Histoplasmosis can be difficult to diagnose, as patients with the disease present with symptoms similar to those of other endemic mycoses (2, 5, 6). The causative agent, Histoplasma capsulatum, is a dimorphic fungus that can be cultured from patient specimens only after several weeks of incubation. Serology is diagnostic only for immunocompetent patients given appropriate time for an immune response. Histopathology can be diagnostic but requires a tissue sample collected invasively (1, 7). Histoplasma antigen detection using polyclonal antibodies is nonspecific but can be a useful method performed on easy-to-obtain urine samples (8, 9).
We read with interest the study by the investigators at MiraVista Diagnostics (MVD) and MiraBella Technologies (4) evaluating the IMMY ALPHA histoplasma antigen enzyme immunoassay (EIA). Working together, IMMY and ARUP Laboratories developed this test, which has been used in production at ARUP daily since March 2006. Our experience (J.L.C. and E.R.A.) with this assay gives us insights that others may not have. We believe that the MVD study suffers from both technical and clinical flaws.
First, the assay results with control specimens reported by the MVD group are vastly different from those from our experience. In clinical specimens, our positivity rate is 2.9% (based on over 10,000 patient specimens tested), yet LeMonte et al. (4) reported that 16% of control specimens were positive by the IMMY assay. We suspect that lack of experience in using the IMMY reagents allowed the authors to accept technically flawed runs. At ARUP, the IMMY stock calibrator is diluted to make a working calibration set of 2, 10, 30, 100, 300, and 1,000 units. A typical absorbance for the 2.0-unit calibrator is 0.020 and is highly reproducible. The calibration absorbances are fitted to a four-parameter log-logit curve having typical R2 values of 0.998 to 1.000 (1a). Specimens are run in duplicate, and results must agree within 10%. Only specimens having an absorbance greater than the average 2.0-unit calibrator absorbance are considered positive.
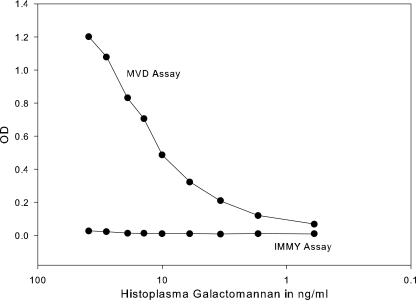
Second, the values of the positive results in the LeMonte study appear to be overly rounded (e.g., four values at 2, seven values at 5, and two values at 10, etc., instead of 2.1, 2.5, 3.6, 4.8, 4.9, and 5.0, etc.). This observation and the figure in MVD's poster on this topic (4a) showing a very flat calibration curve lead us to conclude that the IMMY reagents may have been stored improperly or that the substrate color was not allowed to develop properly. Furthermore, IMMY has no records of MVD purchasing reagents, so reagent delivery may have been circuitous enough to compromise their stability. Thus, we suspect that the MVD laboratory used the IMMY reagents in a technically flawed fashion. We (J.L.C. and E.R.A.) would be pleased to test all of the MVD study specimens in the IMMY assay to help resolve the discrepancies. In addition, if MVD would allow ARUP to purchase the MVD reagents, we would be willing to perform the MVD EIA.
On the clinical side, MVD has used one immunoassay to define a true positive without the benefit of other supporting evidence (PCR, serology, or clinical condition and course). Only 22 of 50 cases were positive using the IMMY assay. The authors assumed that any sample that tested positive by their MVD EIA was definitively positive for histoplasmosis. However, the authors had previously reported that specimens from patients confirmed positive for coccidioidomycosis, blastomycosis, penicilliosis, aspergillosis, or paracoccidioidomycosis had tested positive for the histoplasma antigen using the MVD polyclonal EIA (3, 11, 12). The histoplasma antigen-positive specimens were determined to be positive solely on the basis that they generated a positive result using the MVD EIA, which could have been false positive due to cross-reactivity. Culture, serology, histopathology, and clinical information might have been used to definitively assess infection and ultimately confirm histoplasmosis, but these alternative tests were not included in this study. Furthermore, the MVD EIA has been reported to have a false-negative rate of 15 to 30% for urine specimens (10, 13). It is possible that the MVD EIA may have a lower limit of detection (LOD) than the IMMY assay, but studies to determine the LOD were not reported (e.g., the dilution of a moderate positive below the limit of the lowest calibrator in both assays.) An LOD experiment would be valuable but would require parallel testing of a dilution series in both assays.
Third, LeMonte et al. (4) obtained a set of data that included several discrepancies, yet they did not report how the discrepancies were resolved. A new lot number of IMMY reagents should have been tested to see if there was reagent degradation. Aside from the reagent issue, there remains the issue of competency. How was competency for performing the IMMY EIA validated? ARUP Laboratories has had over 1.5 years of experience performing the IMMY EIA after completing an extensive validation. It is advisable that MVD validate the IMMY assay before drawing the conclusions that they have.
We strongly suspect a conflict of interest for MVD, which introduces a significant bias in their study. We would welcome any reagents, regardless of manufacturer, that would lead to an improved histoplasma antigen assay. At this time, both the MVD and IMMY assays have shortcomings, but the LeMonte study does not demonstrate which is best. Currently, if either the MVD EIA or the IMMY EIA is performed, clinical information and patient history are a necessary component of test interpretation. Alternative testing, such as serology, histopathology, and culture, may be suggested as well, if the samples are available. Because antigen testing is fast and requires noninvasive specimens, we will continue working to build a better assay for antigen detection and welcome any research collaborations to make this happen. Until then, we encourage transparency of information and broad collaborations to discover better targets and improved technology for a specific and sensitive antigen detection assay.
Finally, we comment on the philosophy of tightly holding the intellectual property of laboratory tests. Refusing to provide reagents for purchase so that an unbiased evaluation can be performed stifles the advancement of test improvement and stifles the demand for clinically useful tests. We support a philosophy of licensing technology to all interested clinical laboratories and encourage test improvement for those willing to invest the resources. The current histoplasma antigen assays are in need of improvement. That task is best enhanced by the collaboration of interested investigators.
REFERENCES
- 1.Bialek, R., A. Feucht, C. Aepinus, G. Just-Nübling, V. J. Robertson, J. Knobloch, and R. Hohle. 2002. Evaluation of two nested PCR assays for detection of Histoplasma capsulatum DNA in human tissue. J. Clin. Microbiol. 40:1644-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1a.Cloud, J. L., S. K. Bauman, B. P. Neary, K. G. Ludwig, and E. R. Ashwood. 2007. Performance characteristics of a polyclonal enzyme immunoassay for the quantitation of Histoplasma antigen in human urine samples. Am. J. Clin. Pathol. 128:18-22. [DOI] [PubMed] [Google Scholar]
- 2.Kauffman, C. A. 2006. Endemic mycoses: blastomycosis, histoplasmosis, and sporotrichosis. Infect. Dis. Clin. N. Am. 20:645-662. [DOI] [PubMed] [Google Scholar]
- 3.Kuberski, T., R. Myers, L. J. Wheat, M. Durkin, P. Connolly, B. M. Kubak, D. Bruckner, and D. Pegues. 2007. Diagnosis of coccidioidomycosis by antigen detection using cross-reaction with a Histoplasma antigen. Clin. Infect. Dis. 44:e50-e54. [DOI] [PubMed] [Google Scholar]
- 4.LeMonte, A., L. Egan, P. Connolly, M. Durkin, and L. J. Wheat. 2007. Evaluation of the IMMY ALPHA Histoplasma antigen enzyme immunoassay for diagnosis of histoplasmosis marked by antigenuria. Clin. Vaccine Immunol. 14:802-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4a.LeMonte, A. M., L. L. Egan, P. A. Connoly, M. M. Durkin, and L. J. Wheat. 2007. Abstr. 107th Gen. Meet. Am. Soc. Microbiol., abstr. F-039. American Society for Microbiology, Washington, DC.
- 5.Lortholary, O., D. W. Denning, and B. Dupont. 1999. Endemic mycoses: a treatment update. J. Antimicrob. Chemother. 43:321-331. [DOI] [PubMed] [Google Scholar]
- 6.McNeil, M. M., S. L. Nash, R. A. Hajjeh, M. A. Phelan, L. A. Conn, B. D. Plikaytis, and D. W. Warnock. 2001. Trends in mortality due to invasive mycotic diseases in the United States, 1980-1997. Clin. Infect. Dis. 33:641-647. [DOI] [PubMed] [Google Scholar]
- 7.Weydert, J. A., T. L. Van Natta, and B. R. DeYoung. 2007. Comparison of fungal culture versus surgical pathology examination in the detection of Histoplasma in surgically excised pulmonary granulomas. Arch. Pathol. Lab. Med. 131:780-783. [DOI] [PubMed] [Google Scholar]
- 8.Wheat, L. J. 1994. Histoplasmosis: recognition and treatment. Clin. Infect. Dis. 19:19-27. [DOI] [PubMed] [Google Scholar]
- 9.Wheat, L. J. 2001. Laboratory diagnosis of histoplasmosis: update 2000. Semin. Respir. Infect. 16:131-140. [DOI] [PubMed] [Google Scholar]
- 10.Wheat, L. J., T. Garringer, E. Brizendine, and P. Connolly. 2002. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn. Microbiol. Infect. Dis. 43:29-37. [DOI] [PubMed] [Google Scholar]
- 11.Wheat, L. J., E. Hackett, M. Durkin, P. Connolly, R. Petraitiene, T. J. Walsh, K. Knox, and C. Hage. 2007. Histoplasmosis-associated cross-reactivity in the BioRad Platelia Aspergillus enzyme immunoassay. Clin. Vaccine Immunol. 14:638-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wheat, L. J., H. Wheat, P. Connolly, M. Kleiman, K. Supparatpinyo, K. Nelson, R. Bradsher, and A. Restrepo. 1997. Cross-reactivity in Histoplasma capsulatum variety capsulatum antigen assays of urine samples from patients with endemic mycoses. Clin. Infect. Dis. 24:1169-1171. [DOI] [PubMed] [Google Scholar]
- 13.Williams, B., M. F. Fojtasek, P. Connolly-Stringfield, and L. J. Wheat. 1994. Diagnosis of histoplasmosis by antigen detection during an outbreak in Indianapolis, Ind. Arch. Pathol. Lab. Med. 118:1205-1208. [PubMed] [Google Scholar]