Abstract
Influenza virus of the H7N2 subtype has been introduced into noncommercial poultry in the United States, and this probably resulted in incidents of transmission of H7N2 virus to humans, documented in 2002 and 2003. This virus could be considered a potential threat to public health if it acquired person-to-person transmissibility. A favored approach for global pandemic preparedness includes development of prepandemic vaccines for any potential pandemic virus. To this end, we created a high-growth reassortant virus (H7N2-PR8) containing the genes for the hemagglutinin and the neuraminidase from a low-pathogenicity (H7N2) virus strain and the remaining six genes from a human vaccine strain (H1N1). The reassortant strain was evaluated to assess its antigenicity, safety, and protective efficacy using a mouse model. Antigenicity studies using ferret antibodies raised against H7N2-PR8 indicated that this virus confers broad cross-reactivity with divergent H7 viruses of different years and lineages. Mice and chickens inoculated with high doses of H7N2-PR8 supported virus replication but survived, indicating that this virus is comparable to other avian viruses of low pathogenicity. To assess the protective efficacy of H7N2-PR8, mice were immunized with two doses of formalin-inactivated H7N2-PR8, alone or with alum. Vaccinated mice subsequently challenged with highly pathogenic viruses from homologous and heterologous lineages A/Canada/444/04 (H7N3) and A/Netherlands/219/03 (H7N7) showed pronounced reduction of wild-type virus replication. These studies indicate that H7N2-PR8 is immunogenic, safe, and protective in animal models; these are the essential attributes to qualify for phase I human clinical trials as a prepandemic vaccine.
Influenza A viruses are enzootic among wild waterfowl (36). Viruses of the H5 and H7 subtypes can mutate from low to high pathogenicity after introduction into domestic poultry (2, 12, 29, 35). The high virulence of H5 and H7 viruses from poultry is generally contingent on the insertion of nucleotides in the hemagglutinin (HA) gene that encode basic amino acids at the cleavage site of HA0. This change renders HA cleavable by ubiquitous host cell proteases and facilitates systemic virus spread (3).
Recent outbreaks of H7 avian influenza in poultry have been associated with sporadic transmission to humans. In 2003, an outbreak of highly pathogenic avian influenza virus (subtype H7N7) in commercial poultry in The Netherlands resulted in transmission to people involved in poultry handling. Although most infected individuals developed only mild influenza-like symptoms, one individual developed acute respiratory distress syndrome and died (9, 14). In 2004, an outbreak of a highly pathogenic H7N3 occurred in poultry in Canada, infecting two humans that had close contact with poultry. Both patients developed conjunctivitis and influenza-like illness, which improved after oseltamivir therapy (23). These incidents and the current H5N1 outbreaks in Asia, Europe, and Africa have raised concerns about potential pandemics caused by viruses of the H7 subtype or by any other avian influenza viruses with the potential to be transmitted to humans and have promoted global preparedness to prevent such events (20, 21). For this reason, different H5N1 and H7N7 vaccine candidates have already been prepared to meet pandemic preparedness goals (8, 22, 30, 31).
Viruses of the H5 and H7 subtypes have caused outbreaks in commercial poultry in the Americas (1, 7, 11, 16, 17). These viruses constitute a lineage that is genetically and antigenically distinct from the European and Asian lineages which currently circulate in that hemisphere. Molecular analysis of multiple H7N2 isolates from outbreaks in U.S. poultry revealed that their HA genes are most closely related to the ones that have been circulating in live-bird markets in the northeastern United States since 1996 (28). Recent studies have indicated that, in these viruses, the HA cleavage site sequence is progressing toward a cleavage site sequence that fulfills the criteria established for highly pathogenic strains (27).
An outbreak of low-pathogenicity H7N2 avian influenza virus in turkey farms in Virginia resulted in the destruction of over 4.7 million birds (1). During this outbreak, one poultry worker reported a upper respiratory illness that was later found to be associated with H7N2 infection (4). An independent case of influenza-like illness caused by H7N2 occurred in 2003 in New York (5), but the source of this infection was not determined.
Evidence of H7 avian influenza virus infection in humans indicates that the constant circulation of H7N2 viruses in poultry constitutes a potential threat to public health. Here we report the development of a prepandemic human influenza vaccine, an antigenic representative of North American H7 genes from avian reservoirs.
MATERIALS AND METHODS
Parent virus strains, propagation, and quantification.
The parent virus strain was isolated from an affected animal during the 2002 low-pathogenicity H7N2 avian influenza outbreak (1). A/TurkeyVirginia/4529/02 (TK/VA/02) was characterized by Immunology and Pathogenesis Branch, Influenza Division, CDC, Atlanta, GA. This virus was selected as the donor of H7 HA and N2 neuraminidase (NA) based on antigenic (hemagglutination inhibition [HI] and microneutralization tests) and genetic characteristics (low pathogenicity and absence of extra sequences at the HA cleavage site). A/Johannesburg/82/96-PR8-RESVIR-12 (Joh/PR8, H1N1), provided by the Food and Drug Administration, was used as donor of the genes that encode the viral polymerases (PB2, PB1, PA), as well as NP, M, and NS (nucleotide sequences are available in the Influenza Sequence Database [19]). The five internal genes, encoding PB2, PB1, PA, M, and NS, are derived from A/PuertoRico/8/34 (PR8), whereas the NP, HA, and NA genes originate from A/Johannesburg/82/96 (Joh/96). The preparation of parent virus stocks and derivation of the reassortant seed were performed in accordance with Good Laboratory Practice guidelines. Virus stocks were propagated in the allantoic cavities of 10-day-old embryonated chicken eggs at 35°C for 48 h. The number of egg passages to generate and amplify reassortants was kept to a minimum to avoid spurious mutations. Virus stocks were prepared from seed previously subjected to two rounds of limiting dilution and stored at −80°C. Viral infectivity was determined by end point inoculation into embryonated eggs; the 50 percent egg infectious dose (EID50) was calculated by the method of Reed and Muench (25).
Generation of H7N2-PR8 high-yield reassortant virus.
A volume of 1 ml of TK/VA/02 placed in a 35-mm cell culture dish was exposed to UV light (100 μJ/cm2) from a UV cross-linker (CL1000UVP; 254 nm; UVP) for 6 seconds. The virus was immediately mixed with Joh/PR8, and 0.1 ml was inoculated into 10-day-old embryonated eggs. The eggs were incubated at 35°C for 24 h; allantoic fluid was harvested, diluted 1:100, and incubated with ferret antiserum against Joh/96 (H1N1). The mixture was incubated at room temperature for 40 min, and 0.1 ml was inoculated into embryonated eggs. After 24 h of inoculation, the allantoic fluid was harvested and diluted 1:1,000 for a second incubation with ferret antiserum. The mixture was inoculated into eggs, and after 48 h of incubation, allantoic fluid was harvested for RNA extraction using the QIA Amp viral RNA minikit (QIAGEN, Valencia, CA). Genotyping was performed by reverse transcriptase PCR (RT-PCR) analysis performed using the One-Step RT-PCR kit (QIAGEN, Valencia, CA) and segment-specific oligonucleotide primers designed to detect exclusively the presence of either TK/VA/02 or Joh/PR8 genes (primer sequences are available upon request). Sequencing reactions were performed using a Big Dye Terminator, version 3.1, cycle sequencing kit (Applied Biosystems, Foster City, CA) and subtype-specific primers. Analyses of influenza virus gene sequences were performed using BioEdit, version 7.0.0 (10), and MEGA, version 3.1 (15).
HI tests.
Ferret antisera against TK/VA/02 and H7N2-PR8 were produced for HI tests. For each virus, two adult lightly anesthetized female ferrets (Marshall Farms, North Rose, NY) were inoculated intranasally (i.n.) with 1 ml (106 EID50) of virus. Fourteen days after the first immunization, the ferrets were boosted on the footpad with 400 μl of a mixture containing 40 μg of sucrose gradient-purified virus with the synthetic adjuvant Titermax (CytRx Corporation, Norcross, GA). Blood was collected 2 weeks after boosting.
Ferret antisera against Joh/96 (H1N1) as well as the viruses A/Avian/NY/23/05 (H7N2), A/Avian/NY/24/05 (H7N2), A/NewYork/107/03 (NY/107/03, H7N2), A/Canada/444/04 (CAN/04, H7N3), A/Chicken/Chile/180-54/02 (CK/Chile/02, H7N3), and A/Netherlands/219/03 (NL/219/03, H7N7) were provided by the Virus Surveillance and Diagnosis Branch, Influenza Division, CDC, Atlanta, GA.
Prior to use in HI analyses, sera were treated with Vibrio cholerae NA (Denka-Seiken, Tokyo, Japan). HI tests were performed using turkey red blood cells, according to a WHO protocol (34).
Studies of pathogenicity in BALB/c mice.
Mouse inoculations were performed as described by Chen et al. (6) and Lu et al. (18). Fifty percent mouse infective doses (MID50) of H7N2-PR8, TK/VA/02, and CAN/04 viruses were determined by inoculating groups of 6- to 8-week-old female BALB/c mice (Charles River Laboratory, Wilmington, MA) i.n. with 50 μl of serial 10-fold dilutions of virus. Four mice from each group were euthanized 4 days postinfection (p.i.) to harvest lung, brain, spleen, and nasal turbinate tissues to determine viral infectivity titers. The remaining mice (five per dilution) were examined daily for signs of disease (ruffled fur, respiratory distress) and weighed during a total period of 14 days. Log-transformed viral titers were compared using a two-tailed t test.
Protective efficacy studies with a mouse model.
To prepare the inactivated H7N2-PR8 and TK/VA/02 virions for immunization, sucrose gradient-purified viruses were mixed with formalin (formaldehyde, 36.5 to 38%; Sigma) to a final concentration of 0.025% and kept at 4°C for 3 days. Loss of infectivity was established by two passages of the virus-formalin mixture in 10-day-old embryonated eggs.
The protective efficacy of vaccines was evaluated by intramuscular (i.m.) vaccination of groups of 6- to 8-week old female BALB/c mice (eight mice/group) with 10 μg of vaccine alone, 10 μg of vaccine mixed with alum (2%; Alhydrogel; Superfos Biosectors, Kvistgaard, Denmark), phosphate-buffered saline (PBS) only, or PBS mixed with alum in a final volume of 0.1 ml. Mice received a second i.m. injection after an interval of 2 weeks. All groups of vaccinated mice were challenged by i.n. administration of 106 EID50 (= 100 MID50) of CAN/04 or NL/219/03 and monitored for signs of disease during 14 days. Three mice per group were euthanized at 4 days p.i. for tissue collection and virus titration. To determine antibody titers, bleeding from the retro-orbital plexus was performed before the first and second immunizations as well as before termination of the study.
Studies of infectivity and pathogenicity in chickens.
Pathogenicity tests were performed as described by Chen et al. (6). Briefly, groups of eight 4-week-old pathogen-free White Leghorn chickens were inoculated intravenously (33) with a standard dose (0.2 ml of a 1:10 dilution of stock virus) of H7N2-PR8 (107.9 EID50/ml) or TK/VA/02 (107.1 EID50/ml). For infectivity tests, the viruses were inoculated i.n. (0.1 ml, 105.5 [H7N2-PR8] and 106.5 [TK/VA/02] EID50/ml). The birds were observed daily for signs of illness. Oropharyngeal and cloacal swabs were collected 3 days after virus inoculation and on day 14 p.i. The birds were bled and euthanized 2 weeks after inoculation. The presence of influenza virus-specific antibodies was determined by the agar gel precipitin test.
Laboratory biosafety.
All laboratory and animal studies that included infectious viruses of high pathogenicity or exotic avian viruses of low pathogenicity were conducted under approved biosafety level 3-enhanced protocols. Experiments using low-pathogenic North American viruses of avian origin (TK/VA/02 and H7N2-PR8) were conducted according to approved biosafety level 2 protocols.
RESULTS
Characterization of H7N2-PR8 reassortant virus.
The viral progeny from coinfection of eggs followed by two egg passages in the presence of antibody to the H1N1 parental virus were evaluated by limiting dilution and RT-PCR with lineage-specific primers to determine their genetic makeup (genotype). Viruses containing two genes encoding the major antigenic proteins of TK/VA/02 (H7 HA and N2 NA) and the six genes from Joh/PR8 were identified. These reassortants replicated efficiently in eggs, and after two passages in embryonated eggs without antibody pressure (anti-H1N1), a vaccine seed stock was prepared by pooling different clones out of end point dilutions (1,024 hemagglutinating units/50 μl, 1010.25 EID50/ml).
The antigenic properties of the H7N2-PR8 reassortant virus were analyzed by HI test with a panel of antisera to homologous and heterologous viruses (Table 1). As expected, the titers obtained with homologous ferret antisera (against either H7N2-PR8 or TK/VA/02) were high (from 10,240 to 2,560), which include the human case NY/107/03. Lower titers (80 and 320) were obtained with the North and South American H7N3 heterologous antigens as well as with the Eurasian NL/219/03 strain. The reduction in heterologous HI titers was proportionally larger with increasing percent amino acid sequence distances.
TABLE 1.
Antigenic analysis of H7N2-PR8 reassortant virus
| Strain (subtype)a | HI titer of ferret antisera against:
|
% Amino acid identity of HAb | |
|---|---|---|---|
| H7N2-PR8 | TK/VA (H7N2) | ||
| H7N2-PR8 | 5,120 | 10,240 | 100 |
| TK/VA/02 (H7N2) | 5,120 | 10,240 | 100 |
| Avian/NY/23/05 (H7N2) | 5,120 | 5,120 | 99.4 |
| NY/107/03 (H7N2)* | 2,560 | 5,120 | 98.4 |
| Avian/NY/24/05 (H7N2) | 2,560 | 5,120 | 97.2 |
| CAN/04 (H7N3)* | 320 | 320 | 91.8 |
| CK/Chile/02 (H7N3) | 80 | 320 | 82.1 |
| NL/219/03* (H7N7) | 80 | 80 | 79.9 |
*, virus with a history of infection in humans.
Percent identity compared to TK/VA/02 HA.
Pathogenicity and replication of reassortant virus in BALB/c mice.
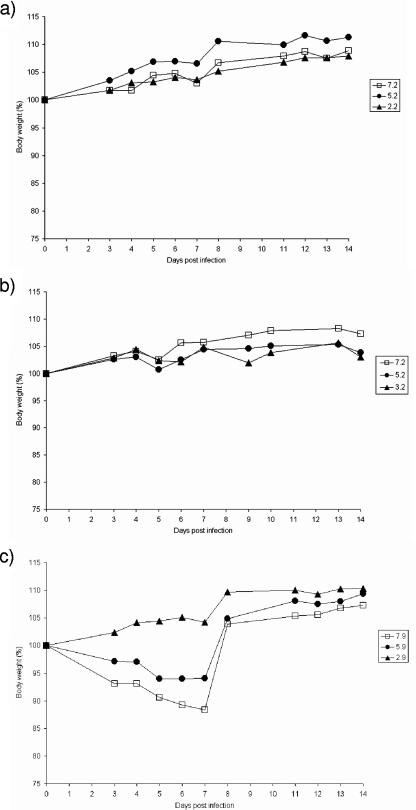
Mice infected with the parent virus TK/VA/02 (Fig. 1a) or H7N2-PR8 (Fig. 1c) did not show any signs of illness during the 14 days of observation. Mice inoculated with lower virus doses of TK/VA/02 or H7N2-PR8 (<7.2 and 7.9 log10 EID50, respectively) gained weight during the experiment (Fig. 1). Modest and transient weight losses were observed on day 7 p.i. in mice inoculated with the highest doses of H7N2-PR8 (12% and 5% weight reductions) (Fig. 1c). However, these animals recovered weight within the next 24 h.
FIG. 1.
Daily body weight recordings after infection with escalating virus doses. In order to assess the pathogenicity of TK/VA (a), CAN/04 (b), and H7N2-PR8 (c), groups of mice were infected i.n. with six different dilutions of either virus and monitored daily for signs of mortality and morbidity during a period of 14 days. The data shown are from mice inoculated with the lowest, highest, and intermediate virus concentrations only and are expressed in log EID50.
All groups of mice infected with H7N2-PR8 showed higher virus titers in lung than mice infected with TK/VA/02 (2 log10 EID50/ml difference; Table 2). There was no significant difference in viral titers between H7N2-PR8 and TK/VA/02 (P = 0.259). Likewise, virus titers from nasal turbinates were higher in mice infected with H7N2-PR8 although the difference was only 1 log10 EID50/ml compared to TK/VA/02 (P = 0.0408). Neither virus was detected in brains or spleens of inoculated mice.
TABLE 2.
Pathogenicity and replication of H7N2-PR8, TK/VA, and CAN/04 viruses in BALB/c mice
| Viruse | Log10 EID50 required for:
|
Mean virus titerb (log10 EID50/ml) ± SD in:
|
||||
|---|---|---|---|---|---|---|
| MLD50a | MID50 | Lung | Turbinate | Brain | Spleen | |
| H7N2-PR8 | >8.9 | 2.6 | 5.7 ± 0.9c | 3.7 ± 1.0c | NDf | ND |
| TK/VA (H7N2) | >8.2 | 5.8 | 3.7 ± 1.0d | 2.7 ± 1.0d | ND | ND |
| CAN/04 (H7N3) | >8.2 | 4.5 | 4.7 ± 0.8 | NAg | NA | NA |
| NL/219/03 (H7N7) | 2.6 | 0.87 | NA | NA | NA | NA |
MLD50, 50% mouse lethal dose.
Tissues were harvested on day 4 after inoculation. The lower limit of detection of virus in organs was 1.5 log10 EID50/ml.
Virus titers are expressed as the mean for 16 mice inoculated with virus dilutions ranging from 2.9 to 7.9 log10 EID50/ml.
Virus titers are expressed as the mean of six mice inoculated with virus dilutions ranging from 5.2 to 7.2 log10 EID50/ml.
CAN/04 and NL/219/03 were used for challenge studies.
ND, not detected (<1.5 log10 EID50).
NA, not applicable.
As a heterologous challenge virus, we selected CAN/04 due to its proven ability to infect humans. To establish an appropriate challenge dose in mice, we first determined the MID50 and 50% mouse lethal dose values. The MID50 was 4.5 log10 EID50 (Table 2). Although CAN/04 has high pathogenicity for poultry, no morbidity or mortality was observed in mice inoculated with 2.7 log10 MID50 during the 14-day observation period. All groups of mice gained weight in a fashion similar to the groups of mice infected with TK/VA/02 (Fig. 1b). Despite the lack of clinical signs of illness, lung titers of CAN/04 were 4.7 log10 EID50/ml, which provides considerable dynamic range to assess protection. Therefore, this CAN/04 virus was selected for challenge studies.
Pathotyping and replication of TK/VA/02 and H7N2-PR8 in chickens.
TK/VA/02 and the reassortant H7N2-PR8 did not cause mortality in chickens inoculated via the intravenous or i.n. route (Table 3). However, virus was isolated from oropharyngeal swabs in chickens inoculated i.n. with either TK/VA/02 or H7N2-PR8 (4.6 and 1.8 log10 EID50/ml, respectively). Low titers of virus could be isolated from cloacal swabs in the group of chickens infected with TK/VA/02, but no virus shedding was observed in the group infected with H7N2-PR8. Infection of chickens inoculated i.n. with H7N2-PR8 was evidenced by seroconversion in the agar gel precipitin test in all eight chickens inoculated intravenously and in five out of eight chickens (six out of eight seroconversions by HI test). All the chickens infected with TK/VA/02 via the either one of the two routes seroconverted.
TABLE 3.
Pathogenicity and infectivity of H7N2-PR8 and TK/VA in chickens
| Inoculation route | Virus | Challenge dose (log10 EID50/ml) | Mobidity (no. of chickens sick/total no.) | Mortality (no. of chickens dead/total no.) | No. of chickens that seroconverted/total no. bya:
|
Virus isolationb (log10 EID50/ml) from:
|
||
|---|---|---|---|---|---|---|---|---|
| AGP | HI | Oropharynx | Cloaca | |||||
| i.v.e | H7N2-PR8 | 7.9 | 0/8 | 0/8 | 8/8 | 8/8 | NAd | NA |
| TK/VA | 7.1 | 0/8 | 0/8 | 8/8 | NDc | NA | NA | |
| i.n. | H7N2-PR8 | 5.5 | 0/8 | 0/8 | 5/8 | 6/8 | 1.8 (8/8) | NA (0/8) |
| TK/VA | 6.5 | 0/8 | 0/8 | 8/8 | ND | 4.6 (8/8) | 1.0 (1/8) | |
| None | Sham | NA | 0/4 | 0/4 | 0/4 | 0/4 | NA | NA |
The HI test used homologous HI antigen (β-propiolactone inactivated). Chickens were sacrificed 14 days after inoculation, and sera were harvested.
Virus titers are expressed as means from eight chickens. The negative threshold for swab samples is <0.9 log10 EID50/ml. Values in parentheses are numbers of chickens sampled/total number of chickens in the group.
ND, not done.
NA, not applicable.
i.v., intravenous.
Immunogenicity and protective efficacy of formalin-inactivated H7N2-PR8 in mice.
In this study we compared the immune responses of mice to whole inactivated vaccines derived from TK/VA/02 or the H7N2-PR8 reassortant (Table 4). All mice immunized i.n. with inactivated vaccines developed detectable HI titers after a single dose; these titers were higher when the vaccine contained adjuvant. No HI antibody was detected in the sera of mice that received PBS or PBS plus alum. The second dose of vaccine resulted in substantial elevation of the titers elicited by the first dose, regardless of the presence or absence of adjuvant.
TABLE 4.
Immunogenicity of formalin-inactivated vaccines prepared against H7N2-PR8 and TK/VA
| Immunogena | Use of alum | HI titerb against indicated strain after challenge with:
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| CAN/04
|
NL/219/03
|
||||||||
| H7N2-PR8
|
TK/VA
|
H7N2-PR8
|
TK/VA
|
||||||
| Dose 1 | p.c. | Dose 1 | p.c. | Dose 1 | p.c.c | Dose 1 | p.c. | ||
| PBS | No | <20 | <20 | <20 | <20 | <20 | <20 | <20 | <20 |
| Yes | <20 | <20 | <20 | <20 | <20 | <20 | <20 | <20 | |
| H7N2-PR8 | No | 20 | 80-160 | 20 | 80 | 20 | 20-160 | 20 | 40-80 |
| Yes | 40 | 640-1,280 | 40 | 1,280 | 40 | 40-640 | 80 | 320-2,560 | |
| TK/VA | No | 20 | 80-160 | 20 | 80-160 | 20 | 20-40 | 20 | 40-80 |
| Yes | 20 | 320-1,280 | 20 | 320-1,280 | 20 | 20-1,280 | 20 | 320-2,560 | |
Groups of mice received two doses of 10 μg of formalin-inactivated vaccine or PBS with or without alum i.m. 2 weeks apart.
Serum samples were collected after two time points: a pooled sample was collected 2 weeks after dose 1, and individual samples from each of three mice were collected 4 days after challenge with either CAN/04 or NL/219/03 virus (p.c.). In the p.c. columns, values are ranges of HI titers from three mice unless otherwise indicated.
Data are from two mice only. One mouse did not show any immune response against either virus.
Each of the six groups of mice immunized with PBS, TK/VA/02, or H7N2-PR8, with or without alum as adjuvant, was divided at random into two and challenged with 100 MID50 of the CAN/04 (H7N3) or NL/219/03 (H7N7) strain.
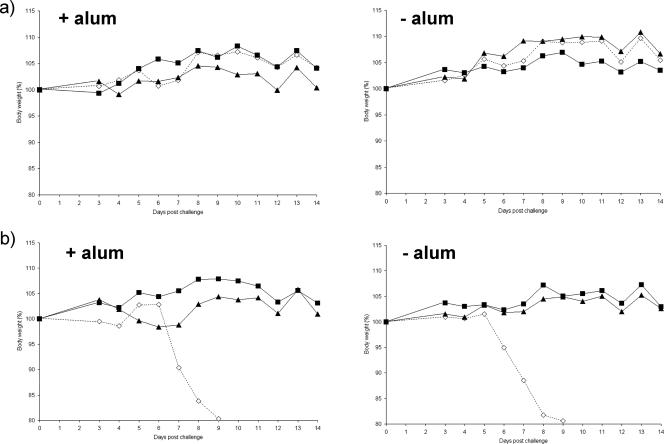
CAN/04 replicated in the lungs of the PBS- and PBS-plus-alum-immunized groups (5 to 5.2 log10 EID50/ml), as well as in the nasal turbinates (1.4 to 2.6 log10 EID50/ml), without inducing any clinical signs of disease (Table 5). No mortality or weight loss was observed in any of the groups of immunized mice challenged with CAN/04, including the groups that received PBS or PBS plus alum (Fig. 2a).
TABLE 5.
Protective efficacy of formalin-inactivated H7N2-PR8 reassortant vaccine
| Immunogena | Use of alum | Challenge virusb | % Survivalc | % Body wt on day 14 postchallenge | Challenge virus titersd in:
|
|||
|---|---|---|---|---|---|---|---|---|
| Lung | Turbinate | Brain | Spleen | |||||
| PBS | No | CAN/04 | 100 | 104 | 5.0 ± 0.46 | 1.4 ± 0.17 | <0.8 | <0.8 |
| Yes | 100 | 105 | 5.2 ± 0.64 | 2.6 ± 0.12 | <0.8 | <0.8 | ||
| H7N2-PR8 | No | 100 | 100 | <0.8e | 2.5 ± 0.64e | <0.8 | 1.2 (1/3) | |
| Yes | 100 | 106 | <0.8e | 1.3 (1/3)e | <0.8 | <0.8 | ||
| TK/VA | No | 100 | 104 | 3.7 (1/3)e | 1.7 (2/3)f | <0.8 | <0.8 | |
| Yes | 100 | 103 | <0.8e | <0.8e | <0.8 | <0.8 | ||
| PBS | No | NL/219/03 | 0 | 0 | 6.5 ± 0.4 | 1.6 (2/3) | <0.8 | 1.8 ± 0.42 |
| Yes | 0 | 0 | 6.8 ± 0.17 | 4.7 ± 2.36 | 2.0 (1/3) | 1.4 (2/3) | ||
| H7N2-PR8 | No | 100 | 100 | 2.5 (2/3)e | 4.4 (2/3)f | <0.8 | <0.8 | |
| Yes | 100 | 102 | <0.8e | <0.8e | <0.8 | <0.8 | ||
| TK/VA | No | 100 | 103 | <0.8e | <0.8f | <0.8 | <0.8 | |
| Yes | 100 | 102 | <0.8e | <0.8e | <0.8 | <0.8 | ||
Groups of mice (n = 8) were injected i.m. with two doses of 10 μg of formalin-inactivated vaccine alone, vaccine with 1% alum, or PBS alone, 2 weeks apart.
Mice were challenged i.n. 4 weeks after the second vaccine dose with 100 MID50 of CAN/04 or NL/219/03.
Five out of eight mice were monitored daily for 14 days after challenge. The rate of survival was determined at the end of the 14-day observation period.
Three out of eight mice were sacrificed on day 4 postchallenge, and virus titers in different organs were determined. Each virus titers is expressed as the mean log10 EID50/ml ± standard deviation for organs with positive virus isolation. The lower limit of detection of virus in organs was 1.5 log10 EID50/ml. The numbers in parentheses indicate the numbers of mice in which >0.8 log10EID50/ml virus was detected/total number of mice.
Lung titers significantly different compared with PBS controls (P < 0.05).
Lung titers not significantly different compared with PBS control (P > 0.05).
FIG. 2.
Protective efficacy of the H7N2-PR8 virus in BALB/c mice. Groups of mice were immunized with H7N2-PR8 (▴), TK/VA (▪), or PBS (⋄), either lacking adjuvant or containing alum. Each group was challenged with 100 MID50 of either (a) CAN/04 or (b) NL/219. Daily body weight was recorded for 14 days after challenge with homologous and heterologous viruses. The body weight variation is expressed as the percentage of averaged weight of each group of mice.
Vaccination with H7N2-PR8 virus alone protected mice from infection in the lungs, but CAN/04 was isolated from nasal turbinates (2.5 log10 EID50/ml; Table 5) and spleen (1.2 log10 EID50/ml) in one out of three mice. Mice immunized with H7N2-PR8 plus alum showed complete protection in the lungs (Table 5). Low-titer CAN/04 virus was detected in the nasal turbinate of one mouse (1.3 log10 EID50/ml). No virus was detected in spleen or brain. In mice immunized with TK/VA/02 plus alum, no virus was detected in any of the tissues. However, in the group of mice immunized without alum, virus was isolated from lungs (3.7 log10 EID50/ml) and nasal turbinates (1.7 log10 EID50/ml).
Weight loss and mortality were observed at days 5 and 6 p.i. in mice that were immunized with PBS or PBS plus alum and challenged with the highly pathogenic NL/219/03 strain (Fig. 2b). These groups had high virus titers in the lungs and nasal turbinates at 4 days p.i. (6.5 to 6.8 log10 EID50/ml and 1.6 to 4.7 log10 EID50/ml, respectively). Virus was detected also in brain tissues (2.0 log10 EID50/ml in one mouse) and spleens (1.8 to 1.4 log10 EID50/ml). In contrast, mice immunized with either H7N2-PR8 or TK/VA/02 in the presence or absence of alum did not reveal any signs of disease or weight loss after challenge with NL/219/03 (Fig. 2b). Both groups of mice that received adjuvanted vaccines were fully protected from challenge with NL/219/03 (Table 5). No virus was detected in lungs, nasal turbinates, spleens, or brains. Similar results were obtained in mice immunized with TK/VA/02 without adjuvant. However, in the group of mice immunized with H7N2-PR8 without adjuvant, virus was present in lungs (2.5 log10 EID50/ml) and nasal turbinates (4.4 log10 EID50/ml).
DISCUSSION
Several incidents of transmission of H7 subtype influenza viruses (H7N2, H7N3, and H7N7) from avian to humans have been reported in recent years (4, 9, 24, 32). Most infections involved poultry workers who were in close contact with infected birds during the outbreaks. Evidence of human-to-human transmission was also reported (14). Therefore, these viruses represent a risk for the human population and a potential for pandemic alert.
We selected TK/VA/02 as a donor of HA for reassortant vaccine because it is very similar to viruses that circulate in the farms that supply the New York live-bird markets (26). This HA lacks multiple basic amino acids at the cleavage site, eliminating the need for genetic manipulation before creating the reassortant. Nucleotide and amino acid analysis of HA sequences from H7N2 strains circulating in the United States showed that TK/VA/02 HA has at least 97% identity with the HA of currently circulating H7N2 North American virus strains. A high-growth H7N2-PR8 reassortant was produced in a Good Laboratory Practice laboratory using TK/VA/02 and Joh/PR8 to provide the two genes encoding HA and NA and the remaining six genes, respectively, through a conventional genetic-reassortment method (13). Antigenicity tests using ferret antiserum raised against H7N2-PR8 revealed that this serum exhibited the same reactivity as the antisera raised against TK/VA/02. Both antisera reacted to a panel of distinct H7 strains and lineages, which were isolated from different geographic regions.
Pathogenicity tests revealed that H7N2-PR8 and the parent virus, TK/VA/02, are viruses of low pathogenicity in mice and chickens. Both viruses were able to replicate in lungs and nasal turbinates of mice. H7N2-PR8 replicated at higher titers in mouse lungs than TK/VA/02, probably because the genes were derived from PR8, a virus highly adapted to replication by multiple laboratory passages in mice. By contrast, i.n. inoculated TK/VA/02 parent virus replicated to higher titers in chickens than H7N2-PR8, probably the result of the PR8 backbone, which has been shown to completely inhibit or severely restrict influenza A virus replication in chickens (6, 30).
Immunization of mice i.m. with the formalin-inactivated whole virus vaccines against H7N2-PR8 or TK/VA/02 elicited the production high titers of HI antibodies, detected 4 days after the mice were challenged. The presence of alum increased the humoral immune response significantly for both viruses and correlated with the protection against challenge. The groups of mice immunized with H7N2-PR8 or TK/VA/02 containing alum were protected against the two heterologous strains isolated in humans, the North American H7N3 strain, CAN/04, and the Eurasian H7N7 strain NL/219/03.
The pathogenicity of CAN/04 was assessed in mice, revealing that, unlike NL/219/03, this virus did not cause signs of pathogenicity in these animals but replicated at high titers in the lungs. The clinical signs observed in humans infected with CAN/04 or related virus can probably explain the mild pathogenicity that was observed in mice. In humans, conjunctivitis and other milder flu-like symptoms developed during infection (12).
H7N2-PR8 virus has been shown to be of low pathogenicity in mammalian and avian animal models. Vaccination was protective in mice after lethal challenge using a heterologous virus. Ferret and mice antibodies generated against the whole-virus vaccines cross-reacted with distantly related strains of the same subtype. H7N2-PR8 was shown to be a potential vaccine candidate that may also induce cross-protection in humans.
Acknowledgments
We thank Alexander Klimov for virus strains and Joan Beck for excellent technical assistance.
C.P. was supported in part by award N10-2004 from the National Vaccine Program Office, U.S. Department of Health and Human Services. D.E.S. was supported in part by USDA/ARS CRIS project 6612-32000-040.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry.
Footnotes
Published ahead of print on 3 October 2007.
REFERENCES
- 1.Akey, B. L. 2003. Low-pathogenicity H7N2 avian influenza outbreak in Virginia during 2002. Avian Dis. 47(Suppl.):1099-1103. [DOI] [PubMed] [Google Scholar]
- 2.Banks, J., E. S. Speidel, E. Moore, L. Plowright, A. Piccirillo, I. Capua, P. Cordioli, A. Fioretti, and D. J. Alexander. 2001. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch. Virol. 146:963-973. [DOI] [PubMed] [Google Scholar]
- 3.Bosch, F. X., W. Garten, H.-D. Klenk, and R. Rott. 1981. Proteolytic cleavage of influenza virus hemagglutinins: primary structure of the connecting peptide between HAl and HA2 determines proteolytic cleavability and pathogenicity of avian influenza virus. Virology 113:725-735. [DOI] [PubMed] [Google Scholar]
- 4.CDC. 2004. Update: influenza activity—United States, 2003-04 season. Morb. Mortal. Wkly. Rep. 53:284-287. [PubMed] [Google Scholar]
- 5.CDC. 2004. Update: influenza activity—United States and worldwide, 2003-04 season, and composition of the 2004-05 influenza vaccine. Morb. Mortal. Wkly. Rep. 53:547-552. [PubMed] [Google Scholar]
- 6.Chen, H., K. Subbarao, D. Swayne, Q. Chen, X. Lu, J. Katz, N. Cox, and Y. Matsuoka. 2003. Generation and evaluation of a high-growth reassortant H9N2 influenza A virus as a pandemic vaccine candidate. Vaccine 21:1974-1979. [DOI] [PubMed] [Google Scholar]
- 7.Davison, S., R. J. Eckroade, and A. F. Ziegler. 2003. A review of the 1996-98 nonpathogenic H7N2 avian influenza outbreak in Pennsylvania. Avian Dis. 47(Suppl.):823-827. [DOI] [PubMed] [Google Scholar]
- 8.de Witt, E., V. J. Munster, M. I. Spronken, T. M. Bestebroer, C. Baas, W. E. Beyer, G. F. Rimmelzwaan, A. D. Osterhaus, and R. A. Fouchier. 2005. Protection of mice against lethal infection with highly pathogenic H7N7 influenza A virus by using a recombinant low-pathogenicity vaccine strain. J. Virol. 79:12401-12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fouchier, R. A., P. M. Schneeberger, F. W. Rozendaal, J. M. Broekman, S. A. Kemink, V. Munster, T. Kuiken, G. F. Rimmelzwaan, M. Schutten, G. J. Van Doornum, G. Koch, A. Bosman, M. Koopmans, and A. D. Osterhaus. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc. Natl. Acad. Sci. USA 101:1356-1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hall, T. A. 1999. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp. Ser. 41:95-98. [Google Scholar]
- 11.Henzler, D. J., D. C. Kradel, S. Davison, A. F. Ziegler, D. Singletary, P. DeBok, A. E. Castro, H. Lu, R. Eckroade, D. Swayne, W. Lagoda, B. Schmucker, and A. Nesselrodt. 2003. Epidemiology, production losses, and control measures associated with an outbreak of avian influenza subtype H7N2 in Pennsylvania (1996-98). Avian Dis. 47(Suppl.):1022-1036. [DOI] [PubMed] [Google Scholar]
- 12.Hirst, M., C. R. Astell, M. Griffith, S. M. Coughlin, M. Moksa, T. Zeng, D. E. Smailus, R. A. Holt, S. Jones, M. A. Marra, M. Petric, M. Krajden, D. Lawrence, A. Mak, R. Chow, D. M. Skowronski, S. A. Tweed, S. Goh, R. C. Brunham, J. Robinson, V. Bowes, K. Sojonky, S. K. Byrne, Y. Li, D. Kobasa, T. Booth, and M. Paetzel. 2004. Novel avian influenza H7N3 strain outbreak, British Columbia. Emerg. Infect. Dis. 10:2192-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kilbourne, E. D. 1969. Future influenza vaccines and the use of genetic recombinants. Bull. W. H. O. 41:643-645. [PMC free article] [PubMed] [Google Scholar]
- 14.Koopmans, M., B. Wilbrink, M. Conyn, G. Natrop, H. van der Nat, H. Vennema, A. Meijer, J. van Steenbergen, R. Fouchier, A. Osterhaus, and A. Bosman. 2004. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363:587-593. [DOI] [PubMed] [Google Scholar]
- 15.Kumar, S., K. Tamura, and M. Nei. 2004. MEGA3: integrated software for molecular evolutionary genetics analysis and sequence alignment. Brief. Bioinform. 5:150-163. [DOI] [PubMed] [Google Scholar]
- 16.Lee, C.-W., D. E. Swayne, J. A. Linares, D. A. Senne, and D. L. Suarez. 2005. H5N2 avian influenza outbreak in Texas in 2004: the first highly pathogenic strain in the United States in 20 years? J. Virol. 79:11412-11421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu, H., P. A. Dunn, E. A. Wallner-Pendleton, D. J. Henzler, D. C. Kradel, J. Liu, D. P. Shaw, and P. Miller. 2004. Investigation of H7N2 avian influenza outbreaks in two broiler breeder flocks in Pennsylvania, 2001-02. Avian Dis. 48:26-33. [DOI] [PubMed] [Google Scholar]
- 18.Lu, X., T. M. Tumpey, T. Morken, S. R. Zaki, N. J. Cox, and J. M. Katz. 1999. A mouse model for the evaluation of pathogenesis and immunity to influenza A (H5N1) viruses isolated from humans. J. Virol. 73:5903-5911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macken, C., H. Lu, J. Goodman, and L. Boykin. 2001. The value of a database in surveillance and vaccine selection, p. 103-106. In A. D. M. E. Osterhaus, N. Cox, and A. W. Hampson (ed.), Options for the control of influenza IV. Elsevier Science, Amsterdam, The Netherlands.
- 20.Monto, A. S. 2006. Vaccines and antiviral drugs in pandemic preparedness. Emerg. Infect. Dis. 12:55-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monto, A. S. 2005. The threat of an avian influenza pandemic. N. Engl. J. Med. 352:323-325. [DOI] [PubMed] [Google Scholar]
- 22.Nicholson, K. G., A. E. Colegate, A. Podda, I. Stephenson, J. Wood, E. Ypma, and M. C. Zambon. 2001. Safety and antigenicity of non-adjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 357:1937-1943. [DOI] [PubMed] [Google Scholar]
- 23.Pasick, J., K. Handel, J. Robinson, J. Copps, D. Ridd, K. Hills, H. Kehler, C. Cottam-Birt, J. Neufeld, Y. Berhane, and S. Czub. 2005. Intersegmental recombination between the haemagglutinin and matrix genes was responsible for the emergence of a highly pathogenic H7N3 avian influenza virus in British Columbia. J. Gen. Virol. 86:727-731. [DOI] [PubMed] [Google Scholar]
- 24.Puzelli, S., L. Di Trani, C. Fabiani, L. Campitelli, M. A. De Marco, I. Capua, J. F. Aguilera, M. Zambon, and I. Donatelli. 2005. Serological analysis of serum samples from humans exposed to avian H7 influenza viruses in Italy between 1999 and 2003. J. Infect. Dis. 192:1318-1322. [DOI] [PubMed] [Google Scholar]
- 25.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 26.Senne, D. A., D. L. Suarez, J. C. Pedersen, and B. Panigrahy. 2003. Molecular and biological characteristics of H5 and H7 avian influenza viruses in live-bird markets of the northeastern United States, 1994-2001. Avian Dis. 47(Suppl.):898-904. [DOI] [PubMed] [Google Scholar]
- 27.Spackman, E., D. A. Senne, S. Davison, and D. L. Suarez. 2003. Sequence analysis of recent H7 avian influenza viruses associated with three different outbreaks in commercial poultry in the United States. J. Virol. 77:13399-13402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suarez, D. L., M. Garcia, J. Latimer, D. Senne, and M. Perdue. 1999. Phylogenetic analysis of H7 avian influenza virus isolated from the live bird markets of the northeast United States. J. Virol. 73:3567-3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suarez, D. L., D. A. Senne, J. Banks, I. H. Brown, S. C. Essen, C. W. Lee, R. J. Manvell, C. Mathieu-Benson, V. Moreno, J. C. Pedersen, B. Panigrahy, H. Rojas, E. Spackman, and D. J. Alexander. 2004. Recombination resulting in virulence shift in avian influenza outbreak, Chile. Emerg. Infect. Dis. 10:693-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Subbarao, K., H. Chen, D. Swayne, L. Mingay, E. Fodor, G. Brownlee, X. Xu, X. Lu, J. Katz, N. Cox, and Y. Matsuoka. 2003. Evaluation of a genetically modified reassortant H5N1 influenza A virus vaccine candidate generated by plasmid-based reverse genetics. Virology 305:192-200. [DOI] [PubMed] [Google Scholar]
- 31.Treanor, J. J., J. D. Campbell, K. M. Zangwill, T. Rowe, and M. Wolff. 2006. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. N. Engl. J. Med. 354:1343-1351. [DOI] [PubMed] [Google Scholar]
- 32.Tweed, S. A., D. M. Skowronski, S. T. David, A. Larder, M. Petri, W. Lees, Y. Li, J. Katz, M. Krajden, R. Tellier, C. Halpert, M. Hirst, C. Astell, D. Lawrence, and A. Mak. 2004. Human illness from avian influenza H7N3, British Columbia. Emerg. Infect. Dis. 10:2196-2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.U.S. Animal Health Association. 1994. Report of the Committee on Transmissible Diseases of Poultry and Other Avian Species. Criteria for determining that an AI virus isolation causing an outbreak must be considered for eradication, p. 522. In Proceedings of the 98th Annual Meeting of the U.S. Animal Health Association, Grand Rapids, MI. U.S. Animal Health Association. Richmond, VA.
- 34.Webster, R., N. Cox, and K. Stohr. 2002. WHO manual on animal influenza diagnosis and surveillance. WHO Global Influenza Programme. WHO, Geneva, Switzerland. http://whqlibdoc.who.int/hq/2002/WHO_CDS_CSR_NCS_2002.5.pdf.
- 35.Webster, R. G., Y. Kawaoka, and W. J. Bean, Jr. 1986. Molecular changes in A/Chicken/Pennsylvania/83 (H5N2) influenza virus associated with acquisition of virulence. Virology 14:165-173. [DOI] [PubMed] [Google Scholar]
- 36.Webster, R. G., W. J. Bean, O. T. Gorman, T. M. Chambers, and Y. Kawaoka. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152-179. [DOI] [PMC free article] [PubMed] [Google Scholar]