were obtained from among the 5,424 cattle tested for bovine TB prevalence and were selected on the basis of the level of skin indurations and willingness of the owners to sell them for this research purpose. The spectrum of PPD-B and PPD-A responses was similar between the two breeds, and each animal was selected when the difference between the response to PPD-and the response to PPD-A was greater than 4 mm.
The lungs and lymph nodes were removed for the investigation of lesions. The seven lobes of the two lungs, including the left apical, left cardiac, left diaphragmatic, right apical, right cardiac, right diaphragmatic, and right accessory lobes, were inspected externally and palpated. Then, each lobe was sectioned into ∼2-cm-thick slices to facilitate the detection of lesions. Similarly, lymph nodes, namely, the mandibular, medial retropharyngeal, cranial and caudal mediastinal, left and right bronchial, hepatic, and mesenteric lymph nodes, were sliced into thin sections (circa 2 mm thick) and inspected for the presence of visible lesions. When gross lesions suggestive of bovine TB were found in any of the tissues, the animal was classified as having lesions. The severity of the gross lesions was scored by the semiquantitative procedure developed by Vordermeier et al. (43), with minor modifications to facilitate performance under field conditions (1). Briefly, lesions in the lobes of the lungs were scored separately as follows: 0 = no visible lesions; 1 = no gross lesions but lesions apparent on slicing of the lobe; 2 = fewer than five gross lesions; 3 = more than five gross lesions; 4 = gross coalescing lesions. The scores for the individual lobes were added up to calculate the lung score. Similarly, the severity of gross lesions in individual lymph nodes was scored as follows: 0 = no gross lesions; 1 = small lesion at one focus (just starting); 2 = small lesions at more than one focus; 3 = extensive necrosis. Individual lymph node scores were added up to calculate the lymph node score. Finally, both lymph node and lung pathology scores were added up to determine the total pathology score per animal.
Isolation of mycobacteria.
Suspicious tissues from 145 cattle were further processed for isolation of mycobacteria in accordance with Office International de Epizooties (4) protocols. Briefly, tissue specimens for culture were collected in sterile universal bottles in 5 ml of 0.9% saline solution and then transported to the laboratory by maintaining a cold chain. In the laboratory, the specimens were sectioned using sterile blades and then homogenized with a mortar and pestle. The homogenate was decontaminated by adding an equal volume of 4% NaOH by centrifugation at 3,000 rpm for 15 min. The supernatant was discarded, and the sediment was neutralized by 1% (0.1 N) HCl using phenol red as an indicator. Neutralization was achieved when the color of the solution changed from purple to yellow (5). Next, 0.1 ml of suspension from each sample was spread onto a slant of Lowenstein-Jensen medium. Duplicate slants were used, one enriched with sodium pyruvate and one enriched with glycerol. Cultures were incubated aerobically at 37°C for about 5 to 8 weeks with weekly observation for growth of colonies.
Data analysis.
Individual animal prevalence was defined as the number of positive reactors per 100 animals tested. Logistic regression analysis was used to assess the association between prevalence and animal risk factors using STATA statistical software (STATA Corporation, College Station, TX). The differences in prevalence between the different breeds and proportions were compared using the dose format of Epitable (Epinfo, version 6). The difference between the effects of different risk factors on prevalence was analyzed using the Pearson chi-square (χ2) test. The odds ratio (OR) was calculated to assess the strength of association of different factors with the prevalence of bovine TB. The Mann-Whitney test was used to compare pathology scores between cattle types.
RESULTS
Prevalence of bovine TB assessed by tuberculin skin testing.
The overall prevalence of bovine TB, as judged by the number of skin test-positive cows, was 13.5% (n = 5,424) in dairy cattle reared in the central highlands of Ethiopia. The prevalence of bovine TB was significantly higher in Holsteins than in either zebus (predominantly of the Arsi breed) (22.2% versus 11.6%, χ2 = 61.8; P < 0.001) or zebu-Holstein crosses (22.2% versus 11.9%, χ2 = 50.7; P < 0.001). In contrast, the skin test prevalence difference between zebus and crosses was not statistically significant (χ2 = 0.11; P = 0.74). The results of a logistic regression analysis of host risk factors for bovine TB are presented in Table 1. Multivariable logistic regression analysis showed that Holsteins were more than twice as likely to present as tuberculin positive, i.e., infected with M. bovis, than zebus (OR = 2.32; confidence interval [CI] = 1.89, 2.85). Similarly, animals between 5 and 9 years of age were at a higher risk of infection (OR = 2.37; CI = 1.80, 3.12) with TB than those 2 years of age or below.
TABLE 1.
Association of host-related risk factors with the prevalence of bovine TB in the central highlands of Ethiopia, determined using multivariable analysisa
| Factor | No. (%) of animals
|
OR (95% CI)
|
||
|---|---|---|---|---|
| Examined | Positive for TB | Crude | Adjusted | |
| Sex | ||||
| Male | 2,289 | 316 (13.8) | 1 | 1 |
| Female | 3,135 | 416 (13.3) | 0.96 (0.82, 1.12) | 0.94 (0.79, 1.11) |
| Breed | ||||
| Zebu | 2,578 | 298 (11.6) | 1 | 1 |
| Cross | 1,921 | 229 (11.9) | 1.04 (0.86, 1.26) | 1.14 (0.94, 1.38) |
| Holstein | 925 | 205 (22.2) | 2.18 (1.88, 2.65) | 2.32 (1.89, 2.85) |
| Age (yr) | ||||
| <2 | 892 | 73 (8.2) | 1 | 1 |
| 2-5 | 1,868 | 237 (12.7) | 1.63 (1.24, 2.15) | 1.63 (1.23, 2.16) |
| 5-9 | 1,792 | 317 (17.7) | 2.41 (1.84, 3.15) | 2.37 (1.80, 3.12) |
| >9 | 872 | 105 (12.0) | 1.54 (1.12, 2.10) | 1.51 (1.09, 2.09) |
| Body condition | ||||
| Lean (thin) | 1,373 | 152 (17.1) | 1 | 1 |
| Medium (meat) | 3,802 | 511 (13.4) | 1.25 (1.03, 1.51) | 1.13 (0.93, 1.39) |
| Fat | 249 | 69 (27.7) | 3.08 (2.23, 4.26) | 2.53 (1.80, 3.57) |
Both crude and adjusted ORs were used to assess the level of association of prevalence with the different host factors.
Relationship between skin reactions to PPD-B and PPD-A.
To assess individual skin test responses to PPD-A and PPD-B, skin indurations greater than 4 mm after PPD injection were considered positive. A strong association (Pearson χ2 = 1,300; P < 0.001) between skin reactions to PPD-A and PPD-B was noted. As indicated in Table 2, 4.8% of the study animals responded positively to both PPD-A and PPD-B. On the other hand, 8.7% of them reacted only to PPD-B, while 1.3% reacted only to PPD-A.
TABLE 2.
Responses to PPD-A and PPD-Ba
| PPD-A result | No. (%) of animals with PPD-B result
|
Total no. (%) | |
|---|---|---|---|
| Positive | Negative | ||
| Positive | 258 (4.8) | 68 (1.3) | 326 (6.1) |
| Negative | 474 (8.7) | 4,624 (85.3) | 5,098 (93.9) |
| Total | 732 (13.5) | 4,692 (86.5) | 5,424 (100) |
Positive and negative reactions were defined as skin indurations of >4 mm and ≤4 mm, respectively. Pearson χ2 = 1,300; P < 0.001.
Necropsy findings.
Lesion distribution and disease severity were established in 153 skin test-positive animals that had gross pathological lesions typical of bovine TB when examined postmortem. Gross lesions typical of bovine TB were detected in 95% (145/153) of the reactor animals studied. The occurrence of TB lesions in the lymph nodes and lungs is presented in Table 3 as percentage of total animals assessed. A significant difference (χ2 = 351; P < 0.001) in the tropism of TB lesions in lymph nodes was found: the percentage of mesenteric lymph nodes containing lesions was highest (94.5%), followed by retropharyngeal (74.5%) and caudal mediastinal lymph nodes (64.4%). In contrast, no tropism of TB lesions for particular parts of the lung was observed (χ2 = 4.43; P = 0.49).
TABLE 3.
Distribution of tuberculous lesions in the lymph nodes and lobes of lungs of 145 skin test positive cattle with lesions in at least one tissue or organ
| Tissue | No. (%) of animals
|
χ2; P | |
|---|---|---|---|
| Examined | Positive | ||
| Lymph nodes and skin | 351; 0.0000 | ||
| Mandibular | 145 | 19 (13.1) | |
| Retropharyngeal | 145 | 108 (74.5) | |
| Cranial mediastinal | 145 | 54 (37.2) | |
| Caudal mediastinal | 145 | 92 (63.4) | |
| Left bronchial | 145 | 59 (40.7) | |
| Right bronchial | 145 | 49 (33.8) | |
| Mesenteric | 145 | 137 (94.5) | |
| Skin | 145 | 11 (7.6) | |
| Lobes of lungs | 4.43; 0.49 | ||
| Left apical | 145 | 6 (4.1) | |
| Left cardiac | 145 | 10 (6.9) | |
| Left diaphragmatic | 145 | 10 (6.9) | |
| Right apical | 145 | 8 (5.5) | |
| Right cardiac | 145 | 6 (4.1) | |
| Right diaphragmatic | 145 | 13 (9.0) | |
| Right accessory | 145 | 11 (7.6) | |
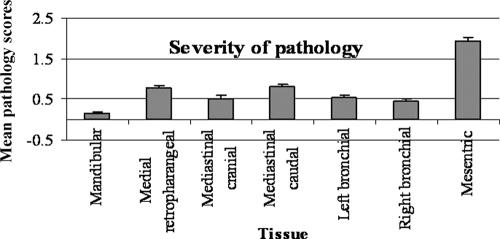
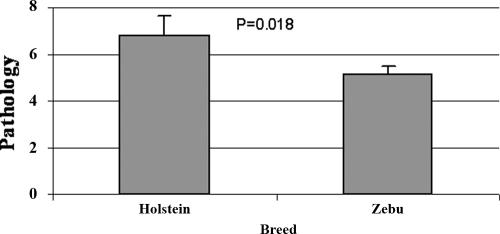
Figure 2 shows the severity of pathology of bovine TB determined using a semiquantitative scoring system (1, 43). Extending the findings presented in Table 3, the mesenteric lymph nodes constituted the most severely affected lymph nodes (mean pathology score ± standard error of the mean [SEM], 1.95 ± 0.08), followed by retropharyngeal (0.80 ± 0.05) and caudal mediastinal (0.8 ± 0.06) lymph nodes. The severity of pathology in Holstein and zebus was also assessed, and as shown in Fig. 3, the severity of pathology in Holsteins (mean pathology score ± SEM, 6.84 ± 0.79; median score [range], 6.0 [2 to 42]) was significantly higher (P = 0.018, Mann-Whitney test) than the severity of pathology in zebus (5.21 ± 0.30; 5.0 [1 to 17]).
FIG. 2.
Mean pathology scores of lymph nodes. Pathology scores were determined as defined by Vordermeier et al. (43). Results are expressed as the mean score for each lymph node ± SEM.
FIG. 3.
Mean pathology score in skin test-positive cattle assessed in this study. These animals were selected from among skin test-positive animals on the basis of the size of skin indurations and willingness of the owners to sell. The pathology was significantly severe (P = 0.018, Mann-Whitney test) in Holsteins (n = 50) than in zebus (n = 73) under identical husbandry conditions.
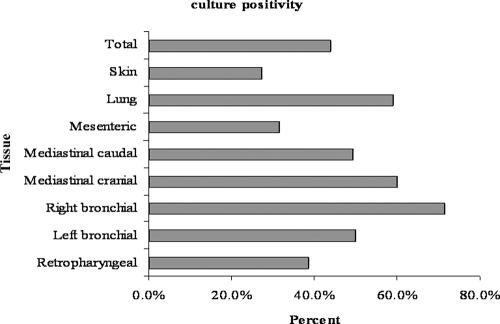
Bacteriology.
Fifty-six percent (81/145) of the animals with gross TB lesions yielded a positive culture from at least one lymph node or other tissue sample. As indicated in Fig. 4, the highest proportion of culture positivity (71.43%) was observed in right bronchial lymph nodes, while the lowest percentage was observed in the skin (27.3%) and in the mesenteric lymph nodes (31.5%). However, culture positivity of suspicious lesions did not differ (χ2 = 0.13, P = 0.72; comparison of proportions by use of the dose format of Epitable [Epinfo, version 6]) between Holstein (54%, n = 50) and zebu (51%, n = 73) breeds kept under identical field husbandry conditions.
FIG. 4.
Rate of culture positivity of suspicious tissues obtained from 145 animals with gross tuberculous lesions, as confirmed by the observation of acid-fast bacilli in the colonies. Culture positivity did not differ (χ2 = 0.13, P = 0.72) between Holsteins (54%, n = 50) and zebus (51%, n = 73) kept under identical field husbandry conditions.
DISCUSSION
The prevalence of bovine TB recorded by the present study (13.5%) is moderate. Previously, a similar prevalence (14.2%, n = 416) (3) was reported for Wolaita Soddo, in southern Ethiopia, where cattle farming is similar to that in the central highlands. In both locations, farmers keep cross-bred cattle and Holsteins in addition to zebus for milk production. Large numbers of cattle were enrolled in the present study, and the area coverage was also larger than in previous studies. Thus, the results of this study represent an accurate picture of the disease in parts of the country where farmers keep three different breeds (zebu, zebu × Holstein, and Holstein) under field (semiextensive) management conditions. However, a lower prevalence (4.1%; n = 460) was reported for zebu cattle under traditional management in the Boji district of western Ethiopia (22). In contrast, a significantly higher prevalence of positive skin test results (46.8%; n = 1,171) was reported for 12 intensive dairy farms which keep crossbreed and Holstein cattle (2). Thus, as also indicated by previous studies (1), the prevalence of bovine TB is predominantly affected by cattle management and, to a lower degree, by cattle breed. The result of the present study showed that the prevalence of bovine TB was significantly higher in Holsteins than in crosses or in zebus kept under identical husbandry conditions. Furthermore, although the distribution of the pathology in reaction-positive animals of the two breeds was comparable, the severity of pathology was significantly higher in Holsteins than in Arsi zebus. This study therefore extends an earlier pilot study that also showed a trend of lower pathology scores in zebus, although because fewer animals were assessed in the earlier study, the difference in disease severity was not statistically significant (1). Historical reports also indicated that Bos taurus taurus animals (the group to which Holsteins belong) are more susceptible to bovine TB than Bos taurus indicus, i.e., zebus (9, 37), although few contemporary data, particularly on African cattle and on Holstein cattle versus native breeds, are available. Our study therefore substantiates and extends these earlier findings.
Experimental studies also support the notion of susceptibility differences between B. t. taurus and B. t. indicus breeds: experimental M. bovis infection of calves of taurine cattle and zebus with 50 mg of a bovine strain of the tubercle bacillus with standard virulence indicated marked resistance in zebu calves, while calves of Ankole (taurine cattle of African origin) and European breeds were susceptible (9). Thus, in general, increased resistance to bovine TB has been attributed to zebu breeds, and the significance of different breed susceptibilities in cattle in developed countries, which are almost exclusively of B. t. taurus background, has been discounted (34). The gene Nramp1 has been shown to correlate with resistance to Brucella abortus and M. bovis BCG in cattle (36). In mice, the Nramp1 protein plays an important role in resistance (17). This protein is a divalent cation transporter and has affinity for both iron and manganese (19, 20). However, Nramp1 polymorphisms associated with resistance in mice failed to protect cattle against TB (7). In humans, some evidence predicts a role for Nramp in resistance (21). However, to reach a conclusion, more extensive studies are needed to define such resistance genes, which could help to support targeted breeding strategies for developing more resistant cattle breeds (25, 27, 42). Other factors, such as nutrition, also influence the susceptibility of cattle to bovine TB. In a case control study, Griffin et al. (18) found an association between recurrent herd outbreaks of bovine TB and the presence of rough grazing, which suggested that nutritional deficiencies lead to reduced resistance to bovine TB. Doherty et al. (14) demonstrated significantly lower numbers of lymphocyte subpopulations in nutritionally deficient cattle. Susceptibility to M. bovis infection may also be enhanced in cattle persistently infected with immunosuppressive viruses, such as bovine viral diarrhea virus or bovine immunodeficiency virus (28). Similarly, responses to the tuberculin skin test depend on the capabilities of the cellular immune response, which in turn is affected by the level of nutrition in terms of protein energy and micronutrients (35). Thus, animals in good physical condition respond to tuberculin skin tests better than those in poor physical condition, as was also observed in this study.
The proportion of reaction-positive animals increased with age, reaching a maximum in animals between 5 and 9 years of age and then declining. Similarly, studies in Canada and Northern Ireland indicated an increased incidence of bovine TB with increased age (30). The reason could be, as suggested earlier by Mackay and Hein (24), the possible influence of γδ T cells, which are predominantly found in the circulation of young calves. Previous studies have shown the role of γδ T cells in antimycobacterial immunity (41). It has been suggested that increased incidence of TB in older animals can be explained by a waning of protective capability in aging animals, as experimentally confirmed in the murine system (33). Furthermore, it could be due to the increase in the likelihood of encountering M. bovis over a longer period (8). The difference in results between cattle of different ages could also be a result of the slow progression of disease to a detectable level.
The frequency and severity of the lesions were higher in the mesenteric lymph nodes than the thoracic lymph nodes. This result differed from results of previous studies, which reported that 90% of TB lesions occur in the respiratory system in developed countries (11, 12, 15, 16, 23, 26, 31, 40, 44). In another study conducted on 2,886 cattle, 57% had lesions in the thoracic cavity, while only 3% had lesions solely in the mesenteric lymph nodes (31). However, these studies were conducted in developed countries with different, and in most cases more intensive, husbandry systems. Therefore, respiratory excretion and inhalation of M. bovis are considered the main route by which animal-to-animal transmission occurs in developed countries (15, 39). In contrast, the result of the present study could suggest that shedding of M. bovis in the feces and ingestion of the bacilli with contaminated pasturage and/or water may be the main route of transmission in cattle kept on pasture, as the mesenteric lymph node was found to be the main lesion-containing site. Nevertheless, in developed countries, shedding of M. bovis in urine and feces is considered to be an insignificant feature of disease transmission in cattle (19, 29).
Reaction bias to M. avium PPD could be due to infection with Mycobacterium avium subsp. avium and Mycobacterium avium subsp. paratuberculosis. M. avium subsp. paratuberculosis causes paratuberculosis and is transmitted by the fecal-oral route (5). Cattle, the most affected species, are most susceptible to infection when they are young (10). M. avium subsp. paratuberculosis is zoonotic and was recently isolated from the blood, urine, sputum, feces, and biopsy samples of an AIDS patient (38). Therefore, the large proportion of PPD-A-biased reactions could be due to M. avium subsp. paratuberculosis, which also has both zoonotic and economic significance and hence requires further investigation.
In conclusion, this study determined the prevalence, based on skin test reactivity, of bovine TB in cattle reared under low-intensity farming conditions in the central highland of Ethiopia. The prevalence was significant yet considerably lower than in cattle reared under more intensive farming conditions. We also found significantly lower prevalence in native zebu breeds than exotic Holstein cattle; this difference in breed susceptibility was also highlighted by the demonstration of increased disease severity in Holsteins. In the light of the introduction of increased numbers of Holstein cattle into this area to raise milk production to satisfy the needs of Addis Ababa's growing population, these findings highlight the need for a control program in these herds.
Acknowledgments
The Wellcome Trust is acknowledged for its financial support.
The technical support of Surane Gemeda and the other technical staff of the Animal Health and Zoonoses Unit of the Aklilu Lemma Institute of Pathobiology is also acknowledged.
Footnotes
Published ahead of print on 29 August 2007.
REFERENCES
- 1.Ameni, G., A. Aseffa, H. Engers, D. B. Young, G. R. Hewinson, and M. H. Vordermeier. 2006. Cattle husbandry is a predominant factor affecting the pathology of bovine tuberculosis and IFN-γ responses to mycobacterial antigens. Clin. Vaccine Immunol. 13:1030-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ameni, G., P. Bonnet, and M. Tibbo. 2003. A cross-sectional study on bovine tuberculosis in cattle and its zoonotic implications in selected zones of Ethiopia. Int. J. Appl. Res. Vet. Med. 1:253-258. [Google Scholar]
- 3.Ameni, G., A. Ragassa, T. Kassa, and G. Medhin. 2001. Survey on bovine tuberculosis in cattle and its public health implications to cattle raising families in Wolaita Soddo, southern Ethiopia. Ethiopian J. Anim. Prod. 1:55-62. [Google Scholar]
- 4.Anonymous. 2000. Manual of standards for diagnostics and vaccines. Office International de Epizooties, Paris, France.
- 5.Anonymous. 23 July 2004, revision date. Manual of standards for diagnostic tests and vaccines for terrestrial animals. Office International des Epizooties, Paris, France. http://www.oie.int/eng/normes/mmanual/A_00045.htm.
- 6.Ayele, W. Y., S. D. Neill, J. Zinsstag, M. G. Weiss, and I. Pavlik. 2004. Bovine tuberculosis: an old disease but a new threat to Africa. Int. J. Tuberc. Lung Dis. 8:924-937. [PubMed] [Google Scholar]
- 7.Barthel, R., J. A. Piedrahita, D. N. McMurry, J. Payeur, and D. Baca. 2002. Pathologic findings and association of Mycobacterium bovis infection with bovine Nramp1 gene in cattle from herds with naturally occurring tuberculosis. Am. J. Vet. Res. 61:1140-1144. [DOI] [PubMed] [Google Scholar]
- 8.Barwinek, F., and N. M. Taylor. 1996. Assessment of the socio-economic importance bovine tuberculosis in Turkey and possible strategies for control or eradication, p. 3-45. Turkish-German Animal Health Information Project, General Directorate of Protection and Control, Ankara, Turkey.
- 9.Carmichael, J. 1940. Bovine tuberculosis. Vet. J. 97:329-339. [Google Scholar]
- 10.Chacon, O., L. E. Bermudez, and R. G. Barletta. 2004. Johne's disease, inflammatory bowel disease, and Mycobacterium paratuberculosis. Annu. Rev. Microbiol. 58:329-363. [DOI] [PubMed] [Google Scholar]
- 11.Collins, J. D. 1996. Factors relevant to M. bovis eradication. Irish Vet. J. 49:241-243. [Google Scholar]
- 12.Corner, L. A. 1994. Post mortem diagnosis of Mycobacterium bovis infection in cattle. Vet. Microbiol. 40:53-63. [DOI] [PubMed] [Google Scholar]
- 13.Cosivi, O., L. A. Robinson, C. J. Daborn, M. C. Raviglionne, T. Fujikura, D. Cousisins, J. M. Grage, H. A. Huch, F. K. Zermeyer, I. de Kantor, and F. Meslin. 1998. Zoonotic tuberculosis due to M. bovis in developing countries. Emerg. Infect. Dis. 4:59-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doherty, M. L., M. L. Monaghan, H. F. Bassett, P. J. Quinn, and W. C. Davis. 1995. Effect of dietary restriction on cell-mediated immune responses in cattle infected with Mycobacterium bovis. Vet. Immunol. Immunopathol. 49:307-320. [DOI] [PubMed] [Google Scholar]
- 15.Francis, J. 1958. Tuberculosis in animals and man. Cassell & Co., London, United Kingdom.
- 16.Francis, J. 1972. Route of infection in tuberculosis. Aust. Vet. J. 48:578. [DOI] [PubMed] [Google Scholar]
- 17.Frehel, C., F. Canonne-Hergaux, P. Gros, and C. De Chastellier. 2002. Effect of Nramp1 on bacterial replication and on maturation of Mycobacterium avium-containing phagosomes in bone marrow-derived mouse macrophages. Cell Microbiol. 4:541-556. [DOI] [PubMed] [Google Scholar]
- 18.Griffin, J. M., T. Hahsey, K. Lynch, M. D. Salman, J. McCarthy, and T. Hurley. 1993. The association of cattle husbandry practices, environmental factors, and farmers characteristics with the occurrence of chronic bovine tuberculosis in dairy cattle in Republic of Ireland. Prev. Vet. Med. 17:145-160. [Google Scholar]
- 19.Hardie, R. M., and J. M. Watson. 1992. Mycobacterium bovis in England and Wales: past, present and future. Epidemiol. Infect. 109:23-33. [PMC free article] [PubMed] [Google Scholar]
- 20.Kehres, D. G., and M. E. Maguire. 2003. Emerging themes in manganese transport, biochemistry and pathogenesis in bacteria. FEMS Microbial. Rev. 27:263-290. [DOI] [PubMed] [Google Scholar]
- 21.Kim, J. H., S. Lee, S. H. Lee, C. Sin, and J. J. Shim. 2003. Nramp1 genetic polymorphisms as a risk factor of tuberculosis pleurisy. Int. J. Tuberc. Lung Dis. 7:370-375. [PubMed] [Google Scholar]
- 22.Laval, G., and G. Ameni. 2004. Prevalence of bovine tuberculosis in zebu cattle under traditional animal husbandry in Boji District of western Ethiopia. Rev. Med. Vet. 155:494-499. [Google Scholar]
- 23.Lepper, A. W. D., and C. W. Pearson. 1973. Tuberculosis of beef cattle. Aust. Vet. J. 49:266-267. [DOI] [PubMed] [Google Scholar]
- 24.Mackay, C. R., and W. R. Hein. 1989. A large proportion of bovine T cells express the δγ T cell receptor and show a distinct tissue distribution and surface phenotype. Int. Immunol. 1:540-545. [DOI] [PubMed] [Google Scholar]
- 25.Malo, D., J. Hu, E. Skamene, and E. Schurr. 1994. Population and molecular genetics of susceptibility to intracellular pathogens. Anim. Biotechnol. 5:173-182. [Google Scholar]
- 26.McIlroy, S. G., S. D. Neill, and R. M. McCracken. 1986. Pulmonary lesions and Mycobacterium bovis excretion from the respiratory tract of tuberculin reacting cattle. Vet. Rec. 118:718-721. [DOI] [PubMed] [Google Scholar]
- 27.McLeod, R., E. Buschman, and L. D. Arbuckle. 1995. Immuno-genetics in the analysis of resistance to intracellular pathogens. Curr. Opin. Immunol. 7:539-552. [DOI] [PubMed] [Google Scholar]
- 28.Menzies, F. D., and S. D. Neill. 2000. Cattle-to-cattle transmission of bovine tuberculosis (a review). Vet. J. 160:92-106. [DOI] [PubMed] [Google Scholar]
- 29.Morris, R. S., D. U. Pfeiffer, and R. Jackson. 1994. The epidemiology of Mycobacterium bovis infections. Vet. Microbiol. 40:153-177. [DOI] [PubMed] [Google Scholar]
- 30.Munroe, F. A., I. R. Dohoo, and W. B. McNab. 2000. Estimates of within herd incidence rates of Mycobacterium bovis in Canadian cattle and cervids between 1985 and 1994. Prev. Vet. Med. 45:247-256. [DOI] [PubMed] [Google Scholar]
- 31.Neill, S. D., J. M. Pollock, D. B. Bryson, and J. Hanna. 1994. Pathogenesis of Mycobacterium bovis infection in cattle. Vet. Microbiol. 40:41-52. [DOI] [PubMed] [Google Scholar]
- 32.Nicholson, M. J., and M. H. Butterworth. 1986. A guide to condition scoring in zebu cattle, p. 1-29. International Livestock Centre for Africa, Addis Ababa, Ethiopia.
- 33.O'Reilly, L. M., and C. J. Daborn. 1995. The epidemiology of Mycobacterium bovis infections in animals and man: a review. Tuberc. Lung Dis. 76:1-146. [DOI] [PubMed] [Google Scholar]
- 34.Orme, I. M. 1987. Aging and immunity to tuberculosis: increased susceptibility of old mice reflects a decreased capacity to generate mediator T lymphocytes. J. Immunol. 138:4414-4418. [PubMed] [Google Scholar]
- 35.Pollock, J. M., and S. D. Neill. 2002. Mycobacterium bovis infection and tuberculosis in cattle. Vet. J. 163:115-127. [DOI] [PubMed] [Google Scholar]
- 36.Qureshi, T., J. Templeton, and L. G. Adams. 1996. Intracellular survival of Brucella abortus, Mycobacterium bovis BCG, Salmonella dublin, Salmonella typhimurium in macrophages from cattle genetically resistant to Brucella abortus. Vet. Immunol. Immunopathol. 50:55-65. [DOI] [PubMed] [Google Scholar]
- 37.Radostits, S. M., D. C. Blood, and C. C. Gray. 1994. Veterinary medicine. A textbook of disease of cattle, sheep, pigs, goats and horse, 8th ed., p. 748-785. Baillière Tindal, London, United Kingdom.
- 38.Richter, E., J. Wessling, N. Lugering, W. Domschke, and S. Rusch-Gerdes. 2002. M. avium subsp. paratuberculosis in a patient with HIV, Germany. Emerg. Infect. Dis. 8:729-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smyth, A. J., M. D. Welsh, R. M. Girvin, and J. M. Pollock. 2001. In vitro pensiveness of γδ T cells from Mycobacterium bovis infected cattle to mycobacterial antigens: predominant involvement of WC1+ cells. Infect. Immun. 69:89-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stamp, J. T. 1944. A review of the pathogenesis and pathology of bovine tuberculosis with especial reference practical problems. Vet. Rec. 56:443-446. [Google Scholar]
- 41.Stamp, J. T. 1948. Bovine pulmonary tuberculosis. J. Comp. Pathol. 58:9-23. [DOI] [PubMed] [Google Scholar]
- 42.Templeton, J., and G. Adams. 1995. Genetics of natural resistance to tuberculosis, p. 28-32. In Proceedings of the second international conference on Mycobacterium bovis held in the University of Otago, New Zealand on 28 August-1 September, 1995. University of Otago Press, Dunedin, New Zealand.
- 43.Vordermeier, H. M., M. A. Chambers, P. J. Cockle, A. O. Whelan, J. Simmons, and R. G. Hewinson. 2002. Correlation of ESAT-6-specific gamma interferon with pathology in cattle following Mycobacterium bovis BCG vaccination against experimental bovine tuberculosis. Infect. Immun. 70:3026-3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whipple, D. L., C. A. Bolin, and J. M. Miller. 1996. Distribution of lesion in cattle infected with Mycobacterium bovis. J. Vet. Diagn. Investig. 8:351-354. [DOI] [PubMed] [Google Scholar]